The role of lymphocytes in the body
Lymphocytes are found in large numbers in the blood, lymph and lymphoid tissues, which include the thymus, spleen, lymph nodes, Peyer's patches of the intestine, tonsils and adenoids.
The main function of lymphocytes is to protect against foreign information represented by RNA (ribonucleic acid) or protein, which can enter the body with bacteria, viruses, fungi and parasites.
Thanks to the immune system, these pathogens foreign to the child’s body are inactivated and destroyed. It is very important that the immune system is activated only to substances that are foreign to the child’s body.
In some cases, children may experience autoimmune reactions, where the immune system is activated and begins to destroy the body's own proteins or cells. Unfortunately, these autoimmune attacks are sometimes fatal.
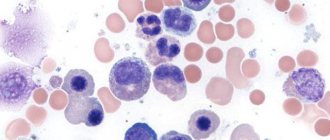
Lymphocyte: scanning with an electron microscope
In response to the penetration of a foreign substance (antigen) into the body, the immune system is activated, which is characterized by two types of immune responses.
- Humoral. The result of this response is the synthesis of immunoglobulin antibodies, which are proteins that interact with antigens entering the body.
- Cellular. The name itself implies the meaning of this immune response, which is that in the body, in response to an antigen, specialized cells are formed that also destroy the antigen. Macrophages play a major role in this process.
Thanks to the “immunological memory” of our immune system, after some viral or infectious diseases have been suffered, the body becomes protected from this pathogen when it is reintroduced.
However, if the virus is subject to modification, for example, the influenza virus, then lasting lifelong immunity does not occur. Each time a new virus enters the body, carrying a new antigen protein, to which the body is forced to react again.
Lymphocytes are formed from pluripotent stem cells, which are also the precursors of all blood cells: red blood cells, white blood cells and platelets. In the fetus, these stem cells are located in the liver, and in the child they are localized in the red bone marrow, where the formation of blood cells occurs. Some cells enter the blood and are transported to the thymus, where their numbers increase and they differentiate into mature lymphocytes.
The thymus and red bone marrow belong to the central lymphoid organs. Of these, lymphocytes migrate to peripheral lymphoid tissues: the spleen, lymph nodes, Peyer's patches of the intestine and tonsils. In these tissues they can interact with the antigen, destroying it. In peripheral lymphoid tissues, T lymphocytes and B lymphocytes are found in different areas.
Lymphocytes constantly circulate in the blood and lymph and can pass from blood to lymph and back, thus connecting these two physiological fluids of the body. According to their functions, lymphocytes are divided into three groups.
- B lymphocyte
B lymphocytes. They make up from 8 to 20% of the total number of lymphocytes and develop independently of the thymus, producing antibodies (immunoglobulins) that initiate the destruction of foreign microorganisms with the help of leukocytes (phagocytes) and complement (blood protein system).
- T lymphocytes. These lymphocytes receive information in the thymus, and therefore are called thymus-dependent. Their amount in the blood varies from 60 to 80%. They are responsible for cellular immunity, recognizing antigen, and are represented by three subgroups: T-killers. They are “killer” cells and require antibodies to activate them;
- T-helpers. They secrete lymphokines (interleukins), substances that are activators of leukocytes. For example, such a lymphokine is macrophage migration inhibiting factor (MIF). It is an inducer of macrophages (monocytes), which, after activation, phagocytose (absorb and destroy) microorganisms;
- T-suppressors. They inhibit (suppress) the activity of other lymphocytes, stopping their interaction with the antigen. There is a close functional relationship between T-suppressors and T-helpers.
Treatment
Since lymphocytosis is the body’s reaction to a pathological process occurring in it, treatment consists of eliminating the root cause that caused the increased production of cells. A lot of leukocytes in the blood is evidence of the presence of a viral disease and an associated bacterial infection. In this case, a course of antibiotics is usually prescribed.
- In acute respiratory infections or acute respiratory viral infections, the immune system must actively fight pathogens. If lymphocytosis is observed at the same time, it means that the body itself effectively destroys foreign microorganisms. The course of treatment should be aimed at helping him suppress the disease, and after recovery, the level of lymphocytes will return to normal.
- In cases of serious pathologies, leukemia or myeloma, more radical measures will be required. Often the only option is chemotherapy and bone marrow transplantation.
Normal blood lymphocyte count in children
T lymphocyte
Only 2 to 4% of lymphocytes circulate in the peripheral blood of healthy people, the remaining 96-98% are in peripheral lymphoid organs. In the blood of a healthy child, lymphocytes circulate in the following ratios:
- T lymphocytes: 60-80%;
- B lymphocytes: 9-20%;
- NK lymphocytes: 4-19%.
In young children, the immune system is imperfect, therefore, lymphocytes play an important role in protecting their body from infection. As the child’s immune system develops, their number also changes. The dynamics of these changes are presented below.
Table - Norm of lymphocytes in children
| Age | Lymphocytes in blood, % |
| Newborns | 15-35 |
| 1st week | 22-50 |
| 1-6 months | 45-70 |
| 6-12 months | 45-65 |
| 1 year | 37-60 |
| 2 years | 33-35 |
| 3 years | 30-54 |
| 4-7 years | 29-50 |
In absolute units, in the first week a newborn’s blood level of lymphocytes ranges from 2.1 to 9.0 x 109/l. In a 1-2 year old child their number reaches 3.1-10.0 x 109/l, and by 6-7 years it decreases slightly to 1.9-5.0 x 109/l.
To assess the child’s health and the activity of his immune system, healthy children are recommended to have a blood test done once a year. If a child has a chronic disease, then it is necessary to donate blood for analysis several times throughout the year.
What protects a child from disease?
Entering this world from the sterile conditions of the mother's womb, the child encounters a numerous world of microorganisms.
View gallery His acquaintance with the smallest representatives of life forms begins with his first breath. For a baby’s sterile body, every microorganism poses a threat. But, fortunately, nature took care of the defenseless creature, rewarding it with powerful protection - immunity. The immunity of a newborn depends entirely on its mother. It is the mother who is able to provide powerful protection to the child’s body along with the first drops of milk. This is how nature intended it, and no one can think of or invent anything better.
But a child is not able to resist all the microorganisms that come across his life. As a result of such a meeting, diseases arise. If we detect symptoms of illness in a child, we rush to contact a specialist - a pediatrician. After carefully examining your child, the doctor will recommend a blood test to get a complete picture.
Increased lymphocyte count
If lymphocytes are increased in a child’s blood compared to the norm corresponding to the child’s age, then this is called lymphocytosis. Lymphocytosis is of two types: relative and absolute.
- Relative lymphocytosis. The child has an increase in the percentage (relative) number of lymphocytes, without changing their total number. There may be an imbalance in the lymphocyte/leukocyte ratio if the child, for example, has a purulent focus. The migration of leukocytes to the site of inflammation leads to a decrease in their number in the bloodstream, as a result of which relative lymphocytosis is observed. The cause of relative lymphocytosis, i.e., a high level of lymphocytes in the blood of a child, may be the following diseases: purulent inflammation;
- flu;
- long-term diseases that cause weakened immunity.
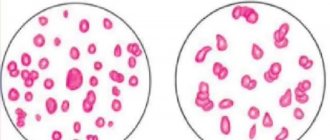
- Left: Human blood smear. 1 - red blood cells, 2 - small lymphocyte, 3 - medium lymphocyte. Right: Electrogram of lymphocytes.
whooping cough;
measles;
Sometimes, based on the nature of the course, experts divide lymphocytosis, when lymphocytes in a child’s blood are increased, into reactive and malignant.
- Reactive lymphocytosis. It is characterized by an active reaction of the immune system to any disease, for example, whooping cough, viral hepatitis, etc. As a rule, this type of lymphocytosis is observed for no more than 30-60 days.
- Malignant lymphocytosis. It is a consequence of a lymphoproliferative disease: lymphocytic leukemia, lymphosarcoma.
What you need to know about lymphocytosis
- In order to determine whether a child is sick, it is necessary to do a blood test and contact a pediatrician. In some cases, in addition to consulting a pediatrician, it may be necessary to consult a hematologist.
- If necessary, the doctor may recommend additional laboratory tests that will identify pathogenic microflora, i.e., the cause of the disease, in order to prescribe appropriate medications to which this microflora is sensitive.
- Sometimes the doctor may additionally prescribe ultrasound, x-rays, red bone marrow cytology and other diagnostic methods.
- If a child's lymph nodes, spleen or liver are enlarged in combination with lymphocytosis, it is necessary to consult an oncologist.
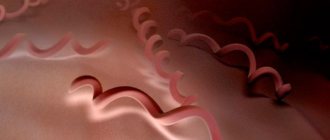
The lymphocyte is surrounded by red blood cells
Causes of lymphopenia
A decrease in the number of lymphocytes in the blood is called lymphopenia. Situations in which a decrease in the number of lymphocytes occurs can be divided into 2 groups:
- A large number of lymphocytes died in the fight against some pathogenic factor, and the blood was taken before new cells entered the blood.
- The organs responsible for the production of lymphocytes are affected by some disease (lymphoma, lymphosarcoma, a consequence of chemotherapy, etc.).
Diseases and conditions accompanied by lymphopenia:
- ARVI.
- Infectious mononucleosis.
- Tuberculosis.
- Viral hepatitis in the late stage.
- Congenital or acquired immunodeficiency (AIDS, congenital Bruton agammaglobulinemia, etc.).
- Malignant diseases: lymphogranulomatosis (Hodgkin's disease), acute and chronic lymphocytic leukemia, lymphosarcoma, paraproteinemic hemoblastoses, heavy chain disease, etc.
- Taking steroidal anti-inflammatory drugs (prednisolone).
- Taking cytostatics (for example, methotrexate).
- Radiation therapy and chemotherapy.
- Diseases of the endocrine system (Itsenko-Cushing's disease, adrenal insufficiency, hypothyroidism, etc.).
Reduced quantity
Just as in the case of lymphocytosis, when calculating the number of lymphocytes, the age of the child is taken into account. If lymphocytes are low in a child’s blood, this indicates lymphocytopenia, which can be relative or absolute.
- Relative lymphocytopenia. It means a decrease in the percentage of lymphocytes when they are normal in the blood. It can occur in diseases accompanied by an increase in the number of leukocytes (neutrophils) in the blood, such as: acute or chronic pneumonia;
- pathologies in which foci of purulent inflammation occur.
- lupus erythematosus;
If you have a question about whether your child is sick, you need to take a blood test as soon as possible and seek advice from a pediatrician.
What you need to know about lymphocytopenia
- After an infectious disease, the number of lymphocytes normalizes.
- If a child has a chronic deficiency of immunoglobulin (IgG), then the administration of this protein is contraindicated.
- In case of congenital immunodeficiency in a child, a stem cell transplant is recommended.
What is a complete blood count and what does it include?
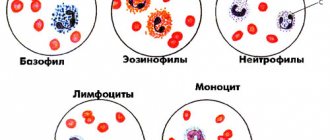
A general blood test in children allows you to detect the disease in the early stages, assess the state of the immune system, and determine inflammatory processes. Often the doctor pays attention to the MID and ratios of other blood cells. MID or MXD - the number and percentage of different types of leukocytes: eosinophils, monocytes, basophils. In addition, using OAC, you can monitor the effectiveness of therapy.
A blood test is done by piercing the child's ring finger with a special disposable instrument - a scarifier. Afterwards, using a pipette, the laboratory assistant draws blood from the capillaries into a test tube and sends it for examination. This includes:
- determination of the number, size and shape of blood elements;
- calculation of hemoglobin content in the blood;
- determination of the average hemoglobin coefficient per red blood cell and calculation of the color index;
- fixing the relationship between plasma and formed elements;
- calculation of erythrocyte sedimentation rate - ESR.