Cerebral vascular infarction, the consequences of which may be irreversible, is the most dangerous complication of atherosclerosis. The pathology is difficult to treat and often leads to a deterioration in the quality of life, causing disability. There can be many provoking factors, including vascular thrombosis.
To avoid serious problems, attention should be paid to preventive measures.
Dangerous complications can be avoided if you contact specialists in a timely manner, which is why you need to pay special attention to assessing the first symptoms and avoid provoking causes. A healthy lifestyle is the key to good health and well-being.
How to recognize the signs of cerebral infarction?
There can be many factors for this disease, and the signs by which the disease is diagnosed are different, but we will only touch on the main, most common ones.
Here are the key signs:
- High blood pressure. If you have high blood pressure, you may not feel any specific symptoms that may alert you to danger. High blood pressure damages or narrows the blood vessels in the brain, which consequently results in less blood and therefore less oxygen. If you feel like your heart is beating faster than usual, talk to your doctor to have your blood pressure checked. If your blood pressure is high, consult your doctor and visit him regularly.
- Tightness in the neck. This sensation in the neck can occur due to stress, awkward posture, or excessive muscle tension. It can lead to rupture or obstruction of a blood vessel in the brain. If you have a headache and cannot touch your chest with your chin, consult a doctor immediately.
- Intense headaches. In case of severe headaches and throbbing for no apparent reason, go to the hospital to get tested because these symptoms may be a sign of an increase in your blood pressure, which needs to be taken care of immediately.
- Partial paralysis: Partial paralysis is a common symptom in people with cerebral infarction. Most often, this paralysis occurs during sleep or a little earlier. It is not easy to diagnose, which is why it is important to consult a doctor at the first sign of paralysis of a body part.
- Vision problems. If you don't usually have problems, but your vision becomes blurry at first glance, see your doctor immediately because this could be a sign of a stroke.
- Sudden fatigue. A sudden loss of energy should alert you as it often precedes a serious health problem. Indeed, sudden and intense fatigue may mean that the brain is not sufficiently supplied with oxygen. What determines the outcome/outcomes of strokes/heart attacks: how quickly treatment was started. Important! If you tend to sleep more than usual, you risk having a cerebral infarction. Get checked.
- Problems with coordination. If you suddenly find it difficult to coordinate the movements of your arms and legs, this could be a warning sign. This symptom is difficult to detect, however, it can also manifest itself as severe pain in the shoulders. See your doctor promptly for a checkup.
- Dizziness. Although dizziness is a symptom of many health problems and is rarely serious, it should be monitored and evaluated medically, especially if you have a cardiovascular problem that increases your risk of cerebral infarction.
All of these symptoms are not easy to detect, so at the first warning signs, we strongly recommend that you consult a doctor as soon as possible, and even take a companion with you just in case. An infarction in the territory of the left middle cerebral artery suggests a combination of speech disorders with a variant of cerebral infarction.
- Hemorrhagic cerebral infarction resembles the focus of a hemorrhagic stroke.
- Lacunar stroke occurs in the territory of the left middle cerebral artery.
- Ischemic stroke is the death of brain tissue (cerebral infarction) due to insufficient blood and oxygen supply to the brain caused by arterial obstruction.
An ischemic stroke occurs when an artery in the brain is blocked, often due to a blood clot or fatty deposits caused by atherosclerosis. Another cerebral infarction is included in the group of diseases of the circulatory system.
A cerebral infarction often ends in recovery. Gradually it is possible to eliminate its consequences.
Symptoms appear suddenly and may include:
- muscle weakness,
- paralysis or numbness on one side of the body,
- slurred speech
- confusion,
- blurred vision,
- dizziness and lightheadedness,
- Impaired balance and coordination.
If the area in the basin of the left middle cerebral artery is affected, neuropsychological syndromes are likely. Venous cerebral infarction has significant variability in symptoms. Cerebral infarction in the left carotid region occurs when blood flow in this area is disrupted.
After a cerebral infarction, recovery is not always complete.
Diagnosis is usually based on presenting symptoms and clinical examination and brain imaging.
Other tests and blood tests are done to determine the cause of the stroke.
Treatment may include medications to dissolve clots or reduce her tendency to form blood clots, as well as procedures to physically remove blood clots.
Preventative measures include controlling risk factors, taking medications to reduce blood clotting, and sometimes surgery or angioplasty to open clogged arteries.
What are the causes of brain strokes?
Hemorrhagic and ischemic strokes
With an ischemic stroke, the lumen of a vessel closes due to the formation of a blood clot in the vessel, most often due to atherosclerosis, or the blood clot comes from other parts of the body (for example, the left side of the heart). The main causes leading to stroke are the following:
- Atherosclerosis of the vessels of the heart, aorta and brain.
- Atrial fibrillation.
- Myocardial infarction.
- Prosthetic valve in the heart.
- Infectious endocarditis.
- Atrial tumor.
- Inflammatory vascular diseases.
- Dissecting aortic aneurysm.
- Brain tumors that compress the vessel from the outside and lead to impaired blood flow.
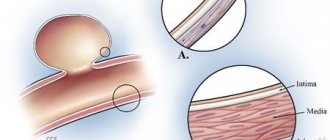
Arterial aneurysm
Hemorrhagic infarction is a condition in which hemorrhage occurs in the brain or subarachnoid space due to rupture of a vessel or increased permeability. The spilled blood compresses the brain and nearby vessels. For this reason, blood flow in this area deteriorates, and brain cells die. The main reasons why cerebral infarction (stroke) develops are:
- Arterial hypertension.
- Arterial aneurysms - congenital or acquired.
- Arteriovenous aneurysms of cerebral vessels.
- Traumatic brain injuries.
- Vascular damage by amyloidosis.
- Encephalitis.
Causes
In case of cerebral infarction, symptoms are determined by the location of the defect. Ischemic stroke is usually caused by obstruction of a cerebral artery, especially on a branch of one of the internal carotid arteries.
It is worth noting that the causes of cerebral infarction may vary. Typically, the obstructions are blood clots (thrombi) or pieces of fatty deposits (atheromas or plaques) caused by atherosclerosis. In this case, atherothrombotic cerebral infarction may occur. These obstacles often occur as follows:
- By forming in and blocking an artery, atheroma in the artery wall can continue to accumulate fatty substances and become large enough to impede blood flow. Even if the artery is not completely closed, atheroma narrows the artery and slows the flow of blood inside, just as a clogged artery slows the flow of water. This slowing of the blood predisposes to clot formation. A large clot can prevent much blood from flowing in the clogged artery, causing the death of brain cells supplied by that artery. If the atheroma ruptures, the material inside can cause a blood clot to form, which blocks the artery.
- When moving from another artery to a cerebral artery: part of the atheroma or blood clot from the vascular wall can become loose and migrate into the bloodstream (forming an embolus). The embolism can then block the arteries supplying the brain and block blood flow. Embolism refers to the obstruction of arteries by materials that travel through the bloodstream to another part of the body. These obstructions are more likely to occur when the arteries are already stenotic and full of lipid deposits.
- From the heart to the brain: Blood clots can deposit in the heart or on a valve, especially on artificial valves and valves that have been damaged by infection of the heart wall (endocarditis). Lumps associated with this type of clot are more common after recent heart surgery, a heart attack, heart valve disease, and arrhythmia, especially an irregular and fast heartbeat. atrial fibrillation.
- In addition to atheroma rupture, several conditions can cause or promote the formation of blood clots, which increases the risk of blockage. Hemorrhagic cerebral infarction is usually localized in the gray matter.
Prognosis for recovery
The final outcome of such a manifestation depends on the influence of many factors: the location of the lesion, the patient’s age and general health.
Statistical data only confirms the danger of vascular infarction.
However, even a doctor will not be able to give a definitive prognosis:
- If the patient has suffered a coma, full recovery is unlikely.
- Approximately 20-25% of patients who have had a cerebral infarction die within the first month.
- After a year, the survival rate reaches 60%, signs of disability appear within the first month with a probability of 40-60%.
- The risk of mortality after 5 years is reduced to 40%.
- After 10 years, the probability of death from complications is 10%.
Positive signs of recovery should appear 1-3 months after the stroke. The first and minor changes are a significant reason for joy, but we should not forget about the doctor’s instructions and following the rules of a healthy lifestyle.
Risk factors
A brain stroke occurs, like many diseases, due to an incorrect lifestyle, and if it is detected in you, then treatment should begin with changing your habits.
The main risk factors for developing ischemic stroke:
- atherosclerosis (arterial narrowing or obstruction by lipids in the arterial walls),
- high cholesterol,
- hypertension,
- diabetes,
- smoking.
Other risk factors include:
- genetic factor
- excessive alcohol consumption,
- use of cocaine or amphetamine,
- an abnormal heart rhythm called atrial fibrillation,
- the addition of another heart pathology, such as a heart attack or infective endocarditis,
- inflammation of blood vessels (vasculitis),
- excess weight, especially of the abdominal type,
- lack of physical activity,
- poor diet (eg, high in saturated fat, trans fat and calories).
What else is needed for prevention?
Stress and worries should be avoided. Scientists have long studied and proven the influence of a tense state on the risk of developing a heart attack. Learn to look at all life's problems with optimism and not get involved in conflicts. If you cannot cope with the problem without the help of others, contact a qualified psychologist.
If an increase in blood cholesterol levels is detected, it is recommended to follow a diet and take statins if prescribed by a doctor. It is recommended to regularly measure your blood pressure and if it continues to rise, consult a doctor so that he can prescribe appropriate treatment.
Physical exercise is also important. You need to devote time to sports regularly. This approach prevents obesity, increases vascular elasticity, and reduces the risk of blood clots.
Symptoms
The stages can follow each other rapidly. The defect can affect the brain stem and other parts, resulting in one or another type of complications.
In principle, symptoms appear suddenly and increase in severity within minutes, since most ischemic strokes occur suddenly, progress rapidly, and cause death of brain tissue within minutes to hours. Subsequently, most of them stabilize and have virtually no damage. These pathologies stabilize in 2-3 days. Sudden embolic obstruction is more likely to cause this type of stroke. Cardioembolic infarction is characterized by the presence of cardiogenic embolic factors.
Less commonly, symptoms develop slowly. They are the result of a stroke that continues to worsen over several hours to 1 or 2 days and causes the brain tissue to expand. The progression of symptoms and damage is usually interrupted by relatively stable periods. During this period, the affected area temporarily stops growing or undergoes some improvement. In principle, these episodes are caused by the formation of clots in a narrowed artery.
There are many different symptoms, depending on the blockage of the artery and therefore the area of the brain that is deprived of blood and oxygen (brain dysfunction varies by location). When the arteries coming from the internal carotid artery (which carry blood along the front of the neck and up to the brain) are affected, the following symptoms most often occur:
- loss of vision,
- inability to see on one side,
- abnormal sensations, weakness, or paralysis of an arm or leg or side of the body.
When the arteries from the vertebral arteries (which carry blood up the back of the neck to the brain) are affected, the following symptoms typically occur:
- dizziness,
- double vision,
- weakness on both sides of the body.
Several other symptoms may also occur, including slurred speech (such as dysarthria), confusion, loss of coordination, and urinary incontinence.
Even less severe forms can cause depression or an inability to control emotions. For example, people may laugh or cry in inappropriate situations.
Some people may have tremors at the onset of a stroke. Seizures may also occur months or years later. Late-onset seizures are the result of scarring or blood deposits that become trapped in damaged brain tissue.
If symptoms, especially disturbances in consciousness, worsen within the first 2-3 days, the cause is often due to excess fluid (edema) in the brain. Symptoms usually improve after a few days as the liquid is absorbed.
However, swelling is especially dangerous because the skull is a non-expandable structure.
The increased pressure on the brain can dislodge it, further impairing brain function even if the area directly damaged does not enlarge. If the pressure becomes very strong, the brain can move down the skull through the rigid structures that separate the brain from other tissues.
Factors that influence the occurrence of cerebral infarction
The main factor is a blockage of the artery, causing a failure of a separate part of the brain. Thrombosis occurs due to changes in one of the vascular walls, due to changes in the rheological qualities of the blood. Prolonged spasms in the veins and arteries of the organ, in turn, also become a negative factor that provokes ischemic infarction of the brain. This process occurs due to a deficiency of nutrients that the human brain requires.
Pathology is divided into five subtypes according to localization:
- carotid artery;
- anterior cerebral artery;
- middle cerebral artery;
- vertebral artery;
- basilar artery;
- cerebellum;
- thalamic regions;
- posterior cerebral artery.
A heart attack occurs when there is insufficient blood flow to the brain. When blood flow is blocked, brain tissue is damaged.
Infarction due to MCA occlusion
Diagnostics
Audible with a stethoscope, the turbulent flow of blood causes a characteristic sound as blood passes through an abnormal heart valve. The same type of sound, somewhat reminiscent of breathing, is heard when blood passes through a stenotic artery. The murmur indicates the presence of atherosclerosis in the blood vessels, a major risk factor for transient ischemic attack or stroke.
A doctor usually makes a diagnosis of ischemic stroke based on your medical history and clinical examination. It can identify a cerebral artery that is blocked based on symptoms (when certain areas of the brain are damaged). For example, weakness or paralysis of the left leg suggests an obstruction in the artery that drains the right area of the brain that controls muscle movement in the left leg.
First, a CT scan is performed. CT also differentiates ischemic stroke from hemorrhagic stroke, brain tumor, abscess, or other types of structural changes. The doctor also measures your blood glucose levels because low blood sugar (hypoglycemia) can cause these symptoms.
If this is possible, then magnetic resonance imaging (MRI) may be performed, which can often be used to detect ischemic strokes within minutes of the onset of symptoms.
If the clot is not visible to visualization, another stroke is likely to occur if the underlying condition is not treated. For example, if blood clots are caused by an abnormal heart rhythm, treating the disorder may prevent new clots from forming, which could lead to another stroke.
Investigations to find causes may include:
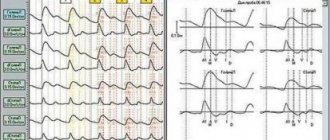
- Electrocardiography (ECG) - in case of suspected cardiac arrhythmias.
- Continuous ECG monitoring (at home or in hospital, continuous ambulatory electrocardiography) to continuously record heart rate over 24 hours (or more), which can detect abnormal heart rhythms that occur quickly or unpredictably.
- Echocardiography - to check for blood clots in the heart or structural abnormalities.
- Imaging such as color Doppler ultrasound, magnetic resonance angiography, CT angiography, or standard (cerebral) angiography to determine whether arteries, especially the internal carotid arteries, are blocked.
- Blood tests for disorders such as anemia, polycythemia, bleeding disorders, vasculitis, and certain infections (such as heart valve infections and syphilis), as well as risk factors such as high cholesterol or diabetes.
This information allows you to determine the necessary treatment. Cerebral infarction develops due to ischemia or blockage of the lumen of the arteries.
Case from practice
A patient was admitted for consultation with a complaint of pain in the upper back and left wrist joint. Ointments and NSAIDs had no effect. He is registered with coronary artery disease and post-infarction cardiosclerosis. On examination, the patient has slight shortness of breath, pale skin, and severe sweating. The attack began as a result of a strong psycho-emotional shock.
Read also: Abstract diagnosis of myocardial infarction
ECG: sinus arrhythmia, single extrasystoles, left-sided hypertrophy. Along the anterior wall there is a scar after a large-focal infarction and at the same time signs of ischemia with transition to the apex and lateral part. (ST segment above isoline I, II, V1-V5, aVF). A blood test confirmed an increase in myoglobin and CPK. He was sent to the hospital with a diagnosis of acute heart attack.
The following sources of information were used to prepare the material.
Forecast
About 10% of patients with ischemic stroke regain almost all of their physiological functions and about 25% regain most of them. About 40% of patients have moderately severe abnormalities that require specific treatment, and about 10% must remain in a nursing home or other alternative facility. Some patients are physically and mentally retarded and cannot move, talk, or eat normally. About 20% of stroke patients die in hospital. This occurs more often in older people.
In the early days of an ischemic stroke, doctors are usually unable to predict whether the patient's condition will improve or worsen. Young people and people who begin to recover quickly are most likely to qualify for a full recovery.
Their intellectual abilities are not affected and they can walk normally, although the use of the affected arm or leg is limited. The use of the arm is often more limited than the use of the leg. Most disorders that are still present after 12 months are permanent.
Cerebral
In cases of this type, signs of cerebrovascular accident come first:
- dizziness;
- fainting, impaired consciousness (lethargy or coma);
- nausea and vomiting that does not bring relief;
- absence of chest pain or its mild severity;
- focal neurological symptoms (muscle paresis, speech impairment).
The real diagnosis can only be determined by performing an ECG or encephalography, after which the patient should be consulted by a neurologist.
Treatment
The discovery of a symptom suggestive of ischemic stroke should prompt the patient to immediately proceed to the emergency department.
If we consider the clinical protocol, the priority is to restore breathing, heart rate, blood pressure (if it is low). Medicines and fluids are given intravenously if necessary. Typically, doctors do not treat high blood pressure until it is high (more than 220/120 mmHg) because when the arteries are blocked, the blood pressure should be higher than normal. However, high blood pressure can damage the heart, kidneys, eyes and should be reduced.
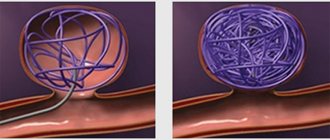
Specific treatments for stroke may include drugs to dissolve blood clots (thrombolytic drugs), drugs to make the blood thinner (anticoagulants). In some specialized centers, blood clots are physically removed from the arteries (called mechanical thrombectomy).
Steps to prevent another stroke include controlling risk factors (including high blood pressure, diabetes and high cholesterol), using medications that reduce the ability of blood to clot, and sometimes surgery or angioplasty to open clogged arteries. In some cases, a drug called tissue plasminogen activator (tPA), can be administered intravenously to dissolve clots and restore cerebral blood flow.
First aid
In case of cerebral myocardial infarction, emergency measures are necessary. 20 minutes after the development of an acute condition, tissue necrosis begins.
The victim should be made comfortable by placing rolled-up clothing under his neck. You must lower the person onto his back carefully, without making sudden movements. He must remain at rest until doctors arrive.
A Nitroglycerin tablet will help avoid a sharp drop in blood pressure. Aspirin is needed to thin the blood. The tablet must first be crushed.
To calm the nervous system, use Corvalol or Valocardine. The dosage should be more than normal - 60 drops.
If the condition worsens and breathing stops, cardiac massage and artificial respiration are necessary.
Heparin is used to stop thrombus formation and prevent it. The first time it is administered intravenously or intramuscularly in a volume of 10,000 units. Then intramuscular injections are performed. This therapy requires monitoring of blood clotting after each injection. It should take a maximum of 20 minutes.
On the third day, indirect anticoagulants are usually prescribed - Phenilin or Neodicoumarin. At the same time, the prothrombin index (blood clotting test) is monitored or the urine is examined for microhematuria (the presence of blood invisible to the eye).
For severe pain, painkillers are used. If they do not bring any effect, then they resort to narcotic drugs. At the same time, neuroleptics are usually prescribed, for example, Aminazine.
Read also: Cell therapy for myocardial infarction
If bleeding increases, the patient is prescribed Vikasol and intravenous infusion of calcium chloride solution (10%).
The patient is prescribed strict bed rest. It must be observed for at least 3 weeks, and for large-focal lesions - more than a month.
The therapeutic complex must include special nutrition. For the first 2 days the patient is only allowed to drink. Then treatment table No. 10 is prescribed, based on dairy and plant foods.
Due to the atypical nature of cerebral myocardial infarction, the prognosis is less favorable. To confirm the diagnosis, instrumental and laboratory diagnostics are necessary. Due to the imperfection of medicine, this process is delayed, so treatment begins late.
Another problem is the similarity of signs of different pathologies. If the diagnosis is not verified, then incorrect treatment may be prescribed.
Cerebral myocardial infarction, like its other forms, can cause many complications. The most severe consequences include paroxysmal tachycardia, pulmonary edema or infarction, and atrial fibrillation.
The cerebral form of myocardial infarction is dangerous due to its atypical manifestations. At the first signs of pathology, it is necessary to call an ambulance, even if they appear in a mild form. The prognosis of the disease depends on the timeliness and correctness of diagnosis and treatment.
Cerebral infarction - symptoms and consequences
Having considered what it is - a cerebral infarction, you need to pay attention to the characteristic symptoms of the disorder, which are worth noting as follows:
- There is numbness in almost half of the person’s body, as well as some weakness, which makes it impossible to feel comfortable in everyday life.
- In the limbs there is a phenomenon called loss of sensitivity (sometimes a situation arises when a person does not fully feel his limbs).
- Sometimes, one of the characteristic signs of a cerebral infarction is the formation of an intense headache; this factor should not be attributed to migraines.
- The person speaks with somewhat difficulty speaking, incoherence is observed, while other people cannot understand him. This is facilitated by some slight stupor, creating the feeling that the person is in a state of fog.
- When considering the symptoms and consequences of a cerebral infarction, a violation of a person’s orientation in space and time deserves special attention. Sometimes it may seem that a person does not know where he is going; he must be constantly guided and helped in reaching the point of arrival.
- Other complications include the occurrence of vomiting and nausea; if such a condition is observed, you should immediately contact a specialist at the clinic, where the correct diagnosis will be made and treatment will begin.
Ischemic cerebral infarction with damage to a small area of nervous tissue in some cases is not easy to recognize due to the blurred symptoms, but with large-scale damage the clinical picture is clearly expressed, and the consequences do not exclude death in approximately forty percent of victims. If help is provided in a timely manner, the chances of a favorable outcome are high.
With a cerebral infarction, warning symptoms are sometimes observed, appearing in most patients in the early morning or at night several hours and even days before the attack. Often this is:
- severe dizziness accompanied by darkening of the eyes;
- numbness in any part of the upper or lower limb;
- short-term speech impairment.
Let us list the main signs of cerebral infarction, some of which are observed in one or another type of pathology:
- loss of consciousness;
- nausea, vomiting;
- headache;
- sudden feeling of heat;
- convulsions;
- severe weakness;
- speech defects;
- visual impairment;
- feeling dazed;
- inadequate emotional state;
- loss of sensation in the limbs;
- memory loss;
- uncontrollability of movements;
- skewed face to one side, etc.
The diagnosis of “cerebral infarction” can entail many other pathologies, the most common of which are:
- congestive pneumonia;
- pulmonary embolism;
- acute heart failure;
- cerebral edema;
- bedsores;
- immobility;
- speech, vision, hearing impairment;
- deterioration of mental activity;
- epileptic seizures;
- coma;
- memory loss.
SILENT INFARCTION: Asymptomatic myocardial infarction
The heart is one of the main organs of our body. To keep him healthy and avoid a heart attack, you need to know simple rules that will prolong your life.
In specialized educational literature, the definition of myocardial infarction sounds like this - an acute violation of the coronary circulation, leading to necrosis of an area or areas of the heart, accompanied by acute, according to the subjective assessments of patients, unbearable pain in the chest, radiating to the left arm, back, jaw. However, in addition to the classic type of heart attack, there are several other types that differ in symptoms and etiological causes.
Prognosis for dysfunction
| Swallowing |
|
| Limb movement |
|
| Breath |
|
| Coordination |
|
| Hemodynamic stability |
|
| Thermoregulation |
|
| Eye movement |
|
Read about the consequences and rehabilitation after large-focal myocardial infarction in another publication.
Brainstem infarction requires professional and long-term treatment. In severe conditions, it may require surgery.