Description of the procedure
In telling what defibrillation is, it should be noted that the procedure is characterized by passing a discharge through the chambers of the heart to restore rhythm and proper functionality.
This is what a defibrillator device is needed and used for. If the goal is to save the patient’s life, then the procedure is carried out by the ambulance team that arrives on call.
It is important to remember that defibrillation is not effective in cardiac arrest.
First, it is necessary to perform indirect cardiac massage and artificial respiration, and only when functions and independent contractile movements have been restored is it permissible to resort to this procedure. Cardiologists, rheumatologists and emergency physicians have the skills to operate the device.
If the procedure is carried out when the electrical activity of the heart is stable, its contractile activity may be disrupted, which will lead to cessation of blood circulation. And with asystole, clinical death occurs.
Methodology
When carrying out resuscitation measures, ambulance teams use the method of electrical cardiac defibrillation. Diagnosis of circulatory arrest in a patient is made using a cardiogram, under the control of which the procedure is carried out.
Process on video:
It has the following sequence of actions:
- The patient is placed on a flat horizontal surface.
- Take off clothes and jewelry hanging on the chest.
- A special gel is applied to the electrodes, which promotes better current conduction. If it is not available, you can use gauze soaked in 7% sodium chloride solution.
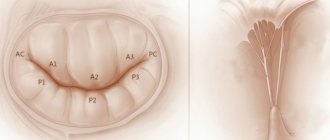
- It is important to correctly position the electrodes on the chest: the first is installed on the left just above the apex of the heart, the second - under the right collarbone. If the patient has a pacemaker, the electrodes should be placed no closer than 8 centimeters from it.
- The electrodes should be pressed to the body with a force of 8-10 kg.
- Turn on the defibrillator and set the required power (the charge strength is calculated individually). There are defibrillators that detect this indicator automatically.
- While the electrodes are being charged, the patient can undergo indirect cardiac massage and artificial respiration.
- Before giving a shock to the patient’s body, it is necessary to make sure that at this moment no one from the medical personnel touches him or touches the surface where he is lying.
- After making sure it is safe, the doctor delivers a shock, then checks the pulse manually (on the carotid artery) or the patient is connected to an electrocardiography machine, where changes will be recorded.
- If there are no changes, then a second discharge of stronger power is applied. While charging the electrodes, perform cardiopulmonary resuscitation (indirect cardiac massage, CPR).
The procedure for providing assistance can be repeated up to four times, but if this does not give any therapeutic effect, then the patient’s death is declared.
Defibrillation in emergencies
Electrical stimulation of the heart is divided into:
- Defibrillation, when measures are taken to normalize the ventricular rhythm.
- Cardioversion, in which manipulations are associated with the restoration of atrial rhythm, and all actions are monitored by an ECG.
In the first case, the procedure is performed in emergency mode, when the orderly heart rhythm is disturbed. The patient is unconscious. First they give a shock of 200 J, then it reaches 360 J.
Cardioversion can be either planned or urgent. This procedure is usually prescribed for a certain time, but the patient’s written consent is required before it is performed. During the procedure, he remains conscious under the influence of a sedative.
What is happening is reflected on the monitor, and everything is synchronized with the QRS rhythm. The voltage during cardioversion is lower than during defibrillation; a shock of 50-200 J is delivered.
In critical situations, a defibrillator is used to eliminate ventricular arrhythmia. The patient in this case is unconscious.
There are several pathological conditions when this procedure is indicated:
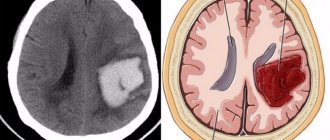
- Ventricular fibrillation, the rhythm is accelerated and erratic.
- Fluttering when the rhythm is orderly but accelerated.
- Tachycardia when drug treatments are ineffective.
Sometimes, against the background of these disorders, hypotension or heart failure can be observed.
The clinical picture develops according to the following scenario:
- The man loses consciousness.
- Heart contractions accelerate chaotically.
- The pulse cannot be felt.
- The patient is diagnosed with clinical death.
Resuscitation should be carried out in the first minutes. If medical assistance is not provided in a timely manner, biological death may occur and electrical defibrillation will no longer be effective.
Briefly about cardioversion
Cardioversion (electrical pulse therapy) is a procedure performed for patients with pathophysiological heart rhythm disorders. Its goal is to restore normal sinus rhythm.
There are two types of it:
- Pharmacological (drug) cardioversion is the intravenous administration of antiarrhythmic drugs (Cordarone, Amiodarone, etc.), which is carried out under strict monitoring of the patient’s condition.
- Electrical cardioversion (atrial defibrillation) is a method that leads to coordinated contraction of the heart muscle. This occurs due to the impact of a strong electrical impulse on it. The voltage is 50-200 J. When performing the procedure, synchronization with the electrocardiogram is performed, which reduces the risk of developing ventricular arrhythmia.
Cardioversion is planned, performed in a hospital setting and has special pre-hospital training. There are cases of emergency cardioversion, for example, in case of atrial fibrillation, aggravated by angina pectoris or heart attack.
The procedure requires special equipment - a cardioverter.
II. Confirmation of a person's death.
The death of a person is declared when the brain or biological death of a person occurs (irreversible death of a person).
Biological death is established based on the presence of cadaveric changes (early signs, late signs).
The diagnosis of “brain death” is established in health care institutions that have the necessary conditions for ascertaining brain death.
The death of a person on the basis of brain death is established in accordance with the Instructions for ascertaining the death of a person on the basis of a diagnosis of brain death, approved by order of the Ministry of Health of the Russian Federation dated December 20, 2001? 460 “On approval of the Instructions for ascertaining the death of a person based on the diagnosis of brain death” (order registered by the Ministry of Justice of the Russian Federation on January 17, 2002 No. 3170).
Treatment of cardiac pathologies with a defibrillator
Cardioversion can be performed either urgently in case of a sudden attack of tachycardia, or plannedly in case of tachyarrhythmia, if it is not controlled by medication. An urgent procedure is needed when the arrhythmia can turn into fibrillation, while the patient is in a pre-infarction state, he is diagnosed with heart failure, low blood pressure.
During planned treatment, electrical stimulation techniques and the use of drugs can be combined.
In the case of atrial fibrillation, the cardioversion procedure is used for:
- Lack of proper effect from drug treatment.
- The presence of paroxysmal arrhythmia along with Wolff-Parkinson-White syndrome.
- Intolerance to drugs for arrhythmia.
- Increased frequency of relapses of paroxysmal arrhythmia.
- Insignificant effectiveness of drug treatment of persistent forms of atrial fibrillation pathology.
Popular models. Defibrillator "DKI-N-10" is the most popular device
This domestic device is quite popular. Its kit includes: a portable part with electrodes for children and adults, replaceable batteries and a charger for them. The first element is made in the form of a monitor; it displays information about the operating characteristics of the device and the patient’s heart performance indicators.
The defibrillator-monitor is portable, therefore it retains all the capabilities of professional devices. When working with it, you can use the voice prompt function. The liquid crystal display displays all the information about how the treatment is progressing. The device has an integrated printer that allows you to quickly print the necessary indicators.
The DKI defibrillator is used not only in medical institutions, it is also used by mobile teams. The device has an enhanced heart rate assessment mode and even a separate ECG channel.
III. Termination of resuscitation measures.
• when a person is declared dead on the basis of brain death, including against the background of ineffective use of the full range of measures aimed at maintaining life;
• if resuscitation measures aimed at restoring vital functions within 30 minutes are ineffective.
No resuscitation measures are carried out.
• If there are signs of biological death.
• When a state of clinical death occurs against the background of progression of reliably established incurable diseases or incurable consequences of acute injury incompatible with life.
Note. This instruction does not define the conditions for refusal to use resuscitation measures or their cessation in newborns and children under 5 years of age.
Prognosis after CPR.
The favorable outcome of CPR in a hospital setting currently ranges from 22 to 57%, the discharge rate of surviving patients is 5-29%, of which 50% leave with a neurological deficit. The outcome of prehospital CPR is an order of magnitude lower (G. Baltopoulos, 1999). The leading complication in people who have experienced clinical death is the development of post-resuscitation illness.
• want to help;
• know how to do it;
• be able to.
Cardiac defibrillation: precautions
The procedure involves the use of electric current, which requires careful handling. To avoid harm to themselves or the patient, people performing defibrillation must follow a number of strict recommendations:
- At the moment of delivering the shock, you must not touch the patient or the surface on which he was placed. Do not touch metal parts on the electrodes.
- If oxygen was supplied at this time, this process must be interrupted. An electrical discharge may cause a fire.
- A large gathering of strangers is unacceptable near the patient. No more than two people should operate the devices.
- After defibrillation, the capacitor should be discharged immediately.
- Do not allow two electrodes to come into contact with each other. Especially if there is a special electrically conductive gel on their surface. Failure to do so may result in a short circuit.
- To prevent burn injury to the skin of the chest, it is necessary to apply significant mechanical force (up to 8-10 kg) to the installed electrodes. This will also reduce resistance and reduce current.
- The defibrillator is not placed on the woman's breast area. It is also prohibited to install electrodes in the area of an implanted pacemaker.
- The procedure cannot be used in the presence of normal electrical activity of the heart. Otherwise, serious disturbances in contractile activity may occur, up to asystole.
Indications for the procedure
Defibrillation: indications
Electrical defibrillation can be performed for health reasons. It is performed in an urgent, relatively urgent and planned manner. In the first case, this method is used when there is no time for drug preparation. The patient's life is measured in minutes or seconds. Emergency defibrillation is performed when acute cardiac arrhythmias occur, which lead to sudden cessation of blood circulation and severe heart failure: ventricular fibrillation (VF), ventricular flutter, ventricular tachycardia, high frequency atrial flutter.
In a relatively urgent manner, electrical defibrillation is used for those conditions that do not lead to a sharp increase in heart failure, but at the same time are not corrected by the use of medicinal methods to restore the heart rhythm. This group includes supraventricular recurrent paroxysmal tachycardia, paroxysmal atrial flutter or fibrillation, and ventricular tachycardia.
Contraindications for defibrillation
There are no contraindications for urgent or emergency defibrillation. If the procedure is carried out as planned, then temporary contraindications are the use of cardiac glycosides. After 3 days of discontinuation of these drugs, elective defibrillation can be performed. This condition is explained by the fact that when the body is saturated with cardiac glycosides, there is a risk of developing irreversible ventricular fibrillation.
The next contraindication for restoring heart rhythm is a permanent form of atrial fibrillation lasting more than 2 years. Arrhythmias that arise against the background of a sharp increase and dystrophic changes in the ventricles, sinus tachycardia, thrombi in the atria, polytopic atrial tachycardia, accelerated AV nodal rhythm are also a contraindication to routine defibrillation.
Defibrillation is carried out as an emergency procedure for ventricular fibrillation, when they contract chaotically at a speed of 200-300 beats/min. The danger of the condition is that due to this rate, the ventricles are not completely filled with blood and blood circulation is impaired. There is usually no pulse.
Also, indications for urgent defibrillation are ventricular flutter, when the speed also reaches 250-300 beats/min, but the contractions are rhythmic. This condition is dangerous due to the transition to fibrillation.
When performing defibrillation, the patient's life is put first and all other factors are not taken into account. The only contraindication is complete cardiac arrest. But during planned cardioversion it is unacceptable to carry out manipulation if:
- The patient is taking cardiac glycosides. Otherwise, it may cause ventricular fibrillation.
- Chronic course of heart failure in the stage of decompensation.
- At the time of the procedure, the patient suffers from an acute infectious disease.
- There are contraindications for the use of anesthesia.
- Electrolyte disturbances were detected.
- There are blood clots in the atria.
- Polytopic atrial or sinus tachycardia was diagnosed.
- Ventricular hypertrophy or dystrophy is observed.
How is elective cardioversion performed?
The patient is prepared for this type of electrical pulse therapy. Preparation scheme:
- An ECG is recorded.
- A transesophageal examination (EchoCG) is performed to detect blood clots in the heart chambers.
- A laboratory blood test is ordered to check potassium levels.
- The patient must make his own decision and give consent.
- When 3-4 days remain before the expected date of the procedure, cardiac glycosides are discontinued.
- Before cardioversion, you must take a 4-hour break without eating or drinking.
The method of conducting planned electrical stimulation includes:
- Preoxygenation (saturation of the body with pure oxygen).
- Immersion of the patient in shallow general anesthesia.
- Preparation and installation of equipment, as with defibrillation.
- Monitoring ECG, blood pressure.
- Delivery of discharges that need to be cardiac synchronized, that is, combined with the QRS complex or with the R wave (this must be done so as not to cause ventricular arrhythmia).
20.4.1. Laryngospasm
Etiology. Mechanical or chemical irritation of the respiratory tract.
Pathogenesis. The syndrome is based on a reflex spasm of the striated muscles that regulate the functioning of the glottis.
Clinic. Against the background of relative well-being, the victim suddenly develops stridor breathing, signs of acute respiratory failure (ARF) of the 1st degree quickly appear, which within a few minutes turns into ARF of the 2nd-3rd degree; this is accompanied by loss of consciousness, disruption of the cardiovascular system and the development of a coma. Death occurs from asphyxia.
Urgent Care. In case of complete laryngospasm, a pathogenetically substantiated method of treatment is general curarization of the patient, followed by tracheal intubation and transfer to mechanical ventilation. Currently, apart from muscle relaxants, there are no other drugs that can quickly (within several tens of seconds - 1 minute) relieve spasms of striated muscles.
If it is not possible to immediately transfer the patient to mechanical ventilation using muscle relaxants, emergency conicotomy is indicated (see section 20.4.3. Foreign bodies of the upper respiratory tract). Tracheostomy in this situation is not indicated due to the complexity and duration of the surgical intervention (3-5 minutes). After eliminating laryngospasm and transferring the patient to mechanical ventilation, nonspecific antihypoxic therapy is carried out.
Steps
Part 1
Preparing to use an AED
- Confirm cardiac arrest.
- Make sure the patient is completely dry.
Make sure the victim is not wet before turning on and using the AED. Otherwise, wipe it dry. If the victim is in close proximity to water, move him to a dry area.
Turn on the AED.
After making sure there is no water, turn on the AED. When the device turns on, instructions for use will be displayed on the screen. The instructions will tell you how to insert the wires with electrodes into the device. Typically, they simply need to be inserted into the slots above the flashing light at the top of the device.
Prepare the victim's chest.
Before attaching the electrodes, remove all unnecessary items from the victim's chest. Unbutton or cut your shirt. If the victim has thick chest hair, you will have to shave it off. Also try to look for signs of implanted devices such as a pacemaker. Remove all metal jewelry and accessories as metal conducts electricity.
Attach the electrodes.
The electrodes are adhesive pads. The instructions for the AED will tell you that electrodes or pads must be placed on the victim's body. Make sure they are in the correct places to ensure the victim receives the maximum shock needed. One pad must be glued under the collarbone in the upper right part of the victim’s chest, and the second under the pectoral muscles on the left, in the lower part of the heart, along the side.
If you see a person in need of emergency care, make sure they are actually in cardiac arrest before using an AED. Make sure the victim is unresponsive, not breathing, and has no pulse. Use the ABC rule. If there is no pulse or breathing, begin artificial respiration.
Try to wake the victim.
If you find a person and don't know how long they have been unconscious, make sure they are awake and that they really need medical attention. To wake him up, try shaking him, yelling in his ear, or patting him next to him. If this does not wake him up, confirm cardiac arrest.
Call an ambulance.
As soon as you confirm that there is an emergency, call an ambulance by calling 103 (from a mobile phone) or 03 (from a landline phone). Explain to the operator where you are and what happened. Let him know that you have an AED and that you are going to use it.
Begin resuscitation of the victim.
If you are not alone, begin resuscitating the victim while another person goes to get the AED. If there is no one else nearby, call an ambulance first, and then begin resuscitation.
Part 2
Using an AED
Among the many modern medical devices, the defibrillator is especially commonly used. How it works and what it is is necessary for those people who are planning a surgical operation to implant the device to know.
A defibrillator is a medical device that was created for use in electrical impulse therapy. Often used for various rhythm disorders that are accompanied by too high heart rates. The first experiments with defibrillation were carried out in 1899 on dogs. Their main goal was to study the mechanism of death from electric current, since the very concept of defibrillation was not yet fully formed. This was done by Hooker's team in 1932. As a result of their experiments, the possibility of performing electroshock resuscitation was proven.
The first autonomous defibrillator was created in the Soviet Union in the mid-50s by Klimov and Eskin, but for various reasons it turned out to be impossible to widely popularize the experiments.
The first prototype cardioverter-defibrillator weighed about 27 kg. It was created by Baruch Berkowitz, while the main development of the device is carried out by Zolla Bernard Lown. Using such a device, a pulse with an energy of 100 J was created, which could be used on an open heart. In order for the shock to be used through a closed chest, an average pulse of 300 J was applied.
Video How does a defibrillator work? — Theories in 1 minute | BrainTime
Types of defibrillators and principles of their operation
A defibrillator is a device for transmitting electrical impulses. It can be stationary or portable.
The device consists of three blocks:
- Electricity storage and converter.
- Electrodes, 1 or 2 depending on the type of device.
- Monitor.
The following types are also distinguished:
- A biphasic device that conducts current in one direction.
- Monophasic device. The operating principle of the defibrillator is based on alternating current energy, which moves from one electrode to another and returns back.
Manual defibrillators are difficult to use but low in cost. They are difficult to use, since transportation is impossible due to their size, so such devices can often be found in clinics.
The advantages of automatic defibrillators are the ability to detect rhythm disturbances and the ability to independently select the discharge power for a specific situation.
Working with this type of defibrillator is not difficult; even a beginner can use it. But the cost is quite high, and the choice of additional settings is scarce. There are also universal devices that combine both types.
Depending on the type of defibrillator, the maximum power it can deliver will vary. Typically this is 5000-7000 volts.
What is this method based on?
An electrical discharge of low power but high voltage affects all bioelectric impulses with a non-coinciding vector.
Defibrillation suppresses absolutely all atypical foci of this activity. As a result, only those remain that in the total result of their eigenvectors give one. It is considered correct.
The very essence of the technique is to pass a current discharge with reduced strength directly through the human heart. It is for this reason that it does not cause any damage, but acts exclusively on other electrical impulses. Its high voltage inhibits their work.
After the electrical impulses during defibrillation stop, only normal lesions remain active. Therefore, the functioning of the heart muscle is stabilized.
Important! This example refers to the ideal flow of the procedure. Most often, restoration of normal heart rhythm is achieved only after repeated defibrillations.
Asthmatic conditions
The asthmatic condition is defined as a syndrome characterized by an acute attack of suffocation. Choking is defined as an extreme degree
severity of shortness of breath, accompanied by a painful feeling of lack of air, fear of death.
Etiology. This condition can develop acutely in diseases of the upper respiratory tract (foreign bodies, tumors of the larynx, trachea, bronchi, attack of bronchial asthma) and in diseases of the cardiovascular system (heart defects, AMI, pericarditis).
The pathogenesis is due to obstruction of the respiratory tract and impaired diffusion of oxygen into the blood.
The development of asthmatic conditions in diseases of the cardiovascular system mainly involves swelling of the bronchial mucosa as a result of the accumulation of interstitial fluid in it and compression of the small bronchi by edematous and interstitial tissue.
The following mechanisms take part in the development of bronchial obstruction: spasm of the smooth muscles of the bronchioles, discrinia and hypercrinia, inflammatory swelling of the bronchial mucosa, dyskinesia of the trachea and large bronchi, expiratory collapse of the small bronchi, sclerotic changes in the wall of the bronchi.
Depending on the reasons that caused the asthmatic condition, cardiac asthma, status asthmaticus against the background of bronchial asthma, and a mixed variant are distinguished.
Complications
Both procedures are quite dangerous. But in the case of a defibrillator, we are talking about saving a person’s life. So the risk in this case is justified.
When planning cardioversion, the danger of atrial arrhythmia must be assessed and compared with the risks of the cardioverter. In some cases, with atrial arrhythmia, it is possible to get by with Amiodarone or Propafenone, which are drugs that fight arrhythmia.
Difficulties during the procedure may include:
- Thrombosis of the pulmonary trunk or other vessels . Urgent treatment is necessary, depending on which artery is dug (medicines or surgery);
- Skin burns . It can appear when using high-power electrical charges. Their treatment involves the use of ointments with a concentration of corticosteroids. The ointment is applied immediately after electrical exposure;
- Ventricular fibrillation . In rare cases, erratic contraction of the heart progresses, but is eliminated by the next shock;
- Decline in blood pressure . It may go away on its own, but if blood pressure (BP) is maintained at a low level, medications are used to normalize it;
- Swelling of the lungs . Progression of this complication can occur up to 3 hours after the cardioversion procedure. Most cases occur in patients who previously suffered from atrial arrhythmia. A sharp restoration of the correct heartbeat rhythm can lead to swelling of the lung. In this case, drug therapy is used;
Ventricular fibrillation
Using a defibrillator in childhood
Ventricular tachycardia, pulseless ventricular fibrillation, is rare in children. But if this does happen, then the same life-saving measures are implemented as for adults.
The main difference between defibrillation in children is the choice of electrodes and the device itself, which is based on:
- Size. It is important that the elements cover the desired area of the sternum, but do not touch. If the child's weight is less than 10 kg, then use electrodes for infants.
- Models of the device and the age of the child. An automatic defibrillator should not be used for children under 8 years of age or weighing less than 25 kg, since it does not have the ability to adjust the shock. To correctly select the size of the latter, it is important to know the baby’s body weight. For every 1 kg, the child is given 2 J. If there is no effect, the dose is doubled to 4 J/kg.
Implantable cardioverter defibrillator
The impact of electric current on the heart can be carried out not only from the outside, through the chest, but also from the inside, using an implanted device called a pacemaker (pacemaker). In case of the above-described rhythm disturbances, a cardioverter-defibrillator is inserted into one of the heart chambers, which is capable of “catching” a rapid heartbeat and rebooting the heart thanks to the computer program installed in it. Currently, there is a sufficient variety of pacemaker, and indications for its implantation are determined taking into account the nature of the arrhythmia in a particular patient.
Video: report on the installation of an automatic cardioverter-defibrillator
Clinical picture
• Lightning fast. Death occurs within a few minutes.
• Acute (fast). Death can occur within 10-30 minutes.
• Subacute. Death can occur within several hours or days.
• Chronic. Characterized by progressive right ventricular failure.
• Recurrent.
• Erased.
In the clinical picture, the first place is occupied by suddenly appearing shortness of breath, both at rest and after minor physical exertion. The nature of the shortness of breath is “quiet”, the number of breaths is from 24 to 72 per minute. It may be accompanied by a painful, nonproductive cough. More often, cough complaints appear already at the stage of pulmonary infarction;
at this time, the cough is accompanied by chest pain and the discharge of bloody sputum (hemoptysis is observed in no more than 25-30% of patients). The widespread belief that hemoptysis is an integral sign of the early stage of pulmonary embolism is not always true. EAT. Tareev (1951) noted hemoptysis in 10-12% in the first 3 days, P.M.
Zlochevsky (1978) encountered this syndrome in 19% of patients. It should be emphasized that hemoptysis is more typical for days 6-9 of the disease, and not for days 1-2. Hemoptysis is caused by hemorrhage into the alveoli due to a gradient between low pressure in the pulmonary arteries distal to the embolus and normal pressure in the terminal branches of the bronchial arteries.
Almost immediately, compensatory tachycardia appears, the pulse becomes thread-like, and atrial fibrillation may occur in every fourth patient. There is a rapid drop in blood pressure. Circulatory shock develops in 20-58% of patients and is usually associated with massive pulmonary occlusion, which is considered one of the common signs of pulmonary embolism.
Depending on the location of the thrombus, the pain syndrome may be angina-like, pulmonary-pleural, abdominal or mixed. With embolism of the main trunk of the pulmonary artery, recurrent chest pain occurs due to irritation of the nerve apparatus embedded in the wall of the pulmonary artery.
In some cases of massive PE, sharp pain with widespread irradiation resembles that of a dissecting aortic aneurysm. The duration of pain can vary from a few minutes to several hours. Sometimes anginal pain is observed, accompanied by ECG signs of myocardial ischemia due to a decrease in coronary blood flow due to a decrease in stroke and minute volumes.
An increase in blood pressure in the cavities of the right heart is also of some importance, which disrupts the outflow of blood through the coronary veins. Sharp pain in the right hypochondrium may be observed, combined with intestinal paresis, hiccups, symptoms of peritoneal irritation associated with acute congestive liver swelling with right ventricular failure or the development of massive infarctions of the right lung.
• syncope (like deep fainting) with vomiting, convulsions, bradycardia;
• comatose.
In addition, psychomotor agitation, hemiparesis, polyneuritis, and meningeal symptoms may be observed.
A common symptom of pulmonary embolism is an increase in body temperature, which usually occurs from the first hours of the disease. Most patients have a low-grade fever without chills, while a minority of patients have a febrile temperature. The total duration of the febrile period ranges from 2 to 12 days.
What is it and what is it for?
The meaning of this device can be understood through its name itself: when the heart muscle begins to contract unevenly, arrhythmically, fibrillation occurs. The functionality of this instrument is to bring about the disintegration of this process, that is, defibrillation. The device generates a short pulse and uses electric current to synchronize and equalize the heart rhythm. The patient undergoes shock therapy, receiving 300 J of electricity, but this procedure prevents death.
This method was tested on animals back in 1899, and only in 1947 on humans.
This invention in medicine is really important and necessary, because only through its use it became possible to solve problems with heart rhythm disorders. Subsequently, the question arose about the urgency of its use - in order to avoid consequences for human health, the device must be used as quickly as possible, minutes count. Some patients died in the ambulance - they simply did not have time to deliver them to the device. To solve this problem, a portable defibrillator was invented in 1965, which could be equipped in ambulances. The weight of this equipment reached 70 kg, so there was something to work on - the invention of a lighter and more mobile portable device. Currently, there are various portable devices that allow the doctor to take them with him when visiting the patient; ambulances should be equipped with them. Moreover, there is a bill and there is a question about passing a law that will allow the use of external defibrillators not only by doctors, but also by an “unlimited circle of people.”
We are talking about the need to install these devices in places with large crowds of people: airports, railway and bus stations, metro stations, sports facilities, swimming pools, fitness centers and gyms. This measure can save many human lives when help is needed immediately and the effect of electric current on the heart will prevent death.