What is myocardial infarction?
The heart is a large muscular organ that creates normal blood supply to the entire body. Thanks to constant rhythmic contractions, the blood flow is continuous and supplies all organs and systems with a sufficient amount of oxygen and other useful microelements. However, often against the background of coronary heart disease (insufficient blood supply to some of its parts), a sharp stenosis (contraction) of the coronary artery occurs. Namely, it nourishes the myocardium. As a result of such a lack of nutrition, myocardial infarction occurs, that is, the work of one or more of its departments stops. As a result, the heart tissue surrounding the myocardium undergoes necrosis (dies). According to the ICD, the disease is classified in section I21 (diseases of the cardiovascular system).
Left ventricular myocardial infarction
To understand what a left ventricular infarction looks like, it is advisable to have a general understanding of the structure of the heart as a whole. So, the heart has several layers of tissue:
- Endocardium. These are the tissues lining all parts and cavities of the heart. The thickness of the endocardium, consisting of connective tissue and fibers, is no more than 0.5 mm.
- Myocardium. The layer of muscle that causes the heart to contract. The main composition of the myocardium is cardiomyocyte cells. They are not only responsible for the contractility of the heart, but also transmit bioelectric impulses at optimal speed.
- Epicardium. This is connective tissue that fits tightly to the myocardium.
When a heart stroke occurs, tissue dies to varying degrees depending on the type and stage of the stroke. And that is why, depending on the depth of necrosis, heart attacks are classified:
- Intramural. Tissue necrosis occurs only in the thickness of the myocardium.
- Transmural. Tissues become necrotic to the full depth (most often such a heart attack is large-focal).
- Subepicardial. Affects the myocardium only in the area of its junction with the epicardium.
- Subendocardial. Tissues die in the myocardium at the level of the junction with the endocardium.
Important : most often the patient experiences myocardial infarction of the left cardiac ventricle and interventricular septum (IVS) due to their insufficient blood supply by nature. Both the anterior/posterior and lower/upper walls can be affected by necrosis.
Infarction of the anterior wall of the left ventricle
With any type of large-focal infarction, the ECG (electrocardiogram) will show a Q wave, which is pathological. Therefore, large focal attacks are often called Q-infarction. It is worth noting here that Q-myocardial infarction of the anterior wall of the left ventricle most often occurs against the background of a blockage of the anterior artery, which branches off from the coronary artery on the left. Basically, with such an anterior or anterolateral impact, the following changes will be noted in electrocardiographic transcripts:
| Q wave | Its amplitude is equal to or slightly higher than the vibrational line of the R wave. |
| R-wave | Below or equal to the Q value. |
| T-wave | Negative |
| ST segment | Noted in the rise dynamics |
Infarction of the inferior wall of the left ventricle
Large-focal myocardial infarction of the lower wall of the left ventricle most often occurs due to impaired throughput of only the right coronary artery. Most often this occurs due to thrombosis of the artery lumen. This type of strike has a very rapid development. Literally a few hours after the start of the attack, all the consequences will be extremely dangerous for the patient, including death. The ECG also shows an abnormal ST segment and Q wave.
Infarction of the posterior wall of the left ventricle
Typically, myocardial infarction of the posterior wall of the left ventricle (LPW) causes tissue necrosis in this area of the heart. Necrosis occurs literally within half an hour from the onset of the attack. In most cases, damage to the posterior wall of the left ventricle is more difficult to diagnose, in contrast to damage by necrosis of the anterior wall. According to statistics, more than half of such attacks are not visible on a cardiogram. Most often, a cardiologist can only see signs of angina pectoris.
Features of infarction of the posterior wall of the heart and its differences from other types of pathology
Infarction of the posterior wall of the heart is a process of necrosis of tissues and cells located locally in the posterior part. The basis of this process is the cessation of blood circulation, which within half an hour leads to tissue necrosis.
Also, with such damage, deposits of protein substances can sometimes form. They are called fibrins, and they provoke acute myocardial infarction in the posterior wall of the left ventricle.
Diagnosis of myocardial infarction
When diagnosing a heart attack, several basic methods of examining the patient are used:
- Blood analysis. Myoglobin (a protein that transports oxygen to cells) can be detected in it approximately 5–6 hours after the onset of a heart attack. In addition, after 8–10 hours, the patient’s blood shows an increased activity of creatine phosphokinase by more than 50%. It later decreases to normal levels (after about two days).
Important : to exclude the possibility of a heart attack, creatine phosphokinase activity is monitored three times every 5–8 hours. And only with three consecutive negative results, the diagnosis of “heart attack” is not confirmed.
- Electrocardiogram (echocardiogram). This type of examination gives the doctor a complete picture of the patient's heart health. The transcripts show all possible pathological waves/segments, etc., arising against the background of a heart attack.
- Coronary angiography. It involves the introduction of a radiopaque substance into the blood and further monitoring of the work of all vessels and arteries of the heart using an X-ray machine. The image will show all areas of stenosis or thrombosis of blood vessels, which will enable the doctor to choose the method of surgical intervention (if necessary).
Relief of an acute attack of myocardial infarction
An acute attack of a heart attack should only be treated by emergency personnel. Before their arrival, you can only provide the victim with all possible first aid if symptoms of pathology occur. You need to do the following:
- Eliminate the cause of the patient's anxiety.
- Sit the patient down and remove all clothing constricting the neck and chest.
- Provide a flow of fresh, but not cold air into the room.
- Give aspirin (the patient must chew it and wash it down).
- Offer a nitroglycerin tablet under the tongue.
- Place warm heating pads on your limbs.
- Track heart rate and blood pressure.
Treatment of small-focal and large-focal infarction
Any heart attack is treated only in a hospital in the cardiology department. Here all standard therapeutic or resuscitation actions can be carried out in relation to the patient.
Reanimation
If a person loses consciousness or his heart stops, doctors provide resuscitation therapy to restore the heart rhythm. For this purpose, a defibrillator is used, which allows the main human organ to start working again. If it is possible to restore heart function, then the patient is given a solution of 5% sodium bicarbonate in a volume of 170 ml.
Important : if there is no defibrillator, the patient can be given intravenous potassium chloride (5–10% solution) and then undergo chest compressions. It is also possible to give the patient an indirect cardiac massage on a hard surface in parallel with artificial respiration until the ambulance arrives. A pericardial blow to the heart area is also indicated. This often works well.
Therapeutic treatment
As soon as the patient's condition has stabilized, drug therapy is administered. It includes the use of drugs from the following groups:
- Anticoagulants. Prevents the formation of blood clots.
- Thrombolytics. They allow you to successfully break down existing blood clots.
- Beta blockers. They make the heart work more economically due to its insufficient blood supply.
- Painkillers. Relieves pain.
- Sedatives. They remove the feeling of panic, as a result of which adrenaline worsens the functioning of an already tired heart.
- Heart rate stabilizers.
Surgery
If the effectiveness of drug therapy is low, the patient is indicated for surgical intervention. Two methods are used:
- Coronary artery bypass surgery. The principle of the operation is to create new blood supply pathways to the heart, bypassing those affected by stenosis or thrombosis. Often the femoral or thoracic veins act as shunts.
- Balloon angioplasty (stenting). During this operation, the doctor, using an artificial balloon inserted into the lumen of the vein, inflates the affected vessel and then secures the result by installing a stent (a special mesh that holds the walls of the vessel in a given position).
Folk recipes
After proper medical or surgical therapy during the rehabilitation period, the patient can use folk remedies to restore heart function. The following methods are used:
- Hawthorn decoction. The berries are brewed in a thermos like tea, and the finished drink is drunk throughout the day. We have collected even more hawthorn recipes here.
- Strawberries and rose hips. Take 50 grams of rosehip and strawberry leaves and immerse it all in 500 ml of boiled water. Simmer in a water bath for about 15 minutes. After complete cooling, strain. The finished volume of the product is brought to 500 ml using boiled water. Drink 50–100 ml twice a day.
- Honey and carrot juice. Mix juice and honey in a ratio of 1 glass to 1 tablespoon and drink after meals 2-3 times during the day.
Important : for acute ulcers and enteritis, such treatment is contraindicated.
- Gray blackberry. A decoction is prepared from the leaves of the plant. Leaves in the amount of 2 tablespoons are steamed with 500 ml of boiling water and kept for at least 2 hours. Then strain everything and take 0.5 cups warm, after mixing with honey.
Rehabilitation
The rehabilitation period lasts for each patient diagnosed with a heart attack from 4 months or more, depending on the degree of heart damage. Rehabilitation activities include:
- drug therapy;
- physiotherapeutic procedures;
- diet therapy;
- help from a psychologist;
- feasible physical activity.
Important : the patient’s hospital stay usually takes from 1 to 3 weeks. The doctor records all changes in the patient’s condition in the medical history.
Forecast
Formally, every patient who survives a heart attack is disabled. Because if even the smallest part of the heart is affected by necrosis, this already disrupts the process of feeding the entire body with blood and causes certain complications. But the prognosis in any case will depend on the zone and extent of damage to the heart by necrosis, the depth of the lesion, the general physical condition of the sick person and his age. Concomitant chronic diseases in the patient also play an important role in prognosis. The more there are and the more complex they are, the greater the likelihood of relapse and repeated already extensive heart attack.
Important : with successful rehabilitation and compliance with all the doctor’s recommendations, the patient may well continue to lead his usual lifestyle, adapting to the new operating conditions of his body.
Treatment of the disease
When treating infarction of the posterior wall of the heart, attention is paid to the causes of its occurrence. In other words, it is not the death of tissue cells that is treated, but the cause of their occurrence – impaired blood flow. To do this, the blood clot is dissolved and conditions are created that prevent its reoccurrence. Thrombolytics break down the blood clot, and Ticlopidine, Clopedagril, and Aspirin prevent its reappearance.
The course of treatment also includes drugs that eliminate the focus of regional cells in the heart muscle:
- Beta blocker - reduces cardiac workload, reducing its need for oxygen.
- Nitroglycyrin and Analgin - reduce heart pain. Lidocaine
- The heart rate decreases - lidocaine and amidarone are used for this.
- For bradycardia, Atropine is prescribed.
To increase the level of oxygen in the blood, the patient is prescribed oxygen therapy. This is a procedure during which the oxygen content in the body increases significantly.
In particularly severe cases, treatment is performed with surgery. During this procedure, the patient is fitted with a stent, a device that prevents the coronary artery from narrowing.
Any prescription for treatment is made by a cardiologist, even with barely noticeable signs of pathology. Any self-medication in this case can lead not only to complications, but also to death.
Myocardial infarction causes irreversible consequences, which will certainly make themselves felt if the disease is left without proper treatment. It can be:
- Weak and untimely contraction of the ventricle. This phenomenon is called flicker.
- The walls of the heart bulge, increasing its volume.
- Weak and uneven blood circulation causes a deficiency of oxygen in the human brain, which leads to disruption of its functioning.
- A ventricle of the heart can suddenly rupture, resulting in a quick and painful death.
Stenning
A patient who has had a heart attack undergoes a very complex rehabilitation scheme, which includes a gradual increase in physical activity. Any prognosis is very individual and depends on the severity of damage to the heart muscle.
In the postoperative period, no specialist can predict the prognosis at all. Much depends on the general physical condition of the patient and even on his will to recover.
Prevention
In order to prevent heart attacks, you need to take care of your health constantly and from a young age. To do this you should:
- give up tobacco in any form and alcohol forever;
- to live an active lifestyle;
- eat right (excluding fatty and fried foods from the diet);
- properly organize a regime of proper rest and work;
- create a favorable emotional background.
It is important to realize that taking care of our own health is only in our hands. Therefore, it is always better to prevent trouble than to deal with its dire consequences later.
Causes of the disease
The sources of such necrotic damage are factors that lead to blockage of the coronary vessels that supply the heart muscle with oxygen and nutrients. The most common reasons include:
- Increased cholesterol levels;
- Atherosclerosis;
- Hypertension;
- Diabetes;
- Excess body weight;
- Smoking;
- Alcohol abuse.
Also, the question of what an inferior myocardial infarction is should concern older people, since they are at risk. It has been established that the risk of developing this disease increases after 55 years of age. Men are more susceptible to this pathology than women. In addition, mental stress is a provoking factor.
Which doctor will help?
Myocardial infarction requires immediate professional help. First of all, having discovered the symptoms of an attack, you should call a team of doctors. It would be better if they were cardiac resuscitators. After the ambulance delivers the patient to a medical facility, you should go to see the following specialists:
Before making a final diagnosis, the doctor must become familiar with the clinical manifestations of the pathology and the individual characteristics of the patient’s body. To do this, he will ask approximately the following questions:
- Is this the first heart attack or a repeat one?
- What pathologies of the cardiovascular system do you have in your history?
- Do you have chest pain?
- How often do you experience shortness of breath?
- What chronic diseases do you have?
- Does any of your relatives suffer from CVS pathologies?
- Do you often get nervous?
The condition of the skin of the fingertips and chin plays an important role, so a specialist will examine them for blueness. The doctor will also measure your blood pressure and pulse. After this, he will write out a referral for instrumental diagnostic methods.
Effective treatments
Therapeutic measures are focused primarily on the speedy restoration of blood circulation in the coronary artery, which was blocked by a thrombus. The faster this is done, the greater the likelihood that complications in the post-infarction period will be minimal. To do this, doctors prescribe the following medications:
- Drugs that dissolve blood clots;
- Antiplatelet agents and anticoagulants;
- Drugs that reduce myocardial oxygen consumption.
Medications that restore heart rhythm may also be prescribed. In extreme cases, surgical treatment methods are resorted to and percutaneous coronary intervention is performed.
The lower myocardial infarction is called basal. This pathological condition most often occurs in relatively young people aged 40 to 60 years. In the older age group, the number of such episodes drops sharply. This pathological condition develops due to the death of many cells in the lower wall of the heart. As a rule, an unfavorable process occurs as a result of disruption of oxygen supply to tissues due to damage to the coronary arteries. The prognosis of lower myocardial infarction depends on many factors, including the timeliness of medical care and the presence of additional chronic diseases.
Therapy for this pathological condition should be carried out in a hospital setting. It is worth noting that the acute phase of this disorder poses a serious danger to the patient’s life. According to statistics, only half of patients can be transported to a medical facility in a timely manner. Subsequent recovery and return to a full life is observed in 40% of patients. However, even with such a favorable outcome, the risk of relapse is extremely high.
Causes
The number of true reasons that lead to the fact that the patient’s heart or atria begins to be insufficiently supplied with oxygen is large. Among them:
- increased cholesterol levels caused by obesity or poor diet, leading to the formation of cholesterol plaques on the walls of blood vessels;
- persistent hypertension, causing rapid myocardial depletion;
- bad habits (tobacco smoking, excessive alcohol consumption), leading to oxygen starvation of the body and IVS of the heart (hypertrophy of the interventricular septum);
- lack of exercise, leading to blood stagnation;
- age criteria (over the years, vascular walls lose flexibility, which leads to poor supply of blood and oxygen to the heart).
Characteristic symptoms
- Cardiac pathology of the posterior wall of the myocardium in its manifestation differs little from other types of infarction. The patient feels severe pain in the chest area. The pain may radiate to the left limb, subscapular region. The attack is often accompanied by the following symptoms:
- arrhythmia, expressed in disruption of the heart;
- sticky cold sweat suddenly appearing on the face;
- trembling in the limbs;
- low blood pressure;
- general weakness of the body.
An analysis of the condition of many patients showed that with posterobasal pathology, the characteristic symptoms are blurred, and the course of an acute attack is not accompanied by pain.
Also read: Symptoms of the anginal form of myocardial infarction Diagnosing such a pathology is somewhat difficult even when using an ECG; due to atypical symptoms, the disease is often confused with a stomach disease such as gastritis.
Etiology of inferior myocardial infarction
This type of heart pathology develops at a relatively young age, and this is not accidental. After 40 years, people experience an intensification of the formation of atherosclerotic plaques. They help narrow blood vessels and saturate tissues with oxygen. At the same time, the need for it remains at a very high level, since a person still continues to lead an active lifestyle, play sports and work. Thus, the heart tissues do not receive enough of the substances they need, which leads to their death.
Most often, the acute phase of this disorder develops against the background of the rupture of an atherosclerotic plaque, which clogs the blood flow in the coronary artery and within 15-20 minutes leads to the death of a large area of heart tissue. The development of such a pathological condition as posterobasal myocardial infarction can be influenced by such unfavorable factors as:
- long history of smoking;
- addiction to alcohol;
- eating foods high in animal fats;
- cardiac ischemia;
- obesity;
- diabetes;
- hypertension;
- passive lifestyle.
It should be borne in mind that such a disorder is more often observed in people who have a genetic predisposition to it. Currently, a number of genes have been identified that, under the influence of additional predisposing factors, can create the prerequisites for the development of this type of myocardial infarction. Those who have relatives whose medical history includes episodes of this condition need to be extremely attentive to their health.
Development mechanism, types
The pathological condition is caused by the appearance of foci of ischemic necrosis affecting the heart muscle. The disease has an unfavorable prognosis; 10 percent of patients who have suffered a posterior myocardial infarction die within 12 months after the attack. In other patients, the possibility of another heart attack increases significantly.
According to statistics, pathological changes most often occur in the anterior wall of the left ventricle of the heart; much less often, a heart attack affects the posterior region of the ventricle or the septum between them.
Patients who have suffered pathology, despite proper treatment and a long period of rehabilitation, feel the consequences of a heart attack for a long time.
All types of the disease are characterized by serious complications and severe course. All affected areas of the myocardium can no longer be restored. Fibrous tissue that appears at the site of necrosis is unable to perform its functions. A patient who has suffered this type of myocardial infarction must carefully monitor his health throughout his life, follow a diet, and take medications prescribed by a doctor.
This type of IHD (coronary heart disease) has the following localization:
- In the posterior diaphragmatic region (posterior wall of the heart adjacent to the diaphragm). Blockage of the inferior coronary vessel leads to large-focal lesions.
- In the posterobasal region (the upper wall of the heart adjacent to its base). In this case, there is a violation of blood circulation in the vessels and arteries that supply the organ with blood and oxygen.
Types of disease by degree of damage:
- Extensive tissue damage. With the development of such a pathological condition, the blood flow is sharply blocked, and an acute attack can lead to the death of the patient.
- Small focal tissue damage. In the initial stage, the pathology almost does not affect the functioning of the heart; with adequate treatment, the patient’s chances of survival are very high.
Distinctive features of inferior myocardial infarction
The heart is an extremely complex organ. Its walls consist of many layers. The severity of the symptoms of lower myocardial infarction largely depends on how deeply the necrosis has spread due to the cessation of oxygen supply to the tissues. Usually, only one layer of tissue is affected, but large-focal infarction of the lower myocardial wall is also quite common.
The second option is considered prognostically less favorable.
In case of extensive myocardial damage, which happens infrequently, the ECG will show characteristic manifestations of this pathological process. When conducting this study, doctors may immediately suspect the cause of the symptoms. In most cases, with inferior myocardial infarction, a pathological Q or QZ wave appears on the ECG.
Pathophysiology or what happens during MI
Atherosclerosis of heart vessels
The pathophysiology of left ventricular myocardial infarction begins long before the disease itself occurs. It all starts with the most important reason, which can be said to form the basis of pathophysiology - atherosclerosis of the heart vessels. This is a metabolic disease that leads to the deposition of lipids in the vascular wall. Subsequently, a chain of processes develops that lead to the formation of an atherosclerotic plaque.
The plaque represents a time bomb in the pathophysiology of myocardial infarction. At a certain moment, under the influence of provoking factors, its “destabilization” occurs, which is the starting point in the pathophysiology of a heart attack. An unstable plaque “attracts” blood cells and coagulation factors, which are involved in the formation of thrombotic masses.
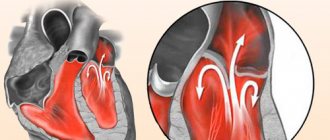
Blockage of a vessel by a thrombus
These masses significantly limit the lumen of the vessel or block it completely. In this condition, blood flow is disrupted, and the myocardium begins to experience a lack of oxygen, which in pathophysiology is called ischemia. If blood flow is not restored, a heart attack develops in the “starving” part of the heart. In pathophysiology, this term means the death of a section of the left ventricular myocardium with the subsequent replacement of this place by scar tissue.
Scar tissue is connective tissue that is unable to contract. If the lumen of the vessel is completely blocked, then acute transmural infarction of the lower myocardial wall develops. In case of incomplete occlusion, small focal damage occurs. Features of the pathophysiology of extensive and small-focal damage determine different treatment tactics in the future.
Diagnosis of lower myocardial infarction
Such myocardial damage should be distinguished from angina pectoris and other disorders of this organ. Comprehensive diagnostics allows us to identify not only the nature of the heart problem, but also the extent of tissue damage. First, the most thorough history taking and examination of the patient is carried out.
In addition, the detection of enlarged lymph nodes indicates the onset of the inflammatory process. Percussion and auscultation are required. During early diagnosis, measurement of blood pressure and body temperature is indicated. To clarify the diagnosis, an ECG is immediately performed.
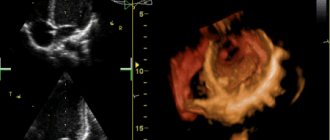
In the future, echocardiography is prescribed, which allows you to see the work of the patient’s heart. This study helps determine disorders of myocardial contractile function, as well as the speed of blood flow.
In addition, the use of this method detects the presence of a blood clot or aneurysm, and also evaluates the functioning of valves and adjacent vessels.
Coronography is often performed. This research method allows you to accurately determine the degree of vascular patency in the heart. Scintigraphy allows you to accurately determine the extent of necrotic damage to the heart. In addition, the use of MRI may be indicated. This study allows us to detect even the smallest changes in tissue structure. In most cases, general and biochemical blood tests are performed. They make it possible to determine characteristic markers of necrosis.
How is it diagnosed?
Diagnosing pathology of the posterior wall of the heart is quite difficult; the doctor studies the ECG results, paying attention to the following indicators:
- If the Q wave is detected in the AVF, third and second leads, this confirms a posterior phrenic infarction. This is also indicated by the characteristic rise of the T wave on the cardiogram.
- A smooth transition of R in leads V1, V2, V3 indicates the onset of a posterobasal infarction.
- ST segment elevation indicates damage to the wall of the left ventricle of the heart.
Other diagnostic techniques include:
- Prescribing general and biochemical blood tests. On the first day, it is important to monitor the increase in the number of neutrophil leukocytes; its peak occurs on the third day of the attack.
- Purpose of radiography. An X-ray helps to identify blood stagnation in the patient’s chest area, which directly indicates the presence of pathology.
- The purpose of echocardiography, with the help of the study, it is possible to clarify the picture of the disease and identify hidden ischemic changes in the heart.
Treatment of lower myocardial infarction
When the first signs of a pathological condition appear, you must call an ambulance. The patient should be placed so that the head is elevated. Nitroglycerin tablet under the tongue. Subsequently, therapy is carried out in a hospital setting. Typically, Aspirin is included in the treatment regimen. It promotes platelet inhibition, therefore preventing the formation of blood clots that can block the lumen of blood vessels.
Usually Plavix is also prescribed, as well as its components. This is a very powerful tool. It prevents the formation of blood clots, which significantly improves the prognosis for lower myocardial infarction. In addition, thrombotic drugs are often introduced into the treatment regimen. In some cases, the use of medications is required to relieve the manifestations of arrhythmia.
In addition, in this pathological condition, the use of beta blockers is prescribed to reduce the myocardial oxygen demand and agents that help reduce the load on the heart. If it is not possible to restore blood flow in the coronary arteries with medications, urgent surgical intervention may be indicated. Angioplasty is usually performed to widen narrowed blood vessels.
In addition, therapy is carried out aimed at maintaining the functioning of the kidneys, respiratory organs, blood pressure and pulse.
Throughout the acute period, the patient requires complete rest and the exclusion of any physical overload and stress. A mandatory aspect of therapy is a gentle diet. Alcohol and nicotine must be completely abandoned during this period of hospital stay and later during rehabilitation. After stabilization of the patient’s condition, short-term walks in the fresh air may be recommended to perform gentle exercise therapy.
The most important point is rehabilitation, since without it there is a high risk of another heart attack. Often people have to radically change their lifestyle and put up with serious restrictions for a very long time. It is necessary to avoid physical and emotional stress, consumption of fatty foods and processed foods, and, in addition, trips that involve changing climatic zones. It is necessary to follow the doctor’s instructions regarding adherence to a special gentle diet and perform the prescribed complex of exercise therapy. In addition, sanatorium-resort treatment in special institutions involved in the rehabilitation of patients suffering from cardiovascular diseases can be of great benefit.
What not to do after a heart attack
After a heart attack, a person’s life changes, and some restrictions are imposed regarding nutrition, daily routine, activity, etc. It is recommended to avoid excessive physical exertion so as not to encounter a second heart attack. Moderate loads are indicated - walking, exercise therapy.
Stress has a detrimental effect on the heart and blood vessels - during a nervous breakdown, the heart beats quickly, the muscle's need for oxygen increases, which can provoke a new attack.
As for nutrition, you should not eat foods high in cholesterol. Such products provoke atherosclerosis, are difficult to digest and overload not only the gastrointestinal tract, but the entire body.
Smoking and alcoholic drinks are harmful even to a healthy person, and after a heart attack they are contraindicated.
The danger of a second heart attack persists all the time, and if it occurs within 3-60 days of the first, it is considered a relapse. In this case, necrosis is localized in the same place as the first time, only the affected area will be much larger. If a second heart attack occurs later, after 2 months or more, then this condition is called a second heart attack. This condition is much more dangerous than a primary heart attack. The fact is that after the first attack, the dead tissue is scarred, as a result of which the heart loses certain compensatory properties.
Prevention of lower myocardial infarction
People at risk of developing this acute disorder need to be proactive in preventing it. It is necessary to give up all bad habits, as they negatively affect the functioning of the entire cardiovascular system.
From the age of 35, you should monitor your blood cholesterol levels. This will reduce the risk of plaque formation. In some cases, you may need to visit a doctor to prescribe special drugs from the statin group. These medications help maintain normal blood cholesterol levels.
You definitely need to play sports. Daily physical exercise will reduce the risk of developing myocardial infarction. In addition, the most important aspect of preventing this heart disorder is adherence to healthy eating habits. All dishes must be steamed or boiled. It is advisable to reduce salt intake. All this will significantly reduce the risk of developing pathology.
Consequences
A person who wants to live a long time must take care of his health, because a pathological complication in the form of myocardial infarction has many consequences.
Complications to be aware of:
- Transmural (extensive) infarction, affecting the entire thickness of the myocardium, can lead to rupture and even immediate death.
- With pathology that has developed in the left ventricle of the heart, fibrillation may begin, which is also a serious complication, often leading to death.
- A posterolateral infarction affecting a large area of the heart can result in protrusion of the anterior wall of the cardiac chamber. Thinning caused by pathology leads to the development of an acute aneurysm. Recovery of a patient with such a complication takes a lot of time.
Thromboembolism is a complication consisting of blockage of a coronary vessel by a blood clot (thrombus), leading to impaired cerebral circulation, lung damage, and problems in the diaphragmatic region of the gastrointestinal tract. Rehabilitation of such a patient takes a very long time.