Causes of rapid heartbeat
If your heart rate increases when falling asleep or after waking up, you should see a cardiologist as soon as possible. This condition may be a consequence of the progression of dangerous disorders not only of the cardiovascular system, but also of other systems. If the heartbeat increases at night, this indicates incomplete filling of the ventricles with blood. The deviation may be periodic or observed on an ongoing basis. Nocturnal tachycardia occurs for the following reasons:
- constant stress factors;
- impaired functioning of the cardiovascular system;
- hormonal imbalance in women that occurs during menopause and pregnancy;
- weight problems leading to obesity;
- endocrinological disorders;
- diseases of the gastrointestinal tract;
- malfunctions of the central nervous system;
- signs of asthma;
- rheumatic disease;
- hypoxia;
- accumulation of gases and air in the pleural cavity;
- pulmonary obstruction;
- thyrotoxicosis;
- allergic reaction.
Tachycardia can occur at night after a day full of stressful situations and strong emotional experiences or after watching a horror movie before bed. A nightmare can trigger an attack.
Also, increased heart rate is provoked by drinking coffee and other nervous system stimulants in the evening. Excessive consumption of alcoholic beverages and nicotine provokes withdrawal syndrome. Taking some medications can cause this side effect. Excessive exercise in the evening or a heavy late dinner can also cause heart problems.
Tachycardia after sleep usually occurs if a person, immediately after waking up, suddenly jumped out of bed and began to move actively, loading the barely awakened body.
If attacks occur occasionally and are associated with one of the factors listed above, then such cases should not be a cause for concern. By eliminating the provoking external factor and resting, you can easily restore normal heart rhythm.
If this condition occurs repeatedly, then we can draw a conclusion about the pathological origin of the symptoms and the need to undergo a medical examination.
A possible cause of tachycardia at night is chronic tension of the nervous system. Neurotic disorders sometimes occur latently, making themselves felt only by nightly attacks of panic attacks.
Another common cause of heart rhythm disturbances is sleep apnea. With this pathology, pulmonary ventilation is suspended for several seconds or even minutes. Due to the temporary cessation of breathing, the body is exposed to oxygen starvation. To compensate for the lack of oxygen, heart rate increases. The same problem can occur if you sleep in a poorly ventilated area.
Nocturnal tachycardia also has the following causes of development:
- heart pathologies;
- hormonal changes;
- endocrine disorders;
- thyroid diseases;
- disruptions in the functioning of the autonomic system;
- infectious diseases;
- lack of sodium in the blood;
- increased body temperature;
- imbalance of magnesium, potassium;
- anemia;
- allergy;
- asthma;
- pneumothorax;
- obesity.
A healthy person should not feel his heartbeat and any deviation becomes noticeable. A common type of arrhythmia is nocturnal tachycardia, which is characterized by an increase in heart rate.
The appearance of tachycardia in a person at rest or during rest may indicate the presence of heart problems. What are the causes of strong heartbeat at night, what signs are considered especially dangerous and what methods of treating the pathology are considered the most effective?
Causes of the symptom
A number of reasons can cause heart palpitations at night!
There are various reasons that can provoke rapid contractions of the heart. Exposure to external stimuli on the body causes various changes in the heart rhythm, but when they are eliminated, the pulse gradually normalizes.
Doctors identify the following factors that can cause increased heart rate:
- various diseases of the heart and vascular system
- insufficient oxygen
- dysfunction of the thyroid gland
- anemia
- rise in body temperature
- allergic reactions
- side effects from medications taken
- consuming large amounts of coffee and energy drinks
- strong emotions and experiences
- stress or fear
Some causes cause only temporary changes in heart rhythm. At the same time, there are reasons that pose a serious threat to the patient’s health and life.
Taking this factor into account, every person should pay attention to the state of their body and seek help from a specialist when the first alarming symptoms occur.
The fact is that with timely detection of pathologies, it is possible to get rid of them much faster and more painlessly.
There are various reasons why your heart rate may increase at night.
Medical practice shows that people who consult a doctor with this problem often have pathologies of the nervous and endocrine systems, as well as disturbances in their psycho-emotional state.
In addition, such night disturbances are often caused by anemia, body poisoning and internal bleeding.
At the same time, rapid heartbeat in the morning and at night can be one of the symptoms of heart failure.
If a person suffers from colds with an increase in body temperature, it is also possible that the heart rate may increase at night. In rare cases, the cause of this condition may be severe dehydration of the human body or a lack of certain substances.
A rapid heartbeat causes nighttime insomnia, since falling asleep in such a situation is quite problematic. This pathological condition can be provoked by constant nervous tension, frequent conflict situations in everyday life and excessive physical activity.
Normally, a person's heart rate is 60–90 beats per minute. A condition when the heartbeat is 90 or more beats per minute is called tachycardia in medicine. It can be physiological - a variant of the normal state, occurs in healthy people, disappears after rest, the patient does not feel any discomfort; and pathological - a sign of various diseases.
Tachycardia can occur during the day: during fright, after physical exertion, during emotional experiences, and even after drinking a cup of coffee.
Tachycardia at night during sleep occurs for the following reasons: watching a horror movie before bed, physical activity in the evening, drinking coffee or a too emotional day, as well as prolonged insomnia.
However, this condition can occur at night and for pathological reasons.
Elderly people often experience the manifestation of this pathology.
If the heart muscle contracts faster at night, there is a scientific and medical explanation for everything. Nocturnal tachycardia has its reasons. Below are the main ones:
- Decreased vagal tone. The frequency of contractions of the main organ slows down due to the influence of this nerve, and a decrease in blood pressure occurs. If nerve tone decreases, nocturnal attacks of tachycardia may occur.
- Panic attacks, neuroses. Mental illnesses can be the basis for the manifestation of accelerated heart contractions.
- Nocturnal hypertension. An increase in pressure at night provokes a rapid heartbeat. It is worth considering that hypertension can be an independent disease or the result of improper selection of medications.
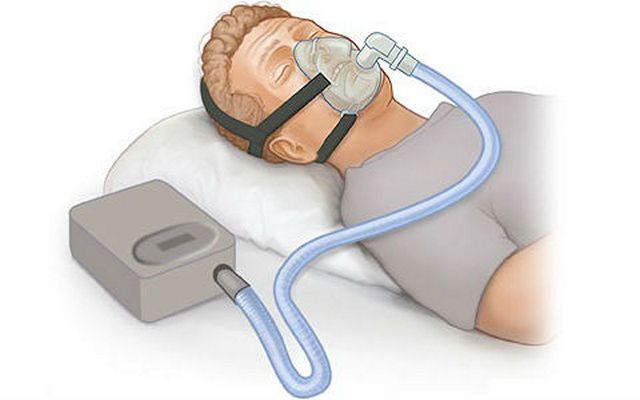
- Sleep apnea syndrome. A fairly common reason for tachycardia. Due to the temporary cessation of breathing during sleep, the heart does not receive enough oxygen, and this causes an increase in the load on it.
Tachycardia at night has other causes: heart disease, disruption of the endocrine system, excessive intake of alcohol-containing drinks, nicotine, incorrect dosage of medications, etc.
IMPORTANT! Only a doctor can identify the exact cause of nocturnal tachycardia. If the heart rate increases after sleep, this is a sign of possible pathologies in the human body.
Paroxysmal tachycardia also manifests itself as attacks. However, their duration varies greatly: it can be a couple of minutes, or maybe several days.
Have you ever woken up at night because your heart felt like it was going to jump out of your chest, that you were short of air, or that you felt afraid? All of the above are symptoms of nocturnal tachycardia.
If you experience such symptoms at night, it is not recommended to delay examination by a specialist. Correct diagnosis and prescribed treatment will help you cope with this disease. And life will sparkle with bright colors again.
Diagnostic methods
An accelerated heartbeat at any time of the day, including at night, when the muscle contracts more than 100 times per minute, indicates the presence of chronic tachycardia. It is necessary to treat this pathology. Diagnosis and treatment should be made by a doctor. To do this, it is initially necessary to identify the reasons why sinus tachycardia occurred.
Certain methods are used to diagnose the disease:
- Examination and interview of the patient. The probable prerequisites for the development of the disease, the presence of diseases in the chronic stage, and medications taken are identified. The pulse is taken and the blood pressure is measured. The skin is examined.
- General blood/urine test. The presence of inflammatory processes, as well as anemia, is revealed.
- Blood chemistry. The presence of diabetes mellitus or abnormalities in the kidneys is revealed. The chemical composition of blood is being studied.
- Hormone analysis. The functioning of the thyroid gland, as well as hormonal levels, are examined.
- ECHO of the heart muscle. Pathologies in the heart are detected.
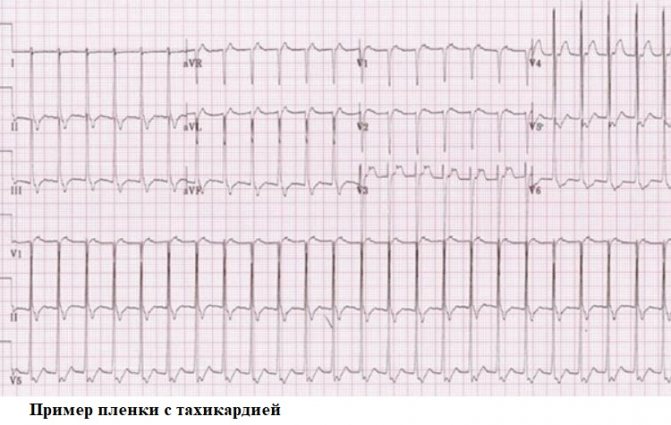
- ECG. The main way to diagnose tachycardia.
ATTENTION! Only after studying the results of all tests and examinations can the doctor prescribe a course of treatment individual for each patient. This is why you should not self-medicate or self-prescribe medications.
Treatment of the disease
Treatment
The basis of treatment for nocturnal tachycardia is medications. Traditional medicine methods are also widely used.
Medication
Drug therapy is aimed at treating the underlying disease, preventing the occurrence of new attacks, as well as preventing possible complications.
If nocturnal tachycardia occurs due to hypertension, appropriate antihypertensive therapy must be adjusted. If a person takes any medications, the specialist increases the dosage of the evening dose.
In the absence of antihypertensive therapy, the doctor prescribes the following drugs:
- ACE inhibitors (Enalapril, Enap 2.5-5 mg 1 time per day) or angiotensin receptor blockers (Losartan, Lozap 50 mg 1 time per day).
- If necessary, diuretics are added (Indapamide, Indap 2.5 mg once a day).

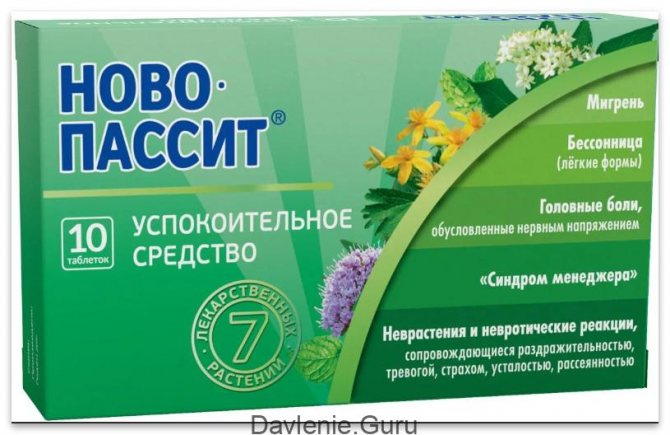
If tachycardia at night is provoked by mental disorders (neuroses, depression), the use of sedatives is indicated:
- Synthetic drugs - Afobazol 30 mg 3 times a day, Grandaxin 50 mg 2-3 times a day;
- Herbal preparations – “Novo-passit” 1 t. 3 times a day, “Dormiplant”, 1 t. 2 times a day, “Persen” 2 t. 2-3 times a day.
If a rhythm disturbance occurs due to sleep apnea, it is recommended to normalize your weight, sleep in a position on your side, and consult an ENT doctor. A good effect is achieved by using special devices that prevent blockage of the airway and snoring.
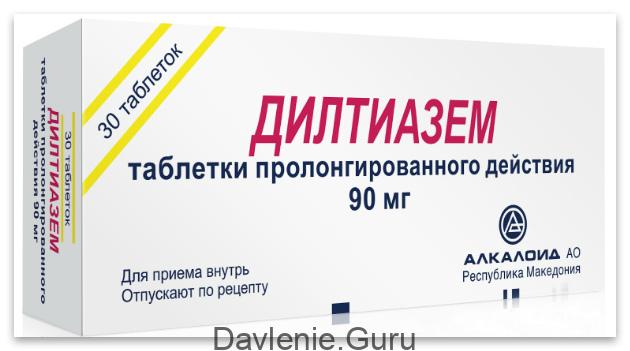
To prevent the occurrence of new attacks, the following medications are prescribed:
- Beta blockers (Bisoprolol 2.5-5 mg per day, Metoprolol 50-100 mg 2 times a day) - block receptors responsible for sensitivity to adrenaline;
- Calcium channel blockers (Diltiazem - 90 mg 2 times a day, Verapamil 40-80 mg 3 times a day) - block ion channels, preventing an increase in heart rate.
To prevent thrombosis, medications from the group of antiplatelet agents are prescribed (Aspirin Cardio, Thrombo Ass); in case of high cholesterol, taking statins (Atorvastatin, Liprimar) is indicated.
Folk remedies
You can also cope with nocturnal tachycardia using traditional medicine methods. Let's take a closer look at the recipes for some of them.
- Infusion of valerian root and motherwort herb. Take 100 g of each plant, pour 300 ml of boiling water and leave for 60 minutes. Then cool, strain and drink 100 ml 3 times a day. It is recommended to take the infusion over a course of 1 month.
- An infusion of mint, chamomile and caraway fruits. Take 5 g of each raw material, grind it and add 200 ml of hot water. Infuse for an hour and consume before bed for three weeks.
- Tea with hawthorn and rosehip. Take a teaspoon of green tea, a tablespoon each of rose hips and hawthorn. Mix the ingredients, pour 0.5 liters of boiling water and leave for half an hour. Take 2 times a day for 20 days.
- Nuts with honey. Take a walnut, chop and mix with one tablespoon of honey and the juice of a lemon wedge. Take the mixture orally with a small amount of water before bedtime.
- Melissa tincture. Take 100 g of dried raw materials and pour 40% alcohol or vodka into a glass. Leave for 10 days and take 5 ml several times a day, after diluting it in 50 ml of water.
- Zyuznik tincture. Take a 500 ml jar, fill it halfway with dried zyuznik herb and fill it with 40% alcohol or vodka. Let it brew for three weeks. Then strain and take 20 drops diluted with water 2 times a day for a monthly course.
- Infusion of white willow flowers. Take the flowers of the plant (10 g), pour 200 ml of boiling water and leave for an hour. Then strain and drink a quarter glass 4 times a day.
Main symptoms
Tachycardia manifests itself in different ways; clinical symptoms depend on age and concomitant diseases. Rapid heartbeat may be accompanied by a feeling of discomfort in the chest, a drop in blood pressure, and weakness. There may be a feeling of shortness of breath, dizziness, darkening of the eyes, fainting. A patient with angina pectoris experiences chest pain as a result of an imbalance between the heart's increased oxygen demand and decreased O2 delivery. In people with heart disease, an attack of tachycardia is accompanied by a sharp increase in shortness of breath.
Features of the floors
There are no particular differences between the manifestations of tachycardia in men and women, except for autonomic reactions and emotional overtones.
The heart beats and bubbles in the throat, gives rise to fever, severe sweating, trembling in the body - this is how the signs of tachycardia in women are vividly described. They are more likely than men to have chronic non-paroxysmal sinus tachycardia - a disease when heart rate does not correspond to the level of physical activity or emotional stress. A possible mechanism for its development is considered to be an anomaly of the sinus node or increased automaticity of the heart.
Postural orthostatic tachycardia is also predominantly characteristic of women. It is accompanied by an inadequate increase in heart rate when the body position changes from horizontal to vertical.
Why does the crash occur?
Few people know why their heart rate increases before bed. In most cases, this condition is attributed to overexertion during the day or stress. That is, a manifestation that has no serious basis. In fact, this is the beginning of the development of tachycardia. At the initial stage, an increase in heart rate is not accompanied by other symptoms. Lack of attention leads to the patient turning to a specialist when complications arise: pain in the chest, bradycardia, pathological changes in the structure of the heart. Tachycardia may be accompanied by the following symptoms:
- heavy breathing, shortness of breath;
- dizziness, nausea;
- headaches, migraine;
- muscle spasms in the chest, back, neck;
- Feeling of a lump in the throat.
How to recognize the symptoms?
The symptom may be preceded by an anxious state in a person.
Tachycardia upon awakening or before bedtime is accompanied by a special clinical picture that is difficult not to detect. The patient exhibits the following symptoms:
- constant anxiety that may occur in the middle of the night;
- poor sleep leading to insomnia;
- rapid heart rate, due to which the patient feels pulsation;
- frequent headache;
- feeling of weakness;
- sharp pain in the heart area;
- semi-fainting state;
- darkening of the eyes;
- tremor of the limbs;
- increased sweating, with the release of liquid and cold sweat;
- feeling of suffocation.
Why is the problem disturbing?
Hormonal disbalance
If the patient’s heart is pounding strongly, even when he is at rest, then you can contact an endocrinologist. More often, strong blows and heavy breathing are associated with impaired functioning of the thyroid gland, which produces insufficient or excessive amounts of certain hormones. Thyroid dysfunction can be provoked by constant stress, psycho-emotional tension and other unfavorable factors. An unpleasant feeling worsens with anxiety or nervous tension. The feeling of rapid heartbeat with a normal pulse goes away only after the functioning of the thyroid gland is normalized.
Often the patient can feel the pulse and hear the heart beating due to diffuse toxic goiter, which increases the sensitivity of the blood vessels.
Impaired cardiovascular function
A rapid heartbeat with a calm pulse can be a consequence of the development of various vascular diseases. Constant strong heartbeat is often associated with pathological processes such as:
An increased heart rate with a normal pulse may be associated with arrhythmia.
- Arrhythmia. In this case, the patient experiences an acceleration of the pulse. The pathology is accompanied by disrupted cardiac impulses, which causes an uneven heartbeat.
- An infectious focus in an internal organ. In medicine, such conditions are known as myocarditis and endocarditis. If there is a deviation, you not only feel your heart pounding, but you also experience fever and a change in skin color. Against the background of pathology, the functioning of other internal organs is often disrupted.
- Changes in heart tissue. Deviations are often explained by the development of myocardial dystrophy or cardiosclerosis.
- Heart defect. The heartbeat is felt with such a disorder, which may be congenital or acquired.
- Constant high blood pressure. In a healthy person, blood pressure levels are within the range of 120 to 80 mm Hg. Art. When they increase, hypertension is recorded, which is accompanied by headache and dizziness.
Return to contents
What other reasons are there?
A loud heartbeat and normal pulse may indicate other problems, including:
- vegetative-vascular dystonia of various types;
- high body temperature;
- decreased hemoglobin level;
- neurosis.
Women may feel a pathological condition during menopause.
In women, a feeling of palpitations against the background of a normal pulse can be observed during menopause, while the patient complains of other unpleasant symptoms, such as pain in the head, weakness. You can often feel your heart beating when you are physically tired or stressed. Intoxication of the body can also contribute to the development of the disorder. In this case, it is enough to eliminate the provoking factor, and the signs of heavy heartbeat will go away on their own.
Clinical case
In my practice, there was a case of sinus tachycardia in a pregnant woman. The woman constantly felt a rapid heartbeat, which was an adaptive reaction of the body: pressure decreased, heart rate increased; but the patient was also diagnosed with anemia. After correcting the hemoglobin level with iron supplements, her health improved and the feeling of palpitations disappeared. Although at first the woman was sincerely surprised when she was not prescribed drugs to slow down her pulse!
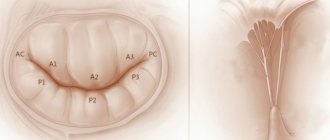
Depending on the location of the source of excitation, tachycardias are divided into supraventricular and ventricular.
The first arise in the structures of the heart up to the level of branching of the trunk of the His bundle: in the atria, AV node, in additional conduction pathways. The source of origin of the latter is the His bundle, Purkinje fibers, and ventricular myocardium.
Based on the nature of the course, paroxysmal and non-paroxysmal types of pathology are distinguished.
According to the mechanism of occurrence - reciprocal, ectopic, with trigger activity, and so on.
Differential diagnosis of arrhythmias is a difficult and responsible task. In particular, when it comes to tachycardia with wide QRS complexes on the ECG. This may be a ventricular arrhythmia or tachycardia involving the accessory tract (accessory tract).
Ventricular tachycardia has a poor prognosis and occurs as a result of damage to the heart muscle. In contrast, arrhythmia involving the AP appears in a person without gross structural pathology of the heart.
To clarify the type of tachycardia, an ECG with an intrathoracic lead should be recorded or a transesophageal electrophysiological study should be performed. However, in real clinical practice, such an opportunity is rarely provided, and in these situations the doctor is guided by the following rule: assess the condition as the most dangerous to human health and life and begin appropriate treatment.
Diagnostic procedures
To make a diagnosis, your doctor may prescribe the following procedures:
- Electrocardiography. It may not be very informative when diagnosing attacks that occur only at night. In this case, daily electrocardiogram monitoring is prescribed.
- ECG Holter monitoring is continuous recording of data using a special portable device for a day or more. This diagnostic method allows you to monitor the functioning of the heart muscle even during sleep and determine the frequency and duration of episodes of heartbeat disturbances.
- If daily monitoring does not produce results, TEE is prescribed - diagnostics of the conduction system of the heart using an electrode inserted through the esophagus. Weak electrical impulses are applied to the heart through an electrode and an electrocardiogram is observed.
- Echocardiography is an ultrasound examination of the heart and the functioning of its individual structures.
If heart pathology has not been identified, an additional examination by other specialists is prescribed, including a consultation with a psychiatrist. Additional diagnostic procedures are prescribed: study of blood composition, urine analysis, ultrasound of the thyroid gland, hormone analysis.
With such symptoms, the patient would benefit from an echoencephalographic study.
- laboratory and biochemical blood tests;
- general urine analysis;
- hormonal tests to determine thyroid dysfunction;
- electrocardiogram, which is the main diagnostic technique;
- echoencephalography.
Prevention of tachycardia that occurs at night during sleep
Even if the symptoms of tachycardia do not appear at night, during sleep, it never hurts to check yourself. And if suspicious signs of an increase in heart rate periodically emerge, then an examination must be completed.
Nowadays, the following methods are used to diagnose tachycardia:
- Electrocardiography is the study of electric fields generated by the activity of the heart. The method may provide little information for tachycardia, which makes itself felt only at night when the patient is sleeping and does not bother him at other times of the day. During the ECG procedure, an attack may simply not be detected.
- Holter ECG is a method for diagnosing the functioning of the heart with electrodes attached to the patient’s body for a long period of time - for a day, including at night, an electrocardiogram is recorded. The data enters the computer and is analyzed by specialists. This method allows for a comprehensive assessment of heart function.
- Esophageal examination of the heart using electrodes inserted through the esophagus.
- EchoCG is one of the types of ultrasound of the heart. Thanks to it, you can visually verify the normal functioning of the heart, its valves, blood vessels, or detect disturbances in their functioning, manifested by nocturnal tachycardia.
Diagnostics: when and with what to see a doctor?
Causes of the symptom
Rapid heart contractions at night can be caused by various factors. The problem occurs with cardiac diseases and under the influence of physiological factors.
Pathological
Frequent heartbeats observed at night may be due to:
- High blood pressure. If blood pressure increases during sleep, then one of the symptoms of this is tachycardia. Hypertension can act as an independent disease or occur as a result of improperly selected hypertensive drugs. In this case, it is necessary to make adjustments to the dosage or select other means.
- Low blood pressure. Hypotonic patients often suffer from nocturnal tachycardia. Increased heart rate occurs when hypotension occurs in combination with vegetative-vascular dystonia, iron deficiency anemia, and increased anxiety. With such problems, sleep is disturbed, as the patient constantly wakes up. Tachycardia is complemented by paleness of the skin, fear and panic. If symptoms are pronounced, you must call an ambulance.
- Pregnancy. During the period of bearing a child, global changes occur in the body, so many women suffer from tachycardia, which can also bother you at night. In most cases, the reasons for this are not pathological. A doctor's help is necessary for tachycardia with chest pain, dizziness, nausea, and fainting. The expectant mother should eat right, avoid stress and excessive exertion, and get proper rest. Then rapid heartbeat will not bother you.
- Panic attacks. If a person experiences severe anxiety attacks at night, he or she suddenly wakes up with a strong heartbeat, sweats excessively, suffers from shortness of breath and numbness in the limbs. This problem is psychological in nature, so to eliminate it you need to consult a psychotherapist.
- Decreased tone of the vagus nerve. One of the main components of the autonomic nervous system is the vagus nerve. At night, it helps slow the heartbeat and lower blood pressure for proper rest of the body. If its tone decreases, then the sympathetic part of the nervous system works more actively and at night the person’s blood pressure rises and tachycardia bothers them.
- Sleep apnea syndrome. Nocturnal tachycardia often occurs for this reason. In this condition, the upper respiratory tract collapses and breathing stops during sleep. During such episodes, the load on the heart muscle increases and hypoxia occurs. When breathing is held, the heart rate increases. The problem most often affects overweight people, mainly men.
Only a doctor after an examination can determine what exactly caused the tachycardia.
Physiological
Even a healthy person can suffer from increased heart rate. Tachycardia is usually observed in people with increased nervous sensitivity. The problem also occurs when:
- insufficient amount of minerals in the body;
- drinking drinks containing caffeine at night;
- high room temperature and insufficient air supply;
- strong emotional stress;
- use of certain medications;
- disorders in the digestive system, which are accompanied by a slight elevation of the diaphragm.
It is possible to normalize the heart rate by eliminating the influence of these factors on the body.
Causes of palpitations at night also include heart pathologies, endocrine system dysfunction, alcohol and nicotine poisoning, infectious diseases, and anemia.
Rapid heartbeat at night may indicate pathological processes in the heart. At the same time, a person clearly feels every heartbeat.
In normal condition, the organ should contract at a frequency of 60-90 beats per minute. If the pulse exceeds these values, then tachycardia is diagnosed.
At night and during the day, arrhythmia can appear for the same reasons, but at night a person feels a rapid heartbeat more clearly.
During periods of wakefulness, heartbeats remain invisible. A person rarely notices a rapid pulse. At night, for the body to fully rest, it must slow down, so tachycardia at this time of day is considered a serious stress for the body.
The problem appears:
- feelings of fear and anxiety for no apparent reason;
- feeling of lack of air;
- premature awakening;
- the appearance of cold sweat.
If there are no deviations in the functioning of the cardiovascular system, then the heart rhythm can return to normal in a short time without any therapeutic measures. This is possible in cases where tachycardia occurs due to physiological reasons.
In addition to the main symptoms indicating pathology, a person suffers from a deterioration in general health, dizziness and fainting.
There are cases where an increased heart rate after waking up resulted in myocardial infarction and other dangerous pathological conditions.
Any first-time attack of tachycardia that negatively affects your well-being is a reason to consult a doctor! And the more pronounced the clinical manifestations, the sooner you need to consult. If a person loses consciousness during a paroxysm, it is necessary to immediately call an ambulance and perform electrical cardioversion (impact of a pulsed current discharge on the heart).
Doctor's advice: check-up list for suspected tachycardia
To establish a correct diagnosis, the following studies and tests are necessary:
- electrocardiogram - at rest and at the time of rapid heartbeat;
- Ultrasound of the heart - data on the structural structure and valve apparatus;
- daily ECG monitoring;
- transesophageal EPI (TEPE);
- general blood test - will provide information about the presence of anemia and/or inflammation;
- blood test for thyroid hormones and TSH;
- consultation with an ENT doctor (if you have a history of frequent sore throats) and a dentist (caries) to identify and treat foci of chronic infection.
This is the minimum research that will help establish the cause of tachycardia, its nature and type, or allow you to choose a further diagnostic direction. Often, the doctor needs to seek help from fellow arrhythmologists who are able, using modern instrumental methods, to determine the area with pathological impulses. After its localization becomes known, the issue of minimally invasive destruction of the lesion can be decided.
If rapid heartbeat is the result of chronic tonsillitis, then by eliminating the cause (by performing surgical removal of the tonsils), you can forget about the heart problem. Such patients complain of pain in the heart area. Why chest discomfort occurs with a sore throat and how to act correctly - read here.
If the study reveals changes in thyroid hormone levels, or pheochromocytoma is suspected, then an endocrinologist will treat such a patient. It is worth noting that in clinical practice the first symptom of thyrotoxicosis is paroxysm of atrial fibrillation. Therefore, all patients with new-onset atrial fibrillation need to determine the concentration of thyroid hormones in the blood.
Monitoring a person with tachycardia first of all involves monitoring by a specialist who treats the underlying disease. It is a competent approach to the pathology that causes arrhythmia that will help get rid of unpleasant symptoms and minimize the consumption of medications.
Etiology and pathogenesis of tachycardia development
So, there are 2 main types of tachycardia, each of which has its own causes and pathogenesis of development. Physiological tachycardia is an absolutely normal phenomenon in people of all ages and is not a consequence of heart pathologies.
Pathological tachycardia is not an independent phenomenon, but is always a symptom of a disease of the cardiovascular system. One of the most characteristic features of pathological tachycardia is the suddenness of its development.
All causes of tachycardia at night can be divided into cardiac and extracardiac. Diseases of the cardiovascular system that often provoke tachycardia include:
- congestive and acute heart failure;
- heart defects;
- severe forms of angina;
- bacterial endocarditis;
- cardiosclerosis;
- myocarditis of various etiologies;
- cardiomyopathy;
- myocardial infarction;
- exudative and adhesive pericarditis.
Tachycardia is especially common in adolescents. The reason for this phenomenon lies in the hormonal changes in the body.
In this case, tachycardia especially often manifests itself at night. Pathological tachycardia, which manifests itself both at night and during the day, is a dangerous symptom, as over time it leads to various disorders of internal hemodynamics, as well as a decrease in the volume of ejected blood.