Consequences of stroke: vascular dementia
Vascular dementia occurs when the brain tissue is severely damaged
With ischemic brain disease (chronic), the following result is possible: vascular dementia. Most often this happens in old age. The cause is damage to the part of the brain responsible for memory or performing skills.
As a result of the disease, the patient’s memory and thinking deteriorate, he cannot perform ordinary skills, which complicates everyday and professional life.
Vascular dementia does not always appear after a stroke, only with severe damage to brain tissue or after a recurrent stroke due to hypertension.
If after a stroke a person becomes lethargic, gets tired quickly, mental activity decreases, and is not interested in family affairs, this may indicate the onset of vascular dementia.
The onset of the disease can be acute. The person suddenly becomes aggressive, memory deteriorates. In this case, urgent consultation with a specialist is necessary.
Vascular dementia always occurs with:
- coronary heart disease
- arterial hypertension
- changes in the blood vessels of the brain
- the risk of the disease depends on whether the patient or his family controls blood pressure, blood viscosity, and cholesterol levels
Thus, if a loved one has suffered a stroke, it is necessary to monitor him for some time.
How does dementia develop?
Alzheimer's disease begins gradually and gets progressively worse, but dementia can occur relatively abruptly – for example, in the context of a stroke. Vascular dementia is sometimes stable for long periods of time and then suddenly worsens. Thus, the disease often takes on a stepwise character, with moments of deterioration alternating with moments of enlightenment. Sometimes the disease stops at a certain stage, and the condition no longer worsens.
In the case of dementia, symptoms can be so severe that patients are no longer able to cope with daily activities independently and depend on outside help around the clock. In the later stages of the disease, they are bedridden, no longer recognize close relatives, and need help with simple activities such as bathing and eating. Additional problems may cause dysphagia. Most people with dementia lose control of their bladder and bowels.
Bladder
Vascular dementia is caused by low blood flow to the brain (cerebral ischemia), which leads to the death of nerve cells. Various mechanisms cause this ischemia:
- The most common type is multi-infarct dementia. This occurs when one or more cerebral infarctions (ischemic strokes) occurring at the same time kill a critical mass of nerve tissue.
- In other cases, dementia is caused by an infarction in a strategic location (such as the thalamus), which leads to disruption of signaling;
- Circulatory disorders are sometimes caused by thickening of the walls of small blood vessels that transport blood to deep areas of the brain. Small infarcts (lacunar) occur and nerve fibers are damaged. Doctors call this "subcortical vascular encephalopathy."
There are also rare types of dementia that are caused by transient ischemic attacks. Various somatic factors also contribute to the development of dementia. These include:
- Hypertension;
- Heart diseases;
- Diabetes;
- Increased cholesterol levels;
- Obesity;
- Sedentary lifestyle;
- Smoking.
Stroke
Dementia after stroke: what kind of disease is it?
Dementia due to stroke is an acquired dementia caused by changes in the blood vessels of the brain. It should not be confused with congenital dementia.
After a stroke, dementia occurs in no more than 30% of patients. It can appear very suddenly (especially if a vessel has burst in the part of the brain that controls mental activity). Poor blood flow leads to the progression of dementia.
Stages of development and life expectancy
At a severe stage of dementia, a complete collapse of the personality occurs
There are three stages of disease development:
- Easy stage. Intellectual activity is significantly reduced, practical skills remain intact, so the patient can live an independent life.
- Moderate stage. Loss of intellectual activity and many life skills. A person forgets how to use basic things (gas stove, telephone). Someone should be with the patient at all times.
- Difficult stage. Complete collapse of personality, the patient is unable to carry out the simplest hygienic procedures.
These stages are very easy to notice, but the disease cannot be completely cured. Dementia cannot be cured with medications.
Dementia leads to personality degradation. If disturbances were noticed quickly and the patient was provided with timely medical care, then over time these changes stop.
With medication, vigilant monitoring, and reduction of vascular changes, there is a greater chance of recovery.
After a stroke, as a rule, patients diagnosed with dementia die (three times more often). If there was a stroke, but mental activity did not change, such people treat their blood vessels, recover and live a full life.
So, it is important to notice the changes in the patient at the very first stage of the disease, otherwise, the changes will be more serious.
Prevention
To avoid relapses of stroke and manifestations of dementia, you need to give up bad habits and establish proper nutrition.
The most important recommendations:
- Select moderate physical activity that is feasible for the patient.
- Monitor blood pressure.
- Find time for mental and intellectual activities.
- Eat foods with low cholesterol levels.
Scientists have compiled a list of natural foods and herbs that help block the development of dementia. If you include them in your diet, the risk of developing dementia after a stroke is significantly reduced.
- Vitamin C. Found in green leafy vegetables and citrus fruits. Helps restore brain function.
- Folic acid . Found in oranges, strawberries, asparagus, peas, papaya.
- Almond. Includes vitamin E. To get the maximum effect, the product should be eaten on an empty stomach, after soaking in water in the evening.
- Sage. Slows down blood clotting, dilates blood vessels, improves blood flow. Relieves attacks of depression and anxiety.
- Ginseng. Helps damaged brain cells recover. You need to drink up to 600 grams of decoction per day; the herb is brewed like tea and left for 15 minutes.
- Milk thistle . The fruits contain seeds rich in silymarin, this substance prevents the loss of connections between brain cells, which manifests itself in dementia. You should take 420 milligrams of extract per day, available in the form of tinctures, tablets or capsules.
- Melissa. Improves the healing of affected brain cells, inhibits the process of memory deterioration, relieves anxiety, and normalizes sleep. Brew like tea: a teaspoon per glass of boiling water, drink 3 servings a day.
- Ginkgo biloba . Contains strong antioxidants that improve memory performance, increase blood flow to the brain, and inhibit the development of dementia. Brew 250 ml of boiling water leaves, 1 teaspoon per serving, drink twice a day.
Read also: Hematoma after a stroke
Although, unlike age-related dementia, post-stroke dementia does not always lead to complete degradation, the risk of progression of the disease always remains very high. It is possible to avoid such manifestations if you recognize the symptoms in the early stages and immediately consult a doctor. With the help of medications, the patient’s condition can be regulated, keeping it at an acceptable level for existence.
What should relatives do?
Relatives of a person with dementia after a stroke should be patient
The leading role in providing care to patients goes to daily comprehensive care for patients with dementia. Drug treatment relieves or weakens the manifestations of the disease and partially slows down its development.
Relatives of patients are advised to:
- Try to avoid contracting infectious diseases. This has a negative impact on the development of dementia.
- Create a familiar and simple environment. Favorite things and household items should be where they are usually found. It is better to avoid strangers in the presence of the patient.
- Monitoring the intake of medications. If medications are taken irregularly, this may worsen the patient's condition.
- Be patient. Remember that this is a sick person with a disturbed psyche. He grumbles more often, is stubborn and offended. There is no need to prove that you are right, to put pressure on your conscience.
Alzheimer's disease: washing and changing clothes
Often at the stage of moderate or severe dementia, a big problem for caregivers is the patient's refusal to wash and change clothes. It must be borne in mind that many of our grandparents grew up in the countryside, and as dementia progresses, their childhood ideas about life remain the strongest.
In the village of the first half of the last century, no one changed their linen every day or took a shower every morning. Taking a bath once a week was the norm. Therefore, first of all, be guided not by your own habits, but by common sense. The skin of older people is dry (this is why, and not “from dirt”, they most often get itchy), and there is really no need to wash it too often, especially with soap.
Unfortunately, in most cases, if you don't force the patient to wash, he won't do it at all. Already with moderate dementia, stubbornness appears that is inexplicable at first glance. At the stage of severe dementia, the patient may even be frightened by the fact that he is being undressed, because he does not understand why this is necessary. Fear may be caused by pouring water, or the need to get into the bathtub, because the patient does not understand what these objects are.
How to behave so that a person with dementia still maintains hygiene?
- Keep track of what time of day the patient is calmer and more flexible (usually this happens in the morning). Try suggesting that he wash himself during this time.
- Voice the offer to wash yourself several times. This measure will increase the likelihood that the forgetful patient will understand that this event was planned and did not happen unexpectedly.
- You can wash in parts: today your head, tomorrow your feet, and so on. Usually these steps are easier than a “full scale operation”.
- You can replace washing by wiping with a damp sponge.
- Explain to the patient what you are doing, even if he no longer speaks. He can understand your speech. When approaching him, warn him about what you are going to do.
- If the patient cannot be managed, tell the attending physician. He will select drugs that will reduce the patient’s aggressive reactions.
Causes of dementia after stroke
Dementia may occur after a left-sided stroke
The main cause of dementia after a stroke is the stroke itself. Dementia can occur unexpectedly, especially if parts of the brain responsible for intellectual functioning are affected.
Risk factors for dementia include:
- Stroke in the left hemisphere
- Previously occurring cerebrovascular accidents
- Having bad habits
- Elderly age
- Low level of education
In addition, dementia can occur due to genetic predisposition, cardiovascular and endocrine diseases.
Vascular dementia is characterized by cognitive impairment, hemiparesis (impaired movement), and urinary incontinence. At first, the motor defect is more pronounced than the cognitive one.
As you can see, there are many factors that cause dementia after a stroke. Therefore, it is important to treat all diseases in a timely manner.
What diagnostic methods can a doctor prescribe?
To confirm the diagnosis, the patient is also examined by a neurologist and a psychiatrist. A diagnostic examination helps determine the number and location of foci of necrosis.
- Ultrasound, angiography. The condition of the cerebral arteries is determined.
- Electroencephalography.
- General and biochemical blood test.
There is no test or test that can immediately accurately diagnose vascular dementia. With the help of special tests, the doctor can detect dementia in the patient, then he will have to understand its causes. Diagnostics must be comprehensive. It is important for a neurologist to know how the patient’s cognitive impairment manifests itself, whether he has suffered a stroke, heart attack, or suffers from atherosclerosis, arterial hypertension or other cardiovascular diseases.
During neuropsychological testing, the patient is asked to perform some tests and tasks, based on the results of which a number of indicators are assessed:
- How well a person speaks, writes and understands what is said.
- How well can he operate with numbers, perform arithmetic calculations, and determine the date and time?
- How well does he remember new information and learn?
- How well can he plan his actions and implement his plans into reality?
- How does the doctor react to hypothetical situations?
Examination by a neurologist
Before examining a sick person, he will be examined by a neurologist, checking reflexes, movements, sensitivity, muscle strength and tone, vision, touch, sense of balance, and coordination of movements.
Head scan
In order to understand the causes of dementia, your doctor may prescribe the following diagnostic methods:
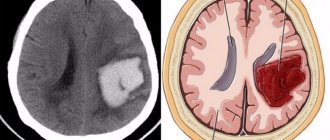
- Computed tomography can detect traces of strokes, transient ischemic attacks, vascular disorders, and intracranial tumors.
- Magnetic resonance imaging shows approximately the same thing, only, compared to CT, it provides the doctor with even more detailed information.
A blood test for cholesterol and sugar helps in diagnosing the causes of dementia. Sometimes you need to check your thyroid hormone levels and other substances.
Symptoms of post-stroke dementia
In post-stroke dementia, memory and speech deteriorate
Symptoms of post-stroke dementia include:
- Disorder of intelligence and daily skills
- The cognitive sphere is impaired (memory deteriorates, speech, counting, reading are impaired)
- Gait is slow and unsteady
- The direction of movement changes abruptly
- Emotional instability, depression
Depending on the affected area, the following signs may appear:
- If the lesion is in the cerebral cortex, then speech disorder occurs and practical skills are lost. Orientation in space is disrupted.
- If subcortical structures are affected, the emotional-volitional sphere, attention are disrupted, and movement disorders appear.
These signs are in many ways similar to simple fatigue (especially in old age). However, it is worth taking a closer look if they appear too often.
Treatment
Treatment is prescribed to compensate for the stroke and restore cognitive and motor impairments. It includes:
- Drug treatment
- Nootropic drugs (increase mental performance)
- Drugs that improve brain metabolism and cerebral circulation
- Antidepressants
- Vitamins
- Massage
- Psychotherapy
The drugs are combined depending on the course of the disease. It is important to monitor the patient's diet. Nutrition should be balanced.
As you can see, there are a variety of medications; treatment concerns not only blood vessels, but also the body as a whole (including the emotional sphere).
cardo-ufa.ru
N.V. Sturov, I.S. Manyakin, E.A. Basova RUDN University, Moscow
Arterial hypertension (AH) is one of the most common diseases in developed countries of the world. Hypertension is often asymptomatic, which makes it difficult to identify the disease, as well as prevent its complications, among which pathology of the central nervous system should be especially noted [1, 2]. Damage to the brain as a target organ in hypertension is manifested not only by acute disorders (ischemic and hemorrhagic strokes), but also by impaired cognitive functions, which include memory, thinking, attention, etc. Even in people without a history of stroke against the background of long-term and In poorly controlled hypertension, cognitive disorders of varying severity are observed, not only in old age, but also in the “middle” years [3]. Risk factors that aggravate cognitive impairment in hypertension include: smoking, dyslipidemia, excess weight, diabetes mellitus and a sedentary lifestyle. Typically, the degree of brain damage in hypertension correlates with systolic blood pressure (BP), however, some studies have revealed a connection between cognitive impairment and increased diastolic blood pressure [4, 5]. Dementia is an extreme degree of impairment of cognitive functions and is a diffuse mental disorder as a result of organic brain damage, manifested not only by impaired thinking and memory, but also by emotional and behavioral disorders [6]. The most appropriate term to reflect brain damage in hypertension, the development of cognitive impairment up to dementia, is vascular encephalopathy, which is also called discirculatory, which associates brain damage with circulatory disorders, including due to hemorheological disorders, and not just with vascular damage (Table 1) [7]. The cause of vascular encephalopathy and dementia is almost always hypertension, atherosclerosis, or a combination of both. Vascular dementia is the result of multiple disturbances of blood flow in the brain, especially the frontal lobes, thrombosis and microinfarction, the consequences of which accumulate for a long time [8]. It is customary to distinguish the following clinical criteria for vascular dementia, which are observed when the patient is in clear consciousness [9]:
1. Memory impairment (short-term, then long-term). 2. Violation of at least one of the following higher functions of the brain: praxis, gnosis, speech, ability to generalize or abstract, regulation of voluntary activity. 3. Violations are so pronounced that they lead to difficulties in the professional sphere and everyday life. 4. Disorders develop as a result of organic brain damage.
The development of vascular encephalopathy is promoted by focal and/or diffuse ischemic damage to the brain, which is based on atherosclerotic damage to the arteries and arterioles of the brain. Cognitive impairments include deterioration of memory (the earliest and most permanent sign is deterioration of short-term memory), thinking, attention, disorientation in time and space, which lead to social maladjustment. This is facilitated by disturbances in logical thinking, unstable attention and errors of perception that occur at different stages of the disease. Patients in the experiment spend more time performing intellectual tasks. Already in the early stages of vascular dementia, rapid psycho-emotional exhaustion can be observed [10]. If dementia is suspected, a history should be obtained from both the patient and those who are knowledgeable about the patient. In the early stages of the disease (initial cognitive impairment), the doctor’s attention should be directed to identifying difficulties in everyday life, because It is in this area that the first signs of mental failure usually appear. Based on clinical manifestations, a neuropsychological research method is used to assess the state of cognitive functions. For severe dementia, so-called screening psychometric scales are usually used, which are a set of the simplest tests for various aspects of cognitive activity: memory, attention, intelligence, praxis, gnosis, speech, orientation, etc. For vascular cognitive impairment, it is better to use neuropsychological tests that are sensitive to frontal dysfunction. Such techniques, for example, include the clock drawing test and the battery of frontal tests [11,12]. For successful differential diagnosis of dementia, it is first advisable to carry out a differential diagnosis between three groups of diseases [13]:
ISCHEMIC STROKE. BRAIN HEMORRHAGE (How to live after a stroke? Doctor's advice)
• Depression: like dementia, depression is accompanied by decreased memory, impaired attention, a narrowing of interests and motivations, and difficulties in everyday life; This form of depression is called pseudodementia and undergoes reverse development under the influence of antidepressants. • Toxic-metabolic encephalopathies: this condition requires screening for metabolic disorders and searching for possible causes of intoxication; Characterized by transient disturbances of confusion and specific changes in the EEG. • Conditions that directly damage brain tissue: tumor, hematoma, multiple heart attacks, etc.
Dementia always indicates organic damage to the brain, and in almost 90% of cases it is the result of either a degenerative disease or vascular pathology (hypertension, atherosclerosis and their consequences). The clinical picture of vascular dementia and Alzheimer's disease are almost identical. Moreover, sometimes these types of dementia are observed simultaneously, which is confirmed by autopsy data. For the differential diagnosis of these types of dementia, the so-called Khachinsky scale has been proposed, based on clear clinical signs and easy to use [14].
Khachinsky scale
1. Sudden onset (2 points) 2. Stepwise course (1 point) 3. Presence of fluctuations (2 points) 4. Nocturnal confusion (1 point) 5. Relative preservation of personality (1 point) 6. Depression (1 point) 7. Somatic complaints (1 point) 8. Incontinence of emotional reactions (1 point) 9. Arterial hypertension (in history or currently) (1 point) 10. History of stroke (2 points) 11. Other (somatic) signs of atherosclerosis (1 point) 12. Subjective neurological symptoms (2 points) 13. Objective neurological symptoms (2 points).
The sudden onset of dementia, its step-like course, the presence of hypertension, a history of stroke and focal neurological symptoms indicate vascular dementia, which is confirmed by a high score (7 or more) on the Khachinsky scale. The absence of the mentioned symptoms and diseases in the anamnesis gives no more than 4 points, which indicates the degenerative nature of dementia, primarily Alzheimer's disease and senile dementia of the Alzheimer's type. Some key differences between vascular dementia and Alzheimer's disease are presented in Table. 2. The results obtained using the Khachinsky scale usually coincide with those of CT and MRI. In vascular dementia, foci of rarefaction are identified (subcortical, cortical and mixed), indicating multiple infarctions. A diffuse decrease in the density of the white matter of the cerebral hemispheres (leukoaraiosis) can also be observed [13]. On the vascular side in hypertension, the most pronounced pathological changes are found in vessels with a diameter of 70-500 µm and in the microvasculature [16]. When treating vascular encephalopathy, the main attention should be paid to preventing further deterioration of the patient's condition by correcting the main causes of the disease - hypertension and/or systemic atherosclerosis. In order to normalize blood pressure, all recommended classes of antihypertensive drugs can be successfully used - ACE inhibitors, sartans, calcium channel blockers, thiazide diuretics, beta-blockers. Blood pressure should be reduced especially carefully, over several weeks, to target levels (in most patients 140/90 mmHg), because otherwise, cerebrovascular insufficiency may occur. Do not forget about the prescription of antithrombotic therapy (acetylsalicylic acid in cardiac doses, clopidogrel, warfarin for persons with atrial fibrillation and a history of thromboembolic stroke). A cholesterol-lowering diet is indicated for all patients with heart and vascular diseases; if indicated, lipid-lowering drugs (statins) are added. Attention should also be paid to the prescription of drugs that improve metabolic processes in brain tissue, which include Actovegin. Actovegin is a highly purified hemodialysate obtained by ultrafiltration from the blood of calves. In addition to inorganic electrolytes and other trace elements, one third of the drug consists of organic substances, such as low molecular weight peptides, amino acids, nucleosides, intermediate products of carbohydrate and fat metabolism, lipids, and oligosaccharides. Magnesium, which is part of Actovegin, is the catalytic center of a number of enzymes. Under the influence of Actovegin, redox processes improve, ATP formation increases, oxidative phosphorylation enzymes are activated, and the process of decomposition of anaerobic glycolysis products (lactate and hydroxybutyrate) is accelerated [17, 18]. Inositol phosphate oligosaccharides included in the drug activate the transport of glucose into the cell [19]. A number of studies have shown that the drug is also an antioxidant [20]. The positive effect of Actovegin on cognitive functions in dyscirculatory encephalopathy, including in the elderly, has been clinically proven [21-23]. The drug helps improve cognitive functions due to its complex antihypoxic and antioxidant effects, but should be used only in combination with basic antihypertensive therapy, since it itself does not have significant hemodynamic properties. Profound cognitive impairment (dementia) cannot undergo complete reversal, since it has a morphological basis in the form of organic damage to the brain. That is why the main attention should be paid to the prevention of vascular encephalopathy and dementia immediately after identifying hypertension in a patient.
References 1. Sharp SI, Aarsland D, Day S et al. Hypertension is a potential risk factor for vascular dementia: systematic review. Int J Geriatr Psychiatry. 2010 Dec; 29. 2. Ostroumova O.D., Smolyarchuk E.A., Srednyakov A.V. Arterial hypertension and cognitive impairment: the potential of long-acting dihydropyridine calcium antagonists. Pharmateka. 2008; 15: 44-54. 3. Kerola T., Kettunen R., Nieminen T. The complex interplay of cardiovascular system and cognition: How to predict dementia in the elderly? Int J Cardiol. 2010 Nov; 19. 4. Skoog I., Lernfelt B., Landahl S. 15-year longitudinal study of blood pressure and dementia. Lancet. 1996; 347: 1141-45. 5. Swan GT, Carmelli D., Larue A. Systolic blood pressure tracing over 25 to 30 years and cognitive performance in older adults. Stroke. 1998; 29 (11): 2334-40. 6. Gavrilova S.I. Mental disorders in primary degenerative (atrophic) processes of the brain. Guide to Psychiatry / Ed. A. S. Tiganova. M.: 1999; 2: 250. 7. Materials of the electronic resource https://www.encephalopathy. ru/information/ 8. Medvedev A.V. Vascular dementia. Modern psychiatry. 1998; 4: 20-23. 9. Erkinjuntti T. Clinical criteria for vascular dementia: the NINDS – AIREN criteria. In: Vascular Demetia. Etiological, Pathological, Clinical and Treatment Aspects / Ed. By L.A. Carlson, C.G. Gottfries, B. Winblad. Basel etc.: S. Karger 1994: 61-64. 10. Damulin I.V., Parfenov V.A., Skoromets A.A., N.N. Yakhno. Circulatory disorders in the brain and spinal cord. In the book: “Diseases of the nervous system. A guide for doctors” / N.N. Yakhno, D.R. Shtulman (ed.). M.: “Medicine”. 2005; 231-302. 11. Dubois B., A. Slachevsky, I. Litvan, B. Pillon. The FAB: a frontal assessement battery at bedside. Neurology. 2000; 55: 1621-1626. 12. Lovenstone S., Gauthier S. Management of dementia. London: Martin Dunitz, 2001. 13. Neurology for general practitioners // Ed. A.M. Veina. M.: "Eidos Media". 2002; 432. 14. Hachinski VC, Iliff LD, Zilkha E. et al. Cerebral blood flow in dementia. Arch. Neurol. 1975; 32: 632-637. 15. Kobalava Zh.D., Gudkov K.M. Secrets of arterial hypertension: answers to your questions. M.: 2004; 246. 16. Gogin E.E., Shmyrev V.I. Complications of hypertension: dyscirculatory encephalopathy, strokes. Ter. archive. 1997; 4:5-10. 17. Chukanova E.I. Actovegin in the treatment of patients with dyscirculatory encephalopathy. Pharmateka. 2005; 17: 71-6. 18. Fedin A.I., Rumyantseva S.A. Selected issues of basic intensive therapy for cerebrovascular accidents. Methodological instructions. M.: 2002; 169-96. 19. Obermaier-Kusser B., Muhlbacher Ch., Mushack J. et al. Further evidence for a two-step model of glucose-transport regulation. Inositol phosphate-oligosaccharides regulate glucose-carrier activity. Biochem J 1989; 261: 699-705. 20. Lyubshina O.V., Talibov O.B., Vertkin A.L. Algorithm for diagnosing stroke at the prehospital stage. Consilium medicum. 2004; 6 (8): 606-9. 21. Ostroumova O.D., Bobrova L.S. Possibilities of Actovegin in improving cognitive functions in patients with vascular diseases of the brain. Atmosphere. Nervous diseases. 2006; 3:28-32. 22. Skoromets A.A., Kovalchuk V.V. Drug rehabilitation of patients after stroke. Journal neurol. and psychiatrist. 2007; 107 (2): 21-4. 23. Herrmann WM, Bohn-Olszewsky WJ., Kuntz G. Actovegin infusion treatment in patients with primarily degenerative dementia of the Alzheimer type and multi-infarct dementia The results of a prospective, placebo-controlled, double-blind study in hospitalized patients. Zeitsch Geriat. 1992; 1-2: 46-55.