© Author: Z. Nelly Vladimirovna, laboratory diagnostics doctor at the Research Institute of Transfusiology and Medical Biotechnology, especially for SosudInfo.ru (about the authors)
Normoblasts (normocytes) are the last, still nuclear, stage of red blood cells (erythrocytes) on the way to an adult, full-fledged state. At this stage, normoblasts have a nucleus, so that, having lost it, they can turn into a young, nuclear-free cell containing hemoglobin and already capable of performing the main task of red blood cells (participation in respiration).
Before becoming normoblasts, future red blood cells go through a certain path. As is known, all blood elements originate from a stem cell - it is the ancestor of future leukocytes, platelets, erythrocytes, etc., since it gives rise to several sprouts, among which is the erythrocyte (from it will come the cells of the erythroid series, including, and those of interest to us are normoblasts).
The youngest, morphologically distinguishable cell of the red row is the erythroblast, which was previously called proerythroblast. This is a fairly large cell (14 - 20 microns), containing an equally large nucleus, but does not even have signs of what an adult red blood cell is so valued for - it does not contain hemoglobin.
Normal blood level is zero
Normally, these cells are not found in the blood, so there can be no talk of increased values of normoblasts when studying preparations (the norm is 0). They may or may not exist, and then it’s time to count if they can be detected. The exception to these rules is newborn children.
In a child in the first days of life, their presence in a general blood test should not be surprising: the increased content in the bone marrow and the appearance of normoblasts in the blood is explained by the increased production of erythropoietin during this period, which leads to an increase in red blood cells and hemoglobin. A few days later, when erythropoietin production decreases, the values of these indicators also drop down.
After some time from birth, more precisely, between 2 and 3 months of life, the child again experiences an increased level of normoblasts and reticulocytes, again due to increased synthesis of erythropoietin, which does not cause concern for pediatricians, because this process is physiological.
After this surge, the child’s norms for these indicators will begin to approach the adult norms more and more every month, therefore, normoblasts will also not be found in children’s blood products, but will begin to be detected, as they should be, only in the myelogram.
normoblasts released from the bone marrow into the blood
Their absence in the blood, however, does not exclude their diagnostic significance, because they do not appear just like that, but due to some pathological changes, one way or another, affecting the main hematopoietic organ - the bone marrow.
Since the word “blast” means “sprout,” all descendants of blast can no longer be considered sprouts, so it would be more correct not to apply this name to further forms, but to attach the ending “cyt” to them. In this regard, the outdated word “normoblasts” is present in the vocabulary of specialists with extensive experience only out of habit, while young doctors already call this cell a normocyte.
From birth to great achievements
However, by focusing on the names, we have deviated somewhat from the topic. So, the events take place in the bone marrow:
Stage 1: erythroblast
The erythroblast is the first cell that can be identified under a microscope in a bone marrow specimen. A rounded nucleus, a delicate mesh structure of chromatin, several small nucleoli (usually 2 - 4), no clearing around the nucleus yet - this is the morphology of the ancestor of cells that will later become erythrocytes. In a general analysis of the blood of a healthy person, you don’t even need to look for it, since it simply cannot be there, because it has only just arisen and, before it goes “out into the world,” it must acquire new features and qualities in order to become workable in the peripheral blood, and, therefore, useful.
Stage 2: pronormocyte
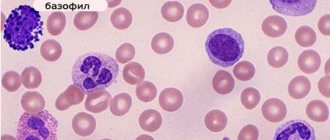
Having passed the erythroblast stage, a very young cell slightly reduces its size (10 - 15 microns) and begins to change the structure of the nucleus, so that later it is easier to get rid of it (the nucleus becomes smaller and coarser, the nucleoli disappear, a slight perinuclear clearing appears around the nucleus) - this is no longer erythroblast. The new cell is called a pronormocyte in a new way, although some continue to call it in the old way - a pronormocyte. At this stage, the cell of the erythroid series is very poorly differentiated in the myelogram, because it has not yet completely lost the features of its predecessor, and has not yet acquired new ones.
Stage 3: normoblast (normocyte)
However, very little time passes before the “hero of our story” appears from an unrecognizable cellular structure - a normoblast or normocyte. It begins to be saturated with hemoglobin, which first concentrates around the nucleus (basophilic normocyte), and then spreads to the entire cytoplasm, turning the cell into a polychromatophilic normoblast, that is, the cell is clearly preparing to perform its responsible function.
As normoblasts accumulate complex chromoprotein (Hb), the need for the nucleus disappears; it only prevents the accumulation of hemoglobin by its presence. Having received a sufficient amount of Hb, the normocyte becomes oxyphilic: the cytoplasm spreads over almost the entire territory, the nucleus loses its significance, therefore it becomes very small (pyknotic), coarsened with a structure changed beyond recognition, reminiscent of a cherry pit.
Stage 4: birth of a red blood cell
A normoblast, which is about to get rid of a nucleus that is no longer needed, remains a normoblast for some time, but in small numbers. Having finally pushed out the nucleus, the cell turns into a “newborn” polychromatophilic erythrocyte, retaining a small amount of hereditary information (RNA), which will finally leave the cell within 24 hours, although it is difficult to call the “newly formed” form a cell (rather, also out of habit).
Young red blood cells, saturated with hemoglobin and having lost their last connection with their “homeland,” are called reticulocytes, which very soon, after arriving in the bloodstream (up to 48 hours), will lose the last thing that emphasizes their young age - reticulum, and turn into full-fledged adult blood cells - erythrocytes. A special stain helps detect reticulocytes in the blood. The entire path traveled by an erythrocyte from an erythroblast to a cell that has lost its nucleus takes at least 100 hours.
It is obvious that normally red cells at the normoblast level (before it becomes a reticulocyte) do not appear in the blood of a healthy person of all ages.
Anemic syndrome
Anemia is a condition characterized by a decrease in the amount of hemoglobin per unit volume of blood, often with a simultaneous decrease in the number of red blood cells. Anemia is considered to be a decrease in hemoglobin in the blood less than 100 g/l, erythrocytes less than 4.0 × 1012/l and serum iron less than 14.3 µmol/l. The exceptions are iron deficiency anemia and thalassemia, in which the number of red blood cells is normal.
There are different classifications of anemia:
- Based on the morphology of erythrocytes, anemia is divided into microcytic, normocytic and macrocytic. The main criterion for this division is the average erythrocyte volume ( SEA
):- microcytosis - SER less than 80 fl.,
- normocytosis - SES - 80-95 fl.,
- macrocytosis - SER more than 95 fl.
- Hypochromic and normochromic anemias are determined by the degree of hemoglobin saturation. The second part of the term, “chrome,” refers to the color of the red blood cells.
In accordance with these classifications there are:
- hypochromic microcytic anemia (small, pale red blood cells; low SES);
- macrocytic anemia (large red blood cells; increased SER).
- normochromic normocytic anemia (cells of normal size and appearance, normal SES).
According to the severity of anemia there are:
- mild degree (hemoglobin 91 - 119 g/l),
- moderate severity (hemoglobin 70 - 90 g/l),
- heavy (hemoglobin less than 70 g/l).
There is a pathogenetic classification of anemia:
- Anemia caused by impaired hemoglobin synthesis and iron metabolism, characterized by microcytosis and hypochromia (iron deficiency anemia, anemia in chronic diseases, sideroblastic anemia, thalassemia).
- Anemia caused by impaired DNA synthesis in conditions of vitamin B12 or folic acid deficiency (macrocytic anemia).
- Normochromic normocytic anemias, which do not have a common pathogenetic mechanism and are divided depending on the bone marrow response to hypoplastic and aplastic, hemolytic and posthemorrhagic anemia.
It should be noted that there are conditions that are characterized by signs of anemia, but are not accompanied by a decrease in hemoglobin or red blood cells, but are manifested by a violation of the relationship between the number of red blood cells and plasma volume (hydremia in pregnancy, overhydration in heart failure, chronic renal failure) and a decrease in plasma volume (dehydration, peritoneal dialysis, diabetic acidosis).
In anemia, the main pathogenetic significance is hypoxia of organs and tissues with the possible subsequent development of degenerative processes. There are compensatory mechanisms aimed at reducing and eliminating the consequences of hypoxia. These include hyperfunction of the cardiovascular system, caused by the effect of under-oxidized products on the regulatory centers of the cardiovascular system. In patients, heart rate and minute volume increase, and total peripheral resistance increases.
Compensatory mechanisms also include: an increase in the physiological activity of red blood cells, a shift in the oxyhemoglobin dissociation curve and an increase in the permeability of the vascular wall to blood gases. It is also possible to increase the content and activity of iron-containing enzymes (cytochrome oxidase, peroxidase, catalase), which are potential oxygen carriers.
The clinic of anemic syndrome is characterized by general anemic complaints of general weakness, dizziness, tendency to faint, palpitations, shortness of breath, especially during physical activity, stabbing pain in the heart area. When hemoglobin decreases to less than 50 g/l, signs of severe heart failure appear.
During the examination, pallor of the skin, tachycardia, a slight increase in the left border of relative cardiac dullness, systolic murmur at the apex, and a “spinning top murmur” in the jugular veins are revealed. An ECG can reveal signs of left ventricular hypertrophy and a decrease in the height of the T wave.
Is normoblastosis a sign of pathology?
The appearance of normoblasts in a general blood test (the word “increased” somehow does not fit - this was mentioned earlier) is a clear sign of pathology in the body. These cells enter the peripheral blood under the following circumstances:
- Anemia of various etiologies (thalassemia), some forms of acute and chronic leukemia. In these cases, it can reach normoblastosis, that is, their values are not just increased - there are a huge number of normoblasts; In addition, these pathological conditions in adults can cause the formation of foci of extramedullary hematopoiesis (liver, spleen), which will also produce their portion of normocytes.
- Massive blood loss - in order to save the body, the bone marrow has no choice but to begin active regeneration of cellular elements;
- In an effort to somehow compensate for the deficiency in the bloodstream, normoblasts leave the bone marrow prematurely with increased destruction of red blood cells (hemolysis) without inhibiting the functioning of the hematopoietic system;
- Acute erythroleukemia (o. erythromyelosis, Di Guillemo's disease) is a rare but malignant disease. The main characteristic feature of acute erythromyelosis is the appearance in the peripheral blood of a large number of erythroid cells that have not lost their nucleus;
- When metastases of malignant tumors spread to the skeletal system, increased concentrations of these cells will be observed in the bone marrow, then they will begin to leave it and enter the peripheral blood. It should be noted that in such cases there is often no direct relationship between normoblastosis and the degree of anemia (significantly increased numbers of normoblasts can be seen in mild anemia);
The sudden appearance of representatives of the young erythroid population in the blood is called a blood crisis, which is characteristic of pernicious anemia. In this case, the appearance of such a sign, on the contrary, is somewhat encouraging, since it is a harbinger of an impending remission. But calm blood in this pathology makes one suspect the low regenerative ability of the hematopoietic organs (aplastic anemia) and expect an unfavorable prognosis.
Sometimes erythroid cells that have not completely passed the normoblast stage leave the bone marrow prematurely due to the person’s serious condition, which is not caused by a pathology of the hematopoietic system. For example, this can happen during various pathological processes occurring with circulatory failure.
Blast cells in a blood test
Blast cells in a blood test indicate the presence of a disease such as leukemia. In medicine, there is a certain division that characterizes the degrees of leukemia. Thus, blast cells in a blood test may be different, but their presence is checked by one examination.
Types of leukemia
In medicine, there are many different forms of this disease. In this article we will look at only some of the most common ones. For example, there is acute leukemia, characterized by a large composition of young blast cells. Therefore, we can say with certainty that up to 55% of all cases develop the myeloblastic form of acute leukemia.
Acute lymphoblastic leukemia is also known, which most often occurs mainly in children. In addition, there is also some division into subtypes. Thus, monoclonal antibodies are used for immunological phenotyping of blast cells. Such features are more important for proper research and for identifying an accurate diagnosis. Therefore, the forms of leukemia are fully taken into account in detail.
As for the symptoms, they do not always coincide with the course of the disease, so it is quite difficult to identify all the features of the disease at an early stage.
Features of the analysis
In order to check the development of the disease, it is enough to take a general blood test, in which the number of red blood cells most often decreases to 1 - 1.5x1012/l. Thus, we can say that anemia is normochromic in nature. A blood test must be checked specifically for normoblasts and their exact number determined. Also, in addition to all this, ESR most often increases, and the number of reticulocytes usually decreases.
As for leukocytes themselves, in the presence of blood cancer, the analysis will always be inconsistent. Indicators most often range from the lowest to the highest. So, for example, from 0.1x109/l to 100 - 300x109/l digits. All numbers fully depend on the course of the disease and its stage. In particular, we are talking about such forms as leukopenic, leukemic and subleukemic.
The youngest cells are detected in peripheral blood in the advanced stage of acute leukemia. These are bone marrow cells and a small number of already mature elements. In this case, they speak of a state of leukemic failure, when there are no transitional forms of cells. The analysis also includes not only blast cells, but also the determination of thrombocytopenia. Within normal limits, it can fluctuate up to 20x109/l.
It is worth noting that with megakaryoblastic leukemia, the platelet level in the analysis is most often significantly higher than normal. To determine blast cells, special procedures are performed for the enzymes alkaline phosphatase, nonspecific esterase and peroxidase. For example, the cytochemical reaction in acute lymphoblastic leukemia is positive for terminal deoxynucleotidal transferase and negative for myeloperoxidase. It is also worth noting that in acute myeloid leukemia the reaction to myeloperoxidase is positive.
Carrying out analysis
No special preparation is required to carry out the analysis. As a rule, this involves taking a small amount of blood from a vein and subjecting it to special processing in laboratory equipment.
It is recommended to carry out the analysis for the first time in the morning on an empty stomach in order to obtain more accurate results. At the same time, it becomes much easier to identify normoblasts and all other abnormal cells. Such an analysis is most often done based on the first symptoms, when a person begins to notice something wrong in his body. For example, acute leukemia manifests itself more severely and quickly than the chronic form of the disease.
Disease cells spread much faster throughout the body, which makes it possible to identify danger at any time. There are many more cases when the disease affects young organisms, especially children. Therefore, as advice for parents, it can be said that it would be useful to regularly conduct such a blood test.
krasnayakrov.ru