What are platelets (PLT)?
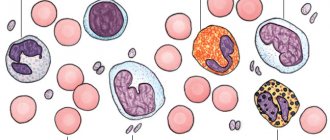
Platelets PLT in blood tests ) are blood cells produced by red bone marrow that are involved in the blood clotting process. Their task is to protect the walls of blood vessels from mechanical damage and prevent significant blood loss.
Blood platelets (also called platelets) are formed from the cytoplasm of megakaryocytes - bone marrow cells.
What is a hemogram? Normal blood count values
Platelets are distinguished by their smallest sizes (2–3 microns), as well as the absence of a nucleus, which does not allow them to be classified as full-fledged cells. Under a microscope they look (in a passive state) as oval or round smooth bodies. The lifespan of platelets is 8-10 days. They then die and are filtered out in the spleen and liver.
What do platelets do?
When a violation of the integrity of the wall of a blood vessel occurs, platelets, under the influence of biologically active substances, rush to the damaged area. There they stick to each other and to the vascular walls, forming a blood clot and stopping the bleeding.
In an activated state, platelets change their shape, which allows them to increase their surface and facilitates the processes of adhesion (attachment to the walls of blood vessels) and aggregation (sticking together).
What is a platelet blood test?
The number of platelets in the blood is determined using a platelet blood test (it is not independent) and is performed during a clinical blood test (complete blood count). First, the blood being tested is diluted in a test tube to the required amount and left for hemolysis (destruction) of electrocytes. The platelets remaining after this are counted using a counting chamber. Blood sampling for analysis should be carried out on an empty stomach.
Certain situations, such as spontaneous platelet aggregation, may result in an unreliable test result.
What should be the norm of platelets in the blood?
The platelet count is measured in thousands per microliter of blood. The norm for healthy people is 150-450 thousand units/μl. If their number exceeds 450 thousand units/μl, then this indicates thrombocytosis. If the rate is less than 150 thousand units / μl, then this is called thrombocytopenia.
When the platelet count decreases below normal values (less than 50 thousand units/μl), there is a risk of bleeding. In more severe cases (when the platelet count is below 10-20 thousand units/μl), spontaneous bleeding is possible.
Thrombocytopenia
Causes of thrombocytopenia
Low platelet count in the blood (thrombocytopenia) is a condition in which the total number of platelets in the blood is lower than normal. The development of severe thrombocytopenia is a serious health hazard and can be fatal without treatment. Most often, thrombocytopenia is a side effect of taking certain medications, as well as a consequence of leukemia. Each of us can face this.
What is SRB? Causes of increased C reactive protein
Bone marrow problems
Bone marrow is the soft tissue inside the bone that produces blood components. The main cause of thrombocytopenia is insufficient production of platelets by bone marrow cells.
The most common causes of decreased platelet production include aplastic anemia, vitamin B12 deficiency, iron and folate deficiency (a compound of folic acid), liver cirrhosis, leukemia, myelodysplasia, excessive alcohol consumption, chemotherapy, exposure to chemicals and radiation, HIV, chicken pox and other viral infections.
Platelet destruction
Regular use of certain medications (anticonvulsants, diuretics, etc.) can affect the destruction of platelets. During pregnancy, the number of platelets in the blood also decreases.
Causes of platelet destruction include diseases such as splenomegaly (enlarged spleen), bacterial infections, hemolytic uremic syndrome, autoimmune diseases such as rheumatoid arthritis and thrombotic thrombocytopenic purpura.
Hemolytic-uremic syndrome: a rare, life-threatening disease characterized by acute kidney failure (uremia), hemolytic anemia, and low platelet counts (thrombocytopenia). Very similar to an E. coli infection that enters the body after eating raw or undercooked meat.
Splenomegaly (enlarged spleen)
The spleen is an important organ that fights infections and filters waste substances from the blood. An enlarged spleen (as a consequence of a number of diseases) can trap too many platelets, which will lead to a decrease in their number in the vascular bed.
Chemotherapy: how to treat cancer, side effects
Thrombocytopenic purpura
This is a pathology caused by a decrease in the number of platelets in the blood and their tendency to stick together. It is characterized by complex and variable neurological symptoms: unilateral paralysis, drowsiness, etc., in severe cases – coma. If the disease is not treated promptly, it can lead to death.
Symptoms of thrombocytopenia
- Purpura (bleeding into the mucous membranes and skin, looks like red, purple or brown spots),
- Bleeding gums
- Nosebleeds,
- Gastrointestinal bleeding,
- Blood in the urine (a sign of internal bleeding),
- Blood in the stool (a sign of internal bleeding),
- Heavy menstruation in women
- Prolonged bleeding from cuts
- Small red or purple dot-shaped rashes on the body called petechiae
- Bloody or very dark mucus (a sign of internal bleeding).
A decrease in platelets in the blood is caused by physiology, for example, during pregnancy, and does not require treatment. In all other cases, as a rule, urgent medical attention is required.
Is thrombocytopenia dangerous?
When the level of platelets in the blood drops below 10 thousand units/mcL, it can cause dangerous internal bleeding. Severe thrombocytopenia, although rare, can cause bleeding in the brain, which can be fatal.
If you have a low platelet count and are experiencing headaches or any neurological problems, you should contact your doctor immediately.
How to increase platelet levels in the blood?
You can increase your blood platelet levels by limiting your alcohol intake and stopping medications such as aspirin and ibuprofen. You should also avoid contact sports and activities that may cause severe bleeding or bruising.
Possible symptoms
An independent clinic of the pathological process under consideration is a relatively rare phenomenon. If we talk about possible manifestations:
- Vision problems. The result of damage to the retinal arteries. Doesn't always happen.
- Increased risk of bleeding. Develops with a high concentration of immature platelets. They are not able to perform their functions, and therefore coagulation is at an insufficient level.
Localization can be very different: from the nose, small capillaries to the intestines, the digestive tract in general, or the lungs. This can be deadly.
- In the presence of mature platelets, the risks shift in the opposite direction. The likelihood of blood clots forming, which clog blood vessels and cause gangrene and fatal complications, increases.
Symptoms of thrombosis of the lower extremities are described in detail in this article.
- Pain in the limbs, fingers. Paresthesia (feeling of pins and needles running down the arms and legs). Disturbances in the normal innervation of tissues.
- Formation of hematomas. Bruises on the body for no apparent reason. Massive “sprinkling” with such is especially noticeable against the background of complete physical rest and the exclusion of a traumatic factor.
- Edema without visible etiology. It is impossible to understand what became the fault.
- Blueness of the skin.
- Weakness, drowsiness.
All these signs in combination are quite rare. More often there is a group of 1-3 manifestations.
Also, signs of the underlying disease are necessarily present if we are talking about a secondary, reactive form of the disorder.
These may be elevated body temperature, neurological problems, dysfunction of the heart, lungs, digestive tract and many other disorders.
Treatment of thrombocytopenia
Treatment varies depending on the underlying cause of low platelet levels in the blood. The disease that led to this should be treated first. Mild thrombocytopenia does not require any treatment; doctors use a wait-and-see approach and monitor the patient’s health. In case of severe thrombocytopenia, treatment is mandatory.
Medical treatment
Treatment options may vary depending on the cause of thrombocytopenia. Depending on the situation, the following therapeutic measures can be recommended:
- Replacing medications that lower platelet levels in the blood
- Prescribing medications such as steroids, corticosteroids, globulin, etc.
- Splenectomy (surgery to remove the spleen)
- Blood or platelet transfusion (red blood cells are transferred to lost blood)
- Prescription of immunosuppressants
- Plasmapheresis (used in the treatment of thrombocytopenic purpura)
Foods to increase platelets
Foods that increase platelet levels include: vitamin C-rich citrus fruits, spinach, Indian gooseberries, beets, papaya, aloe vera juice, pumpkin, raspberries, protein foods rich in vitamin B12, and foods containing vitamin A.
Why are platelets elevated during pregnancy?
During pregnancy, a woman undergoes regular examinations and also donates blood for tests. An important implication of such studies is the platelet level. During pregnancy, the norm of blood cells in the blood is considered to be from 140 to 340 * 109 / liter. In the 3rd trimester and just before birth, the number of squamous cells increases sharply to maintain blood viscosity. This state is maintained until childbirth.
A slight increase during gestation is a physiological process: the body tries to avoid severe blood loss during childbirth. Thrombocytosis during pregnancy is diagnosed when the rate increases above 400*109/l.
In the early stages, an increase in platelets may be due to severe toxicosis: vomiting and diarrhea. At later stages, the reasons for the increase in the number of blood platelets may be:
- Sweating, lack of fluid;
- Viral, fungal diseases;
- Various inflammations;
- Anemia;
- Oncological diseases.
The pregnant woman is referred to a hematologist who prescribes blood thinning medications. The dose of the medication is selected individually, taking into account possible risks for the mother and child.
Increased level of platelets in the blood
Causes of thrombocytosis
Thrombocytosis involves a significant increase in the number of platelets in the blood. If this disorder is triggered by an underlying disease, such as an infection, it is called secondary thrombocytosis (or reactive thrombocytosis).
In the absence of a similar cause as another disease, such thrombocytosis is called primary thrombocythemia. As a rule, primary thrombocythemia is caused by diseases of the blood and bone marrow.
What diseases cause an increase in platelet levels in the blood?
Secondary thrombocytosis
In this case, an increase in the level of platelets in the blood occurs due to some disease. Secondary thrombosis occurs in acute and chronic inflammatory processes (rheumatoid arthritis, ulcerative colitis , etc.), acute blood loss, iron deficiency, cancer, hemolytic anemia, after splenectomy (removal of the spleen), etc.
What is ulcerative colitis? Causes, symptoms and treatment
Essential thrombocythemia (primary thrombocythemia)
As a rule, it is caused by mutations of certain genes. This is a rare disease in which the body produces too many platelets, leading to severe clotting problems and bleeding. According to the MPN Research Foundation*, most patients with primary thrombocythemia have a mutation in the JAK2 gene. Most often it occurs in women over 50 years of age, but it can also occur at a younger age.
*Research Foundation for MPNs (myeloproliferative neoplasms, which are a group of blood cancers caused by mutations in blood stem cells).
Causes of thrombocytosis
Thrombocytosis (causes in adults are given below) in the primary form of the disease may be associated with the following conditions:
- Essential thrombocythemia. This is a chronic disease with a hereditary predisposition, in which active division of megakaryocytes occurs. The disease manifests itself in the form of persistently recurrent thrombosis, most often arterial. Its prevalence is about 3 cases per 100 thousand population. Patients also often experience neurological symptoms - headache, dizziness, blurred vision. About 6% of patients have mutations in the thrombopoietin hormone receptor genes.
- Chronic myeloid leukemia is an oncological disease of the hematopoietic system, which is a cytogenetic anomaly. In half of the patients, leukocytosis is also detected. The disease is often asymptomatic in its early stages, and some patients experience anemia, fever, susceptibility to infection, bleeding, and an enlarged spleen.
- Polycythemia vera, in which excessive formation of cellular elements of the bone marrow occurs. In the blood there is an increased level of hemoglobin (>185 g/l for men, >165 g/l for women), red blood cells, platelet aggregates, and neutrophilic leukocytes. Characteristic signs of this disease are dilated veins under the skin, its unnatural red color, especially in open areas (as well as mucous membranes), which is associated with blood vessels overflowing; skin itching, pain in the fingertips caused by microthrombi in the capillaries; an increase in the volume of the spleen, ulcerative processes in the gastrointestinal tract, a tendency to bleeding gums, joint pain, high blood pressure.
- Primary myelofibrosis , in which excessive division of megakaryocytes is combined with the proliferation of connective tissue in the bone marrow. The latter is gradually replaced by collagen fibers. This is a rare disease, the prevalence of which is 1 case per 100 thousand population. Patients often experience severe anemia, enlarged liver and spleen, and symptoms of tumor intoxication.
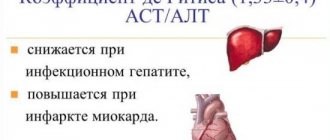
This is interesting: Blood biochemistry - ALT: diagnosis and interpretation
The causes of familial thrombocytosis are mutations in the thrombopoietin genes (4 mutant alleles are known) and thrombopoietin receptors.
Secondary thrombocytosis
The most common causes of reactive thrombocytosis are:
- Inflammatory processes:
- ulcerative colitis;
- Crohn's disease (inflammatory bowel disease);
- systemic inflammatory diseases of connective tissue (scleroderma, dermatomyositis);
- purulent-necrotic processes in the bones and bone marrow.
- Infectious pathologies (pneumonia, sepsis, pyelonephritis, meningitis and others), since platelets are actively involved in the antimicrobial defense of the body. In patients with infectious and inflammatory processes, thrombocytosis is observed in 40% of cases.
- Stress, high physical activity.
- Extensive tissue damage as a result of burns, injuries, surgery (develops in a quarter of patients).
- Malignant neoplasms.
- Chronic autoimmune pathologies:
- juvenile chronic arthritis;
- rheumatism;
- systemic necrotizing vasculitis;
- Kawasaki disease, which occurs mainly in children in the first years of life;
- rheumatoid arthritis;
- systemic lupus erythematosus;
- Behçet's disease, which affects arterioles and venules of medium and small size;
- granulomatosis with polyangiitis (inflammation of the walls of blood vessels).
- Surgical removal of the spleen (or its congenital absence), since the hormones produced by this organ affect the process of platelet formation. Thrombocytosis develops gradually, over 7-10 days after surgery. Normalization of indicators occurs within several weeks (sometimes years).
- Alcohol abuse.
- Blood loss and associated iron deficiency anemia (about 5% of all cases), as well as hemolytic anemia, in which accelerated destruction of red blood cells occurs.
- Taking certain medications (adrenaline, anticancer drugs, vitamin B12, tretinoin, corticosteroids, folic acid, chemotherapy treatment).
- Blood diseases: hemolytic and sickle cell anemia.
In adults
Thrombocytosis in adults is common in 1% of the population. When tested again, most patients' platelet levels return to normal without medical intervention.
Risk factors, in addition to the above reasons, are the following:
- age over 60 years;
- cases of thrombosis of veins or arteries in the patient’s history;
- obesity;
- smoking, drinking alcohol;
- arterial hypertension;
- elevated blood cholesterol levels.
There is also so-called false thrombocytosis, when an automatic blood analyzer mistakenly counts small particles (cell fragments after chemotherapy, cryoglobulins formed at low temperatures, small red blood cells, bacteria, schistocytes - fragments of red blood cells that appear in the blood during hemolytic anemia, thrombocytopenic purpura, hemolytic-uremic syndrome, HELLP syndrome and some other pathologies; parts of cells in tumor diseases of the blood) to platelets.
Detection of thrombocytosis in malignant tumors serves as an unfavorable prognostic sign, since platelets are actively involved in the process of metastasis, which is the last stage of cancer.
In children
In newborns, an increased level of platelets is observed in 13% of cases, in children in the first month of life with low body weight - in 36% of cases, then this indicator decreases again. The normal value is reached by age 11. This phenomenon is associated with instability of the hematopoietic system, and differences in concentration of acceptable values for children are in a wide range.
However, thrombocytosis may also indicate the development of pathologies indicated for adults. Therefore, in such cases, a more detailed study is required, taking into account other laboratory criteria and instrumental examination.
Symptoms of thrombocytosis
- Headache
- Dizziness or loss of balance
- Chest pain
- Fainting
- Temporary visual impairment
- Pain in the hands and feet, their numbness
- Redness, throbbing, and burning pain in the hands and feet (erythromelalgia)
Symptoms depend on the location of the blood clot:
Many patients are asymptomatic with this disease. The first sign of a disorder may be the formation of a blood clot (thrombus). Although a blood clot can form in any part of the body, in primary thrombocythemia the blood clots most often occur in the brain, hands, and feet. In rare cases, if the platelet count in the blood is too high (more than 1 million units/mcL), bleeding may occur in forms such as:
- Nose bleed
- Bruises (bruises)
- Bleeding gums
- Bloody stool.
The clot can lead to a transient ischemic attack (TIA), in which blood supply to an area of the brain is temporarily cut off, or to a stroke. Symptoms of transient ischemic attack and stroke occur suddenly and include the following:
- Weakness or numbness of the face, upper or lower extremities, usually on one side of the body
- Slurred, garbled speech, or difficulty understanding speech (aphasia)
- Blurred vision, double vision, or blurred vision.
Are high platelets dangerous?
If signs of thrombocytosis appear or if there is bleeding, you should consult a doctor. It should be remembered that patients with primary thrombocythemia are at risk of heart attacks. If you experience symptoms of a transient ischemic attack or stroke, such as numbness or paralysis on one side of the body, you should seek immediate medical attention.
Diagnosis of thrombocytosis
First of all, your doctor will check to see if your spleen is enlarged and will also evaluate your general condition for signs of infectious diseases. After you take a blood test, based on its results, it will determine whether the number of platelets in your blood is higher than normal or not. If necessary, additional tests may be done (for example, aspiration biopsy, bone marrow biopsy).
Course and symptoms of thrombocythemia
Thrombocythemia in most cases is a slowly progressive disease, in which many months or even years may pass from the moment the first changes are detected in a blood test until the first clinical symptoms appear. The risk factors and etiology of thrombocythemia are still not clearly defined, but it is known that pluripotent bone marrow progenitor cells are involved in the process.
An increase in the number of platelets is associated with both an increase in the sensitivity of megakaryocytes to cytokines and its decrease in relation to inhibitory factors. Disruption of the bone marrow microenvironment is also thought to play a significant role.
The mechanism of occurrence of thrombohemorrhagic symptoms in thrombocythemia has been well studied. It involves changes in the aggregation and intracellular accumulation of certain chemicals due to an increase in the molecular weight of von Willebrand factor multimers, a decrease in the activity of ristocetin von Willebrand cofactor, and a deficiency of proteins C and S and antithrombin III.
The clinical picture of the disease is characterized by thrombotic and hemorrhagic manifestations in the absence of a clear correlation between the frequency of thrombosis and the level of thrombocytosis, however, due to comorbid vascular damage in old age, thrombotic symptoms of thrombocythemia are recorded more often. In most cases, these are coronary, cerebral and peripheral arterial thromboses. Deep vein thrombosis of the lower extremities and pulmonary embolism occur much less frequently.
Hemorrhagic manifestations can be expressed in the development of pulmonary, gastrointestinal, renal bleeding and skin hemorrhages. Other symptoms of thrombocythemia include:
- Enlarged liver (up to 20%);
- Splenomegaly (up to 40-50%);
- Dizziness;
- General weakness;
- Itchy skin;
- Increased sweating;
- Impaired concentration and memory;
- Headache;
- Erythromelalgia;
- Dysphoric phenomena.
Due to impaired microcirculation against the background of thrombocythemia, a feeling of numbness in the earlobes and tip of the nose, as well as in the upper and lower extremities, may occur. Against the background of a tendency to erosive and ulcerative processes in the gastrointestinal tract, pain may appear along the intestines and in the epigastrium.
Treatment of thrombocytosis
Treatment of secondary thrombocytosis
Treatment depends on the cause of thrombocytosis. The problem of elevated platelet levels is solved by treating the acute or chronic disease that caused thrombocytosis. In case of blood loss due to surgery or injury, the platelet count gradually returns to normal on its own.
If you have your spleen removed, you may have to live with high platelet levels for the rest of your life. However, in this case no additional treatment is required.
Treatment of primary thrombocytosis
Treatment is based on the risk of blood clots. If there are no symptoms, no treatment is required. But, patients over 60 years of age who smoke, have diabetes or any cardiovascular disease, and who have repeatedly experienced bleeding or blood clotting problems should definitely undergo treatment.
As a rule, treatment is reduced to taking aspirin in low doses. In addition, the doctor may prescribe medications that reduce blood clotting and prevent the formation of blood clots. Also, a procedure called plateletpheresis can remove excess platelets from the blood.
If you have recently been diagnosed with primary thrombocythemia, you should stop smoking. In addition, if you have problems with cholesterol, diabetes or high blood pressure, you should exercise regularly and eat a diet (fruits, vegetables, whole grains, lean sources of protein).
Foods that lower platelet levels
Foods rich in Omega-3 fatty acids, as well as garlic, cumin, cloves, and turmeric are the main foods that can reduce the number of platelets in the blood.
Platelet donation
Anyone between the ages of 18 and 60 can become a platelet donor; their total weight must be at least 50 kg. The platelet count in his clinical blood test should be more than 150 thousand units/μl. The procedure lasts about 1.5 hours and is absolutely safe. All the requirements that apply to regular blood donation also apply to platelet donation.
The donor must be healthy and have sufficiently prominent ulnar veins.
Ideally, the blood types of the donor and recipient (that is, the one receiving the blood) should match. But individuals who have a different blood type from the recipient can also donate blood. The donor must stop taking aspirin and its derivatives at least 48 hours before the procedure. The interval between the procedure for donating whole blood (this procedure is called blood donation) and donating platelets using the apheresis method should be at least 4 weeks. During the donation procedure, disposable kits are used. Links: 1- What are Platelets? 2- Platelet Disorders 3- Thrombocytosis
Treatment
Treatment for this condition is primarily aimed at eliminating its cause. There are no general recommendations for such patients. Among the primary forms of the disease, the most clear treatment regimens have been developed for patients with essential and polycythemia vera.
They are divided into 3 categories:
- Patients with a high risk of developing complications (over 60 years of age, with a history of thrombosis or with a platelet count exceeding 1500 billion per liter). They are prescribed hydroxyurea drugs.
- Patients in the intermediate group are persons 40-60 years old, suffering from diabetes mellitus, hypertension, with a platelet concentration of 1000-1500 billion per 1 liter, having an elevated level of cholesterol in the blood or a bad habit - smoking. Interferon or Anagrelide drugs are used
- Low-risk group - patients under 60 years of age who do not have the risk factors listed above. Patients of all groups are shown Aspirin and other anticoagulants.
This is interesting: How is a stomach cyst manifested and treated?
Drug therapy
The main groups of drugs and treatment regimens are listed in the table below.
| Name | Main pharmacological effect | Dosage, per day | Average price, rub. |
| Hydroxyurea (hydroxyurea, hydroxyurea medac) | Reduction of megakaryocytes Antitumor effect. | 15-20 mg per 1 kg of body weight | 1010 |
| Anagrelide | Deactivation of megakaryocyte maturation and platelet formation. | 1-3 mg | 10500 |
| Thromboreductin | 1 mg (in 2 doses) | 47000 | |
| Interferon alfa (Altevir) | Myelosuppression – decreased levels of platelets and leukocytes. | 500 thousand IU | 1200 |
| Acetylsalicylic acid | Prevention of thrombosis. | 40-325 mg | 150 |
| Clopidogrel | 75 mg | 200 |
For some groups of patients, special treatment regimens are used:
- pregnant women - interferon alpha, low doses of Aspirin, constant monitoring;
- patients with thrombosis of large blood vessels - plateletpheresis, anticoagulants, Hydroxyurea, Interferon alfa, surgery;
- preparation for surgery – Hydroxyurea;
- patients with severe itching of the skin - janus kinase inhibitors (Tofacitinib and others), Interferon alfa, photochemotherapy.
Folk remedies
Thrombocytosis, the causes of which in adults can be associated with both physiological and pathological conditions, is dangerous primarily due to thrombotic complications.
To prevent blood clots, you can use the following folk remedies:
- Ginger tea. 1 tbsp. l. chopped root pour 1 tbsp. boiling water and cook over low heat for 5-10 minutes. Cool, drink 3 times a day, 1/3 tbsp. To give a sweeter taste, you can add 1 tsp. honey After 5-7 days of use, take a break for 2-3 days, then continue treatment.
- Garlic tincture. Peel and chop 6-5 cloves of garlic. Pour them with 1 tbsp. vodka and leave in a dark place for 1 week. Take ½ tsp. 2 times a day.
- 50 g of mulberry roots (this plant is also called mulberry) in a blender or on a grater. Place them in a saucepan, add 1.5 liters of water, and after boiling, cook over low heat for 15 minutes. Then cool, strain, drink ½ tbsp. 3 times a day before meals for 10 days, then take a break for 2-3 days. The decoction can be stored in the refrigerator for no more than 3 days.
- Fresh green horse chestnut peel, removed from 5-6 fruits, pour ½ liter of vodka and leave for 1 week. Strain, dilute 40 drops in 1/3 tbsp. water, add a little honey if necessary. Take 3 times a day for 2-3 weeks.
Thrombocytapheresis
Thrombocytapheresis is a hardware technique that is used to isolate a fraction of platelets from the patient’s blood. Most often, this procedure is used for donation, but in some cases it is also prescribed for medicinal purposes.
To do this, blood is taken from the patient (usually from a vein in the elbow), then it is passed through a centrifuge of a special apparatus in which platelets are separated, anticoagulants are introduced into the blood and fed back into the patient’s body.
Thrombocytapheresis is ineffective in people with essential thrombocythemia and polycythemia vera, since the decrease in platelet levels is short-term. This technique is most often used to urgently reduce platelet concentrations during severe bleeding and in preparation for surgery. In the latter case, the procedure can be carried out daily.
Hirudotherapy
Hirudotherapy is one of the methods for the prevention and treatment of thrombosis associated with thrombocytosis. The glands of the head part of medicinal leeches contain hirudin, a substance that prevents blood clotting and also has an analgesic and anti-inflammatory effect.
Thanks to it, the thrombin enzyme is inactivated in the human body.