1How does the heart rest?
The work cycle of the heart
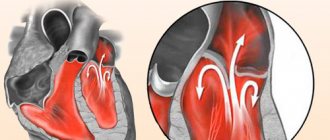
The heart is a unique organ, if only because it works and rests at the same time. The thing is that the chambers of the heart, the atria and the ventricles, contract alternately. At the moment of contraction (systole) of the atria, relaxation (diastole) of the ventricles occurs, and vice versa, when the turn of ventricular systole comes, the atria relax.
So, diastole of the left ventricle is the moment when it is in a relaxed state and is filled with blood, which, with further cardiac contraction of the myocardium, is expelled into the vessels and distributed throughout the body. The work of the heart depends on how fully relaxation or diastole occurs (the volume of blood entering the chambers of the heart, the volume of blood ejected from the heart into the vessels).
Classification of violation
In its development, left ventricular diastole dysfunction goes through several stages. Each of them has its own distinctive features and is characterized by varying degrees of danger.
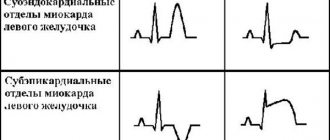
This is the initial stage of the pathology. Type 1 diastolic dysfunction of the left ventricular chamber correlates with a slightly delayed relaxation phase. Most of the blood enters the cavity during the process of relaxation during contraction of the left atrium. A person does not feel the manifestation of violations; obvious signs can only be detected by echocardiography. This stage is also called hypertrophic, since it occurs against the background of myocardial hypertrophy.
- Moderate pseudonormal stage (type 2).
The ability of the left ventricle to relax is further impaired. This is reflected in cardiac output. To compensate for the lack of blood flow, the left atrium works in an enhanced mode. This phenomenon is accompanied by increased pressure in this cavity and an increase in the size of the muscle wall. Now the saturation of the left ventricle with blood is ensured by the pressure difference inside the chambers. A person experiences symptoms that indicate pulmonary congestion and heart failure.
- The stage is restrictive, with a severe degree of impairment (type 3).
The pressure in the atrium, located on the left, increases significantly, the walls of the left ventricle thicken and lose flexibility. The disorders are accompanied by severe symptoms of a life-threatening condition (congestive heart failure). Pulmonary edema and an attack of cardiac asthma are possible.
2What is diastolic dysfunction?
Left ventricular diastolic dysfunction is a complex medical term at first glance. But it’s easy to understand it, understanding the anatomy and work of the heart. In Latin dis - violation, functio - activity, function. So, dysfunction is a disruption of function. Diastolic dysfunction is a dysfunction of the left ventricle in the diastole phase, and since relaxation occurs in diastole, a violation of diastolic dysfunction of the left ventricle is associated precisely with a violation of the relaxation of the myocardium of this cardiac chamber. With this pathology, the ventricular myocardium does not relax properly, its filling with blood slows down or does not occur in full.
Forecast
Violation of the diastolic function of the left ventricle cannot be completely stopped, but with adequate drug correction of circulatory disorders, treatment of the underlying disease, proper nutrition, work and rest schedule, patients with such a disorder live a full life for many years.
Despite this, it is worth knowing that cardiac cycle disturbance is a dangerous pathology that cannot be ignored. If it progresses poorly, it can lead to a heart attack, stagnation of blood in the heart and lungs, and swelling of the latter. Complications are possible, especially with severe dysfunction: thrombosis, pulmonary embolism, ventricular fibrillation.
In the absence of proper treatment, severe dysfunction with severe CHF, the prognosis for recovery is unfavorable. In most of these cases, it ends in the death of the patient.
With regular proper treatment, dietary adjustments with limited salt, control over the condition and level of blood pressure and cholesterol, the patient can count on a favorable outcome, prolongation of life, and an active one.
How dangerous is the disease?
Type 1 left ventricular diastolic dysfunction is caused by a fall in ejection fraction, which subsequently leads to a marked decrease in stroke volume. To prevent stagnation of blood in the lungs and compensate for dilatation, the systolic volume of the ventricle begins to increase. If such a protective reaction of the body does not follow, then there is a clear threat of pulmonary hypertension (repeated), and the load on the other ventricle (right) also increases significantly, which subsequently leads to a decrease in its volume.
What kind of disease?
Diastolic dysfunction of this part of the heart is a significant decrease in its ability to drive blood into its cavity from the pulmonary artery. In other words, such a pathological condition leads to the inability to ensure normal blood circulation.
Thus, type 1 left ventricular diastolic dysfunction is a severe heart disease, which is characterized by the insufficient ability of the mentioned part of the organ to relax during diastole. It should be especially noted that it can take approximately 0.4 seconds. This time is quite enough to completely restore the tone and energy content of the heart muscle.
Diastolic dysfunction and diastolic heart failure
Impaired diastolic function
The volume of blood entering the lower chambers of the heart decreases, which increases the load on the atria, compensatory filling pressure increases in them, and pulmonary or systemic congestion develops. Impaired diastolic function leads to the development of diastolic failure, but often diastolic heart failure occurs with preserved systolic function of the left ventricle.
In simple words, the earliest pathological manifestation of ventricular function is their dysfunction in diastole; a more serious problem against the background of dysfunction is diastolic failure. The latter always includes diastolic dysfunction, but not always with diastolic dysfunction there are symptoms and clinical signs of heart failure.
The concepts of “diastolic dysfunction” and “diastolic heart failure” in modern cardiology are not synonymous, i.e., they mean various forms of impairment of the pumping function of the heart: diastolic heart failure always includes diastolic dysfunction, but its presence does not yet indicate heart failure.
Ventricular dysfunction may result from weak ventricular contraction (systolic dysfunction), abnormal relaxation of the ventricles (diastolic dysfunction), or abnormal thickening of the ventricular walls, resulting in obstruction of blood flow.
One of the main problems of modern cardiology is chronic heart failure (CHF).
In traditional cardiology, the main cause of the onset and development of CHF was considered to be a decrease in myocardial contractility. However, in recent years it has become common to talk about the different “contributions” of systolic and diastolic dysfunction to the pathogenesis of chronic heart failure, as well as about systole-diastolic relationships in heart failure. In this case, disturbances in diastolic filling of the heart play no less, and perhaps even greater, role than systolic disorders.
Treatment
Therapy depends on the stage and severity of the disease; it is strictly contraindicated to prescribe this or that drug to yourself, because the heart is a vital organ, so it is better not to harm your health by improper actions.
If there are no symptoms of deficiency, your doctor may recommend taking angiotensin-converting enzyme (ACE) inhibitors. It regulates blood pressure and protects target organs in this disease.
Target organs are those that suffer primarily from dysfunction of the cardiovascular system, that is, they are the first “targets” along the path of blood failure. These include the kidneys, brain and spinal cord, heart, blood vessels and retina.
By taking ACE inhibitors daily at a dose prescribed by your doctor, you can reduce the risk of complications in target organs and prevent the development of chronic heart failure. Such drugs include Enalapril, Quadropril, Lisinopril. It is difficult to say which is better; everything is discussed at an appointment with a therapist or cardiologist and prescribed based on symptoms and past experience with medication.
If you are intolerant to ACE inhibitors or for some objective reason the doctor has decided that they will not help you, ARA II (angiotensin receptor antagonists) are prescribed. They have exactly the same properties. These include Losartan, Valsartan and others.
If signs of the disease are pronounced, even more drugs are prescribed to relieve symptoms:
- diuretics (diuretics) – reduce the volume of circulating blood by removing excess fluid;
- beta blockers - make the heart rate slower, reducing the load on the organ;
- cardiac glycosides - increase the force of heart contractions;
- Aspirin - prescribed to reduce the risk of blood clots and, therefore, ischemia;
- statins – carry out lipid control in the blood by normalizing cholesterol fractions that are harmful to blood vessels.
Left ventricular diastolic dysfunction
Arterial hypertension
Violation of the diastolic function of the ventricular myocardium can occur due to an increase in its mass - hypertrophy, or a decrease in the elasticity and compliance of the myocardium. It should be noted that almost all heart diseases affect the function of the left ventricle to one degree or another. Most often, diastolic dysfunction of the left ventricle occurs in diseases such as hypertension, cardiomyopathies, ischemic disease, aortic stenosis, arrhythmias of various types and origins, and pericardial disease.
It should be noted that loss of elasticity and increased rigidity of the muscular wall of the ventricles is observed during the natural aging process. Women over sixty are more susceptible to this disorder. High blood pressure leads to increased load on the left ventricle, causing it to increase in size and the myocardium to hypertrophy. And the altered myocardium loses the ability to relax normally; such disorders first lead to dysfunction and then to failure.
Left atrium enlargement
There are three types of left ventricular dysfunction.
Type I - Type 1 left ventricular diastolic dysfunction is classified as mild in severity. This is the initial stage of pathological changes in the myocardium, its other name is hypertrophic. In the early stages, it is asymptomatic, and this is its insidiousness, since the patient does not suspect problems with the heart and does not seek medical help. With type 1 dysfunction, heart failure does not occur, and this type is diagnosed only with the help of echocardiography.
Type II - dysfunction of the second type is characterized as moderate in severity. In type II, due to insufficient relaxation of the left ventricle and a reduced volume of blood ejected from it, the left atrium takes on a compensatory role and begins to work “for two,” which causes an increase in pressure in the left atrium, and subsequently its increase. The second type of dysfunction may be characterized by clinical symptoms of heart failure and signs of pulmonary congestion.
Type III - or restrictive type dysfunction. This is a severe disorder, which is characterized by a sharp decrease in the compliance of the ventricular walls, high pressure in the left atrium, and a clear clinical picture of congestive heart failure. In type III, sudden deterioration of the condition leading to pulmonary edema and cardiac asthma is not uncommon. And these are serious life-threatening conditions that, without proper emergency treatment, often lead to death.
To date, a large number of facts have accumulated that cast doubt on the “exclusive” role of systolic dysfunction as the main and only hemodynamic cause responsible for the occurrence of CHF, its clinical manifestations and the prognosis of patients with this form of pathology. Modern studies indicate a weak connection between systolic dysfunction and clinical manifestations and prognosis of patients with chronic heart failure.
Insufficient contractility and low left ventricular ejection fraction do not always clearly determine the severity of decompensation, exercise tolerance, and even the prognosis of patients with CHF. At the same time, significant evidence has been obtained that indicators of diastolic dysfunction, to a greater extent than myocardial contractility, correlate with clinical and instrumental markers of decompensation and even with the quality of life of patients with CHF. At the same time, a direct cause-and-effect relationship between diastolic disorders and the prognosis of patients with chronic heart failure has been established.
All this forced us to reassess the importance of left ventricular systolic dysfunction as the only and obligate factor of CHF, and to take a fresh look at the role of diastolic disorders in the pathogenesis of this form of pathology.
Of course, at present, systolic function, which is assessed mainly by the left ventricular ejection fraction, is still assigned the role of an independent predictor of the prognosis of patients with CHF. Low left ventricular ejection fraction remains a reliable marker of myocardial damage, and assessment of contractility is mandatory to determine the risk of cardiac surgery and can be used to determine the effectiveness of treatment.
So far, the assessment of diastolic function has not yet become a mandatory procedure, which is largely due to the lack of proven and accurate methods for its analysis. Nevertheless, there is no doubt now that it is diastolic disorders that are responsible for the severity of cardiac decompensation and the severity of clinical manifestations of chronic heart failure.
As it turned out, diastolic markers reflect the functional state of the myocardium and its reserve (ability to perform additional load) more accurately than systolic ones, and can also be used more reliably than other hemodynamic parameters to assess the quality of life and the effectiveness of therapeutic measures.
In addition, there are all prerequisites for the use of diastolic indices as predictors of prognosis in heart failure. The observed trend towards a shift in emphasis from systolic to diastolic dysfunction is not surprising if we look at this issue from an evolutionary point of view.
In fact, if we compare the relationship between the processes of contractility and relaxation of the myocardium with other similar so-called. antagonistic processes in the body (for example, pressor and depressor systems for regulating blood pressure levels, the process of excitation and inhibition in the central nervous system, blood coagulation and anticoagulation systems, etc.
In continuation of this comparison, the contractility of the myocardium is “more powerful” than its relaxation and it cannot be otherwise: the heart is first of all “obliged” to contract, and then to relax (“diastole without systole is meaningless, and systole without diastole is unthinkable”). These and other similar “inequalities” are evolutionarily developed, and the superiority of one phenomenon over another has a protective and adaptive significance.
Naturally, with the body’s increased demands on these and other “antagonists,” dictated by the living conditions of the body, first of all, “the weak link drops out of the game,” which is what is observed in the heart. Left ventricular diastolic dysfunction often occurs before systolic dysfunction.
Let us consider in more detail the pathogenetic essence of the concepts “systolic dysfunction” and “diastolic dysfunction”, taking into account the fact that these concepts are not found very often in domestic medical educational and educational materials (in any case, much less often than in foreign similar literature).
Most often, heart failure is associated with a decrease in the contractile function of the heart. However, in about a third of patients, symptoms of heart failure develop despite virtually normal left ventricular function as a result of abnormal filling, which is commonly called diastolic dysfunction (in this case, left ventricular dysfunction).
The main criterion for left ventricular diastolic dysfunction is its inability to fill with a volume of blood sufficient to maintain adequate cardiac output at normal mean pulmonary venous pressure (below 12 mmHg). According to this definition, diastolic dysfunction results from cardiac damage such that increased pressure in the pulmonary veins and left atrium is required to adequately fill the left ventricular cavity.
What can prevent full filling of the left ventricle?
Two main reasons have been established for a decrease in its filling with blood during diastolic dysfunction: 1) impaired active relaxation (“relaxability”) of the left ventricular myocardium and 2) decreased compliance (“extensibility”) of its walls.
It is likely that diastolic dysfunction is an extremely common form of pathology. According to the Framingham study (note in parentheses: everything that is known in the medical world about the risk factors for any form of heart and vascular pathology was obtained in this study), such an indirect marker of diastolic dysfunction as left ventricular hypertrophy is observed in 16-19% of the population and in at least 60% of patients with hypertension.
Diastolic dysfunction is more often found in older people, who are less resistant to this disease and coronary heart disease, which causes diastolic disorders. In addition, with age, the mass of the myocardium increases and its elastic properties deteriorate. Thus, in the future, due to the general aging of the population, the role of diastolic dysfunction as a precursor of chronic heart failure will obviously increase.
The contraction of cardiomyocytes is an active process that is impossible without the consumption of energy from macroergic compounds. This provision equally applies to the process of relaxation of cardiomyocytes. By analogy with the concept of “contractility,” this ability should be called “relaxability” of the myocardium.
Contractility and relaxation of the myocardium are two sides of the same coin, i.e. cardiac cycle. As already noted, the diastolic filling of the chambers of the heart, normally and when it is damaged, is determined by two main factors - the relaxability of the myocardium and the compliance (rigidity, extensibility) of the chamber wall.
a) load on the myocardium during its contraction;
b) loads on the myocardium during its relaxation;
c) complete separation of actinomyosin bridges during diastole, determined by the reuptake of Ca2 by the sarcoplasmic reticulum;
Signs of deviation
This condition very often leads to the development of secondary pulmonary arterial and venous hypertension. This pathological condition can manifest itself in the following:
- persistent cough (often paroxysmal);
- nocturnal dyspnea (paroxysmal);
- dyspnea.
What other signs are used to determine type 1 left ventricular diastolic dysfunction? Symptoms of such a deviation may not manifest themselves for a long time. However, as the disease progresses, patients begin to experience symptoms such as:
- regular pain in the heart, which is paroxysmal in nature (as with coronary artery disease);
- swelling of the lower extremities;
- shortness of breath (can be observed even at rest);
- spastic phenomena;
- feeling of lack of air.
If these symptoms occur, you should definitely consult your doctor. After all, the sooner this pathological condition is identified, the easier it is to take control. If the presented disease is detected too late, then its treatment will last a very long time, with the use of a large number of medications and all the necessary procedures.
How to cure?
Currently, there is no single treatment regimen that would be recognized by most specialists. This is partly due to the fact that this disease is rather difficult to diagnose. As mentioned above, such a deviation occurs asymptomatically for a very long time, as a result of which the patient seeks medical help too late.
So what should you do if you have type 1 left ventricular diastolic dysfunction? Treatment of such a disease comes down to eliminating the causes that provoke negative tendencies. Thus, patients need:
- cure existing ischemia;
- normalize heart rate;
- lower blood pressure.
Among other things, if such a pathological condition is detected, the patient is prescribed drugs from the ACE blocker group. Most often, the choice of specialists falls on Lizonopril. It is prescribed in the form of tablets of 20-40 milligrams per day (in two doses).
Good results in the treatment of this deviation can be achieved by using calcium blockers. Thus, both drug groups lower blood pressure, significantly reduce the oxygen demand of cardiac tissues, and also stop and reduce left ventricular hypertrophy. By the way, as a result of taking these drugs, the work of heart diastole improves, which subsequently leads to normalization of hemodynamics.
The best results in the treatment of this disease were observed when potassium-sparing diuretics were combined with cardiac drugs. If urgently needed, other antihypertensive medications can be used.
Causes
Factors leading to the development of diastolic dysfunction worsen the relaxation process and reduce the elasticity of the walls of the left ventricle, mainly due to the development of myocardial hypertrophy (thickening).
The following diseases lead to myocardial hypertrophy:
- hypertrophic cardiomyopathy;
- hypertonic disease;
- aortic stenosis (narrowing of the aortic mouth).
In addition, the cause of hemodynamic disorders can be diseases such as:
- constrictive pericarditis – is a thickening of the pericardium, resulting in compression of the chambers of the heart;
- primary amyloidosis – amyloid deposition causes atrophy of muscle fibers and decreased myocardial elasticity;
- pathology of the coronary vessels, leading to the development of chronic coronary heart disease and the development of myocardial rigidity due to scar changes.
Due to the development of compensatory pulmonary hypertension, the preload on the right side of the heart increases, and diastolic dysfunction of both ventricles is formed.
Risk factors include conditions such as obesity, diabetes mellitus
6Symptoms
Shortness of breath during physical activity
In the early, initial stages of development of diastolic dysfunction, the patient may have no complaints. It is not uncommon for diastolic dysfunction to be detected as an incidental finding during echocardiography. In later stages, the patient is concerned about the following complaints:
- Dyspnea. At first, this symptom is a concern only during physical activity; as the disease progresses, shortness of breath may appear with minor exertion, and then even bother you at rest.
- Heartbeat. An increase in heart rate is not uncommon with this disorder of the heart. In many patients, heart rate reaches submaximal values even at rest and increases significantly during work, walking, and excitement.
Dry cough
- Cough. A persistent, obsessive, dry cough, coughing are signs of incipient congestion in the lungs. Often, such patients spend months treating a non-existent bacterial or viral infection, assuming they have bronchitis or another lung pathology. In fact, there is a violation of diastolic function with manifestations of circulatory failure.
- Feelings of lack of air. A common complaint among patients with this pathology is a feeling of chest compression and the inability to breathe deeply.
- Fatigue, poor exercise tolerance. Patients note with surprise that previously easily tolerated physical activity now becomes difficult for them and is accompanied by deterioration in well-being and fatigue.
Diagnostic methods
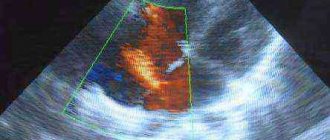
Diagnosis of myocardial dysfunction
In order to receive full information about the patient’s health status, he will be referred for the following studies:
- two-dimensional echocardiography;
- radionuclide ventriculography;
- electrocardiography;
- chest x-ray.
The listed methods will allow you to evaluate structural changes in all parts of the heart, study the frequency and intensity of contraction of the organ, and obtain information about the volume of blood pumped. Doctors will also determine whether the person has signs of pulmonary hypertension, which is quite important in this case.
7Diagnostics
Echocardiography
Diastolic dysfunction is detected mainly during an instrumental examination method such as echocardiography. With the introduction of this method into the practice of clinical doctors, the diagnosis of diastolic dysfunction began to be made many times more often. EchoCG, as well as Doppler EchoCG, allows us to identify the main disorders that occur during myocardial relaxation, the thickness of its walls, assess the ejection fraction, stiffness and other important criteria that allow us to establish the presence and type of dysfunction.