Human blood vessels - structure, functions, role in the body and possible pathologies
Almost a quarter of the human body consists of vessels - highways through which blood moves.
They serve to transport oxygen and nutrients to vital organs and tissues, participate in the removal of waste products, and also participate in maintaining optimal pressure in the body for the individual. Despite the similarity of functions, blood vessels have different sizes and structures.
Their importance for the body is equally important. For example, large arteries and veins cannot perform the work assigned to them without small, sometimes microscopic in diameter, arterioles, capillaries and venules.
Classification
In anatomy there is no extensive and branched classification of blood vessels. All of them are divided into three types depending on the size and location in the human body:
- Arteries are the largest tubular formations with a multilayer wall, through which blood is directed from the heart through the pulmonary or systemic circulation. Vessels of this type are subject to their own regulatory mechanisms, which depend primarily on the intensity of the heart and the volume of blood entering them. The blood flowing through the arteries is saturated with oxygen, which is why its color acquires a bright scarlet hue.
- Veins are a type of vessel in the circulatory system through which blood moves towards the heart. According to the structure of the wall, they are simpler than arteries; all types of tone regulation, except physical, are alien to it. Their inner wall is equipped with an obturator - a valve that prevents the reverse flow of blood. The blood flowing through the veins is saturated with carbon dioxide, which is why its color is much darker than arterial blood.
- Microcirculatory vessels are the most numerous types of blood vessels with a small lumen in diameter. These include arterioles and capillaries, through which arterial blood flows, venules, in which venous blood is present, as well as arteriovenular anastomoses, in which mixed blood (arterial and venous) flows. This group of tubular formations is most susceptible to humoral mechanisms regulating the tone of blood vessels.
The peripheral parts of the circulatory system differ significantly in structure and function from the central veins and arteries. Moreover, they are the most diverse, since each type of microvessel performs different tasks.
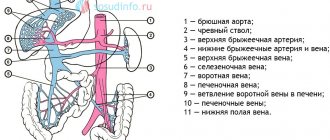
Main large vessels
Among all the blood and lymphatic vessels, the most important are large highways with a diameter of 2 cm or more. Despite the fact that their function is primarily to transport blood, a person’s health and well-being depends on their condition.
The most important blood vessel in the human body is the aorta, which extends directly from the heart. It has the largest diameter (25-30 mm) and has the most complex wall structure.
It is characterized by increased elasticity and strength, since it has to withstand enormous loads from cardiac output.
This is a fairly large and very elastic tube that can stretch when blood flows and contract when the ventricle relaxes.
The aorta is divided into two slightly smaller, but no less significant branches in the human body - descending and ascending. The descending part is divided into the thoracic and abdominal aorta, and the ascending part is represented by the coronary arteries, subclavian and common carotid arteries. They are characterized by increased elasticity and strength. They are able to contract, directing blood to vital organs.
The largest veins with which the human body is equipped are represented by the inferior and superior vena cava. They are more than 2 cm in diameter and their main role is to transport carbon dioxide-rich blood from the lower and upper parts of the body to the heart and lungs.
Structure and functions of blood vessels
The structure of the walls of the transport system of the human body determines the functions of blood vessels and their localization in the body. The closer to the heart, the more complex the anatomical picture: more layers, more functional features and additional receptor cells. The only thing that unites all types of blood tubes is the number of layers in the walls. There are three of them in total:
- Endothelium is the layer lining the inside. The structure of the inner lining of blood vessels varies depending on their types. Thus, large arteries and veins are lined with a dense layer of endothelium, while in microcirculatory vessels they are located in a more scattered, loose order. The sparse layer of endothelial cells located in the capillaries facilitates the penetration of oxygen, carbon monoxide and nutrients into the surrounding tissues and in the opposite direction. In arteries and veins, blood components practically do not interact with surrounding tissues. In all types, the presence of special cells can be traced, located on the basement membrane - the thinnest layer separating the inner cover (intima) of blood vessels from its middle layer. They serve to control the contractility of large and medium-sized blood tubes, the speed of blood flow and metabolism.
- The middle layer is the thickest of all wall elements, consisting of smooth muscle and elastic cells. It is he who narrows and expands the lumen of blood vessels, regulating the movement of blood through a closed system and the pressure created in it. The presence and thickness of these membranes varies in different parts of the circulatory system. For example, arteries are equipped with the thickest layer of collagen and muscle cells, while capillaries and veins are practically devoid of them. In the walls of arteries located closer to the heart, there are more collagen fibers, designed to improve the distensibility of the vascular walls and resistance to blood pressure. In peripheral arteries, which do not experience much stress, muscle fibers predominate, which actively contract to maintain the required blood flow rate.
- The outer (marginal) layer of the vessel consists of connective tissue fibers, the density of which varies depending on the size of the vessel: large veins and arteries are surrounded by a fairly dense connective tissue membrane, while the microcirculatory sections of the circulatory system are surrounded by a very loose membrane. Thanks to this, capillary blood delivers nutrients and oxygen to the lymph and tissues, and “absorbs” from them products that require disposal.
The walls of all parts of the circulatory system are equipped with receptors and effectors - special cells that obey nervous and humoral regulatory mechanisms. The largest number of them was found in the aortic arch and carotid arteries. A smaller number of angioreceptors are located in thin arteries and veins, and the microvasculature.
Despite the fact that the condition of the blood vessels depends on the psycho-emotional state, a person cannot consciously control the mechanism of increasing or decreasing the degree of blood supply in one or another part of the body, regulate blood pressure without taking special medications, etc.
Diseases
Angiopathy, or a disease affecting the functionality of the circulatory system, is a much more versatile and broad concept than it might initially seem.
In medicine, there are at least a thousand deviations directly related to arteries, veins, capillaries, venules and arterioles, arteriovenular anastomoses.
According to statistics, this group of diseases is the most common cause of death in all age and social groups.
Typical arterial pathologies are:
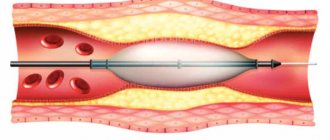
- Stenosis, as a result of which insufficient blood penetrates through the narrowed lumen. As a result of the disease, tissue ischemia develops, in simple words, oxygen starvation. The disease can affect both the main trunk of the coronary artery (aorta) and smaller branches.
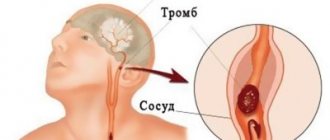
- Occlusion is one of the types of narrowing of the lumen, which can be caused by a blood clot or cholesterol plaque. The presence of a blood clot in a blood vessel leads to the same consequences as stenosis. Obtuse angle branches of arteries and small-diameter tubes are more susceptible to pathology.
- Dilation or dilatation of an artery, which leads to the formation of an aneurysm. The pathology is diagnosed in people with reduced vascular elasticity. Most often it affects the aorta, carotid and cerebral arteries.
- Delamination of the wall followed by its rupture. This disease affects the largest arteries that are subject to increased stress: the aorta, coronary and pulmonary vessels.
Not always medicine can offer methods that improve the course of diseases or completely eliminate them. Initially, improvement is achieved by taking medications to improve the elasticity of the arteries and lower blood pressure.
With narrowing caused by blood clots or atherosclerotic deposits, no drug can lead to complete recovery. The only way to reduce the threat to life is surgery. In case of stenosis, a stent is installed, and in case of occlusion, part of the artery or deposits are removed from their lumen.
Pathologies of the arteries lead to diseases such as angina and myocardial infarction, stroke, aneurysm and intermittent claudication.
Common vein diseases include varicose veins and thrombosis. The first is an irreversible stretching of the walls with the formation of pockets - varicose nodes, in which blood stagnates. The condition is accompanied by ischemia, expressed by a feeling of heaviness in the legs and dull pain, swelling. In varicose pockets, a blood clot often forms in the lumen of the blood vessel. Under favorable conditions, it is fixed against the wall and remains in place. With increased load, stress, or increased pressure, a blood clot can break off and float through the circulatory system, provoking life-threatening conditions: pulmonary embolism, ischemic stroke of the brain and internal organs, etc.
To eliminate vein diseases, conservative and surgical methods of therapy are used. In the initial stages, it is enough to take drugs that increase the tone of the veins and prevent the formation of blood clots. For progressive forms, thrombectomy or removal of the most damaged areas of the veins is used.
The vessels of the microvasculature rarely undergo pathological changes. The most dangerous disease of this part of the circulatory system is considered to be a vascular neoplasm that arises at the site of the arteriovenular anastomosis. By growing into a nearby lymphatic vessel, a malignant tumor can spread to other organs and tissues.
: arteries and veins, arterioles, venules
Source: https://bloodvessel.ru/krovenosnaya-sistema-cheloveka/krovenosnye-sosudy
Forecast
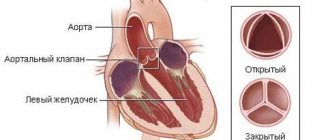
Newborns with transposition of the great vessels require urgent surgical intervention.
In the absence of timely cardiac surgical treatment, the prognosis for the outcome of TMS is always unfavorable. According to statistics, about 50% of children die during the first month of life, and more than 2/3 of children do not survive until the age of 1 year due to severe hypoxia, increasing acidosis and heart failure.
The prognosis after cardiac surgery becomes more favorable. With complex defects, positive long-term results are observed in approximately 70% of patients, with simpler ones - in 85-90%. Regular monitoring by a cardiac surgeon is of no small importance in the outcome of such cases. After corrective operations, patients may develop long-term complications: stenosis, thrombosis and calcification of conduits, heart failure, etc.
Transposition of the great vessels is one of the most dangerous heart defects and can only be corrected surgically. The timeliness of cardiac surgery is of no small importance for its favorable outcome. Such operations are carried out up to 2 weeks of the child’s life, and only in some cases they can be delayed up to 2-3 months. It is desirable that such a developmental anomaly be detected before the baby is born, and that pregnancy and childbirth are planned taking into account the presence of this dangerous congenital heart defect in the unborn child.
Pulmonary and bronchial arteries
The lungs are supplied by two separate vascular systems, consisting of the pulmonary and bronchial arteries. The pulmonary arteries carry deoxygenated blood at low pressure.
The connection between the pulmonary and bronchial arteries also lies in the fact that they, bypassing the capillaries, form vascular anastomoses.
They supply 99% of the blood flow to the lungs and participate in gas exchange at the alveolar capillary membrane.
Functions of the bronchial arteries
These arteries provide nutrition to the supporting structures of the lungs, including the pulmonary arteries, but do not usually participate in gas exchange. The branches of the bronchial artery carry oxygenated blood to the lungs at a pressure six times higher than the pressure in the pulmonary arteries. They are connected to the lungs through several microvascular anastomoses at the level of the alveoli and respiratory bronchioles.
In various cases that involve pulmonary artery compromise (eg, vasculitis and chronic pulmonary thromboembolic disease), the arteries and their anastomotic connections may dilate, allowing a greater percentage of cardiac output to flow through the bronchial artery system.
Location
Bronchial arteries usually originate from the proximal descending thoracic aorta. They are called orthotopic when they are between the superior endplate of the T5 vertebral body and the inferior endplate of the T6 vertebral body. The landmark for orthotopic arteries on angiography is 1 cm above or below the level of the left main bronchus when crossing the descending thoracic aorta.
Bronchial arteries that are located elsewhere in the aorta or arise from other vessels are called ectopic.
On CT angiography that assessed hemoptysis, 64% of patients had orthotopic arteries, and the remaining 36% had at least one ectopic artery, most often arising from the inferior surface of the aortic arch.
Other reports following bronchial artery ultrasonography indicate the presence of ectopic arteries in 8.3% to 56% of all patients, depending on the method of examination (i.e., autopsy or angiography).
Potential ectopic sites of origin include:
- inferior aortic arch;
- distal descending thoracic aorta;
- subclavian artery;
- thyroid cell;
- internal mammary artery;
- coronary artery.
Bronchial arteries that originate from the coronary artery can cause myocardial infarction or angina due to coronary theft.
Clinical relevance
Bronchial arteries can be changed in various pathologies. For example, they dilate and become tortuous in cases of hypertension and pulmonary thromboembolism. For some diseases (bronchiectasis, cancer, tuberculosis, etc.) that lead to hemoptysis, arterial embolization can be used to stop the bleeding.
It is still unknown whether arteriosclerotic disease affects these arteries.
But American scientists conducted a pilot study to estimate the prevalence of arteriosclerosis of the arteries, compare it with certain clinical and laboratory arteriosclerotic parameters or any coexisting coronary artery disease and confirm the clinical significance.
Arteries measuring 10-15 mm in length were taken from 40 patients with an average age of 62-63 years. Their medical history and detailed clinical and laboratory risk factors for arteriosclerosis were recorded.
After ultrasound examination of the bronchial arteries, their average diameter was 0.97 mm. Histology revealed medial calcific sclerosis in only 1 patient (2.5%) without concurrent established atherosclerotic lesions or luminal narrowing.
In addition, vessel diameter was significantly correlated not only with highest disease stage (p = 0.031) but also with proximal bronchial branch occlusion (p = 0.042).
Scientists noted a slight correlation between atherosclerosis and metabolic syndrome (p = 0.075).
Definition of the pulmonary artery and its function
The pulmonary artery begins at the level of the right ventricle of the heart and then splits in two to reach each lung, where it divides into many branches.
The role of the pulmonary artery is to transport deoxygenated blood from the heart to the lungs. A pulmonary embolism can occur in the pulmonary artery when it is obstructed by a clot that cuts off circulation.
Divers sometimes become victims of pulmonary embolism after a gas bubble forms in the pulmonary artery.
Branch location
The branch of the pulmonary artery has a length that ranges from 4.5 cm to 5 cm. Its diameter is 3.5 cm and its thickness is about 1 mm.
The horizontal part of the chest touches the pulmonary branch along its entire length.
The pulmonary artery is surrounded by a serous membrane, which is characteristic of the aorta.
Pulmonary artery diseases
A pulmonary embolism is a blockage of the arteries by a clot or gas bubble that does not dissolve in the blood. The arteries usually suffer from the consequences of thromboembolic disease. Methods for diagnosing pulmonary embolism:
- perfusion scintigraphy, which allows you to see the difference between normal ventilation and vascularization impaired by a clot. This examination is able to detect the difference between ventilation and perfusion, allowing an accurate diagnosis of the patient to be made;
- An angioscope (arteriography/CT) is used to diagnose an already diseased lung.
Some congenital heart defects can negatively affect these arteries:
- absence or atresia of the pulmonary artery;
- narrowing or stenosis of the pulmonary artery;
- incorrect location.
If the pulmonary artery pressure is too high, then pulmonary arterial hypertension or PAH is diagnosed, which is a completely different disease from general arterial hypertension. It can be either primitive (that is, without a reason) or secondary.
Superior and inferior vena cava
The human body has two types of vena cava: superior vena cava and inferior vena cava. Both serve to transport blood from organs to the heart. Thus, the inferior vena cava receives blood from various organs located in the abdominal cavity, digestive tract and lower extremities through the portal vein.
The superior vena cava collects blood from the head, neck, chest and upper extremities through the vena cava. These veins have a common point in the right atrium of the heart.
Conclusion
The bronchial arteries should not be confused with the pulmonary arteries. They are part of the pulmonary circulation and provide functional vascularization of the lungs, bringing oxygenated white blood from the right ventricle to be oxygenated. On the other hand, the bronchial arteries play an important role: they bring oxygenated and nutrient-rich blood to the lungs.
Source: https://FB.ru/article/394318/legochnyie-i-bronhialnyie-arterii
Brief anatomy of the lungs
The lungs are located in the chest and fill most of it. The lungs are a complex structure of a plexus of blood, airways, lymphatic and nerve pathways. Between the lungs and other organs (stomach, spleen, liver, etc.) there is a diaphragm that separates them.
It should be noted that the right and left lungs are anatomically different. The main difference is the number of shares. If the right one has three of them (lower, upper and middle), then the left one has only two (lower and upper). Also, the left lung is longer than the right.
Inside the lungs are the bronchi. They are divided into segments that are clearly separated from each other. There are 18 such segments in the lungs: 10 in the right and 8 in the left, respectively. Subsequently, the bronchi branch into lobes. There are approximately 1,600 of them in total - 800 for each lung.
The bronchial lobes are divided into alveolar ducts (from 1 to 4 pieces), at the end of which there are alveolar sacs, from which the alveoli open. All this together is called the collective name airways, which consist of the bronchial tree and the alveolar tree.
Below we will discuss the features of the blood supply to the pulmonary system.
Pulmonary Vascular Disease: Symptoms, Causes, Tests and Treatment
Pulmonary vascular disease is the medical term for a disease that affects the blood vessels leading to or from the lungs. Most forms of pulmonary vascular disease cause shortness of breath.
What is pulmonary vascular disease?
The definition of pulmonary vascular disease is simple: any condition that affects the blood vessels on the path between the heart and lungs.
Blood flows from the heart to the lungs and back to the heart. This process continually fills the blood with oxygen and allows carbon dioxide to be exhaled. Here's how the process works:
- Low-oxygen blood returns from the body's tissues through the veins back to the right side of the heart.
- The right heart pumps low-oxygen blood through the pulmonary arteries to the lungs. This blood is filled with oxygen.
- Oxygen-rich blood returns from the lungs back to the left side of the heart. The left heart pumps oxygen-rich blood into the body through the aorta and many other arteries.
Any part of the cardiopulmonary blood flow can be damaged or blocked, leading to pulmonary vascular disease.
Causes of pulmonary vascular diseases
The causes of pulmonary vascular diseases vary depending on which pulmonary vessels are affected. Pulmonary vascular diseases are divided into several categories:
Pulmonary arterial hypertension: Increased blood pressure in the pulmonary arteries (the drainage of blood from the heart to the lungs). Pulmonary arterial hypertension can be caused by lung disease, an autoimmune disease, or heart failure. When there is no obvious cause, it is called idiopathic pulmonary arterial hypertension.
Pulmonary venous hypertension: Increased blood pressure in the pulmonary veins (carrying blood from the lungs to the heart). Pulmonary venous hypertension is most often caused by congestive heart failure. A damaged mitral valve in the heart (mitral stenosis or mitral regurgitation) can contribute to pulmonary venous hypertension.
Pulmonary embolism: A blood clot breaks loose from a deep vein (usually in the leg), travels to the right heart, and is pumped to the lungs. In rare cases, the embolism may be a large air bubble or fat globule rather than a blood clot.
Chronic thromboembolic disease: In rare cases, a blood clot in the lungs (pulmonary embolism) is never absorbed by the body. Instead, a reaction occurs in which multiple small blood vessels in the lungs also become diseased. The process is slow and gradually affects most of the pulmonary arterial system.
Symptoms of pulmonary vascular diseases
Symptoms of pulmonary vascular disease vary depending on several factors:
- Suddenness of the process affecting the pulmonary blood vessels
- Which pulmonary blood vessels are affected (where is pulmonary vascular disease)
- How severely is the pulmonary vascular system affected?
For example, a sudden, large pulmonary embolism that blocks a large pulmonary artery can cause severe shortness of breath and chest pain. But a very small pulmonary embolism (blocking just a small blood vessel) may not cause noticeable symptoms.
Although the symptoms of pulmonary vascular disease can vary widely, each cause of pulmonary vascular disease has a number of common symptoms:
Pulmonary arterial hypertension This most often causes slowly progressive shortness of breath. As the condition worsens, chest pain or fainting (fainting) with exertion may occur.
Pulmonary embolism: A blood clot in the lungs usually occurs suddenly. Shortness of breath, chest pain (often worsened by taking deep breaths) and rapid heartbeat are common symptoms. Symptoms of a pulmonary embolism range from subtle to severe, depending on the size of the blood clot.
Pulmonary venous hypertension: This form of pulmonary vascular disease also causes shortness of breath due to congestive heart failure that is usually present. Shortness of breath may be worse when lying down, when blood pressure is not controlled, or when there is excess fluid (edema).
Tests for pulmonary vascular disease
Based on a person's symptoms, signs, and medical history, a doctor may begin to suspect the presence of pulmonary vascular disease. The diagnosis of pulmonary vascular disease is usually made using one or more of the following tests:
Computed tomography (CT): A CT scanner takes multiple X-rays and a computer creates detailed images of the lungs and chest. CT usually detects pulmonary embolism. A CT scan can also reveal problems affecting the lungs themselves.
Ventilation/perfusion scan (V/Q scan): This nuclear medicine test shows how well the lungs fill with air. These images are compared with images of how well blood flows through the pulmonary blood vessels. Discrepant areas may indicate the presence of a pulmonary embolism (blood clot).
Diagnostics
In almost 100% of cases, this heart defect is diagnosed immediately after the birth of a child, in the maternity hospital.
Most often, TMS is detected in the maternity hospital. When examining the child, the doctor detects a pronounced medially displaced cardiac impulse, cardiac hyperactivity, cyanosis and expansion of the chest. When listening to the sounds, an increase in both tones, the presence of systolic murmur and murmurs characteristic of concomitant cardiac defects are revealed.
For a detailed examination of a child with TMS, the following diagnostic methods are prescribed:
- ECG;
- Echo-CG;
- chest x-ray;
- catheterization of cardiac cavities;
- angiocardiography (aorto-, atrio-, ventriculo- and coronary angiography).
Based on the results of instrumental studies of the heart, the cardiac surgeon draws up a plan for further surgical correction of the anomaly.
Diagnostic methods
When examining a baby in the maternity hospital, the pediatrician identifies signs of intracardiac and systemic blood flow disorders:
- increased heart rate,
- skin cyanosis,
- both tones are intense,
- noise during systole and blood passing through the holes inside the septum.
After 1 month, the configuration of the heart changes and signs of pulmonary hypertension appear. This can be confirmed by additional research methods:
- X-ray: the heart is shaped like an egg, its size is larger than normal, the vascular bundle is narrowed in the anterior projection, and enlarged in the lateral projection.
- Ultrasound of the heart: abnormal position of the vessels, the chambers are dilated, the walls are hypertrophied. Symptoms of abnormal septal structure.
- Probing of the cavities: oxygen deficiency in the left half and excess in the right, pressure in the right ventricle does not differ from the aortic.
- Contrasting the ventricles, atria, aorta: the contrast agent passes from the left half to the pulmonary trunk, and from the right to the aortic trunk.
Features of hemodynamics in newborns
The life of an infant with a heart defect depends entirely on the form of transposition and the presence of communication between the two circles of blood flow. If they are not present (complete rearrangement of blood vessels), the death of the newborn is inevitable.
The role of communications that compensate for the hemodynamic disconnection of the arterial and venous circles can be:
- unclosed duct or oval window;
- septal defects;
- malformations of bronchial vessels.
The best option for children are large holes between the ventricles or atria that allow blood to flow in both directions and allow it to mix. Moderate narrowing of the pulmonary artery prevents the lungs from overflowing, then the child’s condition is satisfactory.
Surgery as an emergency aid for a baby
In case of complete displacement of the great vessels, the operation is performed according to vital indications - as soon as possible.
The only limitation is the high level of pulmonary hypertension. Prostaglandin (Vasaprostan or Alprostan) helps prevent closure of the aortic duct at the stage of preoperative preparation.
The following types of surgical treatment of transposition of the great vessels are used:
- endovascular balloon dilatation of the oval window, Botall's duct;
- removal of part of the septum between the atria;
- restructuring of blood flow inside the atrium with a patch for redistribution of arterial and venous blood. A duct is created through which the blood flow is aligned.