Physiological norm and determination of intracranial pressure
The human skull is a cavity in which the brain is located. To protect it from injury, as well as to maintain its normal operation, there are sections filled with liquid. First of all, the liquid fraction is represented by blood, which is located in the vessels. There is also cerebrospinal fluid (cerebrospinal fluid) present here. It is synthesized in special choroid plexuses and enters the skull through the spinal canal, then is located in the ventricles of the brain and is removed through the venous sinuses. This fluid is necessary for the transport of oxygen and nutrients that are used by brain cells to maintain performance.
Intracranial pressure is a complex value that consists of several factors:
- brain pressure (normally it occupies no more than 85% of the skull space);
- blood - up to 8%;
- spinal cerebrospinal fluid - up to 7%.
Blood and cerebrospinal fluid are in constant motion. If blood circulates through the vascular bed, then spinal fluid moves through the ventricles of the brain and along the spinal canal. These fractions are continuously synthesized, enter the cranium and move further along the vascular bed. When they are in the skull, they put pressure on the inside of the blood vessels and ventricles of the brain. For this reason, intracranial pressure is present in every person, and its value can change every minute. An increase or decrease in this indicator may indicate both pathology and normal physiological processes in the human body.
Diagnostics
Only a patient who has undergone a full examination can be given recommendations regarding effective treatment by a specialist.
To confirm the diagnosis, the following methods are used:
- Electroencephalogram of the brain;
- Computed tomography of the brain (during it, a specialist can examine the changes that occur in the human brain);
- Magnetic resonance imaging.
Causes of blood pressure abnormalities
In the CIS countries, increased intracranial pressure is a common diagnosis. It is prescribed for various disorders of the central nervous system in adults and children, and a simple set of therapeutic procedures allows you to quickly normalize the condition and maintain it in the future. However, changes in ICP levels are actually a symptom of a number of dangerous diseases that cannot be treated at home. When making a diagnosis, it is important to pay attention to the patient’s complaints, collect a complete picture and determine whether the pressure inside the skull is really pathologically reduced or increased and threatens human health. In most cases, if ICP is indeed elevated, the patient has a number of additional clinical signs that can be used to identify serious disorders of nervous activity.
Increased intracranial pressure
Increased intracranial pressure is a dangerous phenomenon. It accompanies diseases that threaten the patient’s life. These include:
- inflammatory diseases of the membranes of the brain, including those of infectious origin (meningitis);
- serious poisoning with toxins - in this case there is an increase in the amount of blood in the vessels of the brain and its stagnation;
- traumatic injuries of brain tissue (closed craniocerebral injuries);
- various neoplasms in the cranial cavity;
- hematomas located between the membranes of the brain;
- hydrocephalus is a dangerous disease characterized by impaired outflow of spinal fluid and its accumulation in the ventricles of the brain;
- severe metabolic disorders (advanced forms of diabetes).
In children under the age of 10-11 years, any signs of intracranial hypertension are often associated with birth injuries. Indeed, this factor in history can provoke cerebral hypoxia and various neurological disorders. However, it is important to exclude the possibility of developing hydrocephalus - this disease manifests itself at an early age and is characterized by a rapid increase in the volume of the head. Since the anatomical norm may differ in children (a large head is not a cause for concern), the diagnosis is made based on frequent measurements of head circumference and analysis of the rate of its growth. Signs of increased intracranial pressure in adults are a reason to undergo an examination and exclude the possibility of neoplasms in the cranial cavity.
Reduced pressure
Decreased intracranial pressure is a less dangerous condition. This indicator decreases in certain situations that can be corrected by a set of procedures or by taking medications. No surgical intervention will be required. The reasons for its decrease include:
- production of spinal fluid in insufficient quantities or acceleration of its reabsorption into the blood;
- increasing the permeability of the barrier, which ensures the exchange of fluid between the cells of the central nervous system and the bloodstream;
- decreased tone of blood vessels;
- diseases of the spinal column, especially the cervical region affects the indicator of intracranial pressure;
- any conditions that are accompanied by pathological dehydration of the body: poisoning, taking diuretics, allergic reactions and others.
In some diseases, there is a decrease in the rate of blood circulation through the vessels of the brain. They can also be a consequence of birth injuries, vascular pathologies, and congenital abnormalities of the brain structure. If not treated promptly, this condition can also cause dangerous complications.
Normal in adults
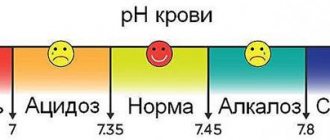
[ads-pc-2]Doctors describe cerebral hypertension in four stages.
The normal intracranial pressure in adults is 10 mmHg. Art. at each “step” another 10 units are added.
The first stage is soft, weak. Appears at readings of 15-20 mmHg. Art. It is characterized by drowsiness and headaches with sudden movements, changes in body position, and coughing.
The second is moderate, average. Diagnosed at values of 21-30 mmHg. Art. Accompanied by tinnitus, apathy, lethargy.[ads-mob-1]
The third stage of intracranial hypertension of the brain is strong, pronounced. Fixed at readings of 31-40 mm Hg. Art. It is characterized by pulsating and shooting headaches, double vision of objects, and nausea.
The normal intracranial pressure in adults reaches 20 mmHg. Art. Anything higher results in symptoms that significantly worsen the quality of life.
The fourth is heavy, very pronounced. Installed at a value of 41 mmHg. Art. and more. It is recognized through the detection of symptoms of severe depression of consciousness, a clear decrease in muscle tone. Also characteristic are hiccups, vomiting, anisocoria - different pupil sizes.
Signs of pathology
Changes in intracranial pressure affect the general condition of the patient. This is often preceded by injuries or blows to the head, complications during childbirth, and diseases of the meninges. In this case, the patient cannot lead a normal lifestyle, and the symptoms of increased or decreased ICP are not relieved by taking medications. Such patients are treated in a hospital setting. It is also impossible not to notice pathological changes in this indicator in children. In addition, in the absence of a reason, the pressure cannot increase or decrease and stop at a critical level for the child - serious reasons are required for this.
The physiological basis of painful sensations with an increase or decrease in pressure, as well as other symptoms, is an insufficient supply of blood to the brain and various disorders of its circulation. If fluid is retained in the vessels and cerebral ventricles, the tissues are under constant pressure, which can provoke gradual necrosis (death) of cells. Hypoxia (insufficient oxygen supply) and nutrient deficiency are also observed - this causes disturbances in brain activity or loss of reflexes, depending on the location of the damaged area of brain tissue.
With high blood pressure
High blood pressure is manifested by a pronounced set of symptoms that affect all vital processes. They may be combined with additional clinical signs characteristic of a particular disease. The symptom complex indicating increased ICP includes:
- painful sensations in the head, which are pressing in nature and spread to all areas, often occur immediately after waking up and intensify during the day;
- sleep disorders, insomnia;
- ineffectiveness of standard drugs against headaches;
- nausea and vomiting, decreased heart rate;
- a sharp decrease in vision, inability to focus on small objects for a long time, deterioration of memory and concentration.
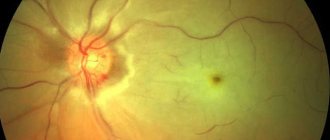
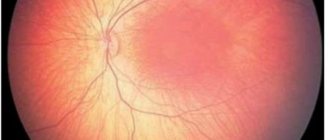
For headaches that occur as a result of serious pathologies of intracranial pressure, the patient remains in bed. During physical activity, attacks of dizziness, loss of consciousness, and memory loss may occur. Also, peripheral vision disorders periodically appear, the appearance of dark spots and “floaters” in the field of vision is a consequence of permanent fluid pressure on the optic nerve. With exacerbation, the situation worsens, normal reflex responses to stimuli may partially disappear.
In children, behavioral problems and hyperactivity are often associated with increased intracranial pressure. However, these diagnoses may not be related. Increased ICP in infants is indicated by symptoms such as bulging fontanel, rapid increase in head circumference, and divergence of the bones of the skull. Another alarming symptom is the overgrowth of the fontanel too slowly. If these signs appear in combination with general apathy or excitability, poor sleep, lack of innate reflexes, this may indicate pathological fluid pressure inside the skull.
At low pressure
Reduced intracranial pressure can also be determined by clinical signs. The symptoms are not as pronounced as when this indicator increases, but also affect the patient’s well-being and performance. If the pressure inside the skull is not normal, this leads to the following consequences:
- headaches, which are especially worse when raising the head;
- frequent mood swings, lethargy, apathy, irritability;
- simultaneous decrease in blood pressure if the syndrome is caused by a general lack of fluid in the body;
- headaches, dizziness, fainting may occur after minor physical exertion;
- decreased visual acuity, appearance of dark spots before the eyes;
- nausea, abdominal pain;
- Possible pain in the heart area that spreads to the chest.
First aid for a sharp decrease in intracranial pressure is to take the correct position. Lying on your back with your head down makes the outflow of fluid difficult, so the pressure is partially restored. This factor may also have diagnostic significance - when you raise your head and sit or stand, the pain intensifies, and lying on your back it decreases slightly.
Symptoms indicating intracranial pressure
The clinical picture of ICP is characterized by a variety of symptoms that differ in adults and children.
Characteristic signs of increased intracranial pressure:
- A pressing and bursting headache of high intensity that occurs after a night's sleep, its location is the forehead, temples, and the back of the head;
- Nausea and vomiting;
- Drowsiness;
- Horse racing hell;
- Impaired cognitive functions (attention, memory, thinking);
- Hyperhidrosis;
- Bradycardia;
- Impaired visual acuity leading to blindness.
Unlike children, most adult patients develop symptoms of increased ICP gradually. The main symptom is headache.
Its parameters:
- Time of appearance - after a night's sleep, is associated with an increase in pressure after a long stay in a horizontal position;
- Character – pressing, pulsating, bursting;
- What provokes the appearance of pain is coughing, sneezing, applying minimal physical effort, staying in a horizontal position for a long time;
- Associated symptoms are dizziness, nausea and vomiting;
- A characteristic feature is that the pain cannot be relieved with painkillers.
Manifestations of autonomic dysfunction syndrome accompanying increased blood pressure:
- Alternating constipation and diarrhea;
- Heart pain;
- Fluctuations hell, pulse rate;
- Hypersalivation (increased salivation);
- Wetness of the palms and soles of the feet;
- Feeling of suffocation;
- Feelings of fear, anxiety;
- increased irritability;
- Apathy and drowsiness.
Less commonly, the patient experiences a combination of increased ICP with symptoms of stroke, which increases the risk of death:
- Loss of consciousness, development of coma;
- Speech disorder;
- Unsteady gait, dizziness;
- Decreased strength in arms and legs;
- Urinary and fecal incontinence;
- Severe vomiting;
- Impaired functioning of the respiratory and cardiovascular systems.
What to do if you find signs of increased intracranial pressure?
Algorithm of actions for a patient suffering from ICP:
- Bring your internal state back to normal, remembering that at the current level of development of medicine, it is possible to maintain the usual quality of life even with increased intracranial pressure.
- Get a consultation with a neurologist, undergo the necessary diagnostic measures (MRI, ultrasound of the brain, X-ray, consultation with an ophthalmologist).
- Compliance with the treatment regimen chosen by the doctor (diet, medications). If surgical treatment is required, you need to decide on it to avoid death.
Diagnostic methods
It is impossible to measure intracranial pressure at home. The only thing a patient can do to help himself is to detect the symptoms in time and consult a doctor for a detailed diagnosis. It is worth understanding that the procedures for measuring ICP are complex and require special equipment and sufficiently qualified medical personnel. All these conditions are available at the Clinical Institute of the Brain, which specializes in the diagnosis and treatment of pathologies of nervous activity.
The only way to accurately determine intracranial pressure is to puncture the cerebrospinal fluid. The technique is invasive and is used only in complex cases. To do this, it is necessary to make a puncture in the lumbar region (into the spinal cord canal) or the ventricles of the brain. The cerebrospinal fluid that is constantly circulating in these spaces will begin to flow out, and its pressure can be measured. The value is measured in mm of water column, and its norm is from 60 to 200 mm. These data are indicative if the patient is in a supine position.
There are also additional diagnostic techniques that allow you to assess the condition of the brain, its ventricles and vascular bed without invasive intervention. These include:
- Ultrasound of the brain - the procedure is performed only for children who have not had fusion of the fontanelle, and in adults it is impossible due to the density of the bones of the skull;
- CT or MRI of the brain - analysis can be done at any age, while the data is quite informative and allows you to obtain a complete three-dimensional image of any area under study;
- echoencephalography is a type of ultrasound examination that can be used to determine the degree of filling and pulsation of the cerebral arteries.
It is impossible to diagnose increased intracranial pressure based on the clinical picture alone. However, all this data must be provided to the doctor during the initial examination. Based on them, specialists from the Clinical Institute of the Brain will prescribe all the necessary diagnostic stages, which will allow a full assessment of the patient’s condition.
Treatment of pathology
The main goal of therapy is to eliminate the cause that caused the increase in ICP. If intracranial pressure does not pose a threat to the patient’s life, the doctor prescribes medication, massage, and physical therapy. If there is a high risk of complications, surgical intervention is necessary.
Physiotherapy
To thin the cerebrospinal fluid, the patient may be prescribed physiotherapy, namely:
- electrophoresis - a phosphodiesterase inhibitor (aminophylline) is injected into the collar area, the procedure is continued for fifteen minutes, the drug improves the supply of oxygen to the brain, normalizes the functions of the organ’s vessels;
- placing a magnet on the collar area - the procedure reduces vascular tone, stabilizes blood pressure, suppresses the sensitivity of brain cells to oxygen deficiency, and reduces swelling of organ tissues;
- massage of the neck and spine - massage promotes improved outflow of venous blood from the head;
- acupuncture – affects reflex zones, eliminates vascular spasms, activates metabolic processes and the activity of the nervous system;
- circular shower - the procedure helps to increase muscle tone, activate receptors, and normalize blood circulation.
- Physical therapy and moderate sports – walking, swimming, cycling – will help reduce intracranial pressure.
Drug therapy
Medicines can only be prescribed by a doctor after the diagnostic results and an accurate diagnosis have been made. Groups of medications prescribed for ICP:
- diuretics (Acetazolamide, Furosemide) - reduce the secretion of cerebrospinal fluid by suppressing the transport of chlorine ions;
- potassium-containing drugs (Asparkam) – normalize electrolyte balance, improve metabolism between tissues, and ensure sufficient absorption of oxygen by the brain;
- corticosteroids (Dexamethasone) – relieve swelling, eliminate intoxication and allergic reactions in the body.
To treat intracranial pressure, patients are often prescribed nootropic drugs; in addition to increasing brain performance, drugs from this group increase the organ’s resistance to harmful effects - excessive stress, hypoxia. Patients may also be prescribed medications to improve cerebral circulation.
Surgery
Surgery is the only method of treating ICP developed against the background of hydrocephalus, trauma, tumors and congenital pathologies.
Depending on the degree and nature of the increase in ICP, the presence or absence of complications, the patient may be prescribed one of several types of surgical intervention - bypass surgery, puncture or endoscopic surgery.
When performing a shunt, cerebrospinal fluid is redirected from the cerebral ventricles to the peritoneal cavity or atrium. During the operation, the surgeon makes a hole in the skull where a catheter is inserted. The doctor places the first end of the tube into the ventricle of the brain, and takes the second out. Depending on the type of procedure, the end of the system is fixed in the right atrium or in the peritoneal cavity. The progress of the operation is monitored by x-ray examination.
Bypass is indicated:
- with the formation of cysts that produce cerebrospinal fluid;
- with hydrocephalus;
- when the cerebrospinal fluid outflow tract is blocked.
Effective surgical methods for removing stagnant cerebrospinal fluid are punctures, namely ventricular and lumbar. The first procedure ensures the outflow of cerebrospinal fluid from the cerebral ventricle through a needle, the second involves the exit of cerebrospinal fluid from the spinal canal.
Cases where puncture is necessary:
- taking a sample of cerebrospinal fluid for histological examination;
- withdrawal of cerebrospinal fluid from the cerebral ventricles;
- ICP measurement;
- administration of medications.
Endoscopy involves perforating the bottom of the third ventricle of the head. Using a rigid neuroendoscope, the surgeon connects the bottom of the cavity and the subarachnoid cisterns, inserts a thin tube into the canal, and the liquid flows through it.
Endoscopic surgery is prescribed to patients in the following cases:
- ICP is caused by traumatic injuries;
- it is necessary to eliminate the shunt system;
- complications arose after bypass surgery.
Treatment and prognosis
Therapeutic measures are prescribed based on diagnostic results. First of all, it is important to get rid of the cause that provokes excessive fluid pressure on the skull. If this phenomenon is caused by traumatic brain injury, the patient is advised to rest completely, take gentle nutrition, and take anti-inflammatory drugs. In some cases, surgical intervention is necessary (in the presence of hematomas between the membranes of the brain, as well as in the presence of injuries that require surgical treatment). Surgery is also prescribed when various tumors are detected in brain tissue that is prone to rapid growth.
A separate set of measures is carried out when diagnosing hydrofecal in a child. To remove excess fluid, a shunt is installed, through which it flows into the abdominal cavity, and the pressure is normalized. The operation is repeated as the child grows, and the patient is constantly monitored. In some children, the need for artificial fluid removal gradually disappears.
Drug therapy for ICP pathologies is secondary. However, drugs are prescribed to eliminate symptoms and make the patient feel better. The following medications may be helpful:
- hormonal anti-inflammatory drugs;
- neuroprotectors and substances for stimulating blood circulation in the brain - the effectiveness of this group has not been proven, despite its widespread use;
- loop diuretics (diuretics) - medications that stimulate the excretion of excess fluid;
- osmodiuretics - including reducing the production of cerebrospinal fluid.
The Clinical Brain Institute specializes in the diagnosis and treatment of diseases of the central nervous system. Increased intracranial pressure is not a separate disease, but a symptom that indicates a number of pathologies. Experienced specialists will accurately determine the cause of such a violation, as well as its severity and possible consequences. It is worth understanding that only timely seeking medical help can guarantee successful treatment and a return to your normal lifestyle without headaches.
Clinical Brain Institute Rating: 4/5 — 51 votes
Share article on social networks
Treatment
When is surgery necessary?
Experts are convinced that the most serious condition is the one provoked by hydrocephalus . This congenital pathology is caused by a violation of the cerebrospinal fluid. When fluid accumulates in excess, it begins to put too much pressure on the membranes of the brain. If not treated promptly, dangerous complications can occur. It may even result in mental impairment.
It is good that today specialists are able to carry out timely and competent diagnosis of this pathology. Usually, parents are informed about this problem by a neurologist during the first examination of their baby.
It must be emphasized that drugs for ICP are ineffective in such a situation. To treat hydrocephalus, only conservative therapy is necessary. The effect of the medications does not go beyond relieving the headache.
To restore normal brain function and cure hydrocephalus, major surgery is necessary. Doctors perform ventricular drainage . This allows excess cerebrospinal fluid to escape. If the cause of ICP is a tumor, then removal of the tumor is also performed surgically.
Treatment with folk remedies
You should not rely on traditional medicine recipes as a panacea for this disease. But it would be useful to consider them as an addition to ongoing therapy.
Folk remedies:
- An operational remedy in the fight against increased ICP is a compress. To prepare it, you need two products: alcohol and camphor oil. They are taken in a 1:1 ratio. This mixture should be applied to the scalp before going to bed. Afterwards, a cellophane cap is put on. To tie the head over it, take a towel. This method will help cope with ICP problems in the morning, while at night the likelihood that it will increase is reduced.
- The next popular express method is to rub lavender oil into the temporal area of the head. It should be hot. You can either buy the oil at any pharmacy or prepare it yourself. For a homemade composition you will need dry lavender herb and high-quality olive oil. To connect the components, a 1:1 proportion is taken. The infusion of the mixture lasts 20 days. Then it is filtered. Its immediate use is recommended as soon as the first signs of pain appear.
- Taking a variety of herbal decoctions gives a good effect . If this is done regularly, then an increase in pressure can also be avoided.
- One of the herbs that helps get rid of pain is mulberry. A decoction of this herb is taken 20 minutes before meals. It is brewed in the following proportion: 20 grams of herb are poured into a liter of boiling water.
- Red clover infused with alcohol also has a positive effect After collecting herbal raw materials, it must be cleaned and placed in a jar as tightly as possible. Then vodka or alcohol is taken and the grass is poured. Infusion time is two weeks.
- You can also prepare a complex herbal tincture. Several herbs are taken equally (you will have to stock up on hawthorn, mint, eucalyptus, motherwort and valerian). They need to be well crushed and packaged. The tincture is prepared from this 1 tbsp. l. composition and alcohol or vodka. They are taken in 0.5 liters. It is necessary to insist for 20 to 30 days. Then the strained mixture is taken when signs of ICP appear. The norm is 20-25 drops per dose.
- Lemon and garlic - these two products not only help fight flu and colds, but are also a proven medicine in our case. The medicine is prepared from two lemons combined with garlic (one head). Eating the gruel in its pure form can cause increased stomach acidity. It is better to dilute it with water (necessarily warm). Taken in the evening. The specified volume is diluted with two liters of water. 30 milliliters are taken at a time.
- maintain normal health not only with the help of decoctions and alcoholic tinctures of herbs. An excellent way to normalize ICP is the use of inhalations. They are made using bay leaves.
Programs:
Functional diagnostics
Ultrasound research methods
Comprehensive examination programs
On-site consultations and research
Headache
Healing procedures
Causes of high blood pressure
The main factors causing ICP are:
- swelling and inflammation of the brain,
- increased production, difficulty in the outflow of cerebrospinal fluid,
- space-occupying formation in the skull - hematoma, tumor, foreign body,
- blood flow disturbance.
These pathogenetic mechanisms occur in the following diseases and conditions:
- ischemic or hemorrhagic stroke,
- head injury (bruise or concussion),
- inflammation due to meningitis, encephalitis, vermiculitis,
- intoxication with ethanol, methanol, poisonous gases, salts of heavy metals,
- tumors of the brain substance or membranes,
- hydrocephalus,
- benign hypertension,
- use of certain medications (corticosteroids, tetracyclines, nitrofurans, oral contraceptives).