An infarction of the posterior wall of the heart is diagnosed if, against the background of an acute circulatory disorder, oxygen starvation occurs in the muscle, due to which the muscle tissue of the posterior wall of the left ventricle begins to die.
This condition is accompanied by acute pain and poses a real threat to the patient’s life. The condition most often occurs in people over 40 years of age. In men, damage to the posterior wall occurs 5 times more often than in women. The number of deaths among representatives of the stronger sex is also higher.
Causes
A heart attack in most patients occurs against the background of coronary heart disease.
The main reasons for the development of the disease preceding the infarction and necrosis itself are:
- elevated cholesterol levels, when a significant atherosclerotic plaque forms on the walls of the coronary arteries, impairing patency,
- hypertension, in which the body is exposed to high blood pressure for a long time, causing serious depletion of myocardial tissue,
- age-related changes in heart tissue.
It is also worth highlighting the reasons that increase the risk of a heart attack.
These are:
- smoking,
- alcohol abuse, including beer,
- obesity,
- lack of physical activity,
- lack of oxygen due to rare exposure to fresh air,
- work in hazardous industries,
- heavy physical overload,
- severe stress,
- chronic fatigue,
- chronic lack of sleep.
By eliminating the influence on the body of factors that predispose to lesions of the posterior wall of the ventricle of the heart, the risk of developing a heart attack can be significantly reduced.
Etiology
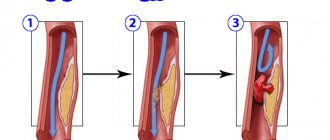
In most cases, infarction leads to obstruction of one or the coronary arteries oxygenating the myocardium.
This obstacle is associated with the thickening of atheromal plaques and their rupture, leading to the formation of a blood clot. The thickening of atheroma plaques is especially favored by:
- high blood pressure,
- smoking,
- diabetes,
- obesity,
- dyslipidemia.
Classification of the disease
Myocardial infarction refers to an acute form of cardiac ischemia. This pathological condition is divided into small-focal and extensive. With the first type of lesion, the patient’s likelihood of recovery is much higher.
With an extensive infarction, if more than 50% of the tissues of the posterior wall of the myocardium are damaged, the organ cannot work, and cardiogenic shock and death of the patient occurs.
The disease is also divided by localization.
- Posterior phrenic infarction. With this form, the posterior wall of the heart ventricle is damaged at the point of contact with the diaphragm. If the pathology is caused by blockage of the lower coronary vessel, then the necrotic lesion is extensive and the risk of death of the patient is high.
- Posterobasal infarction - damage affects the area adjacent to the base of the heart. More often there is a small focal form of necrosis.
- Posterolateral infarction. The disorder extends immediately to the lateral and posterior wall of the left ventricle.
The localization of the focus of necrosis depends on which artery and which vessel have ceased to function normally, and which area of the heart has begun to experience acute oxygen starvation.
How to diagnose?
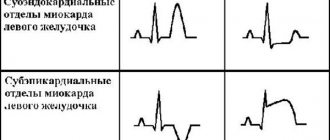
This type of heart attack is very difficult to diagnose. In rare cases, an ECG can only show signs of angina. And since the ECG may not show such a myocardial infarction at all, a full examination needs to be done. It will include systematic survey procedures along with comprehensive analysis.
If the patient has only a third of the total area affected, then the symptoms of a heart attack may not appear at all. Therefore, during the examination, doctors carefully study the following parameters:
- the time period during which the patient discovered his illness,
- duration of pain, because myocardial infarction causes attacks in patients lasting more than 15 minutes,
- note how the patient’s body reacts to nitroglycerin,
- changes in pain when the patient's body position changes.
Of course, along with all of the above, the cardiogram data is constantly updated, ECG indicators are compared and carefully checked.
Only when the patient undergoes the entire complex of examinations, which will give a complete picture of what is happening, can one understand whether there is a posterior myocardial infarction, because one cannot rely on data of an uncertain date. And based on the new data obtained, it is possible to make a further prognosis, prescribe treatment, determine the consequences and understand what kind of rehabilitation is needed.
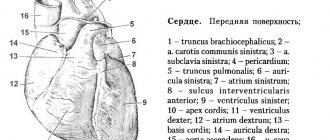
Do not forget that the wall has two sections - upper and lower, known as basal and diaphragmatic. And depending on which of these sections is affected in the patient, a diagnosis will be made: posterobasal myocardial infarction or posterodiaphragmatic infarction.
There may also be extensive infarction of the posterior wall of the heart, which involves both sections and sections located laterally. These sections are located on the lateral surface of the heart.
You cannot self-medicate with such a complex disease. This will only cause harm and lead to negative consequences that will cause additional complications.
Symptoms
The symptoms of the disease are similar to those that appear with lesions of other parts of the heart and the development of a necrotic process.
The fact that there is damage to the main organ in the body is indicated by certain signs of a disorder:
- Pain. Most people experience very intense chest pain that radiates to the shoulder and upper abdomen. In smokers, the pain syndrome affects the lung area. There is no exact localization of pain. If the patient does not receive help, the condition worsens and the syndrome intensifies, leading to breathing problems. Nitroglycerin cannot remove it.
- Arrhythmia. Appears due to a disturbance in the rhythm of heart contractions due to the shutdown of part of the muscle due to necrosis.
- Profuse, sticky cold sweat, appearing immediately with the appearance of the first pain.
- Trembling in the limbs, which is provoked by pain and poor circulation.
- Severe general weakness, during which the patient’s vision becomes dark and fainting is possible.
- A sharp decrease in pressure.
The more intense the symptoms of the disease, the larger the area of necrosis that forms. Preserving the life of a patient is largely determined by how quickly medical care is provided.
How long they live after a heart attack depends on the degree of heart damage, the presence of additional pathologies in the patient and the general condition of the body. In most cases, if the therapy was carried out correctly, a person can live a full life while maintaining a gentle rhythm.
Infarction of the posterior wall of the heart: causes, symptoms, diagnosis, consequences
Posterior myocardial wall infarction is a pathological condition caused by the death of heart tissue due to the fact that oxygen has not been supplied to it for a long time (at least half an hour).
A heart attack of the posterior wall of the heart occurs in humans for various reasons, the main one being a blood clot blocking a coronary artery.
Development mechanism, types
The pathological condition is caused by the appearance of foci of ischemic necrosis affecting the heart muscle. The disease has an unfavorable prognosis; 10 percent of patients who have suffered a posterior myocardial infarction die within 12 months after the attack. In other patients, the possibility of another heart attack increases significantly.
According to statistics, pathological changes most often occur in the anterior wall of the left ventricle of the heart; much less often, a heart attack affects the posterior region of the ventricle or the septum between them.
Patients who have suffered pathology, despite proper treatment and a long period of rehabilitation, feel the consequences of a heart attack for a long time. All types of the disease are characterized by serious complications and severe course.
All affected areas of the myocardium can no longer be restored. Fibrous tissue that appears at the site of necrosis is unable to perform its functions. A patient who has suffered this type of myocardial infarction must carefully monitor his health throughout his life, follow a diet, and take medications prescribed by a doctor.
This type of IHD (coronary heart disease) has the following localization:
- In the posterior diaphragmatic region (posterior wall of the heart adjacent to the diaphragm). Blockage of the inferior coronary vessel leads to large-focal lesions.
- In the posterobasal region (the upper wall of the heart adjacent to its base). In this case, there is a violation of blood circulation in the vessels and arteries that supply the organ with blood and oxygen.
Types of disease by degree of damage:
- Extensive tissue damage. With the development of such a pathological condition, the blood flow is sharply blocked, and an acute attack can lead to the death of the patient.
- Small focal tissue damage. In the initial stage, the pathology almost does not affect the functioning of the heart; with adequate treatment, the patient’s chances of survival are very high.
Causes
The number of true reasons that lead to the fact that the patient’s heart or atria begins to be insufficiently supplied with oxygen is large. Among them:
- increased cholesterol levels caused by obesity or poor diet, leading to the formation of cholesterol plaques on the walls of blood vessels;
- persistent hypertension, causing rapid myocardial depletion;
- bad habits (tobacco smoking, excessive alcohol consumption), leading to oxygen starvation of the body and IVS of the heart (hypertrophy of the interventricular septum);
- lack of exercise, leading to blood stagnation;
- age criteria (over the years, vascular walls lose flexibility, which leads to poor supply of blood and oxygen to the heart).
Characteristic symptoms
- Cardiac pathology of the posterior wall of the myocardium in its manifestation differs little from other types of infarction. The patient feels severe pain in the chest area. The pain may radiate to the left limb, subscapular region. The attack is often accompanied by the following symptoms:
- arrhythmia, expressed in disruption of the heart;
- sticky cold sweat suddenly appearing on the face;
- trembling in the limbs;
- low blood pressure;
- general weakness of the body.
An analysis of the condition of many patients showed that with posterobasal pathology, the characteristic symptoms are blurred, and the course of an acute attack is not accompanied by pain.
Also read: How to treat myocardial infarction at home
Diagnosing such a pathology is somewhat difficult even when using an ECG; due to atypical symptoms, the disease is often confused with a stomach disease such as gastritis.
How is it diagnosed?
Diagnosing pathology of the posterior wall of the heart is quite difficult; the doctor studies the ECG results, paying attention to the following indicators:
- If the Q wave is detected in the AVF, third and second leads, this confirms a posterior phrenic infarction. This is also indicated by the characteristic rise of the T wave on the cardiogram.
- A smooth transition of R in leads V1, V2, V3 indicates the onset of a posterobasal infarction.
- ST segment elevation indicates damage to the wall of the left ventricle of the heart.
Other diagnostic techniques include:
- Prescribing general and biochemical blood tests. On the first day, it is important to monitor the increase in the number of neutrophil leukocytes; its peak occurs on the third day of the attack.
- Purpose of radiography. An X-ray helps to identify blood stagnation in the patient’s chest area, which directly indicates the presence of pathology.
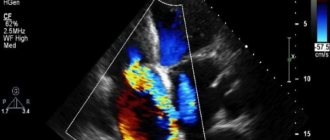
- The purpose of echocardiography, with the help of the study, it is possible to clarify the picture of the disease and identify hidden ischemic changes in the heart.
Treatment
Treatment of pathology is carried out in several directions:
- therapeutic treatment with medications aimed at restoring normal blood flow through damaged vessels, relieving pain and relieving consequences;
- surgical intervention that gives the most effective result; in modern medicine the following techniques are used:
Consequences
A person who wants to live a long time must take care of his health, because a pathological complication in the form of myocardial infarction has many consequences.
Complications to be aware of:
- Transmural (extensive) infarction, affecting the entire thickness of the myocardium, can lead to rupture and even immediate death.
- With pathology that has developed in the left ventricle of the heart, fibrillation may begin, which is also a serious complication, often leading to death.
- A posterolateral infarction affecting a large area of the heart can result in protrusion of the anterior wall of the cardiac chamber. Thinning caused by pathology leads to the development of an acute aneurysm. Recovery of a patient with such a complication takes a lot of time.
Thromboembolism is a complication consisting of blockage of a coronary vessel by a blood clot (thrombus), leading to impaired cerebral circulation, lung damage, and problems in the diaphragmatic region of the gastrointestinal tract. Rehabilitation of such a patient takes a very long time.
Prevention
The prognosis for infarction of the posterior wall of the heart will depend on several signs:
- how much tissue was damaged during the pathological condition;
- what is the area of necrotic lesion;
- how quickly the patient was brought to the clinic;
- How quickly the history (anamnesis) of the disease was collected and adequate treatment was prescribed.
It is important not only to consult a doctor in time if a myocardial infarction occurs and complete the full course of treatment, following all the doctor’s instructions, but also to adhere to preventive measures that are aimed at strengthening the heart muscle.
Prevention of myocardial infarction is a sure way to avoid pathological changes in the heart.
Every person should:
- start exercising periodically;
- review your diet;
- get rid of bad habits;
- avoid nervous tension;
- Monitor your heartbeat by regularly visiting a cardiologist.
Diagnostic measures
To make a diagnosis, a history is taken, which gives doctors enough information to suggest what caused severe symptoms. An ECG and blood biochemistry are also prescribed. If the patient's condition is satisfactory, then an additional chest x-ray and echocardiogram are performed.
Once the diagnosis is made, the necessary therapy begins. The patient is subject to mandatory hospitalization in the intensive care unit.
Symptoms
Doctors identify characteristic signs of myocardial infarction of the anterior wall, which all patients need to pay attention to:
- pain – heart pain is the main symptom of a heart attack. The typical localization of pain is just behind the sternum, but it can radiate to the left arm, shoulder blade, or half of the jaw. Usually attacks begin during the day, the duration of attacks is half an hour or more;
- blue skin – cyanosis, which occurs when there is a lack of oxygen in the body;
- coldness in the fingers of the extremities is the result of a “failure” of the heart muscle;
- breathing problems;
- weakness;
- state of panic - anxiety and panic are not characteristic signs of a heart attack, but they well illustrate the patient’s state of health;
- fainting.
Important! If a change in the anterior wall of the heart occurs according to an atypical scenario, patients may experience severe stomach pain, vomiting, memory problems, and the inability to concentrate on anything. For these symptoms, it is also necessary to call an ambulance.
These are the symptoms of a massive heart attack. But it is not always possible to recognize the signs of a small-focal heart attack, since the pathology has vague symptoms. Typically, signs of a microinfarction are pain and anxiety, but other symptoms may be absent.
Therapy
At the beginning, if possible, conservative treatment is carried out, in which drugs are used to dissolve the blood clot and reduce the heart's need for oxygen, as a result of which it is possible to stop the necrotic process.
They also make sure to use medications to relieve pain, which further aggravates the condition of the heart attack victim.
If treatment with conservative methods is useless, then surgical intervention is performed for myocardial infarction. This treatment gives quick results and allows you to normalize blood circulation in the heart in the shortest possible time.
One of four types of surgery is used:
- Coronary artery bypass surgery. During such an intervention, a new vessel with normal patency is created. For this purpose, a vessel taken from another part of the patient’s body is most often used.
- Installation of a special ring that prevents compression of the artery and restores its normal patency.
- Strengthening the heart walls at the risk of developing their protrusion using special polymer frames.
- In such a situation, suturing the heart wall if it is catastrophically thinned and there is a high risk of its rupture. The wall is strengthened by stitching with a special seam.
Which method of surgical treatment of the pathology will be used is determined by the attending physician. If the risk that the patient will not undergo surgery is high, then it is usually not performed, regardless of the severity of the condition.
What is a heart attack
Myocardial infarction is a sudden cessation of blood supply to the heart muscle. As a result, necrosis occurs - cardiomyocytes die and can no longer perform their function. The anterior wall of the heart is the most vulnerable - necrotic changes often appear here.
Usually the damage is so deep that doctors do not give comforting forecasts for a quick recovery and a complete return of the person to normal life. The consequences of anterior wall infarction are the development of left ventricular failure and cardiogenic pulmonary edema.
Important! Statistics say that every tenth patient with a heart attack of the anterior wall of the heart dies in the first year after the incident. Surviving patients remain forever at risk for the disease. Forty percent of patients are not transported by ambulance to the hospital, and every fifth patient admitted urgently dies in the clinic.
Complications of pathology
Damage to the posterior wall can also provoke a number of consequences, which also pose a great danger to the patient. Thus, a threat to life arises not only due to the primary pathology, but also due to the occurrence of complications.
The main negative consequences pose a danger to the patient’s life:
- Extensive infarction (acute transmural infarction). With such a lesion, the entire thickness of the myocardium is affected, and the likelihood of death is high, even if the patient receives all the necessary medical care.
- Atrial fibrillation - appears precisely when there is a violation in the left ventricle and often leads to the death of the patient.
- Transition of the lesion of the posterior wall into a posterolateral infarction with the spread of the necrotic focus. To recover from such a violation, the patient needs long-term rehabilitation, and in the future he will need to comply with many restrictions.
- Thromboembolism of the arteries of the heart or lungs - in most cases, the patient dies due to complications.
- Pulmonary edema.
- Ascites.
- Kidney failure.
The occurrence of complications largely depends on the general condition of the patient, and therefore it is not always possible to prevent their development even with immediate medical intervention. In the presence of complications, the prognosis is unfavorable.
Treatment of early or late complications
Treatment is expected to be as follows:
- Premature bradycardia - 0.5 mg Atropine intravenously.
- Ventricular premature beats - 1200 to 1600 mg lidocaine/24 hours IV and monitor potassium levels.
- Ventricular tachycardia - Xylocaine 2 mg/kg bolus or Cordarone 150 mg. External electric shock under the influence of reticulum is used as an ineffectiveness of such treatment in antiarrhythmic treatment that prevents relapses. In case of drug intolerance, this approach is also practiced.
- Ventricular fibrillation - electric shock, resuscitation and intensive antiarrhythmic treatment, sometimes combining 2 antiarrhythmic drugs.
Electrical conductivity disturbances in anterior myocardial infarction:
- Acute pulmonary edema or cardiogenic shock. Symptomatic treatment is carried out:
- sympathomimetic amines (a combination of dopamine - dobutamine, adrenaline), correction of acidosis,
- Furosemide in high doses,
- the use of mechanical assistance (ventilation, normalization of blood pressure and circulation, even emergency heart transplantation).
Other cases:
- Mitral valve rupture is a late complication. Introduction of an emergency prosthesis associated with revascularization.
- Pericarditis - non-steroidal anti-inflammatory drugs and a reduction in heparin doses by 2 times.
- The threat of relapse and spread of the pathological area is the resumption of primary therapy (aspirin, heparin).
- Secondary ventricular fibrillation - antiarrhythmic treatment.
- Residual ischemia - revascularization.
- Left ventricular aneurysm - surgical removal.
- Dressler's syndrome (post-infarction pericarditis of immunological origin) - non-steroidal anti-inflammatory drugs.
Provoking factors
Doctors call anterior wall infarction a largely “male” disease, although in older age groups the number of cases of diagnosing this condition in women increases. Often a hereditary factor is clearly visible, and this is associated with disorders of the blood vessels.
Risk factors for extensive damage to the anterior wall of the heart include:
- bad habits, in particular smoking;
- increased blood pressure;
- diabetes;
- increased amount of lipids/lipoproteins in the patient’s blood.