Causes
Thrombosis is a consequence of increased blood clotting, clumping of blood cells and slowing blood flow. Predisposing factors in the pathogenesis of thrombosis:
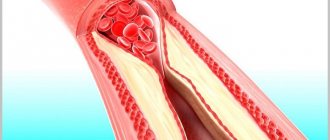
- Atherosclerosis – increased fragility of blood vessels, decreased elasticity of the walls, formation of cholesterol plaques;
- Hereditary predisposition, smoking and long-term use of hormones, especially in women;
- Fever or dehydration when taking diuretics;
- Changes in hormonal levels during pregnancy and the early postpartum period;
- Infections of viral etiology with impaired permeability of vascular walls and increased aggregation of blood cells;
- Inflammatory processes in the ear, nose and throat area, complicated by a purulent course;
- Congenital blood diseases with an increased coagulation index and an increased number of platelets;
- Malignant tumors and their metastasis;
- Kidney pathology that changes the acid-base balance of the blood;
- Diabetes;
- Hypertension with frequent crises;
- Obesity;
- Surgical operations and manipulations;
- Head injuries.
Diagnosis of the disease
The presence of blood clots can only be determined in a specialized hospital setting using the following diagnostic methods:
- Magnetic resonance angiography - this method helps to determine how narrowed the walls of blood vessels are and the intensity of blood circulation.
- Duplex ultrasound scanning will help determine where the blood clots are and what their number is. During the examination, you can measure the speed at which blood moves through the vessels.
- CT is a computed tomography that allows you to obtain information about the condition of all vessels of the neck and head.
If you suspect the formation of blood clots in the carotid arteries and symptoms appear, you must immediately consult a doctor; it is important to undergo all the necessary examinations to prescribe antithrombosis therapy.
Clinical picture
Common complaints:
- persistent or persistent increasing headaches;
- impaired sensitivity and motor skills of the muscles of the face, arms and legs, right or left half of the body;
- persistent distortion of speech and its understanding;
- blurred vision;
- loss of body balance, dizziness;
- feverish condition;
- excessive sweating;
- blood pressure surges;
- uncontrolled acts of defecation and urination;
- loss of consciousness;
- convulsive contractions, muscle twitching;
- nausea, vomiting.
Complaints regarding thrombosis of the basilar artery supplying the brain stem:
Complaints characteristic of deterioration of blood supply to the brain through the internal carotid arteries:
- serious weakening of visual perception, even blindness;
- inability to speak, speech confusion;
- deterioration of motor function of the upper extremities;
- tremor;
- fainting;
- paresis of one or both halves of the body.
Complaints characteristic of deterioration of blood supply to the cerebral cortex, tissues of the neck and face through the external carotid arteries:
- dry mucous membranes;
- neck pain;
- distortion of facial expressions, paralysis of facial muscles;
- fainting;
- slurred speech;
- constant pain in the head.
Complaints characteristic of dysfunction of the cerebellum due to poor blood supply through the vertebral artery, including the clinic of spinal diseases:
- forced head posture;
- unilateral headache;
- muscle tension in the neck and back of the head;
- lack of air;
- loss of balance;
- decreased sensitivity and tingling of the face;
- deterioration of visual perception;
- difficulty speaking;
- pallor and cyanosis.
Treatment of carotid artery thrombosis
If, based on the results of the examination, carotid artery thrombosis is diagnosed, only a doctor can prescribe treatment. Self-medication in such a situation is strictly prohibited in order to avoid even greater health problems. Therapy for thrombosis depends on the severity of the disease and the degree of blockage of blood vessels. Treatment with medications is necessary to restore quality blood circulation to the cerebral cortex. Therapy consists of prescribing the following groups of drugs:
- Thrombolytics promote the resorption of blood clots that have already formed in the vessels. Doctors most often prescribe Urokinase, Fibrinolysin and Streptokinase.
- Drugs that thin the blood are anticoagulants. With the help of these medications, the quality of blood flow improves. The course of treatment with anticoagulants can last from several days to several years. The most popular drugs for carotid artery thrombosis are Heparin, Warfarin, Phenilin and Dicumarin.
Head and neck diagnostics
Research using equipment:
- Ultrasound examination is a method that allows you to assess the condition of the arteries, the presence of lesions and pathologies, the speed of blood flow and its possible disruption.
- Doppler ultrasound (USD) - measuring the frequency of ultrasound waves reflected from moving blood elements, allows us to detect a decrease in blood flow (stenosis), damage and weakening of the tone of the arteries.
- Duplex ultrasound scanning (USDS) - analysis of the image of the ultrasound wave reflected from the blood elements allows you to see blood clots and evaluate the reduction in diameter and thickening of the walls of blood vessels.
- Ultrasound triplex scanning - analysis of the ultrasonic wave reflected from the blood elements in a color image of the vessels allows you to assess their patency; the most informative method of ultrasound examination.
- Electroencephalography is an analysis of a graphical representation of fluctuations in the electrical potentials of the brain in order to identify changes in its functional indicators, which makes it possible to differentiate thrombosis of the cerebral arteries from epilepsy and amnesia; prescribed for slurred speech.
- Magnetic resonance imaging (MRI) - analysis of the absorption and reflection of electromagnetic waves from tissues allows us to identify features of the anatomical structure of blood vessels and their changes: tortuosity, narrowing of the lumen, pathology of the vessel wall; localize the thrombus, assess its extent; assess the pathology of brain structures and determine the area of their damage.
- Computed tomography (CT) is an analysis of cross sections of the brain in order to accurately localize a blood clot, allowing one to study the chemical structure of tissues and their X-ray density, which usually changes in diseases.
MRI visualizes soft tissues with diffuse and focal lesions of brain structures and pathologies of the spinal cord, but practically does not show the bones of the skull. In some cases, both studies should be carried out simultaneously, complementing each other and together giving a complete picture of the disease. - Cerebral angiography is an X-ray examination during which a contrast agent is injected into the artery, which is carried by the bloodstream through the cerebral vessels; the analysis makes it possible to assess the degree of vasoconstriction, identify tumors, hematomas, aneurysms, ulcers and malformations; allows you to decide the feasibility of performing an operation to destroy or dissolve a blood clot, dilate a vessel, and coagulate it.
What are the dangers of a blood clot in the cervical spine?
The jugular venous system simultaneously includes several cervical vessels, which are necessary for the outflow of blood from the head and neck.
If we consider in detail the anatomical structure of a person, we can distinguish 3 main pairs of jugular veins in this system:
- internal;
- external;
- front
The first of the vessels is the largest and allows most of the blood to exit the skull. The vein connects with the subclavian artery.
The external vein is significantly smaller in size and is located in the front of the neck. It is clearly released during singing, screaming or coughing. The last vessel is considered the smallest of the above.
These are the saphenous veins, which create the so-called jugular venous arch.
Thrombosis can occur in any of the above veins, but statistics show that most often it develops in the external jugular vein.
Over time, this process leads to mechanical damage to the vessel wall, and the body begins to intensively produce fibrin and platelets. As a result of this process, a blood clot occurs.
Some chronic diseases can contribute to the appearance of blood clots even without vascular damage.
This disease is a pathological condition caused by blockage of the vessel cavity with a blood clot, which causes blood flow disturbances and, as a result, some organs and systems suffer. The lack of adequate therapy can cause the development of a number of rather dangerous complications, so it is extremely important to stop not only its manifestations, but also the cause itself.
It is impossible to unambiguously answer the question about the age category of patients suffering from this disease.
Both young people and elderly people are susceptible to it, but in the latter the disease is somewhat more common. Doctors also note that gender may be a risk factor.
Thus, among patients who come to medical institutions with a similar problem, the majority are men.
According to the international classification of diseases, created to systematize the statistical information obtained, this pathology has ICD 10 code I82.
Symptoms of jugular vein thrombosis
The symptoms of the disease will be determined by where exactly the pathological process is localized. Also, the severity of clinical signs of thrombosis is determined by the degree of vein occlusion. If there is a small thrombus in the jugular vein, the patient may not know about its existence for a long time, since there are no signs that bother him.
When the lumen of the vessel is seriously blocked, the main symptom of the disease is sharp pain in the neck and collarbone.
Also, along the entire course of the vein there may be aching pain, radiating to the upper extremities and sometimes leading to errors in diagnosis due to the lack of a clear location.
Swelling is often noticeable and increases over several days or hours. Other possible signs of jugular vein thrombosis:
- cyanosis of the skin on the neck, collarbone;
- tension, visually noticeable expansion, bulging of a vein in the neck;
- feeling of bulging, coldness, itching, tingling, heaviness in the vein area;
- neck pain when touched;
- sometimes - limited arm mobility, muscle hypotonia.
The symptoms described above are characteristic only of the acute stage of thrombosis. After such phenomena subside, a reverse development of the clinic, its regression, is observed. But for some people, the disease does not stop completely; it becomes chronic. In this case, pain in the neck and collarbone can sometimes be observed.
Anatomical features
In order to better understand the mechanisms of occurrence and possible localization of pathology, one should turn to anatomy.
In the human body there are 3 main pairs of jugular veins susceptible to thrombosis:
- Internal. The largest among the listed vessels, responsible for the drainage of blood from the skull and normal metabolism in the brain. The venous line begins from the jugular foramen, descends to the area of the sternoclavicular junction, and merges with the subclavian artery. In medical practice, it is most often used for the purpose of catheterization for hemodialysis, plasmapheresis, and long-term infusion therapy.
- Outdoor. In terms of its size, it ranks second among the vessels of this system and is responsible for draining blood saturated with carbon dioxide from the external parts of the cervical spine and head. It is located close enough to the surface that it can be seen and felt.
- Front. The pair is located under the chin and is part of the venous arch.
Each of these pairs is susceptible to thrombosis, but as statistics show, it is the outer vessel that most often clogs the thrombus.
The jugular vein system includes three pairs of blood vessels located in the neck:
- Internal. A fairly large vessel that delivers the bulk of blood from the cranial cavity. It originates in the jugular foramen of the skull and below merges with the subclavian artery.
- Outdoor. Its function is to drain blood from the neck, head, and face. It is a vessel smaller in diameter than the internal one. You can see it if you tense the ligaments.
- Front. This is the smallest vessel in this system.
Possible complications
Thrombosis is always a danger. You should be afraid, first of all, of embolism. If a blood clot breaks off and begins to migrate through the circulatory system, it can instantly block the lumen in the vessel. Fortunately, in the case of the jugular vein this happens very rarely, but sometimes a blockage of the pulmonary artery occurs, which can even lead to death.
Also, a blood clot in the jugular vein can lead to sepsis and serious vision problems, including blindness, due to papilledema.
In the case of the development of postthrombophlebitis syndrome, congestion forms in the veins as a result of the destruction of their valves, the arms and legs may swell, the skin and soft tissues change their appearance.
The prognosis for thrombosis may vary. It will be doubtful if an infectious process has occurred in the internal organs, which can provoke sepsis. If the patient consulted a doctor before the development of any disorders, then the prognosis is very favorable.
Vein thrombosis is always a complex disease that reflects a serious problem in the human body.
First of all, any thrombosis threatens thrombus embolism, although in the case of the jugular veins this rarely happens.
The likelihood of dying from thromboembolism of the veins of the upper body is quite small, but, nevertheless, jugular vein thrombosis occasionally still leads to blockage of the pulmonary artery by a thrombus with a high risk of death.
Complications of the disease can also include swelling of the optic disc and the development of blindness, sepsis. A late complication may be postthrombotic disease. If thrombosis spreads to the brachial or axillary veins (a rare complication), then severe swelling entails compression of the arterial trunks. Sometimes the compression can be so severe that it leads to gangrene.
Drug treatment
The basis of therapy for the formation of blood clots in the circulatory system is the use of direct and indirect anticoagulant drugs. They are aimed at thinning the blood by reducing the level of fibrinogen, a substance whose concentration increases to form clots.
Direct anticoagulants include:
- Fibrinolysin,
- Fraxiparine,
- Heparin.
After a decrease in the prothrombin index, they switch to medications with an indirect anticoagulant effect, such as Curantil or Aspirin.
Another important aspect in complex therapy is the prescription of phlebotonics, whose action is aimed at improving metabolic processes and eliminating inflammation.
Remember! The dosage of any medications and the method of their use are prescribed exclusively by a competent medical professional.
If necessary, antispasmodics are prescribed to reduce the tone of the vascular walls and relieve pain. The addition of sepsis indicates the need for antibacterial therapy.
You can find out what varifort for varicose veins is and the opinion of Elena Malysheva from our article.
Carrying out diagnostics
The main and most accessible diagnostic method is ultrasound with Doppler sonography. The veins of the neck have good visualization for this study, and difficulties may arise only with thrombosis of the internal jugular vein. In this case, the doctor has to rely on the results of Doppler ultrasound, including determining the speed of blood flow.
A more detailed picture of the study is provided to the specialist by phlebography with the introduction of a contrast agent into a vein.
In addition, sometimes CT or MRI techniques are used to diagnose the disease, as well as laboratory tests to identify fibrin breakdown products.
To exclude other pathologies and differentiate pain due to jugular vein thrombosis, the patient may undergo other types of studies:
- chest x-ray;
- ECG, EEG;
- angiography;
- scintigraphy, etc.
Surgical intervention
If conservative therapy does not bring the desired result, minimally invasive surgical procedures can be used to eliminate the blood clot. The frequency of surgical treatment for this disease is significantly inferior to classical therapy.
The most common methods are:
- Aspiration thrombectomy is the mechanical removal of thrombolytic mass through a puncture made through the skin.
- Endovascular thrombolysis is the delivery of a thrombolytic drug directly to the site of a vascular lesion by subcutaneous insertion of a special catheter. Thus, its patency is partially or completely restored.
Read about the manifestations and methods of treating varicocele on both sides in our material.
Treatment methods
Since thrombosis of the veins of the upper body is rarely complicated by thromboembolism, treatment is predominantly conservative. The patient does not have strict bed rest, but physical activity should be prohibited. The following treatment methods are used:
- Taking direct anticoagulants - Heparin, Fibrinolysin, Fraxiparin. In the acute stage of the disease, these drugs are administered intravenously in the hospital. The course of therapy with these drugs continues until fibrinogen disappears in the plasma and until the level of the prothrombin index normalizes. Subsequently, indirect anticoagulants are prescribed, for example, Aspirin Cardio, Cardiomagnyl.
- Taking or administering nicotinic acid to activate blood thinning and blood clot resorption.
- The use of venotonics - Detralex, Troxevasin, Aescusan, Glivenol. These drugs are needed to speed up metabolism in the walls of the veins, relieve inflammation and relieve pain.
- Introduction of antispasmodics to relax the muscle wall - No-Shpa, Papaverine.
- Local application of heparin ointment, troxevasin ointment for additional effect on the vessel walls.
Surgery for jugular vein thrombosis is extremely rare. As a last resort, minimally invasive techniques are used - percutaneous endovascular thrombolysis, transluminal aspiration thrombectomy. These methods involve dissolving the clot. or its removal using a balloon catheter.
Since a thrombus in the jugular vein is a serious pathology, it is advisable to diagnose it in the initial stages. True, it’s quite difficult if he doesn’t make himself known in any way. But, if you still have some suspicions, it is better not to refuse to visit the doctor.
In order to detect a blood clot, modern instrumental and laboratory research methods are used:
- Ultrasound of the area where the jugular vein runs.
- Duplex scanning of vessels, which will allow you to examine possible pathologies of the veins in a two-dimensional image.
- MRI – makes it possible to examine in detail centimeter by centimeter the area under study.
- Thrombodynamics is a study that allows you to identify blood clotting indicators.
- Thrombosis time tests – aimed at assessing the extrinsic clotting pathway.
- Thromboelastography. With this study, the doctor receives a complete picture of the elastic properties of blood clots.
Are you one of those millions of women who struggles with varicose veins?
Have all your attempts to cure varicose veins been unsuccessful?
Have you already thought about radical measures? This is understandable, because healthy legs are an indicator of health and a reason for pride. In addition, this is at least human longevity. And the fact that a person protected from vein diseases looks younger is an axiom that does not require proof.
Judging by the fact that you are now reading these lines, victory in the fight against varicose veins and unsightly areas on the body is not yet on your side...
Have you already thought about inpatient treatment? This is understandable, because varicose veins are a very dangerous disease that, if not treated in a timely manner, can be fatal. Stars on the legs, fatigue, terrible swollen veins... All these symptoms are familiar to you firsthand.
Source: https://sevsity.ru/pozvonochnik/tromb-sheynom-otdele-pozvonochnika-grozit/
Treatment of blood clots in the arteries of the brain
It is necessary to immediately begin a set of therapeutic measures.
- Drugs that directly affect the rheological properties of blood:
- Vasodilators;
Antihypertensives – reduce blood pressure;
The prescription and use of thrombolytics is only under medical supervision and monitoring using a coagulogram.
Uncontrolled use of these drugs can have a negative effect, including the development of DIC syndrome. To prevent a stroke, the following can be done:
- Carotid endarterectomy – removal of blood clots and atherosclerotic plaques on the carotid artery when 70% stenosis is detected and in patients who have suffered a transient ischemic attack (TIA). Surgery is often used to prevent future strokes.
- Stenting and angioplasty is an expansion of the diameter of narrowed sections of arteries, with atherosclerotic changes in those that are located in hard-to-reach areas. A balloon is inserted into the narrowing areas, which, when inflated, increases the diameter of the vessel. A mesh element, a stent, is placed in the artery to prevent the narrowing of the vessel. Allows you to avoid dangerous consequences such as stroke and ischemic attack.
Balloon dilatation and neurosurgery
Another surgical method that can be performed is balloon dilatation. This operation is performed under local anesthesia. A special filter is installed in the damaged vessel to catch blood clots and plaques. A balloon catheter is inserted into the vessel, which uses pressure to move the blood clots towards the filter. The process lasts about an hour. The duration of rehabilitation after surgery depends on the complexity of the operation and the patient’s health status after it. On average, the duration is from 2 weeks to 1 month.
The most reliable type of surgical intervention is the replacement of damaged areas of blood vessels with prostheses. A bypass is created for blood flow due to the operation using an installed shunt, which is located over the damaged areas. Sometimes neurosurgical operations are used, as a result of which nodes, clogged vessels and plexuses are removed.
After surgery, blood circulation to the brain significantly improves, and a slowdown in the atherosclerotic process is observed. The most effective result after surgery is possible if there is an embolic form of vascular damage. Any treatment for carotid artery thrombosis should be carried out under the supervision of the attending physician, after passing all the necessary examinations.
Preventive actions
- Proper nutrition - eating foods low in cholesterol, rich in vitamins and fiber.
- Avoid drinking alcohol and smoking.
- Active lifestyle – daily walking.
- Fighting obesity.
- Treatment of hypertension, diabetes.
- Observation by a doctor, regular laboratory tests.
- Taking antiplatelet agents (cardioaspirin), drugs to strengthen the vascular wall (ascorutin), and lower cholesterol (levastatin).
- Treatment of chronic venous insufficiency.
*Click on the picture to open it in full size.
Cerebral artery thrombosis is a dangerous disease, but you can live with it. The earlier the disease is diagnosed, the higher the likelihood of a favorable outcome. Properly prescribed treatment for diseases of the cardiovascular system and timely prevention of thrombosis reduce the risk of blood clots in the vessels.
Headache, dizziness, tinnitus, spots before the eyes... These are nothing more than signs of vertebral artery syndrome - a disease in which the blood circulation of the posterolateral parts of the brain is affected.
It is necessary to treat the pathology, as it can lead to the early development of ischemic stroke.
Therapeutic measures must be comprehensive.
Thrombosis of the cerebral arteries - carotid, basilar, vertebral: symptoms and treatment
Cardiovascular diseases still occupy a leading position in the list of fatal diseases, which is explained by their acute course and serious complications. One of the most dangerous is thrombosis of the arteries of the brain and neck - blocking of a vessel with a blood clot, which leads to ischemia of the nervous tissue, and then to a stroke.
Causes
Thrombosis is a consequence of increased blood clotting, clumping of blood cells and slowing blood flow. Predisposing factors in the pathogenesis of thrombosis:
- Atherosclerosis – increased fragility of blood vessels, decreased elasticity of the walls, formation of cholesterol plaques;
- Hereditary predisposition, smoking and long-term use of hormones, especially in women;
- Fever or dehydration when taking diuretics;
- Changes in hormonal levels during pregnancy and the early postpartum period;
- Infections of viral etiology with impaired permeability of vascular walls and increased aggregation of blood cells;
- Inflammatory processes in the ear, nose and throat area, complicated by a purulent course;
- Congenital blood diseases with an increased coagulation index and an increased number of platelets;
- Malignant tumors and their metastasis;
- Kidney pathology that changes the acid-base balance of the blood;
- Diabetes;
- Hypertension with frequent crises;
- Obesity;
- Surgical operations and manipulations;
- Head injuries.
Clinical picture
Common complaints:
- persistent or persistent increasing headaches;
- impaired sensitivity and motor skills of the muscles of the face, arms and legs, right or left half of the body;
- persistent distortion of speech and its understanding;
- blurred vision;
- loss of body balance, dizziness;
- feverish condition;
- excessive sweating;
- blood pressure surges;
- uncontrolled acts of defecation and urination;
- loss of consciousness;
- convulsive contractions, muscle twitching;
- nausea, vomiting.
Thrombosis of the basilar artery
Complaints regarding thrombosis of the basilar artery supplying the brain stem:
- throbbing occipital pain;
- dizziness, patients are “stormy, rocking on the waves”;
- blurry visual perception;
- impaired sensitivity of the skin around the mouth;
- gaze paresis – the inability to move both eyes simultaneously in vertical or horizontal directions;
- impaired sensitivity of half of the face;
- fainting;
- noise in ears.
Decreased sensitivity of one half of the face is sometimes a harbinger of blockage of the basilar artery.
Thrombosis of the carotid artery (internal, external)
Complaints characteristic of deterioration of blood supply to the brain through the internal carotid arteries :
- serious weakening of visual perception, even blindness;
- inability to speak, speech confusion;
- deterioration of motor function of the upper extremities;
- tremor;
- fainting;
- paresis of one or both halves of the body.
Complaints characteristic of deterioration of blood supply to the cerebral cortex, tissues of the neck and face through the external carotid arteries :
- dry mucous membranes;
- neck pain;
- distortion of facial expressions, paralysis of facial muscles;
- fainting;
- slurred speech;
- constant pain in the head.
Vertebral arteries
Complaints characteristic of dysfunction of the cerebellum due to poor blood supply through the vertebral artery, including the clinic of spinal diseases:
- forced head posture;
- unilateral headache;
- muscle tension in the neck and back of the head;
- lack of air;
- loss of balance;
- decreased sensitivity and tingling of the face;
- deterioration of visual perception;
- difficulty speaking;
- pallor and cyanosis.
Head and neck diagnostics
Thrombosis leads to oxygen starvation and severe impairment of brain function. The rupture of a blood clot leads to a stroke, which can be fatal. To make a diagnosis, clear and quick action is necessary.
- Anamnesis collection: specific complaints, presence of background diseases;
- Examination of the patient: determination of changes in neurological status (impaired facial sensitivity, different pulse strength in the hands, when turning the head - increased pain or dizziness).
- Laboratory tests: standard general blood test (increased ESR, leukocyte count) and cerebrospinal fluid analysis (increased protein and neutrophils), urine test, coagulogram (increased levels of prothrombin and fibrinogen, decreased blood clotting time);
- Research using equipment:
- Ultrasound examination is a method that allows you to assess the condition of the arteries, the presence of lesions and pathologies, the speed of blood flow and its possible disruption. Doppler ultrasound (USD) - measuring the frequency of ultrasound waves reflected from moving blood elements, allows us to detect a decrease in blood flow (stenosis), damage and weakening of the tone of the arteries.
- Duplex ultrasound scanning (USDS) - analysis of the image of the ultrasound wave reflected from the blood elements allows you to see blood clots and evaluate the reduction in diameter and thickening of the walls of blood vessels.
- Ultrasound triplex scanning - analysis of the ultrasonic wave reflected from the blood elements in a color image of the vessels allows you to assess their patency; the most informative method of ultrasound examination.
- Electroencephalography is an analysis of a graphical representation of fluctuations in the electrical potentials of the brain in order to identify changes in its functional indicators, which makes it possible to differentiate thrombosis of the cerebral arteries from epilepsy and amnesia; prescribed for slurred speech.
- Magnetic resonance imaging (MRI) - analysis of the absorption and reflection of electromagnetic waves from tissues allows us to identify features of the anatomical structure of blood vessels and their changes: tortuosity, narrowing of the lumen, pathology of the vessel wall; localize the thrombus, assess its extent; assess the pathology of brain structures and determine the area of their damage.
- Computed tomography (CT) is an analysis of cross sections of the brain in order to accurately localize a blood clot, allowing one to study the chemical structure of tissues and their X-ray density, which usually changes in diseases.
MRI visualizes soft tissues with diffuse and focal lesions of brain structures and pathologies of the spinal cord, but practically does not show the bones of the skull. In some cases, both studies should be carried out simultaneously, complementing each other and together giving a complete picture of the disease. - Cerebral angiography is an X-ray examination during which a contrast agent is injected into the artery, which is carried by the bloodstream through the cerebral vessels; the analysis makes it possible to assess the degree of vasoconstriction, identify tumors, hematomas, aneurysms, ulcers and malformations; allows you to decide the feasibility of performing an operation to destroy or dissolve a blood clot, dilate a vessel, and coagulate it.
Treatment of blood clots in the arteries of the brain
It is necessary to immediately begin a set of therapeutic measures.
Medication
- Drugs that directly affect the rheological properties of blood:
- Anticoagulants - have an effect on the coagulation process, inhibiting the adhesion of platelets to each other and preventing small clots from forming one large one. Clopidogrel, indobufen, ditazol, ticlopidine;
- Thrombolytics – used for moderate and higher degrees of thrombosis: they dissolve the clot and initiate fibrinolysis. Streptokinase, tenecteplase;
- Antiplatelet agents – suppress blood clotting, reduce thrombus formation. Warfarin, heparin, dicoumarin, hirudin and drugs from other medicinal groups. Aspirin (acetylsalicylic acid) is the most popular of these.
- Drugs acting on the walls of the vessel:
- Vasodilators;
- Antihypertensives – reduce blood pressure;
- Pentoxifylline derivatives enhance microcirculation in brain tissue.
- Nootropics are medications that stimulate metabolism in nervous tissue, increase resistance to oxygen deficiency, and help improve intellectual abilities and memory.
The prescription and use of thrombolytics is only under medical supervision and monitoring using a coagulogram. Uncontrolled use of these drugs can have a negative effect, including the development of DIC syndrome.
Surgical
To prevent a stroke, the following can be done:
- Carotid endarterectomy – removal of blood clots and atherosclerotic plaques on the carotid artery when 70% stenosis is detected and in patients who have suffered a transient ischemic attack (TIA). Surgery is often used to prevent future strokes.
- Stenting and angioplasty is an expansion of the diameter of narrowed sections of arteries, with atherosclerotic changes in those that are located in hard-to-reach areas. A balloon is inserted into the narrowing areas, which, when inflated, increases the diameter of the vessel. A mesh element, a stent, is placed in the artery to prevent the narrowing of the vessel. Allows you to avoid dangerous consequences such as stroke and ischemic attack.
Preventive actions
- Proper nutrition - eating foods low in cholesterol, rich in vitamins and fiber.
- Avoid drinking alcohol and smoking.
- Active lifestyle – daily walking.
- Fighting obesity.
- Treatment of hypertension, diabetes.
- Observation by a doctor, regular laboratory tests.
- Taking antiplatelet agents (cardioaspirin), drugs to strengthen the vascular wall (ascorutin), and lower cholesterol (levastatin).
- Treatment of chronic venous insufficiency.
*Click on the picture to open it in full size.
Cerebral artery thrombosis is a dangerous disease, but you can live with it. The earlier the disease is diagnosed, the higher the likelihood of a favorable outcome. Properly prescribed treatment for diseases of the cardiovascular system and timely prevention of thrombosis reduce the risk of blood clots in the vessels.
Source: https://oserdce.com/sosudy/trombozy/arterij/golovy-i-shei.html
How to cure this type of thrombosis
Since thrombosis of the upper body is rarely complicated by thromboembolism, treatment should be conservative and very careful. The patient is not prescribed strict bed rest, but serious physical exercise should still be completely prohibited.
Most often, treatment involves taking medications such as anticoagulants: Heparin, Fibrinolysin, Fraxiparin. In acute stages of the disease, these drugs are administered intravenously. Therapy usually continues until fibrinogen disappears from the plasma. Subsequently, the patient is prescribed indirect anticoagulants.
Experts recommend administering nicotinic acid to patients, which has a positive effect on the rate of blood clot resorption and promotes blood thinning. Taking venotonics accelerates the metabolic process in the walls of the veins.
This eliminates unpleasant pain sensations. To relax muscle tissue, antispasmodics are usually prescribed, for example, the well-known No-Shpa. Applying Heparin ointment to the jugular vein will only speed up the healing process.
Cervical spine worn out discs what to do
Patients who suffer from jugular vein thrombophlebitis need immediate specialist consultation, examination and subsequent treatment under the supervision of a physician.
Judging by the fact that you are now reading these lines, victory in the fight against varicose veins and unsightly areas on the body is not yet on your side...
And you have already thought about inpatient treatment {q} This is understandable, because varicose veins are a very dangerous disease, which, if not treated in a timely manner, can be fatal. Stars on the legs, fatigue, terrible swollen veins... All these symptoms are familiar to you firsthand.
Features of the disease and ICD classification
This disease is a pathological condition caused by blockage of the vessel cavity with a blood clot, which causes blood flow disturbances and, as a result, some organs and systems suffer.
It is impossible to unambiguously answer the question about the age category of patients suffering from this disease. Both young people and elderly people are susceptible to it, but in the latter the disease is somewhat more common.
According to the international classification of diseases, created to systematize the statistical information obtained, this pathology has ICD 10 code I82.
Reasons for development
The development of vertebral artery thrombosis can be triggered by the following factors affecting the human body:
- congenital disorders of the structure of vascular walls;
- abnormal tortuosity;
- injuries;
- inflammation of nearby tissues;
- atherosclerosis;
- hormonal imbalance;
- osteocondritis of the spine;
- muscle spasm in the neck;
- intervertebral hernia.
https://www..com/watch{q}v=FmJ2wnJRLp8
Risk factors that contribute to the development of pathology include a sedentary lifestyle or constant uncomfortable posture, which results in compression and mechanical damage to blood vessels. The disease is hereditary in nature.
Source: https://osankasovet.ru/pozvonochnik/tromb-sheynom-otdele-pozvonochnika-grozit.html
What it is? ↑
This is a combination of symptoms that occur when the lumen of the above vessel decreases and the compression effect on the surrounding nerve plexus.
In order to understand how the syndrome develops, let us consider the topographic anatomy of the vertebral vessels.
There are two subclavian arteries in total.
They arise from the subclavian arteries on each side, go to the 6th cervical vertebra, enter the canal formed by the transverse processes of the cervical vertebrae, and go in it to the foramen magnum.
With bone pathology of this section, these vessels are almost always affected.
In the cranial cavity they merge together, forming the basilar artery, which supplies the following structures:
- brain stem;
- cerebellum;
- sections of the temporal lobes;
- cranial nerves;
- inner ear.
They account for only 15-30% of blood flow (the rest is provided by the carotid arteries).
When they are damaged, symptoms of damage to all those structures that they supply blood appear.
The vertebral artery is divided into the following segments (they are indicated on ultrasound by Roman numerals):
- I – from its separation from the subclavian artery to the entrance to the bone canal;
- II – from 6 to 2 vertebrae;
- III – from the exit point from the 6th vertebra to the entrance to the cranial cavity. This is where the bends of the artery are located, that is, this place is dangerous because blood clots and atherosclerotic plaques can accumulate in it, blocking the blood flow;
- IV – from the moment the artery enters the cranial cavity until the confluence of the two vertebral arteries.
Most of the vertebral artery passes in a mobile canal of the vertebrae and their processes.
The sympathetic nerve (Frank's nerve) passes through the same canal, which weaves around the artery on all sides.
At the level of the I-II cervical vertebrae, the artery remains covered only by soft tissue (mainly the inferior oblique abdominal muscle).
Prognosis and prevention
Timely seeking help from a medical institution and correctly selected treatment methods eliminate the development of complications. In this case, a favorable outcome of the disease can be predicted. An exception should be considered pathology caused by metastases during the development of malignant neoplasms.
When sepsis is added, it is impossible to clearly assess what the prognosis will be. However, it should be noted that if inflammatory processes occur, provoked by the lack of timely treatment of jugular vein thrombosis, it will be doubtful. When diagnosing a reversible process of organ damage, the recovery period can be 3-6 months.
As a rule, with timely conservative treatment and elimination of risk factors, the prognosis for a person’s life is favorable (with the exception of advanced cancer). However, all measures should be taken to prevent such a serious and life-threatening condition as thrombosis in the future. For this purpose, prevention must necessarily include giving up all bad habits, treating varicose veins under the supervision of a doctor, normalizing nutrition, and maintaining an active lifestyle.
Main symptoms ↑
The disease begins with a person experiencing severe headaches.
They can be associated with a forced uncomfortable position of the head during the day or during sleep, cold or neck injury.
- spreads from the neck through the back of the head to the temples;
- changes depending on head movements (in some positions it can completely disappear);
- pain is felt when palpating the cervical vertebrae;
- the character can be anything: pulsating, shooting, bursting, contracting;
- the duration of the attack can be any: from minutes to several hours;
- accompanied by other symptoms described below.
It most often occurs after sleep, especially if the person rested on a high pillow, but it can develop during the day and lasts from several minutes to hours.
With this symptom, the Shants collar serves as a method of differential diagnosis: if wearing it eliminates dizziness, then we are talking about vertebral artery syndrome.
Photo: Shants collar
With this syndrome, most people notice noise in both ears.
If there is noise in only one ear, then it almost always occurs on the affected side, less often on the opposite side.
This symptom appears at different moments and has different severity, which depends on the state of the labyrinth of the inner ear and those structures that are directly related to it.
The period of remission is characterized by weak and low-frequency noise in the ear; before the onset of an attack, it intensifies and becomes higher-pitched. If the syndrome was caused by osteochondrosis of the cervical spine, then such noise often occurs at night, in the early morning hours.
The nature of the noise changes when you turn your head.
There may be numbness in parts of the face (especially around the mouth), neck, or one or both upper extremities.
This is due to impaired blood supply to certain areas.
If the syndrome was caused by stenosis of one or two vertebral arteries, loss of consciousness is caused by hyperextension of the head for a long time.
The cause of this condition is vertebrobasilar insufficiency.
Before such fainting, one of the following symptoms usually appears:
- dizziness;
- instability;
- numbness of the face;
- speech disorder;
- transient blindness in one eye.
In most cases, nausea and vomiting are warning signs of the disease.
In this case, this symptom is not associated with increased intracranial pressure.
It does not arise immediately; it is caused not only by a disruption of the normal blood supply to the brain, but also by moral reasons, when a person is tired of frequent attacks of headaches, dizziness, and constant tinnitus.
Due to degenerative changes in the intervertebral discs, the vertebrae become displaced relative to each other.
As a result, the lumen of the vertebral artery decreases, and the sympathetic plexus (Frank's nerve) is also involved.
This causes the development of the following symptoms:
- dizziness;
- The headache, which usually has a throbbing or burning character, spreads from the back of the head to the eyebrow or temple. This pain is usually localized in one half of the head, it intensifies when turning the head and neck;
- noise in both ears;
- hearing impairment;
- fog before the eyes;
- nausea, vomiting;
- fluctuations in blood pressure in any direction;
- feeling of heartbeat;
- there may be pain in the shoulder and arm on one side;
- Pain in the eyes.
Thrombus in the carotid artery: internal thrombosis, treatment, symptoms, diagnosis – About Blood
Arterial thrombosis is a disease characterized by the formation of a blood clot in the lumen of a vessel and impaired circulation in the tissues below the blockage. When a thrombus blocks more than 75% of the artery lumen, signs of tissue hypoxia appear and metabolic products accumulate. With obstruction of 90% or more, necrosis develops.
Reasons for appearance
Arterial thrombosis can occur anywhere in the human circulatory system. Clot formation is a natural process that helps prevent bleeding. If it forms in a healthy vessel, we are talking about pathology - the blockage interferes with normal blood circulation and can disrupt the functioning of vital organs.
There are various causes of blood clots, the identification of which is important. Without eliminating the provoking element, it is impossible to prescribe adequate treatment. And without understanding the risk factors, it is difficult to prevent the disease.
Causes of arterial thrombosis:
- damage to the arterial wall (mechanical, allergic, infectious) makes its surface rough, this contributes to the retention of blood elements, they overlap each other;
- disorders in the blood coagulation system - the higher the blood viscosity, the more likely the formation of blood clots;
- a slowdown in blood flow in various parts of the arterial network provokes the development of stagnation, which contributes to the formation of blood clots.
The most common cause of acute arterial thrombosis is atherosclerosis . This disease affects many arteries of various sizes.
Lipoproteins and cholesterol are deposited on them, the vessels become less elastic and their lumen decreases.
In such areas, blood flow is hampered, and the presence of atherosclerotic plaques contributes to the sedimentation of other blood elements, and a blood clot forms.
Risk factors:
- atherosclerosis;
- age;
- disorders in the blood coagulation system;
- smoking and drinking alcohol;
- injuries;
- heredity;
- excess weight;
- kidney pathology;
- sepsis;
- taking hormonal medications;
- chemotherapy;
- postoperative period;
- physical inactivity;
- staying in a static position for a long time;
- oncological pathology;
- blood vessel diseases.
Symptoms of arterial thrombosis
However, arterial thrombosis is manifested by a number of common features: all patients experience a feeling of numbness, pain that radiates to adjacent areas in the form of pulsation.
There is an increase in discomfort during physical activity and pressure on the lesion.
Regardless of location, there is a high risk of clot rupture or the development of a dangerous complication - pulmonary embolism.
Aortic thrombosis
With prolonged ischemia, the following symptoms are observed:
- paroxysmal pain in the abdomen after eating, radiating to the lumbar region, back of the head, neck, chest on the left;
- nausea, vomiting, alternating constipation and diarrhea;
- due to constant intestinal dysfunction, a person refuses to eat, body weight decreases;
- arterial hypertension;
- when the aorta is blocked in the bifurcation area, intermittent claudication develops due to the transition of the pathological process to the iliac arteries;
- duodenal ulcer;
- performance decreases and depression develops.
When the aortic lumen is completely blocked, acute ischemia develops. There are 3 successive stages of intestinal damage: ischemia, infarction, peritonitis. The prognosis is favorable if assistance is provided in the first two stages.
Main symptoms:
- severe pain syndrome;
- the abdominal muscles are tense;
- diarrhea, involuntary bowel movements;
- after 6 hours the patient feels dramatically better;
- hypotension, tachycardia;
- paralytic intestinal obstruction, a sharp deterioration in health.
Blockage of the abdominal aorta is life-threatening; without qualified assistance provided on time, organ necrosis, intestinal necrosis, infarction of the kidneys, spleen, liver and death are possible. The difficulty of diagnosis lies in the fact that the symptoms of the pathology are characteristic of an acute abdomen.
Carotid artery thrombosis
Thrombosis affects 2 carotid arteries:
- the external carotid artery (ECA) delivers blood to the tissues of the face and head, the outer meninges, it is more susceptible to thrombosis;
- The internal carotid artery (ICA) supplies blood to the cerebral lobes and pituitary gland.
Men over 50 years of age are more susceptible to carotid artery thrombosis, but there is a risk of the disease in a person of any age and gender.
Symptoms of damage to the external carotid artery are: severe pain in the neck and head, numbness, dizziness, loss of consciousness; complications develop as a result of the pathology: cataracts, increased intracranial pressure, the appearance of noises of varying volume and tone, damage to the optic nerve, blurred vision during physical activity. loads, changes in the retina.
Thrombosis of the internal carotid artery has other symptoms. There are speech disturbances, mood changes, memory impairment, numbness and cramps in the arms and legs, decreased vision, hallucinations, headaches occur in the form of attacks, during which the stomach spasms.
Pulmonary artery thrombosis
Blockage of the pulmonary artery develops when a clot that has formed in the superior vena cava, right side of the heart, or vessels of the lower extremities breaks off. With the flow of blood it reaches the vessels of the lungs.
The pulmonary artery reaches 2.5 centimeters in diameter, so to block its lumen the thrombus must be large. A smaller clot gets stuck in one of the branches. This condition may be asymptomatic.
If a large clot enters, the functioning of a segment or even a lobe of the lung is disrupted.
Symptoms:
- shortness of breath for no reason;
- heart murmurs;
- breathing becomes shallow and rapid
- decreased blood pressure;
- pale grayish skin;
- increased heart rate;
- pain on palpation of the abdomen;
- chest pain.
Thrombosis of the subclavian artery
Acute blockage of the subclavian artery causes disruption of blood flow, development of ischemia of the upper extremities and vertebrobasilar insufficiency. The main symptoms are headache, hearing impairment, dizziness, disturbances in gait and vision, coldness, pale skin of the hands and decreased sensitivity.
The acute form of the disease, leading to irreversible changes in tissues - gangrene - appears rarely. More often, the disease grows gradually, in several stages:
- initial (numbness, paresthesia, coldness);
- partial compensation (pain, coldness, weakness of the arms, impaired blood supply to the brain);
- pronounced symptoms (manifestations occur not only during exercise, but also at rest, fine movements of the hands are difficult);
- necrosis (cyanosis, swelling, ulcers and gangrene).
Tissue necrosis during thrombosis of the subclavian artery rarely develops due to the well-developed bypass blood flow.
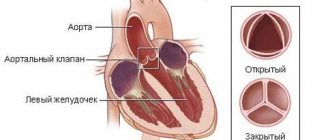
Coronary artery thrombosis
The most common cause of blockage of the coronary vessels is atherosclerotic disease.
Pathogenetic factors that increase the risk of the disease are the same as in other localizations: heredity, concomitant diseases, poor lifestyle.
Coronary thrombosis is not always provoked by the formation of clots in these arteries; often the damage occurs due to the detachment of a blood clot in another vessel in hypertensive patients.
It is important to timely assess the symptoms of coronary artery thrombosis, since only medical care will prevent the development of myocardial infarction.
Coronary thrombosis has the following symptoms:
- severe pain in the chest;
- pallor;
- difficulty breathing;
- loss of consciousness.
It is possible to develop stent thrombosis, which has similar symptoms to coronary artery disease. Such patients require emergency care. The person who has the stent placed must constantly monitor their condition. If you experience a sudden feeling of fatigue, shortness of breath, exhaustion, or angina, you should immediately consult a doctor.
Thrombosis of the splenic artery
Splenic artery thrombosis occurs in 1-3% of patients and is rarely diagnosed. The cause of the development of the pathological process may be the formation of a blockage in the area of the splenic vessel or existing pathology in the abdominal organs, as well as injury.
//www..com/watch?v=9R8tIqtxOPM
Symptoms of splenic artery embolism are manifested by pain in the left hypochondrium, which intensifies with inspiration or during coughing. In some cases, the lesion is asymptomatic. The result of ischemia is the development of splenic infarction with subsequent scarring, the formation of an abscess or cyst.
Diagnostics
Laboratory methods:
- Complete blood count: increased erythrocyte sedimentation rate, thrombocytosis, leukocytosis, change in color index may indicate thrombosis. Which indicators will be increased depends on the cause of the disease.
- An enzyme-linked immunosorbent test detects the presence of infectious diseases, tumor markers and hormonal imbalances.
- The coagulogram determines the state of the blood coagulation system: coagulation time, prothrombin index, activated partial thromboplastin time, plasma fibrinogen.
- The patient is referred for molecular genetic analysis if there is a suspicion of a hereditary form of the pathology.
Instrumental methods:
- duplex scanning;
- computed and magnetic resonance imaging;
- X-ray contrast angiography;
- radionuclide scanning to detect a thrombosed area;
- electroencephalography and rheoencephalography for carotid artery thrombosis;
- electrocardiography and echocardiography for coronary thrombosis.
Treatment
Thrombosis of vascular arteries is treated in a hospital setting. Various groups of drugs are used:
- anticoagulants (Heparin);
- antispasmodic therapy (No-spa);
- thrombolytics are administered during treatment, as well as during emergency transportation of the patient to the hospital (Streptokinase, Urokinase);
- antiplatelet agents should be given to the patient immediately after the onset of symptoms (Aspirin);
- means for improving tissue trophism (Reopoliglyukin);
- sedatives;
- antiarrhythmic drugs for coronary artery thrombosis;
- analgesics, novocaine blockades;
- to reduce the manifestations of hypoxia, the patient is placed in pressure chambers with a high oxygen content;
- with an uncompressed thrombus, it is possible to administer a large dose of thrombolytic drugs through a catheter, this helps dissolve the clot.
If drug therapy does not have the desired effect, surgical intervention is performed - thrombectomy. The blood clot is removed and the affected segment of the vessel is replaced. Artificial and organic materials are used as a substitute.
In addition, suturing, bypassing, or vein ligation may be used. To prevent embolism of the pulmonary arteries at high risk, vena cava filters are installed. Surgical treatment also depends on the location of the blockage.
A common procedure for coronary artery thrombosis is dilation of the affected vessel using balloon angioplasty.
Prevention
Prevention of arterial thrombosis involves eliminating risk factors. The first measure to prevent the disease that the patient must follow is maintaining a healthy lifestyle.
Exercising, walking, quitting smoking and drinking alcohol reduce the risk of thrombosis. Changing your diet reduces the likelihood of one of the main causes of blockage of blood vessels - atherosclerosis.
Following a diet allows you to normalize weight, which also has a positive effect on the condition of the circulatory system.
Source:
Thrombus in the carotid artery: causes, symptoms, first aid and treatment
- Patients are often interested in what consequences such a phenomenon as a blood clot in the carotid artery can have for the brain and the body as a whole.
- Let's consider what symptoms this type of thrombosis is characterized by, and what actions should be taken if you discover its signs.
What is carotid artery thrombosis
Carotid artery thrombosis is the formation of a blood clot (thrombus) in the lumen of the artery.
It is dangerous in that, since this artery is the path through which blood is sent to the brain, the clot can be carried by the flow into the vessels of the brain soon after formation.
Source: //igl-clinic.ru/venerologiya/tromb-v-sonnoj-arterii-thromboz-vnutrennej-lechenie-simptomy-diagnostika.html
Causes ↑
There are two main groups of reasons:
Vertebrogenic vertebral artery syndrome
This is one that is associated with pathologies of the spine.
Thus, in children, the disease can often be caused by abnormalities in the development of the vertebrae, as well as injuries to the cervical spine. In adults, the syndrome develops with spinal injuries, spasms of the cervical muscles, as well as with degenerative lesions (with ankylosing spondylitis, osteochondrosis) and some types of tumors.
A prerequisite for the development of vertebrogenic vertebral artery syndrome is the anatomical features of the bone canal in which the designated artery passes.
Nonvertebrogenic causes (not related to spinal pathologies)
These reasons are divided into three groups:
- occlusive pathologies of arteries: arteritis, thrombosis, their atherosclerotic lesions, embolism;
- deformation of blood vessels: their kinks, pathological tortuosity, abnormalities in the course of arteries;
- compression of the vertebral arteries from the outside - by spasmed muscles, abnormally developed cervical ribs, scars (for example, after catheterization of blood vessels or neck surgery).
The child develops the syndrome due to the following reasons:
- abnormal course of arteries;
- congenital pathological tortuosity of blood vessels;
- trauma, including birth trauma;
- muscle spasm due to hypothermia or torticollis - congenital or acquired, arising due to various reasons.
Root Causes
Why does such a disease appear? Thrombosis of the internal carotid artery can be divided into types based on the area of localization of the blood clot. The main reasons for the appearance are listed below:
- Formation of a blood clot in the subclavian vessel.
- Pulmonary vein thromboembolism.
- Thrombosis in the veins of the heart.
- Acute atherosclerosis.
- Vascular stenosis.
- Age above sixty years.
- Having diabetes of any type.
- Active smoking.
- Predisposition to blood clots.
The appearance of a blood clot in a vein without any reason is extremely rare, in about three cases out of a hundred. According to statistics, thrombosis occurs due to atherosclerosis in 90 percent of cases. We should not exclude a situation where a blood clot in the carotid artery, which appeared in a vein, breaks off and quickly reaches the vessels in the head.
Diagnostics ↑
Suspecting vertebral artery syndrome is the task of not only a neurologist, but also a general practitioner.
Based on the description of the symptoms, as well as examination data (tension of the neck muscles, pain when pressing on the processes of the cervical vertebrae and scalp), the doctor questions this diagnosis and refers it for instrumental examination.
It is carried out using several basic methods:
- Doppler ultrasound. It looks and is performed like a regular ultrasound and allows you to evaluate the anatomy, patency, speed and nature of blood flow in the arteries. It is this study that is fundamental for making this diagnosis.
- MRI of the brain. Allows you to assess the state of the blood supply to the brain, identify areas of leukomalacia, ischemic foci, post-hypoxic cysts - that is, those complications that could result from a violation of trophism.
- X-ray of the cervical spine. Helps identify bone causes of the disease.
Detection methods
Since a thrombus in the jugular vein is a serious pathology, it is advisable to diagnose it in the initial stages. True, it’s quite difficult if he doesn’t make himself known in any way. But, if you still have some suspicions, it is better not to refuse to visit the doctor.
READ MORE: Treatment of spinal scoliosis in Volgograd
In order to detect a blood clot, modern instrumental and laboratory research methods are used:
- Ultrasound of the area where the jugular vein runs.
- Duplex scanning of vessels, which will allow you to examine possible pathologies of the veins in a two-dimensional image.
- MRI – makes it possible to examine in detail centimeter by centimeter the area under study.
- Thrombodynamics is a study that allows you to identify blood clotting indicators.
- Thrombosis time tests – aimed at assessing the extrinsic clotting pathway.
- Thromboelastography. With this study, the doctor receives a complete picture of the elastic properties of blood clots.
Since thrombosis of the veins of the upper body is rarely complicated by thromboembolism, treatment is predominantly conservative. The patient does not have strict bed rest, but physical activity should be prohibited. The following treatment methods are used:
- Taking direct anticoagulants - Heparin, Fibrinolysin, Fraxiparin. In the acute stage of the disease, these drugs are administered intravenously in the hospital. The course of therapy with these drugs continues until fibrinogen disappears in the plasma and until the level of the prothrombin index normalizes. Subsequently, indirect anticoagulants are prescribed, for example, Aspirin Cardio, Cardiomagnyl.
- Taking or administering nicotinic acid to activate blood thinning and blood clot resorption.
- The use of venotonics - Detralex, Troxevasin, Aescusan, Glivenol. These drugs are needed to speed up metabolism in the walls of the veins, relieve inflammation and relieve pain.
- Introduction of antispasmodics to relax the muscle wall - No-Shpa, Papaverine.
- Local application of heparin ointment, troxevasin ointment for additional effect on the vessel walls.
Surgery for jugular vein thrombosis is extremely rare. As a last resort, minimally invasive techniques are used - percutaneous endovascular thrombolysis, transluminal aspiration thrombectomy. These methods involve dissolving the clot. or its removal using a balloon catheter. It is imperative to influence the factors that led to the development of the disease, for which you should eliminate bad habits and undergo cancer treatment in a specialized hospital.
How to treat vertebral artery syndrome? ↑
Therapy for the disease must be comprehensive.
This is the only way to achieve effect.
Wearing a Shants collar for this pathology is mandatory.
It includes taking the following medications:
A set of exercises should be selected by a doctor individually, since excessive activity can only cause harm, as well as physical inactivity.
So, the following movements can be used:
- The assistant places his hand on the forehead, the patient must press on it. The back pressure should be small at first and increases over time.
- Counterpressure from the assistant's hand is applied to the back of the head.
- Light and careful turns of the head to the sides with a gradual increase in amplitude.
- Back pressure on the sides of the head. Initially, such exercises are performed with the patient lying down, then sitting. The pressure force should increase.
- Shrug.
- Nodding.
- Tilts of the head to the sides.
It is prescribed starting from the subacute period of the disease.
Its main goal is to relax tense neck muscles, which will help reduce compression (squeezing) of the vertebral arteries.
Unprofessional implementation of massage techniques can lead to the development of very serious and life-threatening complications: pulmonary embolism, complete compression of neck vessels with the development of syncope, or even stroke.
In case of ineffectiveness of drug and physiotherapeutic treatment, as well as when the arteries are compressed by osteophytes, tumors, surgical treatment cannot be avoided.
Such operations are carried out in neurosurgical departments: osteophytes, pathological bone and non-bone formations are removed.
A separate type of operation, periarterial sympathectomy, can also be performed.
Therapy includes performing a set of exercises and medications prescribed by a doctor.
There are no effective folk methods for treating this pathology.
It includes the following techniques:
- wearing a Shants collar;
- osteopathy;
- therapeutic exercises, including NISHI exercises;
- autogravitational therapy - traction, which should only be used by qualified specialists;
- manual therapy;
- massage;
- physiotherapeutic methods of treatment: magnetic therapy, phonophoresis with hydrocortisone, diadynamic currents.
Acupuncture or electrophoresis, as well as taking any medications, are contraindicated during pregnancy.
Treatment
Therapy is carried out using conservative and surgical methods in combination. Individually they are ineffective.
Apart from blockage of small vessels and superficial structures, then you can resort to the use of exclusively pharmaceutical agents.
Among the medications for therapy:
- Antithrombic. Dissolve the abnormal formation. Streptokinase, Urokinase. In an adequately high dosage.
- Anticoagulants. Thin the blood. Restore its fluidity. Aspirin Cardio or standard acetylsalicylic acid, Heparin.
- Relief of spasm of arteries and veins. Pentoxifylline, Papaverine, Drotaverine.
- Phlebotonics to normalize vascular flow. Troxerutin, Detralex, Venarus and analogues.
- Anti-inflammatory non-steroidal origin. Nimesulide, Ketorolac.
Among the surgical techniques:
- Mechanical removal of a thrombus with excision of the vessel.
- Elimination of a segment of the affected artery or vein.
- Amputation of part of the intestine or limb (at the onset of necrosis).
- Endovascular surgery using a trap catheter and implantation of a filtering device (vasa filter) to prevent further movement of the clot along the bed.
Treatment of thrombosis is mixed, drug and surgical effectiveness varies from 20 to 90%.
Prevention ↑
Preventive measures are as follows:
- Perform exercises for the neck and shoulder girdle every hour: raise and lower your shoulders, gently move your head in different directions, perform exercises with counterpressure with your own palm. This is especially important for those who work in a sedentary position.
- Sleep on an orthopedic pillow in any position, just not on your stomach, and not in a position with your head thrown back.
- Take neck and collar area massage courses once a year – six months.
- Treatment in sanatoriums specializing in neurological diseases.
It is important to remember that vertebral artery syndrome and alcohol are incompatible things.
With this syndrome, the blood supply to a part of the brain is already impaired, and alcoholic drinks will further intensify the brain steal syndrome.
Neoplasms in the neck: treatment of tumors in the neck
What can cause such a phenomenon as the presence of a tumor in the neck? The reasons vary. And the neoplasms themselves can be benign or malignant, but treatment is prescribed each time purely individually.
Below we will look at the main types of formations in the neck area, and in what cases this phenomenon occurs.
Causes of tumors on the neck
This phenomenon may be due to the following:
- injuries If you are sure that a formation on the neck is the result of an injury, bruise or other mechanical impact, then the problem should be looked for internally;
- infections and viruses. The presence of a formation on the left and right sides may be the result of an infectious infection, and this can cause inflammation in the area of the lymph nodes. If viruses are attached, this provokes breathing problems, the lymph nodes become enlarged and the throat hurts. This may be a symptom of a sore throat, acute respiratory viral infection or flu. Treatment consists of getting rid of the underlying disease;
- anatomical features of the neck structure. The cervical region includes the esophagus, larynx, muscles, nerves, spine, lymph nodes, thyroid gland and blood vessels. If there is a disease in the area of each of these parts of the department, a tumor of the head or neck may appear. And to determine the localization, complex diagnostics is required;
- lymphocytic leukemia, mumps or mononucleosis. They provoke swelling of the neck on the left and right sides. These diseases are infectious in nature, the lymph nodes are also affected.
Types of tumors in the neck area
Formations on the neck have the following varieties:
- according to the place of occurrence - organ and extraorgan. The first occur in organs in the neck area; they are often malignant in nature and retain the structural elements of a normal organ. But extraorgan phenomena can be malignant or benign and originate from muscle or nervous tissue;
- by origin - primary and secondary. The former are not the result of the growth of metastases, and the latter are tumors of the lymph nodes in the neck during metastasis of cancer of any organ;
- according to the characteristics of their course - benign (slow growth without metastases) and malignant (aggressive and fast-growing neoplasms).
Characteristics of benign tumors on the neck
Below is a detailed description of benign tumors in the neck area.
Papillomas and their characteristics
Papillomas are a disease characterized by small growths. They have the following symptoms:
- develop on the basis of the surface epithelium;
- have a black-brown or pale color;
- formation grows on the base or on a thin pedestal;
- has a rough structure and can become keratinized;
- older people are more prone to papillomas;
- they grow slowly;
- when the inflammatory process occurs, there may be pain;
- may develop into cancer upon presentation.
Papillomas in the neck area become malignant only when they are exposed to mechanical or chemical influence. In most cases, papillomas on the neck are only simple.
Pigmented formations that can provoke melanoma stand apart. They are treated with laser method.
Lipoma and symptoms
This formation grows from adipose tissue. It often appears on the neck or head. The key symptoms of lipoma are:
- can be located on the head in front or behind in the occipital area, sometimes on the right side;
- sometimes they touch the hairline;
- may appear in the anterior part and imitate a bird's crop;
- lipomas are sometimes very large, often resembling a hump at the back of the neck;
- lipomas on the neck most often do not have capsules;
- They are predominantly characterized by a soft consistency; in some cases, such formations are dense or elastic;
- they are smooth to the touch. Shine in the sun;
- mobile and painless.
The treatment for these formations is their removal. Since the lipoma does not have a defined frame, it can be difficult to remove it entirely. Large size can cause changes in muscle structure, which causes pain. The disease may recur.
What is fibroma?
Fibroma is a benign tumor that develops on the basis of connective tissue. It is recognized by the following symptoms:
- appearance on the left and right side of the neck;
- the nature of the formation can be nodular or diffuse;
- nodular fibroids are smooth and located under the skin. The structure may be densely lumpy;
- fibroids are mobile upon palpation;
- may have different sizes;
- fibroids that are dense in structure are often larger than soft ones;
- homogeneous internal consistency;
- with a fatty admixture, such tumors on the neck are called fibrolipoma;
- Diffuse formations have clear outlines, form in the capsule and can grow into other tissues. This indicates an invasion;
- fibromas can appear both in the organs of the neck and on its surface;
- tend to compress blood vessels and cause pain, as well as restriction of mobility.
Fibroma can be diagnosed at the initial stage, and treatment in this case can take place without pain and quickly enough. To make a sure diagnosis, a puncture of the tumor is performed. Treatment is a surgical method using radiography.
Neuromas: what are they?
Neuroma is a rare form of tumor that is formed on the basis of the internal nerve fibers of the neck. Often they are saturated with fibrous content, in which case they are called neurofibromas.
These tumors grow in the upper cervical spine. Characteristic mainly for people of mature age and characterized by the following symptoms:
- sensitivity and slow growth of formation;
- tumor shape - oval;
- smooth surface and dense structure of the neuroma;
- it can become very hot and pulsate, causing pain;
- The pulse may slow down when pressure is applied to the tumor. The symptom is rare;
- When a neuroma penetrates the brachial plexus, shooting pain appears.
Neuromas are often confused with lymphadenitis, homodectomas and metastases. The doctor prescribes treatment only after an accurate diagnosis. And it is diagnosed on the basis of histological examination. If the tumor is benign, the patient is sent for surgery, where it is removed.
Lymphangioma and its symptoms
This type of benign tumor is formed on the basis of lymphatic vessels. This results in a large accumulation of lymph and can develop on the sides of the neck. Symptoms of the tumor are:
- soft and elastic consistency;
- when pressed, the tumor shrinks in size;
- does not cause pain;
- the size of the tumor is insignificant.
Treatment involves removing the tumor itself and partially healthy tissue that surrounds it.
Common symptoms of the disease
Thrombosis of the internal jugular vein in the neck is manifested by a huge number of symptoms. The main symptoms are caused by processes in those places where pathological changes occur. Symptoms may depend on the extent of the blood clot blocking the vessel. If a small blood clot is concentrated in a vein, then most often the patient does not even suspect his problem, since the disease does not manifest itself in any way.
With a large blockage of the vessel, the first sign of a problem is the occurrence of severe pain in the area of the collarbone, shoulder and neck. The pain is usually aching in nature and can also be observed in the arms. All this only complicates the diagnostic process, since it is difficult to determine the only location of the thrombus.
Often there is swelling in the neck, which quickly increases in the first few hours. Often the disease manifests itself in the form of rashes on the neck and collarbone. This process is accompanied by bulging veins even without singing or screaming. When touching the neck, the patient feels severe pain. There is also limited hand mobility and hypotonia of muscle tissue.
The above symptoms are observed exclusively in patients with the acute stage of thrombosis. After this period, a subsiding stage begins. But if it never begins, then the disease becomes chronic. In this case, the patient experiences pain constantly. If you notice such problems, be sure to seek help from a specialist, otherwise the consequences can be disastrous.
Causes
The spinal artery begins under the collarbone and reaches the transverse space of the 6th vertebra of the neck. It passes through the openings of the vertebrae of the neck and enters the cranial region through a large opening in the back of the head. The two cervical arteries provide one third of all arterial blood access to the brain. The occipital regions of the brain and its trunk are fed through them. This explains the appearance of symptoms in vertebral artery syndrome.
Taking into account the fact that these arteries interact not only with the spine, but also with the soft tissue around it, the syndrome and its symptoms can develop for various reasons. The reasons can be divided into two groups:
- Pathological changes in the spine - in such a situation the syndrome is called vertebrogenic. This occurs against the background of degenerative changes in the intervertebral discs and vertebrae, curvature of the cervical spine;
- Other causes (non-vertebral symptoms). The problem here is already in the work of the arteries themselves, their athersclerosis or congenital disorders of the vascular system.
On the left side of the neck, vertebral artery syndrome appears much more often than on the right. The reason is that the artery on the left arises directly from the aortic arch, so it is more often affected by atherosclerosis or an abnormality of the extra rib in the cervical spine on the left. The most common source of symptoms of cervical artery syndrome is:
- Arthrosis of the intervertebral joint between the 1st and 2nd vertebrae;
- Kimmerly Pathologies;
- Abnormally high located tooth-like growth of the 2nd vertebra of the neck;
- An unusually large distance between the vertebral artery and the artery under the collarbone;
- Tension of the oblique cervical muscles.
You risk getting cervical artery symptoms if you move your neck suddenly. When an artery is pinched, its choroid is deformed.
Pressure from a herniated disc
- 1 What is a hernia?
- 2 What are the symptoms of a hernia in the cervical spine?
- 3 How does pressure affect the mechanism of development of the problem?
- 4 What to do?
Scientists have proven that blood pressure is affected by disorders in the cervical spine. A common disease of the spine is osteochondrosis. Almost 80% of people suffer from this disease starting from the age of 20. The disease is characterized by the presence of complications, but the most dangerous is a herniated disc.
What is a hernia?
Between the vertebrae there are peculiar “pillows” that act as shock absorbers - intervertebral discs, which make the spinal column flexible and strong, and compensate for vibrations and shocks during movement. The discs are composed of a hard outer tissue (annulus fibrosus) and a semi-fluid inner tissue (nucleus pulposus). When the annulus fibrosus ruptures, the nucleus pulposus is displaced outside the disc. This displacement is called a hernia. The disc bulges and becomes like a compressed balloon.
on
Almost always, a hernia is preceded by osteochondrosis - a degenerative-dystrophic change in the structure of the intervertebral disc. Other causes include kyphosis, scoliosis, lordosis and various spinal injuries. The disc is nourished by the deep muscles of the back, as it lacks blood vessels. With insufficient physical activity, the discs do not receive enough nutrients. Therefore, the fibrous ring can rupture even with insignificant load on the spine.
Return to contents
What are the symptoms of a hernia in the cervical spine?
Sudden pressure surges can be caused by a hernia.
Often a person experiences pain in the neck, which is accompanied by a crunching sound that intensifies when the head is rotated or tilted. Often the pain radiates to the arms, shoulders, under the collarbone, scapula and intensifies when raising the arms up. Such symptoms most likely indicate a hernia in the cervical spine. Pain occurs even with a small hernia size - 3 mm. The tumor compresses the spinal cord membrane or nerve, which causes pain. Often the root cause of migraines and chronic ischemia is a hernia in the cervical spine. Also, the formation of a hernia is accompanied by the following symptoms:
- a sharp decrease or increase in blood pressure, and the difference in values often reaches 50-60 mm Hg;
- dizziness, nausea, fainting;
- attacks of headache;
- muscle weakness and numbness of the hands;
- short-term visual and hearing impairment.
Return to contents
How does pressure affect the mechanism of development of the problem?
A herniated cervical spine partially or completely compresses the vertebral artery, which impairs cerebral circulation. The brain lacks oxygen, and the vessels “look” for a way to improve blood flow. The area responsible for pressure is the medulla oblongata, which in this case gives the command to increase blood pressure. The arteries dilate and the pressure rises. Less commonly observed is a decrease in blood pressure. This occurs when the body is unable to solve a circulatory problem by increasing the speed of blood flow. Then the body artificially “freezes” the system, reducing the oxygen consumption of brain cells. With a cervical hernia, pressure fluctuations are abrupt and often insignificant. Therefore, the patient often does not pay due attention to pressure surges, triggering his disease.
Return to contents
Drug treatment
The basis of therapy for the formation of blood clots in the circulatory system is the use of direct and indirect anticoagulant drugs. They are aimed at thinning the blood by reducing the level of fibrinogen, a substance whose concentration increases to form clots.
Direct anticoagulants include:
- Fibrinolysin,
- Fraxiparine,
- Heparin.
After a decrease in the prothrombin index, they switch to medications with an indirect anticoagulant effect, such as Curantil or Aspirin.
Another important aspect in complex therapy is the prescription of phlebotonics, whose action is aimed at improving metabolic processes and eliminating inflammation.
Remember! The dosage of any medications and the method of their use are prescribed exclusively by a competent medical professional.
If necessary, antispasmodics are prescribed to reduce the tone of the vascular walls and relieve pain. The addition of sepsis indicates the need for antibacterial therapy.
You can find out what varifort for varicose veins is and the opinion of Elena Malysheva from our article.
Danger of jugular vein thrombosis
Jugular vein thrombosis rarely leads to the development of pulmonary embolism, although such cases have been reported. In the absence of treatment, sepsis and papilledema may develop. Postthrombophlebitic syndrome is fraught with destruction of vascular valves and the development of venous stagnation, which is manifested by swelling of the arms and legs.
Timely access to medical care allows you to avoid the development of dangerous consequences. With adequate therapy, the prognosis is favorable, complete recovery occurs within 3-6 months.