Classification
Most often in clinical practice, the Frederickson classification of hypercholesterolemia is used, which is based on the division according to the predominance of one or another cholesterol fraction:
- Type I – increased concentration of chylomicrons (CM).
- Type IIa – increased levels of low-density lipoproteins (LDL).
- Type IIb – high content of low and very low density lipoproteins (VLDL and LDL).
- Type III – increased levels of intermediate density lipoproteins (IDL).
- Type IV – increased VLDL values.
- Type V – high level of VLDL and cholesterol.
Based on its origin, hypercholesterolemia is divided into:
1. Primary
. This form is in turn divided into:
- Polygenic. The most common variety. Caused by a combination of genetic predisposition and exposure to exogenous factors (diet, smoking, etc.).
- Family. Caused by various hereditary disorders of lipid metabolism due to genetic mutations.
2. Secondary
. High levels of cholesterol in the blood, which develops against the background of certain diseases, endocrine disorders, or taking medications.
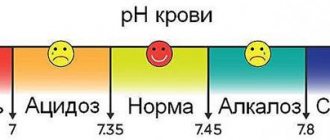
Based on the degree of increase in blood cholesterol levels, the following are distinguished:
- Mild hypercholesterolemia
– from 5.0 to 6.4 mmol/l. - Moderate hypercholesterolemia
– from 6.5 to 7.8 mmol/l. - High hypercholesterolemia
– 7.9 mmol/l and above.
Symptoms, diagnosis and treatment of hypercholesterolemia according to ICD 10 code
Hypercholesterolemia, according to the international disease code ICD 10, refers to diseases of the endocrine system in the group of metabolic disorders.
In numerical terms, the diagnosis is determined when the cholesterol level in the blood serum exceeds 200 mg/dl. This is not yet a disease, but a complex of prerequisites for the probable development of diseases. This is a syndrome that combines lipid metabolism disorders, high cholesterol levels and vascular occlusion, followed by the development of obesity and atherosclerosis.
People at risk for hypercholesterolemia belong to the elderly age sample. This is facilitated by changes in hormonal levels. Until the age of menopause, men are most susceptible to the disease, then the difference between the sexes is leveled out.
Pure hypercholesterolemia has an ICD 10 number: E78.0
It is caused by a large amount of cholesterol (more precisely, the predominance of LDL over HDL) and a symptom complex consisting of disorders in the endocrine system, psychological problems and non-compliance with healthy eating rules.
Causes
Risk factors include heredity, sedentary lifestyle, overeating (leading to excess weight problems) and stress.
Hypercholesterolemia is divided into several forms, each with its own causes:
- Primary form. Occurs infrequently. Its cause is a hereditary factor, namely the receipt from parents of a gene, in the presence of which excessive synthesis of cholesterol occurs and is not restrained by anything. This may be a manifestation of one of the options: a) genetically determined absence of a receptor that serves to bind cholesterol; b) the absence of an enzyme used for the transport of low-density lipoproteins; c) the inability of LDL to penetrate into cells.
The result of the manifestation of the primary form of hypercholesterolemia is the development of cardiovascular pathologies in early or middle age. Early heart attacks are caused by this form of hypercholesterolemia.
- The secondary form of hypercholesterolemia is caused by other diseases that a person has. This is an underactive thyroid gland (can be caused by heredity, surgery or inflammation); diabetes mellitus with impaired carbohydrate metabolism; disorders of the gallbladder and liver; taking medications that affect lipid metabolism.
- Alimentary form. It is completely the result of an unhealthy diet and lifestyle of the patient, when the presence of carbohydrates and fatty animal products in food becomes constant and excessive, and in addition, is combined with physical inactivity. Obesity develops, which in turn increases the content of fat molecules in the bloodstream.
Symptoms
Hypercholesterolemia as a pathology of human health, noted by the ICD, does not manifest itself in any way at the beginning of the development of this condition. It is rarely detected before circulatory problems begin due to increased lipids. Gradually the disease becomes advanced and manifests itself more and more.
Accumulating in the arteries, fat molecules impede blood supply to the brain and lower extremities, which reduces memory, attention, and performance. Xanthomas appear - compactions of a fat-like substance, localized in the area of the tendons and on the fingers of the upper and lower extremities.
Similar deposits, xanthelasmas, also appear on the eyelids. A gray stripe, a “corneal arch,” may appear framing the cornea of the eye.
A clear clinical evidence of advanced hypercholesterolemia is the stage of development of atherosclerosis, stroke and heart attack.
Diagnostics
To determine the diagnosis, the patient undergoes an examination at a medical institution; the doctor at the appointment measures his blood pressure, height and weight.
When collecting anamnesis, the likelihood of familial hypercholesterolemia is determined; in case of doubt, the whole family is examined.
As laboratory tests, it is necessary to study the lipid profile of the patient’s blood to determine the level of high and low density lipoproteins, cholesterol and triglycerides. Exceeding these indicators in all four positions allows us to determine the diagnosis of hypercholesterolemia, a pathological process registered by ICD 10.
Treatment
Treatment measures consist of two necessary components: drug therapy and changes in the patient’s lifestyle, diet and physical activity (gymnastics and regular physical activity, walking are necessary to lose weight and improve blood supply to organs).
Nutrition
Proper nutrition, taking into account metabolism and limiting fats of animal origin, can help eliminate excess cholesterol from the body.
It is necessary to adjust the patient's diet:
- Ensure the predominance of food of plant origin;
- Reduce salt intake;
- Exclude sausages, smoked sausages, lard, and canned food from the menu;
- Eliminate cream, sour cream, butter;
- Refuse products offered by fast food outlets;
- Do not eat white baked goods and sweet baked goods;
- Dose the presence of liver, egg yolks and kidneys in the diet towards a decrease.
Pay special attention to the presence of products on the table:
- Any fish, including limited fatty varieties of sea fish;
- Lean meat in small portions;
- A small amount of nuts;
- Bean products;
- Whole grain porridge;
- Fruits and vegetables contain fiber, which helps reduce cholesterol.
It is preferable to use food products raw; they can also be boiled, baked, steamed and stewed in a small amount of vegetable oil.
Vegetable oil does not contain cholesterol, but limiting its amount is necessary to get rid of excess weight in case of obesity.
Subject to dietary restrictions, cholesterol levels are reduced and the patient’s weight is normalized, which has a positive effect on lipid metabolism.
A small amount of red wine is allowed due to the presence of resveratrol in it, which strengthens the walls of blood vessels and has a vasodilating effect.
Natural herbal remedies, herbs, decoctions and tinctures from them can also help improve the health of the body and reduce cholesterol levels. These are pollen collected by bees, garlic, artichoke extract, apples, flax seeds, flaxseed oil, alfalfa sprouts, linden blossom, milk thistle, green tea.
A separate point is the need to quit smoking and drinking alcohol. When nicotine enters the blood, conditions are formed that aggravate the narrowing of the lumen of blood vessels. According to statistics, among smokers there are three times more patients with hypercholesterolemia than among non-smokers.
Drug therapy
Drug treatment begins with statins. They resort to medications if, after six months of following a diet and following a set of sports exercises, the level of low-density lipoproteins in the body has not decreased.
Statins (Atorvastatin) act as anti-inflammatory drugs while reducing cholesterol levels in the blood. They interfere with its synthesis.
In addition, bile acid sequestrants are used, which counteract the synthesis of cholesterol in the blood plasma and have very few side effects.
Fibrates prevent the accumulation of triglycerides in the blood.
For liver diseases, many medications are contraindicated, and to normalize the amount of triglycerides, doctors prescribe Omega-3 polyunsaturated fatty acids.
Familial hypercholesterolemia is treated using plasma filtration and lipoprotein immunosorption techniques.
Prevention
Preventive measures logically continue the recommendations for therapeutic nutrition and maintaining a healthy lifestyle:
- Elimination of harmful factors from life - smoking (as well as passive smoking) and drinking alcohol;
- Physical education that strengthens the cardiovascular system;
- Saturation of the body with sufficient amounts of vitamins, minerals and antioxidants;
- Formation of a diet that includes healthy foods.
Regular monitoring of blood composition and health using tests, avoiding harmful substances, a balanced diet and maintaining physical fitness will help protect blood vessels from cholesterol deposits and take timely measures to cleanse them.
Source: https://MyHolesterin.ru/lechenie/giperholesterinemija-kod-po-mkb-10.html
Causes of hypercholesterolemia
Physiological
Cholesterol values can also exceed normal levels in healthy people. For example, changes in the balance of female sex hormones during pregnancy cause an increase in cholesterol levels. After childbirth, the indicators return to normal. In case of improper preparation before taking a biochemical blood test (eating fatty foods on the eve of blood donation), cholesterol turns out to be higher than normal.
Hereditary disorders of lipid metabolism
This group of diseases is called “hereditary (familial) hypercholesterolemia.” They are caused by mutations in genes encoding the expression of lipoprotein receptors (LDLR, ApoB-100, PCSK9) or the lipoprotein lipase enzyme. This leads to disruption of catabolism and absorption of lipoproteins by cells, as a result of which the concentration of cholesterol in the blood begins to increase significantly.
A distinctive feature of familial forms of hypercholesterolemia is the detection of very high levels of cholesterol (in homozygous patients it can reach 20 mmol/l) already from early childhood (5-7 years). All this is associated with the rapid progression of atherosclerosis and the development of serious cardiovascular complications already at 20-25 years of age. Aggressive lipid-lowering therapy is required to normalize cholesterol levels.
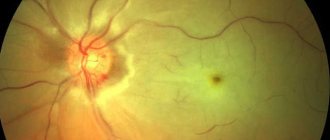
Xanthelasma on the eyelids is a sign of hypercholesterolemia
Obesity
Excess weight ranks first among the etiological factors of hypercholesterolemia and accounts for more than 90% of all its cases. The pathogenesis of the effect of excess weight on cholesterol levels is as follows. Adipocytes secrete a large amount of biologically active substances that reduce the sensitivity of cells to insulin, and insulin resistance is formed.
As a result, lipolysis and the release of free fatty acids (FFA) are activated. From excess FFA entering the liver, a large amount of VLDL, one of the cholesterol fractions, is synthesized. Hypercholesterolemia increases slowly and is directly proportional to the degree of obesity; it can gradually return to normal with weight loss, but over a long period of time it becomes irreversible.
Kidney diseases
The cause of hypercholesterolemia can be kidney diseases accompanied by nephrotic syndrome: the initial stage of glomerulonephritis, diabetic or hypertensive nephropathy, nephropathy with multiple myeloma. An increase in cholesterol levels is associated with the loss in urine of carrier proteins and enzymes involved in lipid catabolism (lecithin-cholesterol acetyltransferases, lipoprotein lipases).
The severity of hypercholesterolemia correlates with the degree of proteinuria. After specific therapy for the underlying disease and relief of nephrotic syndrome, cholesterol levels usually normalize, but in some cases they remain elevated for a long time, which may require additional therapeutic measures to prevent the progression of atherosclerosis.
Endocrine disorders
Diseases of the endocrine system occupy a special place in the structure of the causes of hypercholesterolemia. Insufficiency or excess production of a particular hormone causes significant changes at different stages of lipid metabolism.
- Diabetes mellitus type 2.
The most common cause among endocrine diseases. The mechanism of development of hypercholesterolemia is the same as in obesity (relative insulin deficiency, increased synthesis of VLDL). The degree of increase in cholesterol corresponds to the severity of diabetes. To normalize indicators, both antidiabetic and lipid-lowering therapy are necessary. - Hypothyroidism.
Thyroxine and triiodothyronine stimulate the formation of VLDL receptors and regulate the activity of cholesterol-7-alpha-hydroxylase, the main enzyme in the synthesis of bile acids. A decrease in the concentration of thyroid hormones in hypothyroidism leads to a slowdown in the catabolism of VLDL and the conversion of cholesterol into bile acids. Hypercholesterolemia is moderate, completely reversible. Disappears along with other symptoms of the disease after hormone replacement therapy. - Cushing's disease/syndrome.
Primary and secondary hypercortisolism increase cholesterol levels both directly (adrenocortical hormones and glucocorticosteroids reduce the number of VLDL receptors) and indirectly (through the development of steroid-induced diabetes mellitus). Hypercholesterolemia is more pronounced and more persistent than with hypothyroidism.
Cholestasis
An increase in serum cholesterol levels can be observed in diseases of the liver and biliary tract, accompanied by intra- or extrahepatic cholestasis (stagnation of bile). Hypercholesterolemia is caused by impaired utilization of cholesterol for the production of bile acids. Its degree correlates with the severity of cholestasis.
The highest rates are observed in primary sclerosing cholangitis, primary and secondary biliary cirrhosis, less pronounced in parenchymal liver diseases (alcoholic, viral hepatitis, fatty liver). Elimination of cholestasis leads to a fairly rapid normalization of cholesterol.
Other reasons
- Autoimmune diseases:
systemic lupus erythematosus, hypergammaglobulinemia. - Metabolic disorders:
gout, storage diseases (Gaucher disease, Niemann-Pick disease). - Mental illness:
anorexia nervosa. - Taking medications:
oral contraceptives, beta-blockers, thiazide diuretics.
Hypercholesterolemia - what is it? Causes, symptoms and treatments
Currently, metabolic disorders, which arise under the influence of various causes and risk factors, have become an urgent problem for modern society. Most often, doctors diagnose fat metabolism disorders, resulting in hypercholesterolemia.
Having heard a diagnosis of hypercholesterolemia from their doctor, patients immediately ask a lot of questions: “What is it? What are the symptoms, causes and consequences of the disease? Is there an effective diet and treatment?
Hypercholesterolemia - what is it?
Hypercholesterolemia ( ICD code 10 E78.0) is a pathological condition manifested by a persistent increase in the concentration of cholesterol in the blood plasma.
According to the international classification of diseases, this pathology is a predictor of serious problems with the heart and blood vessels and significantly increases the risk of developing atherosclerosis.
Hypercholesterolemia most often occurs in adults and the elderly, but can also be detected in childhood or adolescence.
Cholesterol is a biologically active substance belonging to the group of fatty alcohols. Endogenous cholesterol is produced by the cells of the parenchymal tissue of the liver, and exogenous cholesterol comes from the outside along with consumed foods. Dietary fats are also broken down and utilized by the liver.
Total cholesterol consists of several fractions, the correct balance of which ensures the normal functioning of the body.
When lipid metabolism is disturbed, the balance between them is disturbed - the level of fatty acids, very low density lipoproteins (VLDL), low density lipoproteins (LDL) and chylomicrons is increased in the blood.
The concentration of high-density lipoproteins (HDL), which have an antiatherogenic effect, on the contrary, decreases.
With liver pathology or excessive intake of exogenous cholesterol, the organ cannot cope with its utilization, the level of lipoproteins in the blood plasma increases and hypercholesterolemia develops. This condition subsequently becomes the cause of pathological changes in the liver and kidneys, heart, as well as blood vessels of all vital organs.
Symptoms of the disease
In order to suspect a problem in time, you need to know the characteristic symptoms of hypercholesterolemia. The very first manifestation of pathology is considered to be elevated cholesterol levels in the blood, which are recorded over a long period of time. Visible symptoms indicating excess serum cholesterol are:
- Xanthomas are accumulations of fatty molecules in body tissues. They can be located in the area of the buttocks, thighs and have the appearance of yellowish tubercles (eruptive), in the area of the knees, elbows, extensor surfaces of the fingers and toes in the form of yellow tubercles with a purple edging (tuberous), tendon xanthomas affect the tissue of the Achilles or other tendons, There are flat fat spots on the palmar surface of the hands;
- xanthelasma - accumulation of excess cholesterol in the form of yellowish blisters under the skin around the orbital fissures, on the eyelids;
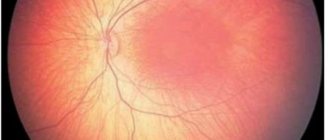
- fat arc - deposition of lipids in the form of a yellow-gray strip along the perimeter of the cornea.
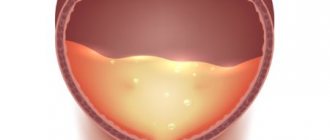
With pathology of lipid metabolism, a dangerous disease occurs, accompanied by hypercholesterolemia, such as atherosclerosis.
Its peculiarity is the deposition of fats on the endothelial lining of the vessels that carry blood to the brain, lower and upper extremities, kidneys, and abdominal organs. Very often, atherosclerotic lesions of the vascular bed occur without pronounced clinical manifestations.
Sometimes patients complain of dizziness, decreased vision, numbness in the arms and legs, pain while walking, pain in the chest, in the abdomen during rest or during physical activity.
Typically, atherosclerosis along with hypercholesterolemia is diagnosed already at the stage of development of dangerous complications - heart attacks, thrombosis of intestinal vessels, lower extremities, acute cerebrovascular accidents. Diseases of the urinary system are also characterized by hypercholesterolemia.
Excess fat is deposited in the vascular network of the kidneys, which leads to deterioration of blood flow in them and the development of ischemia.
The result of this is a violation of their structure and function, which is manifested by an increase in blood pressure, a delay in the excretion of metabolic products from the body, a decrease in daily diuresis and can result in the formation of chronic renal failure.
Causes and stages of development of pathology
Hypercholesterolemia occurs under the influence of certain causes and risk factors. This pathology has several varieties, which depend on its development mechanism.
Primary hypercholesterolemia is hereditary in nature , transmitted from generation to generation, its first manifestations can occur in childhood due to the fact that the biochemistry of fat metabolism is disrupted at the genetic level.
The secondary form is a consequence of the patient’s existing ailments (decreased thyroid function, diabetes, liver pathologies).
The causes of hypercholesterolemia of alimentary origin are excessive human consumption of food rich in animals or hydrogenated fats, frequent consumption of simple carbohydrates (sweets, baked goods).
In addition to the above reasons, the failure of lipid metabolism with the subsequent addition of hypercholesterolemia is due to a number of provoking factors:
- presence of bad habits (abuse of alcoholic beverages, smoking hookah or cigarettes);
- lack of adequate physical activity;
- presence of excess kilograms:
- love of foods rich in fats (fast food, baked goods and flour products, lard, fatty cheeses, margarine or butter, sausages);
- being under conditions of chronic stress;
- lack of work and rest schedule;
- reaching adulthood;
- gender (females before menopause are less susceptible to hypercholesterolemia than males due to the hormonal characteristics of the body)
According to statistics, secondary or nutritional hypercholesterolemia is most common. The hereditary form of the disease is registered with a frequency of 1 sick person per 500 healthy people.
Diagnostic methods
In order to correctly diagnose and find the reasons for the increase in plasma cholesterol concentrations, the doctor prescribes the patient to undergo a full examination.
Patients are interested in the question: “What does a complete examination mean?” Pure hypercholesterolemia is detected through a special analysis - a lipid profile. This study helps the specialist to most accurately assess the state of the patient’s fat metabolism.
For this purpose, venous blood is taken from the patient on an empty stomach, it is analyzed and deviations from the norm, if any, will be obvious.
If an elevated cholesterol level is detected, the patient must take a glucose test, thyroid hormonal profile, undergo monitoring of nitrogenous blood waste (urea, creatinine), and take liver tests.
These auxiliary tests will allow you to assess the condition of vital organs, excluding or confirming their pathology. If a hereditary form is suspected, patients are advised to undergo genetic testing.
Identification of defective regions of genes responsible for fat metabolism indicates familial hypercholesterolemia.
In order to early detect atherosclerotic vascular lesions against the background of high cholesterol and prevent fatal complications, patients are recommended to undergo Doppler testing .
This study helps to assess the state of blood flow in the organs being examined and to identify deviations from the norm in a timely manner. Doctors recommend performing an angiographic study in cases where there is a violation of blood flow in any part of the vascular bed.
Using this method, it is possible to determine the location of fatty plaque deposits and assess the degree of stenosis of blood vessels.
Treatment and prevention of hypercholesterolemia
Patients diagnosed with hypercholesterolemia often ask their doctor: “What to treat and how to treat?” Therapy aimed at reducing serum cholesterol levels should be comprehensive . Before starting medication, patients should change their diet. For hypercholesterolemia, the diet should include foods that are completely free of transgenic and animal fats and simple carbohydrates.
The consumption of sausages, fatty cheeses and meat products, lard, margarine, baked goods, sweets, fast food, sweets, and carbonated drinks is prohibited.
Medicines that have a lipid-lowering effect are represented by statins, fibric acid-based drugs, and anion exchange resins. In case of severe hypercholesterolemia, combined use of drugs is possible.
The selection of a medicine and its dosage is carried out exclusively by the attending physician after assessing the results of the patient’s examination! Some experts recommend the additional use of folk recipes (infusions or decoctions of medicinal plants with hypolipidemic properties) to combat high cholesterol.
Modern science does not stand still. Global pharmaceutical companies are developing new drugs for the treatment of hypercholesterolemia, as well as its consequences.
American scientists believe that the future lies in antisense therapy, which is the development of genetic engineering.
Its essence lies in introducing special nucleotide chains into the genome of a sick person, which will inhibit the production of the protein that provokes the onset of the disease.
Prevention of the disease is based on maintaining a healthy lifestyle. Doctors recommend paying great attention to your diet, actively playing sports, avoiding stressful situations, setting aside enough time for sleep, maintaining normal body weight, and getting rid of bad habits.
Source: https://holestein.ru/analizy/giperholesterinemiya
Diagnostics
Laboratory hypercholesterolemia is detected by examining venous blood. In addition to the concentration of total cholesterol, the determination of its fractions and triglycerides is of great information. For differential diagnosis, the patient’s age and other anamnestic data are important - taking medications, the presence of close relatives with a confirmed familial form of hypercholesterolemia. To clarify the etiological factor, the following examination is carried out:
- Routine laboratory tests.
The content of liver transaminases (ALT, AST), markers of cholestasis (alkaline phosphatase, gamma-glutamyl transpeptidase), and glucose are measured. If nephrotic syndrome is suspected, a general urinalysis, analysis for microalbuminuria, and daily proteinuria are performed. - Hormonal studies.
The concentration of TSH and thyroid hormones (free T4 and T3) is determined. To confirm hypercortisolism, the level of cortisol in the blood is checked after performing small and large dexamethasone tests. - Immunological tests.
Tests are performed for markers of viral hepatitis (HBsAg, HCV), antimitochondrial (AMA), antineutrophil (ANCA) antibodies. - Ultrasound.
An ultrasound of the abdominal organs may reveal gall bladder stones, wall thickening, and signs of fatty infiltration in the liver. - Genetic research.
If hereditary hypercholesterolemia is suspected, mutations in the LDLR, PSCK-9, and ApoB-100 receptor genes are detected using the polymerase chain reaction.
For drug correction of hypercholesterolemia, different groups of drugs are prescribed
Hypercholesterolemia - description, causes, symptoms (signs), diagnosis, treatment
Hypercholesterolemia (HC) is an increase in serum cholesterol more than 200 mg/dL (5.18 mmol/L). One of the main risk factors for atherosclerosis. Frequency. 120 million people have a blood cholesterol level of 200 mg% (5.18 mmol/l) or more; 60 million - 240 mg% (6.22 mmol/l) or more. Predominant age: elderly. Predominant gender: male. Code according to the international classification of diseases ICD-10:
|
Correction
Conservative therapy
If hypercholesterolemia is detected, it is imperative to consult a doctor to find out the cause of this laboratory phenomenon and select appropriate treatment. Much attention is paid to the fight against the underlying disease (immunosuppressive therapy for nephrotic syndrome, hormone replacement therapy for hypothyroidism, choleretic therapy for cholestasis), since its elimination can lead to normalization of cholesterol levels without additional intervention.
Non-drug methods for correcting hypercholesterolemia include complete smoking cessation and limiting alcohol consumption. Also, in order to reduce body weight, obese patients must follow a diet with a decrease in the proportion of animal fats in the diet (butter, fried meat, sausages) and an increase in vegetable fats (vegetables, seafood), fruits and whole grains, and regularly perform various physical exercises.
For the drug correction of hypercholesterolemia, the following drugs are used:
- Statins
(atorvastatin, rosuvastatin). The most effective and frequently prescribed means to reduce cholesterol levels. The mechanism of action is based on the suppression of cholesterol synthesis in the liver. - Fibrates
(clofibrate). These drugs stimulate the activity of the LPL enzyme, thereby accelerating the degradation of the drug. They reduce not only cholesterol, but also triglycerides, so they often become the drugs of choice for patients suffering from diabetes. - Ezetimibe
. Inhibits the absorption of cholesterol in the intestine. Used in combination with statins. - PCSK9 inhibitors
(alirocumab). These are monoclonal antibodies that bind to LDL receptors in the liver, which stimulates the breakdown of lipoproteins. Prescribed when statins are ineffective. - Bile acid sequestrants
(cholestyramine, colestipol). They are ion exchange resins that suppress the absorption of bile acids in the intestine. Depletion of FA reserves activates their synthesis from cholesterol in the liver. Used in patients with cholestasis. - A nicotinic acid
. This drug reduces the flow of fatty acids into the liver, which suppresses the synthesis of lipid. It has a weak hypocholesterolemic effect, therefore it is used as an addition to other drugs. - Omega-3 fatty acids
. Eicosapentaenoic acid and docosahexaenoic acid are components of fish oil. These substances bind to the nuclear PPAR receptors of liver cells, which leads to a decrease in serum lipid levels.
Surgery
One of the prerequisites for the effective treatment of hypercholesterolemia is normalization of body weight. For patients with morbid obesity (body mass index above 40), especially in combination with type 2 diabetes mellitus, if conservative methods are unsuccessful, bariatric surgery is indicated - gastric banding, gastric bypass or resection.
If hypercholesterolemia is caused by cholestasis due to cholelithiasis, surgical removal of the gallbladder (cholecystectomy) is performed. Patients with Cushing's disease undergo endoscopic transnasal adenomectomy (removal of the pituitary adenoma). For Itsenko-Cushing syndrome, bilateral adrenalectomy is used.
What is hypercholesterolemia?
In the general population, abnormal blood cholesterol levels are quite common. This fact indicates that hypercholesterolemia is characterized as a medical and social problem of the population.
Hypercholesterolemia is a pathological disorder characterized by an increase in the level of atherogenic lipids in the blood serum.
In the international statistical classification of diseases, pathology is listed in the section of endocrine dysfunctions and in the subsection affecting lipoprotein metabolism disorders and other lipidemias. ICD code 10-E78.0 – pure hypercholesterolemia.
Slightly elevated levels of cholesterol in the blood do not pose a threat to the human body. An increase in levels to abnormally high levels contributes to the development of atherosclerotic changes in blood vessels.
Hypercholesterolemia is an endogenous factor in the development and progression of cardiovascular pathologies.
Pathogenesis of the disease
Hypercholesterolemia progresses against the background of obstructive changes in the body. The leading links in general pathogenesis consist of modifiable and non-modifiable risk factors.
Modifiable risk factors:
- Elevated blood glucose levels.
- Liver pathologies.
- Thyroid dysfunction.
- Arterial hypertension.
- Proteinuria.
- Physical inactivity.
- Long-term use of medications.
- Stress.
Non-modifiable risk factors:
- Individual life history.
- Family history.
- Age.
- Floor.
In the presence of the above factors, it is more advisable to treat the general condition of the body with particular care and promptly eliminate existing problems.
Forms of hypercholesterolemia
In the clinical picture of the disease, the following typical forms of manifestation are distinguished:
- Primary – has a hereditary nature, based on disturbances in the functioning of genes.
- Secondary – progresses against the background of pathological disorders that contribute to changes in the level of cholesterol in the blood serum.
- Nutritional – the development of this form is directly related to a person’s lifestyle. Progresses due to modifiable causes of pathology development.
Fredkinson classification of hypercholesterolemia
A detailed classification of the pathology in question was compiled by Donald Fredrickson .
The Fredkinson classification of pathology has been adopted by the World Health Organization as the international standard nomenclature for the disease.
Classification is a structuring of the pathology in question according to etiology and determining the type:
- Type I – characterized by high levels of chylomicrons in the blood serum. This type progresses provided that the body has a deficiency of the enzyme that breaks down triglycerides and the structure of the apolipoprotein C2 protein is disrupted.
- Type II – characterized by a decrease in the level of lipoprotein lipase and an increase in the level of apolipoprotein B protein.
- Type III – characterized by the manifestation of dyslipoproteinemia, the presence of a defect in the structure of the apolipoprotein E protein.
- Type IV – characterized by the active appearance of esterification products of carboxylic acids and an increase in apolipoprotein B.
- Type V – characterized by the rapid appearance of triglycerides and a sharp decrease in lipoprotein lipases in the blood serum.
Types of hypercholesterolemia:
- Genetic.
- Family.
- Homozygous and heterozygous familial.
- Children's room.
Genetic hypercholesterolemia
Pathology according to the type of autosomal dominant form.
Character traits:
- Part of the monogenic group determined by the monogene.
- Passed on by inheritance.
- Is congenital (hereditary hypercholesterolemia)
The defective gene is transmitted if the parents have a medical history aggravated by the deviation in question. The carriers can be either one parent or the wallpaper.
Familial hypercholesterolemia
Progresses due to a genetic defect in low-density lipoprotein receptors.
Character traits:
- Lipoproteins lose their ability to bind to cholesterol and transport it to the required organ.
- The quantitative indicator of synthesized deposits of fat-like substances, which contribute to the development of cardiovascular pathologies, increases.
- Development of coronary disorders.
Homozygous familial hypercholesterolemia
Character traits:
- The presence of two mutated allelic low-density lipoprotein genes.
- Development of rapid dysfunction of lipid breakdown.
Mutational changes in genes of this type are quite common.
Heterozygous familial hypercholesterolemia
The most common type of variety of the pathology in question.
Character traits:
- A mutation of one gene that contributes to its defective lesion.
- Presence of tendon xanthomas.
Mutational changes in genes of this type are most common in childhood relapse.
Pediatric hypercholesterolemia
Hypercholesterolemia in children has a pronounced atherogenic orientation. This indicator can be detected for the first time during the life of a newborn.
It is more expedient to diagnose the clinical picture in infancy, which will allow monitoring the indicator parameter, preventing obstructive changes in the child’s body.
Symptoms
With a slight increase in blood cholesterol levels, the pathology proceeds latently. More pronounced symptoms of the disease appear when the pathological disorder enters a progressive stage. The symptom complex is quite specific.
Main symptoms of the pathology:
- Xanthomas are neoplasms on the skin in the form of papillomas, formed due to dysfunction of fat metabolism, which contains cholesterol and triglycerides.
- Xanthelasma is the formation of flat plaques on the skin. Most often localized on the eyelids.
- Lipoid arc of the cornea - visually they represent a pathological rim along the edges of the cornea, of a grayish tint.
Increased levels of atherogenic lipids in blood serum can be detected through timely diagnosis.
If similar symptoms are detected, it is advisable to seek advice from a specialist.
Diagnostics
Hypercholesterolemia is an indicator detected using laboratory tests. In clinical practice, laboratory tests are considered the most effective and informative methods for diagnosing human vital systems.
Standard diagnostic measures include:
- Psychological history.
- Analysis of the patient's life.
- Physical examination.
- Urine examination.
- Biochemical blood test.
- Study of the lipid spectrum.
- Immunological blood test.
Timely diagnosis of the pathology in question allows you to minimize the risk of complications.
Treatment
When diagnosing the pathology in question, it is more advisable to immediately begin adequate treatment in order to avoid negative consequences.
Therapy for hypercholesterolemia is not specific and includes the following treatment methods:
- medicinal;
- modern;
- folk;
Modern methods
Modern treatment includes a number of actions:
- Body weight control.
- Therapeutic physical training class.
- Dietary diet.
- Rejection of bad habits.
This technique is based on achieving positive dynamics of the disease without using medications.
Drug therapy
Mostly, patients with this pathology are prescribed lipid-lowering drugs.
The main functions of lipid-lowering medications:
- Effectively lowering cholesterol levels in human blood.
- Neutralization of the enzyme that activates the production of cholesterol in the blood serum.
Basic medications regulating lipid metabolism:
- "Lipobay" is a medicinal drug from the statin group . Acts in liver cells. Reduces intracellular cholesterol content and activates sensitive low-density lipoproteins on the cell surface.
- Fluvastatin is an inhibitor of HMG-CoA reductase . It is administered orally to the body, regardless of food intake. The dosage is prescribed by a specialist. It is not recommended to take the medication with other drugs of this profile.
- " Lipantil" is an effective medicine . Fenofibrate is the active substance. Enhances the metabolic process of fat breakdown and the removal from plasma of atherogenic lipoproteins with a high content of carboxylic acid esterification products, due to the activation of lipoprotein lipase and a decrease in the synthesis of proteins formed in the cells of the liver and small intestine.
- "Ezitimib" is a lipid-lowering drug that selectively inhibits the absorption of cholesterol. Leads to a decrease in the flow of cholesterol from the intestines to the liver, due to which its reserves in the liver are reduced and its removal from the blood increases.
The above medications must be used under the supervision of a specialist, since lipid-lowering drugs can lead to damage to liver tissue.
During the period of drug therapy, lipid laboratory tests and other biochemical tests are carried out regularly.
Folk remedies
There are many recipes for cleansing blood vessels from cholesterol plaques.
The most effective are decoctions of medicinal herbs and berries:
- perennial dioecious vine;
- rose hips;
- artichoke sativa;
- sandy golden flower;
- water trefoil;
- spotted milk thistle seed powder;
- blue cyanosis rhizomes;
- herbs Tribulus terrestrial;
- celandine;
It is more expedient to use traditional methods of treatment in parallel with methods of traditional medicine.
Possible complications and consequences
The symptom complex of the disease has predominantly latent manifestations. A person does not feel changes in the body, the lifestyle remains unchanged. This creates a cumulative effect. Natural lipophilic alcohol accumulates in the body, increasing the risk of complications.
The main complications are considered:
- Development of atherosclerosis.
- Obstructive circulatory disorders.
- Formation of atherosclerotic plaques.
- Atherosclerosis of the aorta.
- Ischemic disease.
To avoid an unsatisfactory prognosis of the disease, it is advisable to promptly begin a comprehensive program for the treatment of hypercholesterolemia.
Prevention
Preventive measures are an important part of successful treatment.
To avoid relapse of the disease, it is necessary to adhere to the following preventive recommendations:
- normalization of body mass index;
- blood pressure control;
- complete or partial cessation of harmful addictions;
- following a special diet;
- dosed physical activity;
- control over blood serum glucose levels;
- the use of medications to stabilize cholesterol levels;
The recommendations must be followed so that the level of cholesterol in the bloodstream does not increase.
Nutrition for hypercholesterolemia
With this pathology, it is necessary to maintain a rational and balanced diet. A dietary diet provides the body with the maximum amount of nutrients.
It is necessary to significantly limit the consumption of foods that supply cholesterol to the body.
According to statistical studies, a special diet in tandem with physical activity helps to reduce the level of natural polycyclic lipophilic alcohol contained in cell membranes in the body.
General dietary recommendations:
- Limit your intake of saturated fat.
- Add plant-based polyunsaturated fats to your diet.
- Eliminate foods containing cholesterol.
- Use baked goods made from whole grain wholemeal flour.
- Reduce consumption of fatty dairy products.
- Add seafood to your diet.
- Eat foods rich in fiber.
A dietary diet should be balanced and include foods that will provide the body with the nutrients it needs in full.
According to medical statistics, about 110 million of the population have elevated levels of cholesterol in the bloodstream. Thus, they are susceptible to hypercholesterolemia.
In clinical practice, there is a huge choice of methods for treating hypercholesterolemia.
With timely diagnosis of pathology, adequate therapeutic therapy, compliance with preventive measures and a specialized diet, the risk of negative consequences is significantly reduced.
Source: https://kardiohelp.com/bolezni/giperxolesterinemiya.html
Forecast
Hypercholesterolemia leads to the deposition of cholesterol on the walls of arterial vessels, the formation of atherosclerotic plaques, narrowing of the lumen and deterioration of blood supply to organs and tissues. This is of primary clinical importance for the coronary and cerebral arteries. Therefore, a long-term increase in cholesterol concentration is an unfavorable prognostic factor for cardiovascular diseases and is associated with such serious complications as acute myocardial infarction and acute cerebrovascular accident.
Causes
Risk factors include heredity, sedentary lifestyle, overeating (leading to excess weight problems) and stress.
Hypercholesterolemia is divided into several forms, each with its own causes:
- Primary form. Occurs infrequently. Its cause is a hereditary factor, namely the receipt from parents of a gene, in the presence of which excessive synthesis of cholesterol occurs and is not restrained by anything. This may be a manifestation of one of the options: a) genetically determined absence of a receptor that serves to bind cholesterol; b) the absence of an enzyme used for the transport of low-density lipoproteins; c) the inability of LDL to penetrate into cells.
The result of the manifestation of the primary form of hypercholesterolemia is the development of cardiovascular pathologies in early or middle age. Early heart attacks are caused by this form of hypercholesterolemia.
- The secondary form of hypercholesterolemia is caused by other diseases that a person has. This is an underactive thyroid gland (can be caused by heredity, surgery or inflammation); diabetes mellitus with impaired carbohydrate metabolism; disorders of the gallbladder and liver; taking medications that affect lipid metabolism.
- Alimentary form. It is completely the result of an unhealthy diet and lifestyle of the patient, when the presence of carbohydrates and fatty animal products in food becomes constant and excessive, and in addition, is combined with physical inactivity. Obesity develops, which in turn increases the content of fat molecules in the bloodstream.
Diagnostic methods
The most informative study is the lipid spectrum, during which cholesterol is divided into “good” and “bad” and its atherogenicity coefficient is determined.
Additional research methods:
- Studying the patient’s medical history, complaints, his opinion about the causes of xanthomas and xanthellasmas;
- Determination of probable familial hypercholesterolemia, somatic diseases;
- Examination of the patient with blood pressure measurement and auscultation;
- A general blood and urine test to determine the presence of inflammation;
- Blood test for biochemistry (determination of sugar, creatinine, uric acid levels);
- Lipidogram for the presence of elevated levels of lipoproteins;
- Study of immunological status;
- Study of the genetic pattern of hereditary diseases in all family members.
Standard Treatments
Non-drug methods used in the treatment of hypercholesterolemia:
- Correction of body weight.
- An individually designed physical activity plan, taking into account existing pathologies and oxygen flow.
- Normalization of the diet: increasing the proportion of vegetables and fruits, avoiding fatty and fried foods, reducing the calorie content of the diet.
- Avoiding the use of alcohol to slow down weight gain and reduce side effects when taking medications systematically.
- Smoking ban, as nicotine increases the risk of developing heart and vascular pathologies and reduces the concentration of anti-atherogenic substances.
Familial hypercholesterolemia
The disease is caused by a genetic disorder of fat metabolism. There are two types: homozygous - the defective gene is received from both parents, heterozygous - from one. The first disease is more rare (1 person per 1,000,000), but much more severe. The level of cholesterol in it exceeds the norm by 4-6 times. The second pathology is more widespread (1 person out of 500), but less dangerous. The level of sterol is 2-3 times higher than that of a healthy person.
People with this disease are at risk of early development of atherosclerosis, as well as its complications: coronary heart disease (CHD), myocardial infarction.