ECG for ventricular overload
The term “overload” implies dynamic ECG changes that appear in acute clinical situations and disappear after the patient’s condition normalizes. ECG changes are usually in the ST segments and T waves.
Left ventricular overload
The cause of overload of the left ventricle can be: long-distance running, intense training in athletes, physical overexertion, hypertensive crisis, attack of cardiac asthma... In these cases, the following is observed on the ECG in most cases:
- in the left chest leads V5, V6 – a decrease in the ST segment and a flattening or negative T wave;
- in leads I, aVL, overload of the left ventricle can manifest itself with a horizontal electrical axis of the heart;
- in leads III, aVF, overload of the left ventricle can manifest itself when the electrical axis of the heart is vertical.
Right ventricular overload
The cause of overload of the right ventricle can be: pneumonia, an attack of bronchial asthma, in an asthmatic condition, acute pulmonary failure, pulmonary edema, acute pulmonary hypertension... In these cases, the following is observed on the ECG in most cases:
- in the right precordial leads V1, V2 – a decrease in the ST segment and a flattening or negative T wave;
- sometimes these ECG changes are determined in leads II, III, aVF.
Diagnosis of LVH
Inspection
Left ventricular hypertrophy can be suspected already during the initial examination of the patient. Upon examination, the bluish color of the nasolabial triangle or hands, increased breathing, and swelling are alarming. When tapping, there are expansions of the boundaries of the heart. When listening - noise, dullness of tones, accent of the second tone. The survey may reveal complaints about:
- shortness of breath
- interruptions in heart function
- dizziness
- fainting
- weakness.
Left ventricular hypertrophy on the ECG shows a characteristic change in the voltage of the R waves in the chest leads on the left.
- In V6 the tooth is larger than in V. It is asymmetrical.
- The ST interval in V6 rises above the isoline, in V4 it falls below.
- In V1, the T wave becomes positive, and the S wave is higher than normal in V1.2.
- In V6, the Q wave is larger than normal and this is where the S wave appears.
- T negative in V5,6.
Systolic and diastolic ventricular overload
Systolic overload (resistance overload) of the ventricles occurs when there is an obstacle in the way of expulsion of blood from the ventricles that impedes blood flow (narrowing of the outlet from the ventricle; increased pressure in the pulmonary or systemic circulation). In such cases, the ventricle contracts, overcoming external resistance in systole, and its hypertrophy develops (ventricular dilatation is mild).
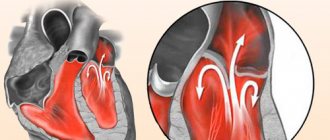
Diastolic overload (volume overload) of the ventricle occurs as a result of its overflow with blood, and the ventricle is overfilled with blood in diastole with an increase in the amount of residual blood in it. The cause of diastolic overload is valve insufficiency or increased blood flow, resulting in an increase in diastolic filling and muscle fiber length, leading to increased contractions of the ventricle. With diastolic overload, dilatation of the ventricle mainly occurs (hypertrophy is mild).
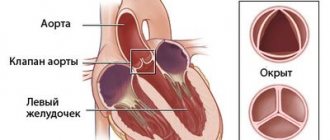
Left ventricular systolic overload
Common causes of left ventricular systolic overload:
- aortic stenosis;
- hypertonic disease;
- symptomatic and arterial hypertension;
- coarctation of the aorta.
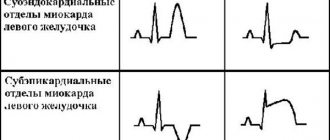
ECG signs of left ventricular systolic overload:
- qV5,V6 RV4 with deep SV1,V2;
- the STV5,V6 segment is located below the isoline, the TV5,V6 wave is negative (similar changes in the ST segment and T wave are usually observed in leads I, aVL);
- the activation time of the left ventricle in leads V5, V6 is increased and exceeds 0.04 s.
Right ventricular systolic overload
ECG signs of systolic overload of the right ventricle:
- high RV1,V2 (RV1 ≥ SV1), a high late R wave in lead aVR is often observed;
- the STV1,V2 segment is located below the isoline, the T wave is negative (similar changes in the ST segment and T wave are often observed in leads II, III, aVF);
- deviation of the electrical axis of the heart to the right;
- the activation time of the left ventricle in leads V1, V2 is increased and exceeds 0.03 s.
Diastolic overload of the left ventricle
ECG signs of left ventricular diastolic overload:
- qV5,V6 > 2 mm, but less than a quarter of a tooth RV5,V6 and less than 0.03 s;
- high RV5,V6 > RV4 with deep SV1,V2;
- the STV5,V6 segment is located on the isoline or slightly higher, the TV5,V6 tooth is positive (often high and pointed).
Diastolic overload of the right ventricle
A sign of diastolic overload of the right ventricle on the ECG is the appearance in leads V1, V2 of complete or incomplete blockade of the right bundle branch:
- The ECG looks like rsR' or rSR';
- The electrical axis of the heart is usually deviated to the right.
What is malignant hypertension and how to treat it
Have you been struggling with HYPERTENSION for many years without success?
Head of the Institute: “You will be amazed at how easy it is to cure hypertension by taking it every day...
Read more "
What can provoke a type of disease such as malignant hypertension? Unfavorable living conditions, constant stress, susceptibility to depression, and non-compliance with a healthy lifestyle have an extremely negative impact on the functioning of the “heart” organs. For this reason, many people, even in middle age, are faced with various pathological conditions. One of the most dangerous among them is the malignant form, the occurrence of which is influenced by certain factors.
Moments influencing the occurrence of the disease
Most often, malignant arterial hypertension reveals itself at the very beginning of its development with certain symptoms, which makes it possible to achieve success in identifying the causes of the disease and their subsequent rapid elimination.
Typically, high blood pressure occurs in people suffering from:
- renovascular hypertension, which consists in a violation of the supply of the necessary genetic material to the renal organs, is rarely detected in the early stages;
- diseases of the parenchymal type, causing excess pressure in every tenth patient;
- pheochromocytoma, which consists of inflammatory processes that occur in the adrenal region, is found in fifty percent of patients;
- inflammatory processes and tumor-like formations of the renal and adrenal organs, which requires immediate contact with a specialist to eliminate the risk of developing renal failure.
Symptomatic manifestations
Among the main signs of such a disease as malignant hypertension are the following:
- a feeling of “dirty” in the eyes;
- severe pain in the head and neck area;
- double image of surrounding objects;
- the occurrence of fainting conditions for no apparent reason;
- accompanied by increased blood pressure with nausea and vomiting;
- regularity of increases in blood pressure;
- an increase in controlled indicators mainly at night and in the evening;
- the occurrence of complications in the functioning of internal organs, which manifest themselves during the first two weeks after the onset of a systematic increase in pressure;
- deterioration in the ability to remember dates, numbers, names and other important information;
- a sharp deterioration in vision - up to the appearance of blindness in a short time;
- rapid weight loss;
- presence of a constant feeling of weakness.
Carrying out diagnostics
To identify a disease such as malignant hypertension, specialists usually resort to the following diagnostic methods:
- Personal examination and questioning of the patient allows you to find out more information about the symptoms that appear, which becomes the initial stage of the final diagnosis.
- Conducting laboratory tests of genetic and urinary materials - allows you to eliminate or confirm guesses about the presence of diseases relating to the kidneys and adrenal glands.
- Carrying out an ECG (electrocardiogram) makes it possible to clarify information about the state of the main organ in the “cardiac” system of the body.
- Constant recording of blood pressure makes it possible to see the dynamics of the development of the disease.
- Scanning the thyroid gland allows you to detect disturbances in its activity.
- Ophthalmological examination - provides information about the condition of the eye vessels and fundus, which is important for identifying the cause of constantly increasing pressure.
- Carrying out a study to identify the level of hormones in the body allows us to establish the presence of tumor-like formations in the body in the early stages.
Often, specialists use all diagnostic methods, since only having complete information about the functioning of the body will make it possible to make an accurate diagnosis and select optimal treatment methods.
Directions for treating the disease and possible complications after the crisis
Treatment of malignant hypertension is an extremely important measure that should be taken immediately after diagnostic procedures. This is due to the fact that hypertensive crises that occur against its background often cause death for the patient.
Well, the main task of specialists is to make such an outcome impossible in the early stages of the development of the disease.
The main methods of treating the pathological condition include:
- maintaining a healthy lifestyle;
- adjusting the diet to help reduce excess fat deposits;
- selection of physical exercises that will allow you to stay in shape without increasing blood pressure (blood pressure).
In addition, it is extremely important to take care of eliminating the cause that influenced the development of the disease. At certain stages of the development of the disease, the systematic use of medications that help normalize blood pressure begins. They can only be prescribed by a specialist who takes into account the individual characteristics of the patient. It is strictly forbidden to engage in independent “prescription” of medications, that is, self-medication.
If you do not take timely measures to eliminate the cause of the increase in pressure, and also do not begin treatment of the pathological condition, you can “earn” certain complications.
These include:
- a stroke condition that periodically results in disability or death;
- blindness occurring due to the effusion of blood into the retinal area of the eyes;
- ischemic disease arising due to inadequate blood supply to internal organs;
- angina pain that occurs in the chest area due to narrowing of the lumens in the vessels;
- a heart attack condition, often leading to death;
- diseases of the kidneys and adrenal glands.
However, if you turn to specialists in time and start treatment, you can extend your healthy life for many years.
Having found out what the illness presented above is, you should take care in advance to ensure that it is never recorded in a person’s outpatient card as a formidable diagnosis with unpleasant consequences. Achieving this is quite simple; it is enough to follow certain rules to maintain your own health. These primarily include maintaining a healthy lifestyle, observing the basic principles of proper nutrition, giving up bad habits, as well as maintaining a daily routine and moderate physical activity.
In such situations, you should not stay at home if hospitalization is proposed for additional examination or monitoring of the patient. Refusal of specialist help can lead to irreversible consequences, the worst of which is death.
What is left ventricular overload?
Ventricular systolic overload
in congenital heart defects, it is observed with isolated pulmonary artery stenosis (for the right ventricle), stenosis of the aortic mouth and coarctation of the aorta (for the left ventricle), diastolic - with blood discharge from left to right: atrial and interventricular septal defect, patent ductus arteriosus, transposition of the great vessels. With the development of pulmonary hypertension in these defects, systolic overload is added to the diastolic overload of the ventricles.
Due to heart overload
(systolic or diastolic), hyperfunction and hypertrophy of the myocardium of all parts of the heart develop early, but mainly of the ventricle on which the maximum load falls (L. D. Krymsky, 1962, 1963).
G. F. Lang
proposed to distinguish the following causes of heart failure: I - causing overwork of the heart muscle (heart defects, hypertension); II - disorders of the blood supply to the myocardium (diseases of blood vessels, anemia); III - direct chemical effect on the myocardium (intoxication, fasting, vitamin deficiencies, infections); IV - neurotrophic and hormonal (endocrine diseases).
Sometimes in the same patient
there is a combination of several reasons. For example, in most patients with congenital heart defects, overwork of the hypertrophied heart muscle is accompanied by circulatory disturbances caused by infection (pneumonia, childhood infections), which leads to an earlier development of clinically pronounced heart failure. In cyanotic heart defects, impaired blood supply to the myocardium also plays a role, due to the fact that mixed blood, poor in oxygen, enters the coronary arteries.
All types of heart failure
are characterized by the following changes in intracardiac hemodynamics: an increase in residual systolic volume, blood; increased end-diastolic pressure; dilatation of the heart; decrease in cardiac output; an increase in pressure in those parts of the circulatory system from where blood flows.
These shifts
lead to clinical manifestations of heart failure and metabolic disorders in various organs and tissues: disturbances of water and electrolyte metabolism, liver damage in the form of cardiac cirrhosis, damage to the kidneys and adrenal glands, in particular increased secretion of aldosterone, leading to an even greater increase in edema.
The clinical picture of heart failure
is varied. This depends on the rate of development of heart failure (acute or chronic) and the location of congestion.
G. F. Lang
distinguishes four types of heart failure depending on the location of pulmonary congestion (left ventricular);
in a large circle, with enlarged liver and edema (right ventricular); in the portal vein system, usually due to the development of liver cirrhosis; in the area of the head, neck and upper extremities (with compressive and effusion pericarditis). Foreign authors
divide heart failure into right ventricular, left ventricular and mixed forms.
Classification of heart failure
, which is currently used by most therapists and pediatricians, was proposed by G. F. Lang (1934) and developed by N. D. Strazhesko and V. X. Vasilenko (1949). Heart failure is divided into three stages:
I - latent: there are no symptoms of heart failure at rest; during physical exertion, shortness of breath, palpitations, and fatigue appear; hypertrophy and tonogenic dilatation of one or another part of the heart are noted;
II - severe: shortness of breath and tachycardia that occurs during light physical activity. The heart enlarges due to myogenic dilatation. Congestion develops in a large or small circle, depending on which part of the heart is decompensated.
This stage
usually divided into two periods: 1) symptoms of heart failure are not pronounced; 2) a pronounced clinical picture of heart failure occurring in the systemic and pulmonary circulation: enlarged liver, congestion in the lungs, edema;
III - dystrophic: symptoms of heart failure are accompanied by irreversible dysfunction of internal organs and metabolic disorders.
Right atrium overload: signs, causes, treatment methods, reviews
According to WHO statistics, more than 5 million people die every year from heart pathologies. Right atrium overload (RAO) or its hypertrophy is rare among cardiac pathologies, but its significance is great because it entails changes in other body systems.
A little physiology
The human heart includes 4 chambers, each of which, for certain reasons, can enlarge and hypertrophy. Typically, hypertrophy is an attempt by the body to overcome any organ failure with this compensation. Hypertrophy of the heart does not become an independent disease - it is a symptom of other pathologies.
The main function of the heart is to create blood flow to supply all tissues and organs with nutrients and oxygen.
Situations with GPP
Venous blood from the venae cava enters the right atrium. Overload of the right atrium occurs when blood enters from the vena cava in excess or with pulmonary hypertension, when blood from the right atrium to the right ventricle cannot pass immediately and completely. As a result, the atrium cavity begins to gradually expand and the wall thickens.
Another reason for overload of the right atrium is hypertension in the pulmonary circulation, which leads to hypertension in the right ventricle. For this reason, blood from the PP cannot immediately pass into the ventricle, which also leads to GPP. The load on the right side of the heart also increases with chronic lung diseases. The main reason is excess blood and pressure.
This condition occurs when there is stenosis of the tricuspid valve, which separates the atrium from the ventricle. In this case, some of the blood gets stuck in the atrium. Most often, this defect occurs after a rheumatic attack, with bacterial endocarditis.
Another defect is the insufficiency of the specified valve, in which its valves do not close completely and some of the blood returns. This condition occurs when the left ventricle dilates.
Pressure load will occur with pulmonary pathologies: bronchitis, emphysema, asthma, genetic disease of the pulmonary artery. These diseases increase the volume of blood in the ventricle, and after this the atrium becomes overstrained.
This is why overload of the right atrium and right ventricle are so often combined.
To restore normal blood flow, the atrium has to push blood out with greater force, and it hypertrophies. Overload of the right atrium develops gradually when the causative disease remains undiagnosed and untreated.
The time is individual for each patient, but the result is always depletion of the compensatory capabilities of the heart muscle and the onset of decompensated heart failure in a chronic course.
Other diseases leading to GPP
The development of right atrium overload can be provoked by:
- Myocardial remodeling - this phenomenon is considered part of post-infarction cardiosclerosis, when a scar develops at the site of necrosis. Healthy cardiomyocytes become more voluminous - they thicken, which outwardly looks like hypertrophied muscle. This is also a compensatory mechanism and most often involves the left ventricle. This creates another combination of right atrial overload and left ventricular diastolic overload.
- Postmyocardial cardiosclerosis - scar tissue is formed by the same mechanisms, but after inflammatory processes in the myocardium.
- Coronary heart disease - here we are talking about blockage of the coronary artery with a thrombus or plaque of atherosclerosis. This necessarily causes myocardial ischemia, and the contractile function of cardiomyocytes is impaired. Then the areas of the myocardium adjacent to the affected areas begin to thicken compensatoryly.
- Hypertrophic cardiomyopathy - occurs due to gene disorders in which uniform thickening of the myocardium of the entire heart muscle occurs. It is more often typical for children and involves the myocardium of the right atrium, then overload of the right atrium in the child is recorded.
Of the congenital pathological conditions of the heart muscle, heart overload is caused by:
- Defective septum between the atria. With such a deviation, the heart supplies blood to the right and left half of the heart under the same pressure, as a result of which the atrium receives an increased load.
- Ebstein's anomaly is a rare defect in which the atrioventricular valve leaflets are adjacent to the right ventricle rather than to the atriogastric ring. Then the right atrium merges with part of the right ventricle and also hypertrophies.
- Transposition of the great vessels - the main arteries of the cardiovascular system change their anatomical position - the main artery of the lungs is separated from the left parts of the heart, and the aorta is separated from the right. In these cases, GPP occurs in a child under 1 year of age. This is a very serious deviation.
- It is also possible to overload the right atrium in adolescents prone to fanatical sports. Regular physical activity is a common cause of HPP.
Symptomatic manifestations of pathology
GPP itself has no symptoms. Only symptoms associated with the underlying disease, which are complemented by venous stagnation, may be of concern.
https://www.youtube.com/watch?v=Bl2iGDwWkcc
Then we can say that signs of overload of the right atrium are shortness of breath even with minor exertion, pain behind the sternum.
Circulatory failure and cor pulmonale may develop. With cor pulmonale:
- shortness of breath in a horizontal position and with the slightest exertion;
- cough at night, sometimes mixed with blood.
Insufficient blood flow:
- heaviness in the right side of the chest;
- swelling in the legs;
- ascites;
- dilatation of veins
There may also be causeless fatigue, arrhythmias, tingling in the heart, and cyanosis. If these complaints arose only during infections and for the first time, you can count on their disappearance after treatment. For monitoring, a dynamic ECG is performed.
Diagnostics
There are no specific signs of pathology. It is only possible to assume the presence of overloads if a person suffers from chronic lung pathologies or has problems with valves.
In addition to palpation, percussion and auscultation, an ECG is used, which is used to determine some signs of right atrium overload on the ECG. However, even these indicators may be present only temporarily and disappear after the processes are normalized. In other cases, a similar picture may indicate the beginning of the process of atrial hypertrophy.
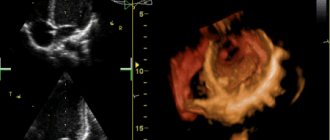
Ultrasound helps determine the increase in pressure and the volume of blood located in various parts of the heart. This method can detect disorders in all parts of the heart and blood vessels.
Pulmonary heart (P-pulmonale)
With it, pathological changes occur in the pulmonary circulation, and this is the main reason for overload of the right atrium.
On the ECG this is reflected by a modified P wave (atrial wave). It becomes tall and pointed in the form of a peak instead of the smooth apex of normal.
Functional overload of the right atrium on the ECG can also give an altered P - this is noted, for example, with overactivity of the thyroid gland, tachycardia, etc. Deviation of the heart axis to the right does not always occur only with HPP; it can also be normal in high asthenics. Therefore, other studies are used for differentiation.
If signs of right atrium overload are detected on the ECG, the patient is recommended to undergo echocardiography. It is considered safe for any category of patients and can be repeated many times over time. Modern devices can give answers about the thickness of the heart walls, the volume of the chambers, etc.
Together with echocardiography, the doctor may also prescribe Doppler ultrasound, then you can obtain information about hemodynamics and blood flow.
If there is a divergence of opinions, CT or radiography is prescribed. X-ray examination shows abnormalities of the right atrium and ventricle. Their contours merge with the contours of the vessels. In addition, an x-ray will show the condition of other structures of the chest, which is very valuable in case of pulmonary pathology as the root cause of HPP.
Consequences of GPP
In chronic diseases of the pulmonary system, the active alveoli are replaced by fibrous tissue, and the gas exchange area becomes smaller. Microcirculation is also disrupted, which leads to increased pressure in the pulmonary circulation. The atria have to actively contract, which ultimately causes their hypertrophy.
Thus, the complications and consequences of GPP are:
- expansion of the heart chambers;
- circulatory disorders, first in the small and then in the large circle;
- formation of the pulmonary heart;
- venous congestion and heart valve insufficiency.
If left untreated, pulse irregularities and attacks of heart failure may develop, which can lead to death.
Treatment
Normalizing the size of the atrium and improving the functioning of the heart muscle is only possible if the underlying disease – the cause of the pathology – is treated. Such treatment is always complex; monotherapy does not make sense.
In the presence of pulmonary pathology, these are bronchodilators (tablets and inhalers), antibacterial therapy for bacterial etiology of disorders, anti-inflammatory drugs.
For bronchiectasis, surgical treatment is used.
In case of heart defects, the best solution is corrective surgery. After heart attacks and myocarditis, it is necessary to prevent remodeling with the help of antihypoxic and cardioprotective drugs.
Antihypoxants are indicated: “Actovegin”, “Mildronate”, “Mexidol” and “Preductal”. Cardioprotectors: ACEs or angiotensin II receptor antagonists (ARA II). They can actually slow down the onset of chronic heart failure. More often than others, Enalapril, Quadropril, Perindopril, etc. are prescribed.
Nitrones, beta blockers (“Metoprolol”, “Bisoprolol”, “Nebivalol”, etc.), ACE inhibitors, antiplatelet agents that prevent the formation of blood clots, statins that normalize the amount of cholesterol are required.
Also used in treatment are glycosides (according to indications) and antiarrhythmics, agents that improve metabolic processes in the heart muscle. Judging by the reviews, good results were obtained when prescribing Riboxin.
Relapse Prevention
If drug therapy is the prerogative of the doctor, greater responsibility falls on the patient himself. Without his participation, the efforts of doctors will not produce results.
A person must definitely reconsider his lifestyle: give up smoking and alcohol, establish proper nutrition, eliminate physical inactivity, adhere to a daily routine, exercise moderate physical activity, and normalize body weight.
If pathologies of the cardiovascular and pulmonary systems become chronic, they cannot be completely cured.
The condition can only be improved by preventing exacerbations of these pathologies. Then the load on the cardiac system decreases.
GPP and pregnancy
During pregnancy, the body undergoes enormous changes not only in terms of hormonal balance, but also in the functioning of internal organs.
A difficult situation arises when diagnosing right atrium overload during pregnancy, which in this situation is considered an extragenital disease.
The diagnosis must not only be established, but also the woman’s ability to bear a fetus and give birth.
The best option, of course, is to diagnose heart pathologies before conception, but this does not always happen. Most often, pregnant women with heart pathologies are hospitalized three times during gestation; this is done to monitor the condition over time.
When first admitted to the hospital, the defect is examined, the activity of the process is determined and the work of the blood circulation is assessed, taking into account the question of a possible termination of pregnancy.
Repeated hospitalization is necessary because the physiological stress of the body to maintain the functioning of the heart muscle in a woman reaches its peak. The third hospitalization helps doctors choose the method of delivery.
Preventive actions
Prevention of right atrium hypertrophy begins with a review of the lifestyle, which involves proper balanced nutrition and a rational work and rest schedule.
If you are not a professional athlete and you do not necessarily need Olympic medals, do not show stubborn fanaticism in playing sports. This exhausts the body and exhausts the heart. The pressure in the circulatory system increases, and hypertrophy will not take long to occur.
Daily walks of an hour a day, swimming, and cycling are quite enough.
Another problem is eliminating stress. They also have a very negative impact on the functioning of the heart and the entire body as a whole. Yoga, meditation, and relaxation can help solve the problem.
Source: https://FB.ru/article/397136/peregruzka-pravogo-predserdiya-priznaki-prichinyi-metodyi-lecheniya-otzyivyi
What is left ventricular hypertrophy of the heart?
Cardiac hypertrophy, or, in other words, hypertrophic cardiomyopathy, is a thickening of the wall of the left ventricle of the heart, which leads to malfunction of the aortic valve. The problem is common among patients with hypertension, as well as athletes, people leading a sedentary lifestyle, addicted to alcohol and those who have inherited a tendency to pathology.
Myocardial hypertension of the left ventricles of the heart belongs to class 9 on the ICD 10 scale, along with other diseases of the circulatory system. This pathology is mainly a syndrome of other heart diseases, of which it exhibits indirect signs. In order to prevent possible problems in the future, it is necessary to intensively treat the hypertrophied organ in a timely manner, immediately after pathologies are detected.
Degrees of left ventricular hypertrophy
Depending on the signs of LVH and the size of the deformed muscle tissue, several stages of the development of the disease can be distinguished:
Moderate left ventricular hypertrophy (LVH) occurs as a consequence of hypertension or other heart disease. This seemingly insignificant increase signals an overload of the heart and that the risk of myocardial diseases (heart attack, stroke) for the patient increases. It often occurs without any symptoms and is detected only by ECG analysis. If the left ventricle is enlarged, it is necessary to be treated with the help of specialists, preferably in an inpatient setting.
Severe LVH is characterized by dystrophic changes in which the mitral valve is located close to the surface of the septum and interferes with blood flow, causing excessive muscle tension and stress on the left ventricle.
Classification by types of hypertrophy
Depending on the causative factors and the type of anatomical changes in the left side of the heart, the following types of pathology are distinguished:
- Asymptomatic hypertrophy syndrome in the left ventricle, detected only on an ECG;
- Concentric hypertrophy of the left ventricular myocardium;
- Eccentric left ventricular hypertrophy;
- with an increase in cavity;
— without changing the size of the left ventricular chamber;
- Asymmetrical form of thickening of the heart muscle.
The overall increase in heart size depends on the expansion of the ventricles and atria. With any type of reduction in the lumen of the aorta (stenosis due to a defect or with atherosclerosis), the load on the left ventricle increases, the muscle of which must work harder to pump the accumulated blood into the vascular system.
In this situation, an eccentric expansion of the cardiac cavity occurs. Concentric hypertrophy of the left ventricle, which occurs with hypertension, is caused by a pronounced systolic load during contraction: the heart muscle thickens due to increased work, and not due to the expansion of the cardiac chambers.
The first variant of cardiac changes is asymptomatic and typical in athletes and hard working people. With other types of pathology, symptoms and signs will certainly be present.
Enlargement of the left ventricle of the heart - causes
The causes of hypertrophy of the left ventricle of the heart can be varied, including both chronic and acquired diseases of different parts of the body:
- hypertension;
- obesity: the development of the disease is very dangerous in young children who are overweight;
- ischemia;
- diabetes;
- arrhythmia, atherosclerosis;
- frequent excessive physical activity;
- alcoholism, smoking;
- high blood pressure;
- lung diseases;
- aortic stenosis;
- disturbances in the functioning of the mitral valve;
- stress, psychological illness, nervous exhaustion.
The development of the body in a child can occur with disruption of the processes of myocardial repolarization and, as a result, an increase in the walls of the ventricle. If such a situation arises, it must be prevented, and then monitored on a regular basis throughout adulthood and prevent progression. Constant exercise can naturally lead to heart enlargement, while work associated with heavy lifting is a potential threat of systolic overload, so you should normalize your physical activity and monitor your health.
Another indirect cause is sleep disturbance, in which a person stops breathing for a short period of time. It can be observed in women during menopause or in older people and entails consequences such as expansion of the diameter of the heart vessels, growth of the septum and walls of the heart, increased blood pressure, and arrhythmia.
Treatment is considered successful if:
- obstruction at the exit of the left ventricle decreases
- The patient's life expectancy increases
- rhythm disturbances, fainting, angina pectoris do not develop
- heart failure does not progress
- quality of life improves.
Thus, left ventricular hypertrophy should be suspected, diagnosed and corrected as early as possible. This will help avoid severe complications with decreased quality of life and sudden death.
It’s good that there are such explanatory articles for people of all professions. This gives you an expanded understanding of your illness and allows you to catch yourself in time to try to restore your health. Thank you.
Thank you. Important and understandable information that cannot be obtained from a clinic doctor
I underwent medical examination. underwent an ECG. it is written there . left ventricular hypertrophy. went to the therapist. she looked at the cardiogram. and said everything is fine with my heart. and that's all. I have stage 2 hypertension. risk 2. pressure is 180 to 105. it varies. pulse 100. there may be less.more. hypertension for a long time. 30 years old, didn't ask. what you drink or don’t drink. doesn't matter. So she prescribed herself atenolol at a dosage of 50 mg and enalapril at a dosage of 20 mg. I hit it once in the morning and that’s it. The pressure drops. I also have a pulse.
The most important thing now is to find, as they say, your doctor. Doctors are also very different, although of course they are now far from being the same as they were in the USSR. Nevertheless, don’t be complacent by going to one or two doctors, and you will definitely find an attentive, sensitive, understanding doctor. who will prescribe the appropriate treatment for you. From my own experience, I can say that there is nothing worse than self-medication.
Hello Anna! I have the same CCC status parameters. Do you take both tablets in the morning or alternate according to a schedule? I would be very grateful for your advice.
Thank you for the competent and detailed article.
Thanks for the comprehensive information. I'm quitting smoking...
Thank you very much for the article, they really don’t even look at the clinic, everything is in accordance with age, but isn’t it possible to add the same sartans to my treatment (LOZAP+ Tablet in the morning and Concor 5 mg, maybe the LV mass will decrease (I have 145) but for me only 51 years old. If possible, please write in a personal message with what dosage to start taking them. Here is the ECG result from 09/15/2017 Rhythm irregularity 5% frequency of heart rate 90-92 beats per minute normal position of the EO, load on the left ventricle (LV mass index 145, with a norm of 110) Changes in the myocardium at the bottom. Thank you.
Hello Anna, I was diagnosed with stage 2 hypertension. risk 2. and left ventricular hypertrophy. They prescribed the following medications: bisoprolol 5 mg 1 time in the morning enalapril 5 mg 2 times a day ASA 100 mg 1 time in the evening after meals and atorvastotin 20 mg 1 time in the evening, try it and you should feel much better
And we have a local doctor in Moscow (Mitino). We needed an examination for a trip to a sanatorium. For the first time in my life I went to our clinic. Everything is automated, machines everywhere, recording, but the doctor doesn’t even want to watch or listen to the patient. Previously, they wrote on the chart, now they write on the computer, speak rudely, abruptly. I immediately receive SMS during the appointment - there is a list of tests that the doctor writes on the computer. That's the whole reception. The search for tests and specialists begins. They are also indifferent and cold. Keep their distance. But they are so cheerful when they chat among themselves! They can't talk enough. The patients wait patiently. Nothing has changed... Thank God that I have been regularly seeing Ph.D. for 15 years. Homeopathic doctor. Therefore, there are no special diseases. He looks at the device, uses computer programs, precisely selects the drug that is needed now. He immediately tells me what my sugar level is, whether I am at risk of cancer, what microelements I am missing, and so on. He reviews all tests and the condition of all organs in 20 minutes and talks about the condition and prospects for the functioning of the entire organism. Therefore, those who are treated by good homeopaths will never go to ordinary doctors. There they very often humiliate your human dignity and the doctors behave arrogantly. And patients don’t want to argue about homeopathy; they maintain their health and that’s it. If only Russian doctors would behave mercifully... In the meantime, you need to be healthy in order to undergo all the tests in our clinics. How can a sick person, especially a heart patient, cope with this? God forbid you get sick in Russia.
Signs of left ventricular hypertrophy
Symptoms of cardiomyopathy are not always obvious, and people are often unaware that there is a problem. If the fetus does not develop properly during pregnancy, there may be a congenital defect and hypertrophy of the left side of the heart. Such cases must be observed from birth and complications should not be allowed. But if there are periodic interruptions in the heart's function and a person feels any of these signs, the walls of the ventricle may be abnormal. The symptoms of this problem are:
- labored breathing;
- weakness, fatigue;
- chest pain;
- low heart rate;
- swelling of the face in the afternoon;
- disturbed sleep: insomnia or excessive sleepiness;
- headache.
{SOURCE}
What does it mean when a person’s blood pressure is 170 over 80, what to do?
High blood pressure is a problem for many hypertensive patients as it can lead to negative consequences. The danger is represented by pressure of 170 to 80, with an increased upper reading. Growing over 120 mm. rt. Art., it carries irreversible changes in the cardiac and vascular systems, as well as the brain.
When only the systolic pressure increases, while the lower pressure remains within the normal range, we speak of isolated systolic hypertension (ISH).
Description
Many people wonder when the tonometer shows a pressure of 170 to 80, what it means and what results can be observed. In this case, we are talking about one of the forms of hypertension, which leads to an increase in systolic pressure of more than 140 mm. rt. Art., while the lower one does not increase, is normal or slightly reduced.
With isolated systolic hypertension, any person, regardless of age and gender, feels unwell, is exhausted and feels the fear of death.
Epidemiology
One third of people with hypertension have ISH. In 25% of cases, this pathology develops in adults over forty years old; in young people it occurs only in 3%.
The prevalence of the disease increases with age; in patients over sixty years of age, the disease occurs in 40%. In medical practice, it has been established that isolated systolic hypertension increases the risk of death by 51%.
Causes
Wear and tear of blood vessels is one of the main mechanisms for the development of hypertension; this disease is most often observed in the elderly. With increasing age, the distensibility of the arteries decreases, calcium settles in them and atherosclerosis develops, which leads to a deterioration in their response to pressure fluctuations in the upper range.
Also, the appearance of ISH causes a slowdown in blood flow as a result of a slower ejection of blood from the heart. Answering the question about when the pressure is 170 to 80 and why there is a large gap, doctors note that such a large difference indicates a critical pathology of the cardiovascular system.
In young people, the onset of the disease is provoked by excessive consumption of alcohol and nicotine, fatty and salty foods. Also, an increase in blood pressure is affected by the presence of diseases such as diabetes, anemia, heart disease, kidney and adrenal tumors, stroke, prolonged stress, etc.
Doctors identify the following most common causes of the disease:
- Hormonal disorders;
- Consequences of diabetes;
- Severe stress;
- Disturbances in the functioning of the endocrine and cardiovascular systems;
- Obesity;
- Head injuries;
- Bad habits;
- Taking medications for a long period of time;
- High physical activity against the background of high blood pressure.
Forms of pathology
There are several forms of this disease:
- A medicinal form characterized by an increase in upper blood pressure due to long-term use of steroid hormones or contraceptives.
- Primary (essential), which develops for unknown reasons, the disease is inherited.
- Secondary (symptomatic) ISH, developing against the background of pathologies of the brain, kidneys, adrenal glands and other things.
- False ISH, which is observed in people who are afraid of doctors.
- Orthostatic ISH occurs as a result of head trauma and is often temporary.
Symptoms and signs
The most common symptom of the disease is pain in the head, which is accompanied by the appearance of dots before the eyes and dizziness. Representatives of the fairer sex often experience fainting, nausea, pain in the heart, decreased performance, weakness, and inability to perform physical activity.
In representatives of the stronger sex, the disease progresses faster due to the presence of addictions. Old people often experience so-called nocturnal hypertension, which may indicate the development of a stroke or heart attack.
The most common signs of pathology, which are observed in all patients, include:
- Pain syndrome in the head area;
- Fever and redness of the face;
- Increased heart rate;
- Presence of tinnitus;
- Palpitations.
Complications
In old age, the risk of developing complications and negative consequences of the disease increases. High upper pressure can lead to hypertensive crisis, stroke, heart attack or other serious pathologies, which can result in death.
If you do not respond to the manifestations of the disease and do not take appropriate measures, then there is a high probability of rupture of a vessel in the brain and hemorrhage into its cavity.
Diagnostics
The diagnosis is made when a person has a blood pressure of 140/90 mm. rt. Art. long period of time. The doctor prescribes examinations to identify the causes of the pathology. The patient needs to have a blood test and thyroid hormone tests, undergo an ultrasound of the kidneys and heart, an ECG, and a lipid profile.
Treatment
When the pressure is 170 over 80, doctors will tell you what to do. Treatment. First of all, it is aimed at reducing the risk of complications. To do this, the doctor prescribes medications and diet to the patient on an individual basis. It is recommended to forget about bad habits, lose excess weight, go for walks, and avoid stress.
Doctors often prescribe diuretics to patients, which help reduce the stroke volume of the heart, as well as beta-blockers to prevent complications from the cardiovascular system.
Calcium antagonists are also used for treatment, the action of which is aimed at relaxing blood vessels and stopping their spasms. If you have diabetes, doctors prescribe ACE inhibitors. The medications prescribed by the doctor are taken every day.
ethnoscience
For this pathology, it is recommended to use the following along with medications:
- Juices of beets, red and chokeberries;
- Infusions of motherwort, valerian and hawthorn;
- Garlic juice;
- Mulberries, currants and cranberries;
- Fresh vegetables and fruits.