Symptoms and signs, frequency of occurrence
The first pronounced symptoms of heart disease appear when the lumen of the aorta is closed by at least half.
The compensatory capabilities of the human heart are so great that until this moment the disease is practically asymptomatic: a person may feel tired, he is often dizzy, but he is unlikely to associate these ailments with heart disease. The patient may experience shortness of breath after physical exertion, and sometimes experience chest pain and palpitations. If the area of the aortic opening increases to 0.75-1.2 cm², then the symptoms become more distinct. These include the following:
- shortness of breath - at first only after physical exertion, and as the disease worsens, even at rest;
- weakness, fainting and presyncope;
- pallor of the skin – the so-called “aortic pallor”;
- muscle weakness;
- slow and barely palpable pulse;
- tachycardia and chest pain that radiates between the shoulder blades, into the arm or shoulder;
- frequent headaches;
- hoarseness of voice;
- swelling of the face and legs;
- dry suffocating cough.
- abdominal pain and ascites (fluid accumulation in the abdominal cavity).
If the stenosis of the aortic opening has reached 0.5 - 0.75 cm2, then this condition is called severe stenosis and is considered critical. Signs of the disease appear even in normal conditions. The person develops heart failure. It appears as follows:
- Swelling of the lower extremities is pronounced, spreading to the legs, thighs and feet.
- Sometimes swelling spreads to the abdomen and the entire body of a person.
- Shortness of breath is accompanied by attacks of suffocation.
- The skin color becomes marbled and even bluish, this is especially noticeable on the face and fingers (acrocyanosis).
Hemodynamic angina pectoris is manifested by constant pain in the heart. The overall incidence ranges from 2 to 7% of cases.
In newborns
Stenosis in infants is congenital. It appears as follows:
- the baby becomes lethargic;
- has difficulty taking the breast;
- the skin on the face, hands and feet becomes bluish.
Pathology is observed in 8% of cases, and much more often in boys. The task of parents is to identify such violations as early as possible and seek medical help. If a heart murmur is observed during listening, additional diagnosis of the disease will be required.
In children and adolescents
Often in childhood, pathology develops due to hereditary predisposition. The disease begins to actively manifest itself between the ages of 11 and 15 years. The disease can be suspected by shortness of breath, increased heartbeat and pain in the chest area.
In old people
In old age, the disease worries many people; according to statistics, up to 20% of old people. The symptoms are the same as in patients of other ages. Due to the deterioration of the body at this age, fainting is not uncommon. This circumstance alone should prompt an elderly person to see a doctor. Occurs
Considering that the first characteristic symptoms of aortic stenosis appear quite late, when the disease has long passed its initial stage, contacting a cardiologist should be immediate if they are detected.
Symptoms
Depending on the stage of the disease, clinical manifestations may vary. In the first stages of development of the pathology, symptoms are invisible and often absent altogether.
With a slight narrowing of the artery there will be practically no manifestations. The disease can be discovered by chance after a few years during a routine examination by a cardiologist or pediatrician.
Newborns with stenosis experience congestive heart failure and shortness of breath even at rest. If the gap is 1 mm, urgent surgery is required. Otherwise, death may occur.
The first signs of pulmonary artery stenosis are:
- shortness of breath even with minor physical exertion,
- increased fatigue,
- heart murmur
- general weakness,
- frequent dizziness,
- fainting,
- pain in the heart area,
- swelling and pulsation of the neck veins.
Upon examination, a cardiac hump may be detected. Symptoms tend to get significantly worse with physical activity. Therefore, sports and physical education are contraindicated for children with this diagnosis.
If during a routine examination by a pediatrician your baby is diagnosed with a heart murmur, do not panic. Only a cardiologist can make an accurate diagnosis based on research results.
Diagnosis of pulmonary artery stenosis
To diagnose the disease, you must do the following:
- FCG (phonocardiography) to study the presence and type of heart murmur;
- ECG (echocardiography), which allows to detect right ventricular hypertrophy;
- X-ray, which shows an increase in the size of the heart.
Analyzes of the obtained data make it possible to make an accurate diagnosis and determine the degree of stenosis. Only after this is treatment prescribed.
If you are in doubt about the correct diagnosis, consult several cardiology specialists.
Pulmonary artery stenosis can manifest itself in a varied clinical picture, which depends on the stage of the disease.
With minor degrees of narrowing, signs of pathology are not observed.
In children
The clinical picture of the disease in childhood is characterized by:
- pallor of the skin or acrocyanosis - blueness of the cheeks, lips, fingertips, shortness of breath, frequent pneumonia, tendency to colds;
- child's retardation in physical development;
- fast fatiguability;
- pathological murmurs when listening to the heart;
- fainting.
In adults
The most common signs of narrowing of the lumen of blood vessels in the lungs in older people are:
- frequent dizziness;
- difficulty breathing;
- general weakness;
- hemodynamic disturbance;
- the presence of systolic tremor during auscultation;
- squeezing pain in the left side of the chest;
- swelling of the lower extremities;
- ascites;
- anasarca.
Treatment
Patients are under constant medical supervision in the hospital. At the same time, specialists carry out rehabilitation of foci of chronic inflammation, if any. Everything is also done to prevent infective endocarditis. If necessary, antibacterial therapy is carried out as prophylaxis. But this is a concomitant treatment. The main method of treatment is surgery.
There is no need to be afraid of the operation. Today, surgeons use techniques that are completely safe for both newborns and adults. In addition, surgical treatment techniques are constantly being improved.
As a rule, doctors recommend surgery at stages 2 and 3 of the disease. At stage 1, the patient is constantly monitored by specialists, but no preparation for surgery is carried out.
Today, doctors most often resort to closed and open operations.
Open pulmonary valvuloplasty is performed as follows:
- Surgeons open the patient's chest to gain access to the artery.
- The patient is transferred to artificial blood circulation.
- The pulmonary artery is dissected. Through the incision, doctors examine the fused valves.
- Surgeons cut the valves in a certain way, thereby returning them to the necessary functionality.
Closed operations are also performed using artificial circulation. Surgeons reach the heart in the fourth intercostal space and enter the right ventricle in the avascular zone. After this, a valvulot is inserted into its cavity, which is then passed into the artery. With its help, the fused membrane is dissected and expanded to the desired size using a dilator.
By the way, these methods are used less and less today. Most clinics are switching to less traumatic operations. For example, the intervention method. It consists of using special catheters with balloons. The latter are introduced into the lumen of the fused valve and inflated until the stenosis is eliminated. If necessary, the procedure is repeated several times. This pathology technique is considered very effective.
Types of disease
In this case, the disease can occur in several degrees of severity. It can be mild, moderate or severe stenosis.
Much also depends on the level of systolic pressure and the gradient between the artery and the right ventricle. In moderate stenosis, the pressure will be about 60 mmHg.
Art., at the second stage this figure already reaches 100 units, and with a pronounced disease, blood pressure is even higher with a gradient of more than 80. There is also a 4th degree of the disease.
We are talking about the decompensatory stage, in which myocardial degeneration and a sharp drop in pressure in the ventricle are not excluded.
The most common congenital heart defect is isolated stenosis, the share of which among such diseases is up to 12 percent of the total. Valve-type vasoconstriction is more common (up to 90 percent of cases) than combined forms of the disease, which combine subvalvular and supravalvular stenosis, and some other types of heart disease.
”alt=””>
In almost 90% of cases of this disease, stenosis is diagnosed as valvular. The remaining 10% consists of the subvalvular and supravalvular types.
Valvular stenosis is characterized by the absence of division of the valve itself into certain leaflets and its acquisition of the shape of a diaphragm in the form of a dome with an opening of up to 10 mm. Subvalvular stenosis is accompanied by an abnormal proliferation of both fibrous tissue and muscle with a funnel shape that narrows towards the outflow tract in the right ventricle.
Supravalvular stenosis is characterized by local narrowing, the presence of several peripheral stenoses, etc.
In this case, there is fusion of the valve flaps and a small hole in the middle. Supravalvular stenosis is characterized by numerous decreases in the circumference of the artery, a complete or incomplete membrane (thin plate), and congenital underdevelopment.
Funnel-shaped narrowing of the vessel in the outflow tract of the right ventricle is characteristic of subvalvular stenosis. The unnatural increase in fibrous and muscle tissue significantly complicates the release of blood into the pulmonary circulation.
Specifics of the disease and reasons for its development
Stenosis is a pathological decrease in the diameter of a vessel transporting blood. The pulmonary highway is the only one in the human body through which venous blood circulates. Anatomically, it is designed in such a way that blood flows to the lungs through a large vessel from the right ventricle of the heart through the tricuspid valve. As a result of the narrowing of the vessel, biological fluid from the right ventricle of the heart cannot properly flow to the lungs. This pathology forces the heart to function with “increased” performance in order to maintain the body, thereby causing significant harm to itself. The right ventricle of the heart is stretched and deformed due to intense work, and the so-called “heart hump” is formed.
Medicine tends to classify pulmonary stenosis as a congenital heart pathology, however, there are often precedents for the development of the disease in mature people. The root causes of thinning of the pulmonary branches in babies are considered to be a genetic factor, as well as the presence of health problems in the mother during pregnancy. Most often, pulmonary artery stenosis in newborns is provoked by the following precedents that occur during the baby’s uterine development:
- Failures of embryonic evolution due to taking medications that have a negative effect on the fetus. These can be psychoactive, narcotic or antibacterial drugs that critically affect the embryo in the first trimester of its formation.
- Presence of the disease in the genealogical history.
- Infectious diseases of the mother of the viral category during pregnancy. These include smallpox, rubella, complex herpes, mononucleosis, and active hepatitis.
- Factors of the environmental category: unfavorable working conditions for the expectant mother, mainly in toxic enterprises, excess radioactive background in the area of her residence.
- Alcohol abuse by the mother while pregnant.
- Consumption of genetically modified products in excessive quantities.
In adults, the disease is diagnosed much less frequently; the following indicators may be the reasons for the evolution of the pathology:
- inflammatory processes in the inner layer of the heart, which over time spread to the pulmonary vessels;
- calcification of the heart valve leaflets;
- tumor formations in cardiac tissues;
- rheumatism, which causes deformation of the heart valves;
- enlargement of lymph nodes or protrusion of the aorta.
Medicine distinguishes several modifications of stenosis depending on its location and the degree of thinning of the artery. The treatment methodology and prognosis for the patient’s recovery vary from these criteria.
Prevention of the disease and prognosis for recovery
Preventive measures to prevent the genesis of stenosis in yourself or your unborn child in most cases come down to the trivial rules of a correct lifestyle, rational nutrition, and giving up addictions. In addition, timely visits to doctors in order to eliminate the possibility of contracting infectious diseases and their poor-quality treatment is considered an excellent preventive measure. Modern medicine takes all possible measures to prevent the birth of a child with pathology of the pulmonary ducts. If there are genetic prerequisites in the family for the birth of a baby with stenosis, doctors recommend that the expectant mother, before planning a pregnancy, undergo a full examination of the body, preventive therapy, and eliminate negative factors that accompany the progression of the disease.
If it so happens that it was not possible to avoid the disease, and the diagnosis of “pulmonary artery stenosis” is a real verdict, you should not lose hope. Medicine allows you to effectively get rid of a disease if it is detected in a timely manner and medical care is provided to the patient.
The prognosis for recovery and the possibility of a full life in most cases depend on the efficiency of the operation performed to eliminate the pathology. When born with a mild stage of the disease, the baby does not require surgery, however, he is under the close supervision of pediatricians and cardiologists. The average life expectancy of such children is no different from the life expectancy of ordinary people. Such children develop according to age, however, they may be more susceptible to viral diseases. In older age, people with congenital minor stenosis are not recommended for severe physical strain and intense sports.
If a child is born with a severe pathology, then the baby will need surgery, the timing of which is determined by specialists. In most congenital precedents, surgery is prescribed in the first months or years of a young patient’s life. If parents refuse surgical intervention for any reason, the prognosis is disappointing; the disease can develop quickly and take the child’s life within five years.
Surgical intervention in operable stages offers excellent prospects for quality and life expectancy.
Catheter balloon valvuloplasty
If it is impossible to perform endovascular replacement in a child with aortic valve stenosis, the doctor recommends plastic surgery. The operation is performed on young children and very rarely on adults. As a result of surgical treatment, hemodynamic parameters improve, and the patient's condition stabilizes.
Transcatheter aortic valve implantation is performed in cardiac surgery centers. The indication for surgery is the severe condition of the child and a short life prognosis - up to 1 year. Some newborns have severe comorbidities and are therefore contraindicated for open heart surgery. Surgery is not performed for patients suffering from infective endocarditis, with an increased risk of blood clot formation and lung diseases. Before the operation begins, the doctor evaluates all risk factors. At the stage of diagnosis, the patient is prescribed the following procedures:
- coronagraphy;
- computed tomography;
- cardiac probing.
The following conditions are contraindications to the operation:
- combined damage to the aortic and tricuspid valves;
- severe mitral insufficiency;
- defects in the valve structure.
The operation is performed under general or local anesthesia for 1-2 hours. Complications may occur after surgery:
- allergic reaction;
- renal failure;
- bleeding at the puncture site;
- temperature;
- arrhythmia;
- air embolism.
After the operation, the child is monitored by a cardiologist. After 6-12 weeks, the patient is prescribed the following studies: echocardiography, electrocardiogram, biochemical blood test.
The child is given antibacterial therapy with penicillin drugs.
Aortic stenosis is a heart disease in which the patient experiences stenosis (narrowing) of the aortic opening or deformation of the heart valve leaflets. Blood from the left ventricle “passes” worse and normal blood flow through the systemic circulation, and accordingly, to all organs, is not ensured.
The left ventricle begins to work harder, which compensates for poor valve patency and less blood flow. That is why a person may not immediately feel the symptoms of the onset of the disease. Over time, due to the increased number of contractions, the walls of the ventricle become thicker, and the muscle itself weakens. The result is heart failure.
Aortic stenosis is most often observed in adults; it can occur with age due to the accumulation of salts in the heart valve area, but sometimes it also occurs in children.
Another type of heart defect is a bicuspid aortic valve (a healthy person has three valves). For children, such a deviation from the norm most often does not cause any harm, but in an adult, stenosis may occur. In this case, surgery to replace the valve will be necessary.
What is stenosis and why is it dangerous?
Pulmonary artery stenosis is a narrowing of the vessel, which can have varying degrees of severity and localization. Based on the degree of severity, they distinguish between mild, moderate and severe arterial damage.
Based on location, stenosis is divided into:
- Valvular - narrowing occurs in the area of the arterial valve. In this case, the valve itself can be single-leaf, tricuspid or bi-leaf. Behind the stenotic area there is usually a zone of vessel dilatation. Valvular pulmonary artery stenosis accounts for about 90% of the total number of cases of the disease.
- Subvalvular - narrowing of the blood drainage line under the arterial valve and the formation of a muscle bundle that prevents the ejection of blood from the heart.
- Supravalvular - isolated pulmonary artery stenosis, occurring in the supravalvular type, can have several morphological forms.
- Pulmonary artery stenosis is a narrowing of the passage directly between the ventricle and the trunk of the pulmonary artery.
The presence of narrowings reduces the capacity of the artery, which leads to its incomplete performance of its function. At the same time, the right ventricle of the heart works under high load, stretches, hypertrophies, and its insufficiency develops. Increased pressure inside this chamber of the heart causes the oval window to open and dump excess blood into the left half of the organ. In this case, the patient develops clinical signs of heart disease.
Note: a mild degree of valve stenosis practically does not lead to the appearance of symptoms of the disease, so the disease may not be detected in a timely manner. The development of such newborns proceeds without deviations . They grow normally, mature and lead full lives. The life expectancy of patients is practically no different from people who do not suffer from cardiac pathology.
Diagnostics
In addition to examination data, auxiliary methods are important in diagnosis.
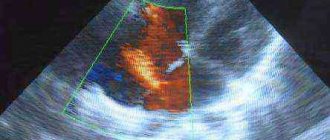
Echocardiography in two-dimensional mode determines the thickening of the valve leaflets with a dome-shaped deflection towards the vessel during systolic contraction of the right ventricle, and an increase in the thickness of the walls.
A Doppler study uses the difference in pressure in the pulmonary trunk and the right ventricle to determine the degree and levels of narrowing. This indicator is called the pressure gradient. It distinguishes 3 degrees of narrowing:
- mild - gradient up to 50 mm Hg. Art.;
- medium - from 50 to 80;
- severe - above 80 mm Hg. Art.;
- extremely pronounced - 150 and above.
The arrows on the radiograph show the dilated pulmonary artery arch and the left atrium
X-ray examination shows an increase in the right border of the cardiac shadow, a bulging of the arch in the area of the projection of the pulmonary artery, with a significantly depleted pulmonary pattern, bright fields are visible. This is explained by the low filling of the vascular bed.
To make a diagnosis, a specialist must take the following steps:
- Identification of complaints in order to recognize dangerous symptoms.
- Examination of the patient, which may reveal: pallor of the skin, cyanosis of the whole body or limbs, pulsation, swelling of the veins in the neck, systolic trembling in the chest, cyanosis of the body or limbs, development of a cardiac hump.
- Biochemical and general analysis of blood and urine;
- ECG (EOS deviation to the right, symptoms of right ventricular overload);
- Ultrasound of the heart;
- X-ray examination (characterized by an increase in the boundaries of the heart in the presence of disease, deterioration of the pulmonary pattern, post-stenotic expansion of the pulmonary artery trunk);
- Echocardiography (poststenotic dilatation of the pulmonary artery, dilatation of the right ventricle);
- Phonocardiography (presence and splitting of the weakening of II tone over the pulmonary artery, rough systolic murmur);
- Sounding (performed on the right side of the heart to establish the pressure in the right ventricle and the pressure gradient).
By percussion, the borders of the heart are shifted to the right; upon palpation, the systolic pulsation of the right ventricle is determined. Auscultation and phonocardiography data are characterized by the presence of a rough systolic murmur, weakening of the second sound over the pulmonary artery and its splitting.
X-ray allows you to see the expansion of the borders of the heart, post-stenotic expansion of the pulmonary artery trunk, and depletion of the pulmonary pattern.
An ECG with stenosis of the pulmonary artery mouth reveals signs of overload of the right ventricle, deviation of the EOS to the right. Using echocardiography, dilatation of the right ventricle and post-stenotic dilation of the pulmonary artery are detected; Dopplerography allows one to identify and determine the pressure difference between the right ventricle and the pulmonary trunk.
By probing the right parts of the heart, the pressure in the right ventricle and the pressure gradient between it and the pulmonary artery are established. Ventriculography data are characterized by an increase in the cavity of the right ventricle and a characteristic slowdown in the disappearance of contrast from the right ventricle.
Selective coronary angiography is indicated for patients over 40 years of age and those complaining of chest pain.
Diagnosis of pulmonary artery stenosis includes a combination of various instrumental studies and physical data.
- In the second intercostal space, to the left of the sternum, a rough systolic murmur is heard. It is carried out towards the collarbone and is perfectly audible in the interscapular region. The second tone in the first and second stages of the disease is heard practically unchanged, but with severe stenosis it can disappear completely.
- With minor stenosis, the electrocardiogram does not show any abnormalities. At all other stages of the disease, signs of hypertrophy of the right ventricle of the heart muscle are observed. Supraventricular arrhythmias may occur.
- Echocardiography shows dilatation of the right ventricle of the heart muscle and poststenotic dilatation of the pulmonary artery. Doppler sonography allows you to identify and determine the pressure difference between the pulmonary trunk and the right ventricle.
- X-ray studies show depletion of the pulmonary pattern and post-stenotic expansion of the pulmonary artery trunk.
Next, we will tell you about the features of treatment of pulmonary artery stenosis in children.
Causes
Based on the level of circulatory disturbance, doctors divide the defect into four types:
- Subvalvular type of stenosis, 5% of the total. With it, funnel-shaped changes in the outflow structures of the right ventricle are observed due to abnormal proliferation of muscle and fibrous fibers.
- Supravalvular stenosis is observed in 5-10% of patients. This is underdevelopment or damage to the walls of the artery.
- Valvular form of stenosis. It develops in 85% of cases. This is a condition in which the valve leaflets thicken, become deformed and obstruct the flow of blood.
- Combined forms. It is characterized by a combination of two or more types of stenosis with the development of severe clinical symptoms.
For practicality, a classification is used that is based on the pressure gradient between the artery and the cavity of the right ventricle, as well as systolic blood pressure in it:
- The first stage of stenosis is moderate narrowing. At the same time, the indicators of the pressure gradient and systolic pressure level are in the range of 20-30 mmHg. Art. and 60 mm Hg. Art. respectively.
- The second stage of the pathology is severe stenosis of the artery lumen. The gradient level is 30-80 mm Hg. Art., and the systolic pressure indicator is 60-100 mm Hg. Art.
- The third stage of the disease is severe stenosis. The pressure gradient level is more than 80 mmHg. Art., and the systolic pressure is more than 100 mm Hg. Art.
- At the fourth stage of the disease, decompensation processes develop. In this case, there is a decrease in the gradient and level of systolic pressure as a result of the development of a contractile type of failure.
Congenital defect
https://www.youtube.com/watch?v=zcHkjUEXZqk
Among the etiological factors of congenital heart disease in newborns, doctors identify:
- unfavorable living and working conditions of a woman during pregnancy, affecting the health of the fetus;
- the presence of a genetic predisposition to various defects of the structures of the cardiovascular system in the fetus;
- consumption by the expectant mother of alcoholic beverages, psychoactive and narcotic substances, antibacterial drugs;
- diseases of viral etiology in a pregnant woman, among which rubella and infectious mononucleosis are considered the most dangerous;
- exposure to X-rays and other types of ionizing radiation during pregnancy.
Acquired vice
The main factors in the development of the acquired form of the disease are:
- atherosclerotic lesions of the walls of the coronary arteries;
- rheumatic damage to the heart valves;
- the presence of calcific changes in the area of the pulmonary valves and aorta;
- hypertrophic cardiomyopathy;
- compression of the artery with enlarged lymph nodes, the presence of malignant neoplasms and aneurysms;
- foci of inflammation in the vascular walls, which are caused by pathogens of tuberculosis infection and syphilis.
The main factors influencing the development of congenital stenosis are:
- intoxication of the mother's body during pregnancy,
- transferred rubella,
- heredity.
The causes of acquired pathology can be:
- infectious endocarditis,
- myxoma of the heart,
- formation of carcinoids,
- aortic aneurysm,
- ventricular hypertrophy,
- enlarged lymph nodes.
According to localization, pulmonary artery stenosis can differ in:
- valve,
- subvalvular,
- mixed.
The disease has four stages:
- moderate,
- expressed
- pronounced,
- stage of decompensation, which is characterized by serious disruption of blood circulation.
Diagnosis of the disease
Diagnosis of narrowing of the pulmonary artery is quite difficult. To make an accurate diagnosis, doctors have to conduct a large number of different studies:
- Auscultation of the heart. As a rule, if the narrowing of the vessel is severe, then during normal listening with a phonendoscope, noise behind the sternum in the second intercostal space can be clearly heard. Also, a heart murmur can be easily heard from the back between the shoulder blades.
- If the disease is at the 1st or 2nd stage of development, then the tonality of the noise does not change. However, if it moves to the 3rd stage, then the tonality of the noise changes. They become smoother and sometimes disappear completely.
- An ECG is required. Peaks are clearly visible on the tape, indicating an enlargement of the right ventricle due to excess load. Also, an electrocardiogram can detect supraventricular arrhythmia, which very often accompanies narrowing of the pulmonary artery.
- If necessary, doctors can perform Doppler ultrasound. It allows you to identify the difference in pressure between the right ventricle and the pulmonary trunk.
- All patients without exception undergo echocardiography. With its help, the inevitable dilation of the vessel is detected.
- A chest x-ray with contrast agent is performed. As a rule, with its help, doctors identify a simplification of the vascular pattern in the lungs and an expansion of the artery trunk.
Life forecast
The prognosis for pulmonary artery stenosis in children and adults, if all the instructions of the attending physician are followed, is favorable. The minimum risk of complications is observed in situations where surgical treatment was performed in childhood. But the lack of timely treatment is very dangerous; serious consequences and the likelihood of death increase by 4-5 times.
The average life expectancy with narrowing of the mouth of the pulmonary trunk depends on the characteristics of the development and course of pathological processes. On average it is 30-40 years. If the attending physician's instructions are not followed, the patient does not live more than 5 years.
With minimal congenital forms of stenosis, the patient’s quality of life and life expectancy do not decrease. Such patients are observed by a cardiologist and in most cases do not have a disability group. After surgical manipulations using stents, the average life expectancy of patients in 91% of cases is more than 5 years.
Author of the article:
Dmitrieva Yulia (Sych)
– In 2014, she graduated with honors from Saratov State Medical University named after V.I. Razumovsky. Currently working as a cardiologist at the 8th City Clinical Hospital in the 1st clinic.
Pulmonary artery stenosis is a heart defect of congenital or acquired etiology, as a result of which the patient experiences a narrowing of the lumen of the pulmonary trunk, which is a factor in the development of circulatory disorders.
To understand the danger of pathology, you need to have an idea of its causes, clinical picture, diagnostic methods, as well as treatment and prognosis of the disease.
Diagnostics
Pulmonary artery stenosis (PAS) is a pathological condition that changes the size of the pulmonary trunk, causing it to become narrower, which interferes with normal blood flow. This disease is one of the types of heart defects.
During narrowing, there is a weak exit of blood from the right ventricle, due to the fact that the lumen of the pulmonary artery becomes smaller. Therefore, a malfunction of the small circle of blood circulation occurs.
Diagnosis of the disease occurs in children from an early age. In most cases, stenosis is observed in combination with various changes.
According to various statistics, per one thousand registered heart defects, there is from 3 to 12 percent narrowing of the pulmonary trunk.
The main classification of stenosis occurs according to the location of the narrowing, which can form in the following places:
- Valve. The decrease in the lumen of the pulmonary artery occurs directly in the heart valve. This type of pulmonary artery stenosis is mainly recorded;
- Undermined. The artery narrows below the valve;
- Supravalvular. There is a decrease in the passage of the artery higher up the trunk, above the valve;
- Combined. If the artery narrows in several places.
Forms of pulmonary artery stenosis
In ninety percent of cases of pulmonary artery stenosis, valvular stenosis is diagnosed.
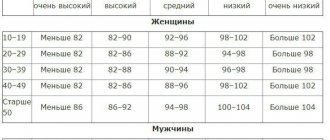
The division also occurs according to the degree of overlap of the lumen:
- Mild degree;
- Average degree;
- Severe degree.
In practice, qualified doctors successfully use division, which is based on the level of detection of systolic blood pressure (blood pressure) in the right ventricle, and the pressure ratio between the right ventricle and the pulmonary trunk.
The levels of this pressure are divided into degrees:
- 1st degree. Blood pressure in systole – 60 mmHg, ratio – 20-30 mmHg;
- 2nd degree. Blood pressure in systoles ranges from 60 to 100 mmHg, and the ratio is 30-80 mmHg;
- 3rd degree. The pressure in this case is more than 100 mmHg, and the ratio is more than 80;
- 4th degree. It is a decompensatory stage. Ventricular failure progresses due to its weak contractions, dystrophy of the heart muscle occurs, and the pressure in the ventricle decreases.
Pulmonary stenosis
Throughout life, the decrease in the lumen of the pulmonary artery progresses quite rarely. In the vast majority of cases, it is a congenital disease, and is in second place in terms of prevalence among all congenital heart defects.
Factors influencing pulmonary stenosis include those that, during pregnancy, can affect the formation of the vascular system and lead to congenital heart defects.
These include:
- Taking psychoactive substances, narcotic drugs, antibiotics by women bearing a child, mainly in the first trimester of pregnancy;
- Unsuitable working conditions during pregnancy. When carrying a child, work at paint and varnish, chemical, industrial enterprises, and other structures in which the expectant mother can inhale chemical and toxic fumes is contraindicated;
- Genetic disposition. In this case, arterial stenosis is transmitted primarily from mother (or father) to child;
- Diseases of viral origin during pregnancy. Congenital pulmonary stenosis can be affected by: rubella, herpes, mononucleosis and other viral diseases;
- Ionizing radiation, including X-rays, when carrying a child;
- Environmental factors. Unfavorable environment, mostly manifested in high concentrations of radiation in certain regions of the country.
As the narrowing of the pulmonary artery progresses throughout life, the most common causes may be the following:
- A disease of the rheumatism group. They affect the pulmonary valves, causing stenosis;
- Inflammatory processes of the walls inside the pulmonary artery. They are registered in rare cases, but damage to syphilis, tuberculosis, etc. should not be excluded from the list;
- Deposition of atherosclerotic plaques. Cholesterol plaques can also be deposited on the walls of the pulmonary artery, causing it to narrow;
- Pressure on the artery of the lung from the outside. In most cases, the reasons for this are tumor formations, enlarged lymph nodes, and saccular protrusion of the aorta;
- Calcification. Deposits of calcium salts on the walls and valve of the pulmonary artery. The walls of the artery become irritated, leading to narrowing.
Valve for congenital stenosis
Detection of symptoms directly depends on the magnitude of the narrowing of patency in the pulmonary artery. At a mild stage, stenosis may not appear for a long time. Mostly in children under one year of age.
https://www.youtube.com/watch?v=LR6WL7cuBZs
Manifestations of symptoms in more severe forms of stenosis make themselves felt almost from birth.
They manifest themselves in the following signs:
- Clearly expressed cyanosis, which manifests itself in blue shades of the skin on the tips of the fingers and toes, the area between the nose and lip, or in the bluish color of the skin throughout the body;
- Hard breath;
- Possible loss of consciousness;
- Weak weight gain;
- Lethargy and obvious anxiety of the baby.
In the adult age category, the manifestation of symptoms occurs somewhat differently. They may not signal for many years, or throughout their lives.
Obvious symptoms of pulmonary artery stenosis in more severe stages include:
- Rapid fatigue after minor physical exertion, progressing to constant fatigue;
- Dizziness and loss of consciousness;
- On auscultation of the heart, muffled tones and rough systolic murmur are heard in the left side of the chest and in the third intercostal space;
- Heavy breathing during physical activity or at rest, which becomes stronger when lying down;
- The fingers have a flat “drumstick” appearance;
- The veins of the cervical region pulsate;
- Swelling of the legs, and with the progression of heart pathologies and swelling of the whole body.
Severe stenosis
The formation of pulmonary artery stenosis can occur both due to acquired causes and congenital.
During its formation, the following processes occur in the heart:
- When the artery narrows, it becomes more difficult for the right ventricle to push out blood, and a greater load is created on it;
- As a result, less blood is delivered to the lungs. Hypoxia of internal organs occurs, causing insufficient oxygen saturation of the blood;
- The heart muscle wears out over time when heavy loads are regularly placed on the right ventricle. This leads to its failure, provoked by an increase in the mass of the heart muscle;
- Due to the fact that the amount of blood that is not completely ejected into the artery of the lung regularly increases, a reverse release of incoming blood occurs into the right atrium, which leads to a disruption in blood circulation, as well as processes of stagnation and oxidation of the blood. More severe oxygen starvation occurs;
- Clearly manifested stenosis leads to the progression of heart failure. If timely surgery is not performed, the most common outcome is death.
Which doctor treats you?
At birth in a maternity hospital, absolutely all newborn children undergo an examination by a neonatologist, who determines the presence of diseases and pathological conditions in the baby. If abnormalities are detected, he draws up a plan for further examination.
If you experience symptoms of pulmonary stenosis during adolescence, you should consult a qualified pediatrician.
When signs of pulmonary artery stenosis appear in an older age group, you need to consult a therapist or cardiologist.
Endovascular balloon valvuloplasty
Treatment
Treatment of pulmonary artery pathology in a newborn is only surgical. In severe forms of the disease, surgery can be performed in the first days, and sometimes even hours, of the child’s life. This only happens when delay can lead to the death of the baby. Planned interventions are postponed to a later age. To correct the condition of the pulmonary artery, the child is hospitalized at the age of 3-4 years.
The surgical procedure may vary depending on the capabilities of the clinic and the qualifications of the surgeon. 15-20 years ago, the most common method was the open method of manipulation, in which the cardiac surgeon had to work on an open heart. This method was dangerous and had high mortality rates.
Today, the preferred surgical technique is balloon valvuloplasty. When performing it, a wide incision of the chest is not performed. An inflatable balloon is passed through the main blood vessel to the affected area, which is fixed in the area of narrowing and inflated. The balloon expands the stenotic area, ensuring normal blood flow in the pulmonary artery and the lungs themselves.
Drug and surgical treatment
For minor stenosis, drug therapy is prescribed.
| Group | Drugs |
| Potassium-containing products | Asparkam, Orocamag, Potassium orotate, Panangin |
| Vitamin complexes | Vitamins A, B, C, P |
| Cardiac glycosides | Digoxin, Korglykon, Celanide, Strophanthin |
Medicines are prescribed to maintain the functioning of the heart and large vessels. A radical way to treat stenosis is to perform surgery.
The purpose of the procedure is to normalize blood flow in the right side of the heart. The type of procedure is determined taking into account the localization of pathological foci.
Among them:
- Balloon valvuloplasty. It is effectively used when the patient has valvular venous stenosis. To carry it out, a special balloon is inserted into the mouth of the affected vessel. After this, a stent is installed in it, with the help of which the narrowing is eliminated.
- In the case of narrowing of the supravalvular localization, the most effective is resection of part of the vascular walls that have undergone stenosis. Instead, patches taken from the patient's pericardium are applied.
- The essence of surgical therapy for subvalvular stenoses is to eliminate areas of cardiac muscle hypertrophy in the area of the right atrium.
- To treat a combined type of disease, a combination of the above methods is used.
After the narrowing is eliminated surgically, blood circulation in the area of the mouth of the pulmonary trunk is normalized over time. Symptoms of the pathology gradually decrease, the patient’s general condition stabilizes.
Isolated pulmonary artery stenosis in adults and children is treated in the following ways:
- conservative. They are used for minor pathologies that cannot cause serious disturbances in the functioning of the cardiovascular system. Also used when the patient's parents refuse treatment with surgery. They help relieve complications from myocardial ischemia (low oxygen supply to the heart muscle) as well as heart failure (the heart's inability to fully perform its duties of transporting and pumping blood). This method is also used in preparation for surgery;
- operational. Includes surgical intervention. Pulmonary artery stenosis is eliminated by dilating a narrow section in the vessel (an effective treatment method). The time frame within which the operation must be performed is set for each patient separately. The operation can be performed while the baby is in the womb. In this case, the uterine walls are cut, and the fetus is operated on. The sooner treatment is provided, the better for the child’s health.
After examining the patient's heart, the doctor makes a diagnosis and creates a treatment plan for the stenosis. If a mild form of pathology is detected, it is recommended to take cardiac glycosides, vitamins, and potassium supplements. This will help keep your heart functioning normally.
At an advanced stage, when a person is bothered by severe symptoms of pathology, surgical intervention is required. This is the only way to get rid of pulmonary artery stenosis and restore blood circulation to the heart.
There are several surgical methods used to treat pulmonary stenosis. For each patient, a different technique is selected that will help in a particular case. Sometimes the valve is removed, replaced with a prosthesis, or a commissurotomy is performed. It is possible to install a stent to widen the artery walls.
After the operation, blood circulation is normalized, venous blood is no longer thrown into the left ventricle. The lung tissues begin to actively feed on oxygen, as a result of which the clinical manifestations disappear. The rehabilitation period takes quite a long time, about 3 months.
If the patient has a large left-to-right shunt, such as a patent ductus arteriosus or ventricular septal defect, and is in respiratory distress, diuresis is effective in reducing cyanosis secondary to pulmonary edema.
Oxygen should be given to any patient with cyanosis due to respiratory failure. The use of oxygen can reduce pulmonary artery pressure in patients with a reactive pulmonary vasculature, thereby increasing pulmonary blood flow.
Treatment depends on the degree of stenosis. Thus, clinical assessment as well as imaging will be the immediate guide. Cardiology or cardiothoracic consultation is necessary if imaging studies show right outflow tract obstruction.
Please note the following:
Severe stenosis, peak gradient 60 mm Hg. Art. and more, requires emergency dilatation of the valves with balloon valvotomy.
Patients with mild pulmonary valve stenosis usually do not require treatment.
Patients with severe or symptomatic infundibular or supravalvular pulmonary stenosis require immediate intervention. Valvotomy is the standard of care in these patients.
Often cyanotic children with respiratory distress and hypotension/shock are evaluated in the same way as patients with sepsis.
The second Natural History Study of Congenital Heart Disease examined 592 patients with pulmonary valve stenosis over 10,688 person-years; only one patient had an episode of bacterial endocarditis.
Endocarditis prophylaxis is recommended for 6 months after repair of congenital heart disease. Additionally, prevention is required for life for people who have prosthetic valves.
Intervention with balloon angioplasty or valve repair is indicated for patients with peak valve gradients greater than 50 mmHg. Art. or patients with angina, syncope, dyspnea on exertion, or presyncope. Corrective options include open heart surgery, balloon angioplasty, percutaneous stenting, percutaneous valve replacement, or percutaneous conduit placement.
Patients with severe or symptomatic infundibular or supravalvular pulmonary stenosis require surgical intervention.
Critical pulmonary valve stenosis may present with near pulmonary atresia (cyanotic lesions) with a small and often inadequate right ventricle. These patients survive because of a patent ductus arteriosus. Pulmonary valve atresia or critical pulmonary valve stenosis with an inadequate right ventricle requires a shunt after the duct is patented pharmacologically with prostaglandin E1.
Definitive repair may not be possible if the right ventricle is hypoplastic, requiring a single ventricular palliation such as the Fontan procedure or a variation such as a direct right atrial appendage to the main pulmonary artery anastomosis. Often the main and branch pulmonary arteries need to be enlarged.
Main stages of pathology
There are four stages of pulmonary artery stenosis:
- moderate stenosis - stage I. The patient has no complaints, the ECG shows a slight overload of the right ventricle of the heart muscle. Systolic pressure up to sixty millimeters of mercury;
- severe stenosis - stage II. Characterized by obvious symptoms. The systolic pressure of the heart muscle in the right ventricle is from sixty to one hundred millimeters of mercury;
- severe stenosis - stage III. Severe stage of the disease, signs of circulatory disorders appear, pressure on the pulmonary valve and right ventricle is above one hundred millimeters of mercury;
- decompensation - stage IV. Clear signs of myocardial dystrophy, very severe disruption of blood flow. Contractile failure of the right ventricle develops, so systolic pressure may be low.
Based on the level of blood flow, valvular (the most common), subvalvular and supravalvular pulmonary artery stenosis in a newborn can be distinguished. A combined form of the disease is also very rare.
- With valvular stenosis, the valve leaflets fuse together, and it has a dome-shaped shape with a hole in the middle.
- The subvalvular degree of the disease looks like a funnel-shaped narrowing of the outflow tract of the right ventricle as a result of abnormal proliferation of fibrous and muscle tissue.
- Supravalvular stenosis can be represented by an incomplete or complete membrane, localized narrowing, multiple peripheral pulmonary artery stenoses, and diffuse hypoplasia.
Pulmonary stenosis in newborns is quite common, as it is one of the types of congenital defects. In addition to ordinary stenosis, there is complex stenosis, which can develop due to pathology of the subvalvular and supravalvular sections. In most cases, only valve stenosis is diagnosed.
This phenomenon is characterized by the absence of a septum of the valve itself, as well as a change in its shape. In addition, there is a proliferation of fibrous tissue, and the efferent part in the right ventricle narrows.
The stages of pulmonary artery stenosis differ significantly in the nature of manifestation and symptoms:
- moderate stenosis (stage 1, the patient does not feel discomfort, only the ECG shows overloaded work of the right ventricle);
- severe stenosis (stage 2, upper blood pressure increases);
- severe stenosis (stage 3, there are symptoms of circulatory disorders, failures of the cardiovascular system are observed);
- decompensation (stage 4 of the manifestation of stenosis, in which a disturbance in the nutrition of the heart muscle and blood flow is clearly visible, but due to contractile insufficiency of the right ventricle, the pressure is often low).
Therapy tactics
Pulmonary stenosis is treated by a cardiologist or cardiac surgeon. If there are no clinical manifestations and heart failure (minor or moderate stenosis), then specific therapy is not required. The following drugs are sometimes prescribed to support the functioning of the heart and blood vessels:
- cardiac glycosides;
- potassium-containing products;
- diuretics;
- beta blockers;
- vitamin complexes.
Attention! For such patients, monitoring the condition 2 times a year will be sufficient.
The treatment regimen is determined only by a specialist, taking into account the characteristics of the patient’s body (age, concomitant diseases) and based on each specific case. The severe degree of the disease requires treatment. Surgery is the only effective method to prolong a person’s life. The surgical technique depends on the location of the defect:
- Balloon valvuloplasty is the insertion of a special balloon into the affected vessel, into which a stent is then installed to eliminate the narrowing. The operation is indicated for valvular stenosis of the pulmonary artery.
- Resection of part of the vascular walls is used for supravalvular localization of stenosis. The operation involves excision of the affected part of the vascular wall and installation of a patch from the layers of the own pericardium.
- In case of subvalvular stenosis, the affected part of the myocardium is excised at the exit from the right ventricle.
- The combined type of pathology is treated by combining several surgical techniques.
After surgical elimination of a narrowing of the vessel, normalization of blood circulation does not occur immediately. Signs of the disease gradually decrease, the patient’s condition stabilizes.
History taking
When diagnosing a disease in children, it is necessary to obtain as much information as possible about the factors that caused the development of cardiac pathology. You should ask the mother about the presence of bad habits, concomitant diseases, and previous infections during pregnancy.
The child is examined by a cardiologist and auscultates (listens) the patient. Aortic valve stenosis may be suspected when a systolic murmur occurs. Classic signs of a severe valve defect include hearing unusual sounds in the carotid arteries. A bifurcation of the second tone and a slow pulse in large vessels are noted. Systolic murmur is heard to the right and left of the upper edge of the sternum.
The appearance of aortic stenosis in a newborn is facilitated by maternal diseases:
- severe anemia;
- inflammation of the genital organs.
Increased pulsation is often detected on the baby’s upper and lower extremities.
A normal split second heart sound indicates the absence of severe aortic stenosis. The stable condition of the baby ensures the development of distal blood flow.
General description of the pathology
Before looking at the causes, symptoms and effective treatments, it is worth reviewing general information about stenosis. The pulmonary arteries are paired, fairly large branches of the pulmonary trunk that arise from the right ventricle.
The main function of this vessel is to transport venous (oxygen-poor) blood from the right atrium to the capillary system of the lungs, where gas exchange occurs and the blood is saturated with oxygen. In fact, this is where the pulmonary circulation begins. At the point where the pulmonary trunk exits the right atrium there is a tricuspid valve, which regulates blood flow.
Why is it developing?
The causes of aortic valve stenosis are the following:
- Genetic diseases. Deformation of the coronary artery may be accompanied by Williams syndrome, caused by chromosomal abnormalities.
- The presence of bad habits in the mother. Alcohol and drug use during pregnancy contributes to the development of severe congenital heart defects in the fetus.
- Infectious diseases. When a pregnant woman is initially infected with herpes or cytomegalovirus infection, the pathogen enters the fetus’s body, disrupting the formation of internal organs. Infection in the first trimester is especially dangerous.
- Stress, non-compliance with the daily routine, heavy physical activity. These factors negatively affect the development of the fetus, contributing to the appearance of birth defects.
- Living in an unfavorable environmental environment. High air and drinking water pollution negatively affects the course of pregnancy in women with chronic diseases of the excretory, digestive and cardiovascular systems.
- Poor nutrition. A deficiency of vitamins and nutrients in the mother's body contributes to the appearance of congenital heart defects in the unborn child.
- Exposure to ionizing radiation. Radiation promotes the death of embryonic cells, from which the internal organs of the fetus are subsequently formed.
- Taking medications that have a teratogenic effect. Such drugs include cytostatics, some antibiotics, antipsychotics, painkillers, and anticoagulants based on warfarin.
Symptoms depend on the severity of the narrowing of the aorta of the newborn’s heart:
- The first degree is considered compensated, the stenosis is mild. Blood circulation is not impaired, there are no signs of pathology. The defect is detected during mandatory examination of the newborn. Surgical intervention is not prescribed, the child remains under the supervision of a cardiologist.
- With second degree narrowing, acute heart failure develops. Shortness of breath appears, the child becomes weak and lethargic. He refuses to breastfeed and sleeps poorly. The skin of the nasolabial triangle acquires a bluish tint. The child often spits up and does not gain weight well.
- The third stage is accompanied by severe disturbances in the functioning of the heart. Due to the decrease in blood flow, the pulse may be difficult to feel. The rhythm of heart contractions is disturbed, shortness of breath is constantly present. There are short-term loss of consciousness caused by deterioration of blood supply to the brain. Treatment for narrowing of the 3rd degree is carried out only surgically.
- At the fourth stage, shortness of breath is pronounced. The skin becomes bluish and the child often loses consciousness. Surgery at this stage may not be effective.
- Fifth degree narrowing has an extremely severe course. Most children die in the first hours after birth. Surgery for this type of pathology is impossible.
Symptoms of pulmonary artery stenosis in children
Clinical manifestations of pulmonary stenosis in children depend on the severity of the narrowing of the lumen. Thus, minor and moderate stenosis may not manifest itself clinically for many years.
Severe stenosis appears almost immediately after the birth of the child and includes symptoms such as:
- Severe acrocyanosis or diffuse cyanosis is a bluish discoloration of areas of the skin (nasolabial triangle, fingertips, palms, feet) or the skin of the entire body,
- Dyspnea at rest and when feeding the baby,
- Lethargy or severe restlessness of the child,
- Poor weight gain in the first months of a child’s life,
- Shortness of breath on exertion as the baby's motor skills develop.
Description of the disease, code according to ICD-10
Aortic stenosis is a change in the structure of the aortic valve in such a way that the normal conduction of blood from the heart to the aorta is disrupted. As a result, the blood supply to most internal organs and systems of the human body, “connected” to the systemic circulation, deteriorates.
Among other valvular heart defects, aortic stenosis is the second most common after mitral stenosis: 1.5-2% of people of retirement age suffer from this disease, most of them (75%) are men.
In any healthy person, at the border of the left ventricle of the heart and the aorta, which originates from it, there is a tricuspid valve - a kind of “door” that allows blood from the heart into the vessel and does not release it back. Thanks to this valve, which is at least 3 cm wide when fully opened, blood flows from the heart to the internal organs in only one direction.
For various reasons, this valve may not begin to open completely; its opening becomes overgrown with connective tissue and narrows. As a result, the ejection of blood from the heart into the aorta decreases, and the blood not sent through the vessels stagnates in the left ventricle, which gradually leads to its enlargement and stretching.
The human heart, thus, begins to work in an abnormal mode, congestion in it worsens - all this has the most negative impact on overall health.
ICD-10 code for congenital aortic valve stenosis:
ICD-10 code for acquired aortic valve stenosis:
What happens to the body?
With aortic valve stenosis, the aorta will change: its valve contracts or tissue scarring occurs in it, eventually developing stenosis. In the heart, when the aortic valve does not function properly, blood flow is disrupted, resulting in the development of a defect.
The disease is manifested by angina attacks of the heart; blood flows to the brain with disruptions, which causes migraines and loss of orientation in space. As a result of the fact that blood is delivered to the aorta in small quantities, the pulse slows down, systolic pressure decreases, and diastolic pressure is either normal or increased.
What is aortic stenosis - just about the complex ones in the video:
What happens to blood pressure and why?
Ideally, the aortic opening is approximately 4 cm². With stenosis, it becomes narrower, and as a result, blood flow in the left ventricle becomes difficult. In order not to disrupt the normal functioning of the body, the heart is forced to work harder and increase the pressure in the chamber of the left ventricle so that blood moves freely through the narrowed lumen of the aorta. As blood enters the aorta, pressure increases. In addition, systole time is mechanically prolonged.
Such work of the heart does not go unpunished. An increase in systolic pressure causes an increase in the muscles (myocardium) of the left ventricle. Diastolic pressure increases.
What is the orifice area and what happens to it depending on the stage?
The dimensions of the valve opening show how much the aortic lumen is reduced. Normally, the area indicators are 2.5-3.5 cm². Conventionally, the dimension of the lumen can be divided into stages:
- A slight stenosis is determined, the lumen is from 1.6 to 1.2 cm².
- Moderate stenosis (from 1.2 to 0.75 cm²).
- Severe stenosis - the lumen decreases to 0.74 cm² or less.
Pulmonary artery stenosis in children and adults: causes, symptoms, surgery
The pulmonary artery (PA) is one of the largest vessels in the human body, carrying blood from the heart to the vessels of the pulmonary tissue, where the blood is enriched with oxygen, and thus the formation of the pulmonary circulation is completed.
In another way, this vessel is called the pulmonary trunk. If the lumen of the vessel becomes smaller, then they speak of stenosis, or pathological narrowing, of the pulmonary artery.
picture: valve form of pulmonary artery stenosis
Stenosis occurs due to congenital or acquired causes, and is characterized by the following hemodynamic processes in the heart:
- The right ventricle experiences stress as it pushes blood through the narrowed lumen of the pulmonary artery.
- The load on the ventricle may vary depending on the severity of the stenosis.
- Less blood enters the lungs than normal, as a result of which less blood is saturated with oxygen, and the body receives less oxygen overall, which leads to the development of hypoxia (oxygen starvation) of the internal organs.
- Constant load on the right ventricle leads to gradual wear and tear of the heart muscle, which is initially compensated by an increase in myocardial mass (right ventricular hypertrophy), and later leads to the development of severe cardiac right ventricular failure.
- Due to the constantly increased final volume of blood, which cannot be completely released into the artery, tricuspid regurgitation develops, that is, a reverse flow of blood is formed into the right atrium, which leads to stagnation of venous blood and disruption of microcirculation in the vessels of the internal organs - hypoxia is aggravated.
- Severe stenosis leads to the development of severe heart failure, which can cause death if left untreated.
Depending on the location of the lesion, supravalvular, subvalvular and valvular forms of stenosis are distinguished, that is, the narrowing is located above, below or at the level of the valve, respectively. Valvular pulmonary artery stenosis is more common than other forms.
forms of pulmonary artery stenosis by location
Isolated acquired pulmonary stenosis is rare. Pulmonary stenosis of a congenital nature is recorded much more often, ranking second in frequency among all congenital heart defects.
Congenital pulmonary stenosis (CPS)
Among the causes of congenital pulmonary artery stenosis, the following factors are identified that can influence the formation of the fetal cardiovascular system and the occurrence of congenital heart defects (CHD) during pregnancy:
valve for congenital stenosis
Genetic predisposition to malformations of the heart and large vessels, especially on the maternal side,
- Use of psychoactive substances, drugs, antibiotics by a pregnant woman, especially in the first trimester of pregnancy,
- Unfavorable working conditions during pregnancy, for example, work at chemical, paint and varnish and other types of industries, when a pregnant woman constantly inhales toxic substances,
- Viral diseases of the mother during pregnancy - rubella, infectious mononucleosis, infection by herpes group viruses,
- X-rays and other types of ionizing radiation during pregnancy,
- Unfavorable environmental conditions, for example, increased background radiation in some regions.
- Atherosclerosis of large vessels,
- Calcification of the aortic and pulmonary valves,
- Rheumatic damage to the heart valves, including the pulmonary valve,
- Specific inflammation of the inner wall of the pulmonary artery - syphilis, tuberculosis (rare),
- Hypertrophic cardiomyopathy with an increase in the mass of the myocardium of the right ventricle, resulting in an obstruction (obstacle) in the path of blood flow from the ventricle to the pulmonary artery,
- Compression of the pulmonary trunk from the outside - by a tumor of the mediastinum, enlarged lymph nodes, aortic aneurysm, etc.
Among the reasons that most often cause the development of acquired pulmonary artery stenosis are:
example of acquired stenosis due to rheumatism
Preventive actions
Prevention of the disease requires:
- eliminating potential risks for women during pregnancy;
- compliance with the rest and wakefulness regime;
- avoiding stress, psycho-emotional stress;
- maintaining a healthy lifestyle - engaging in feasible sports, giving up smoking and alcohol;
- early recognition and treatment of pathologies.
Children and adults with narrowing of the orifice of the pulmonary artery must be registered with a cardiologist. Twice a year or if necessary, you need to visit a doctor to monitor the condition.
Valvular stenosis of the pulmonary artery is detected at different stages of life. The more severe the obstruction, the earlier the valve abnormality is usually detected. Often the disease has no clinical picture. The disease is diagnosed when the only treatment option is surgery. Medicine offers safe surgical methods that will effectively and permanently eliminate narrowing of the artery.
';document.body.appendChild(d);document.pnctLoadStarted=(new%20Date()).getTime();document.pnctCnclLoad=function(){document.pnctLoadStarted=0;pl=document.getElementById('pnctPreloader' );if(pl)pl.parentNode.removeChild(pl)};document.getElementById('pnctCancelBtn').addEventListener('click',function(e){e.preventDefault();document.pnctCnclLoad()}); setTimeout(function(){var%20st=document.pnctLoadStarted;if(st>0&&((new%20Date()).getTime()-st>=14000)){document.pnctCnclLoad();alert('%3C %3F%3DYii%3A%3At%28%22uniprogy%22%2C+%22Unfortunately%2C+the+image+search+is+not+available.%22%29%3F%3E')}},15000);var %20e=document.createElement('script');e.setAttribute('type','text/javascript');e.setAttribute('charset','UTF-8′);e.setAttribute('src', '//postila.ru/post.js?ver=1&m=b&rnd='+Math.random()*99999999);document.body.appendChild(e)})());”>
Prevention
There is no special prevention for arterial stenosis, but the risk of developing pathology can be reduced. To do this, a woman during pregnancy must adhere to certain rules and monitor her health:
- If pregnancy is detected, you should immediately go to the antenatal clinic.
- Throughout your pregnancy, visit a gynecologist, take all necessary tests and ultrasound examinations.
- Take any medications only as prescribed by a doctor.
- Before planning pregnancy, get vaccinated against measles and rubella.
- Stop smoking and drinking alcohol.
- Watch your diet, eat only high-quality and fortified foods.
- For chronic pathologies, visit a doctor regularly.
All these measures will help not only reduce the risk of developing the stenopulmonary artery in the fetus, but also eliminate other disorders in its development. If, after birth, the baby is diagnosed with arterial stenosis, there is no need to delay treatment; the sooner appropriate treatment is carried out, the greater the chances of a successful recovery prognosis.
Pulmonary artery stenosis is one of the dangerous, but at the same time common diseases associated with heart and vascular disease. However, if the disease is recognized in time and treated, the child will be able to fully live a full life.
Disease statistics
To find out in more detail what pulmonary hypertension is, you should familiarize yourself with the statistics. The disease occurs in only 1-2 newborns out of every thousand. Almost 10% of children who require intensive care suffer from pulmonary hypertension. It is worth noting that most of them were born at term or slightly post-term.
Pulmonary hypertension is several times more common in children who were born by cesarean section - about 85% of all cases. Almost the entire number of diagnoses were made to newborn babies within the first three days of their life. Thanks to such early diagnosis, it is possible to minimize the number of deaths, because if treatment is not started in time, then approximately 80% of sick babies can die after living only a few days. Today, medicine is well aware of what it is – pulmonary hypertension, so the disease is treatable.