A child has low platelets in the blood: what does this mean - causes and consequences
This video explains in detail what happens when the number of blood platelets in a child changes, almost all the causes of thrombocytosis and thrombocytopenia are listed.
Blood is the most important fluid in our body. By the slightest changes in its composition, you can find out whether everything is fine with the child. One of the important elements of this fluid are platelets.
https://www.youtube.com/watch?v=XYENONS6wiI
An increased content of blood platelets not only indicates the presence of another disease in the body, but in some cases it is also dangerous for the baby’s life. Thrombocytosis is just a symptom of an underlying disease or pathology, but if you do not treat it carefully and take action, serious complications are possible. That is why, at the slightest suspicion, you should immediately contact specialists.
Have you ever paid attention to the platelet count shown on your child's test results? Has your baby ever had abnormal platelet counts? If you have encountered the problem of high levels of blood platelets in your child, share your experience with us in the comments, tell us what treatment the doctor prescribed for you.
Thrombocytosis is considered to be a condition in which the platelet volume exceeds 500 billion/l. Statistical studies have shown that in 3-13% of blood tests in children there is an increased number of blood platelets, that is, this anomaly is quite common. In order to understand the possible causes of thrombocytosis, it is necessary to consider the mechanism of platelet formation.
The substance thrombopoietin is synthesized in the liver, kidneys and medullary stroma, which is identified by special receptors located on the surface of megakaryocytes. The combined effect of thrombopoietin and interleukin activates the synthesis of blood platelets. The reasons for excess thrombocytopoiesis can be divided into several groups:
- infectious, among which are bacterial (meningitis, pneumopathy, lesions of bones and joints), viral (gastroenteritis, meningoencephalitis, hepatitis), parasitic (pneumocytosis, toxoplasmosis), fungal diseases (aspergillosis, Candida infection);
- hematological (iron deficiency, congenital and autoimmune hemolytic anemia, acute bleeding, completion of chemotherapy);
- congenital defects of the spleen or condition after splenectomy;
- traumatic (during surgery or tissue necrosis);
- inflammatory diseases, mainly of a chronic nature (sarcoidosis, polyarthritis, enteropathy, Kawasaki disease, collagenosis, rheumatoid purpura) (see also: idiopathic thrombocytopenic purpura in children: symptoms and treatment methods);
- tumor processes (hepatoblastoma, lymphoma, neuroblastoma);
- pulmonary, as a result of hypercapnia - excess carbon dioxide in the blood;
- medicinal, developing after taking corticosteroids, drugs with adrenaline, heparin injections, as well as after discontinuation of certain cytostatic drugs (Vincristine, Vinblastine) used to treat tumors;
- genetic congenital abnormalities that cause excessive production of interleukin and thrombopoietin.
Blood consists of plasma, red blood cells, white blood cells and lymphocytes. One type of blood cell is platelet. They received their second name because of their shape - blood platelets. Platelets are synthesized in the bone marrow from giant cells (megakaryocytes) by budding and enter the blood where they perform their function.
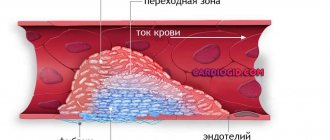
Platelets participate in the process of stopping bleeding: they move to the site of damage and form a primary thrombus, which is overgrown with fibrin, turning into a full-fledged thrombus. Human blood contains 200-400 billion platelet cells per liter. What happens if their number exceeds the norm? What does an increased platelet count in a baby indicate?
Human blood consists of plasma and formed elements (erythrocytes, leukocytes, platelets), each of which performs its own function. A change in the quantity and quality of these components can serve as a signal that a malfunction has occurred in the body. A decrease in the level of platelets in a child’s blood is a cause for concern for parents.
A low level of platelets in a child may indicate the development of some disease READ IN DETAIL: the role of platelets in a child’s body
Platelets are blood cells that organize the process of blood clotting. A decrease in their level in the child’s blood entails the appearance of unwanted bleeding, multiple bruises and bruises, and weak bleeding after injuries. A lack of platelets is scientifically called thrombocytopenia. Platelets in the blood perform the following functions:
- quickly repair damage;
- nourish and maintain the functioning of blood vessels;
- transport substances involved in blood renewal;
- provide immunity support.
The platelet count is measured in thousands per milliliter or femtoliters (fl). Their level in the blood differs in people of different sexes and ages; it changes night and day. There are average platelet volume values for children from birth to 18 years of age. In medical tests it is often designated by the letters MPV (mean platelet volume).
The level of platelets is determined from a general clinical blood test. READ ALSO: high level of platelets in the blood of a child: what to do?
| Age | Norm, mpv, thousand pcs/ml |
| Less than 1 month | 100-420 |
| 1-12 months | 150-350 |
| 1-12 years | 160-300 |
| over 14 years old | 180-320 |
Platelets below normal are observed for various reasons. In adults and children, the decrease in these cells may be different. For example, this indicator decreases in pregnant women and people suffering from alcohol addiction. Low platelet levels occur in babies born prematurely and with low birth weight.
Newborns who are underweight will also have low platelet counts.
The following factors lead to a reduced MPV in children:
- incompatible blood types of mother and newborn (in this case, leukocytes perceive healthy cells as foreign elements and destroy them);
- maternal disease transmitted to the child (thrombocytopenia or lupus erythematosus);
- being born earlier or later than expected;
- blood transfusion;
- asphyxia;
- low hemoglobin level (more details in the article: what hemoglobin level should a child have at 3 months?);
- liver disease (eg, hepatitis);
- past infectious diseases;
- HIV;
- long-term use of analgesics and antibiotics;
- thrombohemorrhagic syndrome;
- oncological diseases;
- viral diseases (herpes, ARVI, tonsillitis, laryngitis);
- mononucleosis;
- traumatic bleeding and hemodialysis;
- excessive consumption of blood thinning products (garlic, lemon, onion);
- the presence of parasites in the body;
- lack of folic acid;
- intoxication of the body;
- tuberculosis;
- lack of vitamin B in the body.
READ IN DETAIL: What are the signs of low hemoglobin in a child?
There are several degrees of severity of thrombocytopenia. With a mild form of the disease, the average volume of platelets in a child’s blood is in the range of 99-50 thousand. per ml.
In this case, there are enough platelets to maintain the integrity of the capillary walls, and bleeding does not occur.
Severe thrombocytopenia is characterized by sudden and frequent bleeding from the nose and mouth. Even microtraumas can cause bruising under the skin. Hemorrhages in internal organs are possible. The platelet count drops below 20 thousand. per ml. At the same time, the child says that he feels good because he does not feel the severity of the disease.
A decrease in the platelet count in the body may not have any effect on the baby’s well-being. Thrombocytopenia almost does not manifest itself externally as long as the level of cells in the blood remains above 50 thousand. per ml. If there are few platelets in the body, then the nutrition of the capillaries is disrupted and they become brittle. There is an intensive release of blood into the surrounding tissues.
If your platelet count is low, your child will often experience nosebleeds
Symptoms of thrombocytopenia:
- The baby has subcutaneous bruising and hemorrhages in the mucous membranes (purpura). With slight pressure, bruises appear on the body. In places where clothing fits tightly, small red spots appear. They are not painful and do not disappear after a while. Reddish dots (bursted blood vessels) may appear in the eyeball. Bruises can be either blue or bright pink, yellowish or greenish.
- Due to the fact that there are a large number of capillaries in the nasal membrane, frequent nosebleeds are observed. They occur even with small impacts and minor physical activity. For example, when sneezing, picking your nose, walking fast, or making sudden movements. Bleeding may continue for more than 10 minutes. The blood that flows out is bright red.
- Gums bleed heavily. This process can continue for a long time.
- Urine turns pink, red, or brown. This occurs due to hemorrhages in the bladder mucosa.
- Darkening of stool to black.
- If MPV is decreased, the spleen becomes enlarged.
- The baby often has headaches.
- Children suffer from vomiting with blood.
- There is heavy blood loss from cuts and injuries.
However, severe forms of thrombocytopenia can lead to serious and irreversible consequences. Treatment of such patients should occur in a hospital setting:
- A low platelet volume can lead to bleeding in internal organs. At the same time, it becomes extremely difficult to stop the bleeding; several organs can be injured at the same time. Small cuts will lead to a large loss of blood, which means that with significant injuries, these losses may be incompatible with life.
- Retinal hemorrhages with low platelet counts can cause vision problems and partial or complete loss. The first signs of retinal hemorrhage will be loss of visual acuity, after which the child may complain of the appearance of spots in the eye. Only a qualified specialist can provide assistance to a child.
- In severe cases, if the levels of these cells are reduced, varying degrees of brain hemorrhage may occur. This can happen either as a result of a minor injury or for no apparent reason. Brain hemorrhage is preceded by increased nosebleeds and hemorrhages in the facial skin. About a quarter of these patients die.
- Severe blood loss leads to severe anemia. It often occurs as a result of bleeding in the gastrointestinal tract, which cannot be quickly diagnosed. The patients' skin is pale, weakness and dizziness appear. With significant blood loss, death can occur.
Elevated platelets in the blood of a child under one year old: what does this mean and what could be the reasons?
An increase in platelets may be due to the presence of ulcerative colitis.
The growth of blood platelets is influenced by the following factors:
- presence of erythremia;
- inhibition of the process of platelet destruction;
- unequal distribution of blood platelets - typical in the presence of overvoltage.
Thrombocytosis can occur in children of any age. We can talk about such a diagnosis when there is a significant increase in platelets. Much more common is a slight excess of the upper limits of the norm.
Secondary thrombocytosis develops against the background of such pathologies:
- ulcerative colitis;
- tuberculosis;
- rheumatism (active form);
- osteomyelitis;
- infections, acute and chronic;
- anemia;
- result of spleen removal;
- fractures of bones, in particular tubular bones;
- cirrhosis of the liver;
- severe blood loss;
- multiple surgical interventions;
- oncology;
- amyloidosis.
In addition to diseases, the use of certain medications, namely the side effects of these drugs, for example, epinephrine, adrenaline, and corticosteroids, can affect the growth of this indicator.
Serious complications with this disease are rare and are characteristic of the primary form of thrombocytosis. Such complications include:
- blood clot formation (quite easily eliminated with proper therapy);
- transformation to leukemia (mainly with long-term treatment with cytostatics);
- myelofibrosis (develops with a certain type of gene mutation).
Secondary thrombocythemia is less dangerous in terms of complications. The symptoms and prognosis are greatly influenced by the factor that caused the disease.
Classification of thrombocytosis
Depending on the origin, primary and secondary thrombocytosis are distinguished. The primary one is called essential thrombocythemia and mainly occurs in older people. In pediatric practice, this disease is rare - 0.09 cases per million children under the age of 14 years.
Secondary thrombocytosis develops as a response to various pathological processes occurring in the body, trauma, and drug treatment. Most cases of increased platelet cell numbers are secondary.
According to the duration of the disease, thrombocytosis is divided into transient and chronic. Transient is a reaction of the hematopoietic system to infections, injuries and other conditions. It does not require specific treatment and goes away on its own when the cause that caused it is eliminated. The chronic type requires a more thorough hematological examination and comprehensive treatment measures.
Characteristic manifestations
General weakness may indicate the presence of thrombocytosis
The following signs may indicate that a child has thrombocytosis:
- heaviness in the legs, their swelling;
- general weakness;
- cyanosis of lips and limbs;
- dizziness;
- itching;
- painful sensations in the fingers;
- cold extremities.
Diagnostics
Diagnostic methods that are used for examination of thrombocytosis are not limited to laboratory blood tests, but cover an extensive examination of many organs and systems. The study helps to understand why platelet levels are elevated. List of diagnostic procedures:
- a detailed blood test with counting of lymphocytes, leukocytes, erythrocytes, blood platelets (this method allows you to identify and confirm the presence of thrombocytosis);
- C-reactive protein test;
- coagulation tests (assessing the level of prothrombin and the rate of thrombus formation);
- a blood test for ferritin, a protein that binds iron (helps diagnose a deficiency of this element);
- serological tests to detect antiviral or antibacterial antibodies;
- measuring the level of vitamins in the blood (B12, E);
- ultrasound scanning of the abdominal organs (particular attention in this study is paid to the condition of the spleen and liver);
- X-ray of the chest and lungs;
- determination of the blood formula of the child’s closest relatives;
- study of platelet aggregation;
- diagnostic biopsy and histological examination of bone marrow;
- myelogram;
- determination of thrombopoietin levels.
In most cases, there is no need to apply the entire list of diagnostic methods; the scope of the examination depends on the specific case. The more unclear the reasons for the development of thrombocytosis, the more extensive research must be carried out. For example, transient disorders do not require detailed diagnosis, but chronic thrombocythemia requires the use of many of the listed techniques.
If a deviation exceeding the normal limits has been detected for the first time, it is advisable to conduct an additional examination.
- Ultrasound;
- identification of c-reactive protein content;
- determination of ferritin and serum iron levels;
- study of the coagulation system;
- consultation with a hematologist, if necessary;
- If a specialist suspects any pathologies of the circulatory system, he will refer you for a bone marrow test.
Useful video about clinical blood test
List of sources:
- Diagnosis of diseases of the blood system. Educational and methodological manual for students of higher medical educational institutions / Edited by Professor I. V. Maev // Moscow, 2002.
- Reactive thrombocytosis. T. 13 / gr. authors // Transfusiology, May 10, 2012.
- Doctor’s pocket guide to laboratory diagnostics / V. S. Kamyshnikov // MEDpress-inform, 2011.
- What the tests say / L. Rudnitsky // Peter, 2014.
Author
Elena Medvedeva
Specialist
Graduated from the Ural State Medical Academy of Yekaterinburg with a degree in General Medicine. Work experience: intensive care team, physician at an enterprise. All articles by the author
I like!
What is the danger
Possible blockage of blood vessels
- As a result of excess platelets in the blood, the clotting process accelerates.
- Platelet agglutination and vascular blockage are observed. This leads to the formation of blood clots.
- It is necessary to understand that this phenomenon has a serious impact on the functioning of organs. This condition will be especially dangerous if there is blockage of blood vessels leading to the brain or heart. The likelihood of developing a stroke or heart attack increases.
What is the role of platelet cells in our body?
Platelets (PLT) are small, red, spherical platelets. They have no core and are designed to perform two functions:
- Form a plug that blocks the flow of blood from the damaged vessel.
- Accelerate the plasma coagulation reaction.
It has been found that with the help of platelet plates, the process of regeneration of damaged tissue occurs much faster, since they release growth factors. After such stimulation with polypeptide molecules, the division of cells of different structures and purposes is accelerated.
The main feature of the red plates is their rapid activation and irreversible transition to a new substance. After exposure to a physiological activator (collagen, thrombin), PLTs attach to the site of injury, sticking to each other. Aggregation of the plates leads to the formation of a plug or thrombus. α-granules are responsible for coagulation.
How to treat?
Treatment of secondary or reactive thrombocytosis involves eliminating or tightly controlling the underlying cause. Transient forms of the disease, for example, the consequences of injuries or surgical interventions, do not require treatment, since their symptoms disappear on their own as the patient recovers.
There is no need to worry if lymphocytes and platelets are increased as a result of an infectious disease. This does not mean that you need to start treatment immediately. Some time after recovery, blood counts return to normal. Thrombocytosis as a result of removal of the spleen or its congenital underdevelopment is lifelong, but does not lead to any serious complications, so treatment is not carried out.
Drug treatment is more often used to treat essential thrombocytosis. Groups of medications used for this disease:
- Hydroxyurea drugs (Droxia, Hydrea) suppress the production of cells in the bone marrow. During treatment, monitoring of liver and kidney function is mandatory. Doctors treat these drugs with caution, since according to some reports, long-term treatment with them can lead to acute leukemia.
- Anagrelide has fewer side effects, but the drug itself is not as effective.
- Interferon alfa - due to the high severity of side effects, injections are rarely prescribed and only for certain medical indications.
Bloodletting is practiced as a folk remedy. It allows you to get rid of excess platelets in the blood, but is used only when there is a risk of blood clots. Traditional medicine offers a number of recipes and remedies that help thin the blood. These include garlic tincture, ginger root decoction, and cocoa drink.
Diet
If your platelet count is high, it is harmful to consume a lot of carbohydrates. The child's diet should include foods rich in iodine (seaweed, seafood, walnuts). Vitamin C, which is present in large quantities in citrus fruits, cabbage, and tomatoes, has a positive effect. It is imperative to add these products to your child’s diet.
Introduction
With the advent of automatic blood formula counting (NFS) machines, platelet counting has become an integral part of the analysis.
Thrombocytosis (defined as a platelet count > 500 G/l when the normal platelet count ranges from 150 to 400 G/l) is detected incidentally or during systemic examination (preoperatively) or clinically a priori without any relationship to the abnormality platelet count. It turns out that from 3 to 13% of children who undergo NFS in the hospital, the platelet count exceeds 500 G/l, that is, we are talking about a relatively common anomaly in pediatrics.
The reasons for this are numerous: but most often we are talking about secondary thrombocytosis or reactive and extremely rarely about primary. In the first case, the platelet count is usually less increased (from 500 to 700 G/l), but the platelet count is not specific to the diagnosis. We propose to reconsider the causes of hyperplaketosis in children in order to determine the place of biological research to be carried out in everyday practice.
Treatment
- Therapy is determined taking into account the disease, which entailed changes in the quantitative composition of platelets. Then the basis of treatment will be aimed specifically at getting rid of a specific disease.
- If changes in the bone marrow are to blame, medications are prescribed that inhibit the production of new platelets.
- Along with this, blood thinning medications are also prescribed.
Diet food
https://www.youtube.com/watch?v=arLn-Z53ib0
In a situation where there is a slight increase in platelets, the use of medications is not justified. The doctor will recommend changes to the child's feeding process.
The following foods should be included in the diet:
- fortified with calcium, in particular dairy products;
- high in iodine, such as seafood and seaweed;
- high in iron, such as liver and green apples;
- that affect the blood thinning process, for example, cranberries or ginger.
The following should be excluded from the diet:
- nuts;
- lentils;
- banana;
- grenades.
It is important to consume a sufficient amount of fluid appropriate for the baby's age.
Platelet Reduction Methods
Significant deviations in laboratory tests require specialized examination and treatment of the child in a hospital setting. If fluctuations in platelet concentration are insignificant and no concomitant diseases are identified, there is no need for drug therapy. Ways to lower platelets in the blood.
The child's food should be rich in healthy vegetables and fruits
Normalization of platelet levels can be achieved by adhering to the following recommendations, of course, after prior agreement with your doctor, nutrition to normalize platelet levels in the blood:
- The volume of liquid consumed daily by the child must be increased, with emphasis placed on berry juices, tea, and carbonated drinks should be strictly excluded from consumption.
- Increase the amount of fresh fruits and vegetables in your daily diet.
- Eliminate foods from your diet that can trigger the activation of blood clotting processes (walnuts, pomegranates, bananas).
- Exclude spicy, fatty and smoked dishes from the menu.
- If possible, temporarily adhere to a vegetarian diet. The only exception is dairy products.
- Be wary of the use of medications. Some groups of medications contribute to blood thickening, so taking any medication should be discussed with your pediatrician before giving it to your child.