Stages of recovery for patients who have had the disease
Rehabilitation after a heart attack includes a number of measures, the task of which is to prevent recurrent attacks, eliminate complications and return the patient to normal life.
The main directions of the restoration process are:
- normalization of physical activity;
- drug therapy;
- diet;
- psychological help.
The choice of rehabilitation tactics is based on the individual condition of the patient, as well as his age and the reasons that led to the development of a heart attack.
If the disease does not cause serious complications, rehabilitation of patients after myocardial infarction can be successfully carried out at home.
In the serious condition of the patient, when he has complications such as arrhythmia or heart failure, rehabilitation should initially be carried out in a specialized medical institution, with further transfer to home recovery of the body and compliance with the nursing process for myocardial infarction.
Cardiogenic shock
It can be identified by the following signs:
- Blood pressure is usually below 60 mm Hg. Art.
- Oligouria (decreased amount of urine output) or anuria (complete absence of urine).
- Dewy and pale skin.
- Cold extremities.
- Body temperature is reduced.
- Muffled heart sounds.
- Tachycardia.
- Moist rales in the lungs on auscultation.
- Breathing is shallow and frequent.
- Central nervous system disorders (confusion or loss of consciousness).
The described early complications of myocardial infarction occur most often and require immediate medical attention. Among the late complications of this pathology, the most common are post-infarction syndrome and CHF.
Goals of rehabilitation after a heart attack
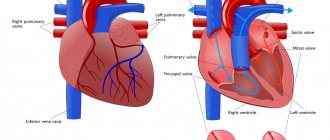
The coronary arteries supply blood to the heart muscle. A sharp disruption of blood flow causes hypoxia (oxygen starvation), and then cell death - a heart attack. After scarring, the tissue does not perform the necessary functions, circulatory failure develops, and the body has to adapt to new conditions. The quality and length of life of patients after a heart attack and stenting is determined by the development of compensatory mechanisms.
The rehabilitation program for patients after a heart attack or cardiac surgery (bypass surgery, stenting) pursues the following goals:
- prevention of early and late complications: acute and chronic aneurysms (thinning and protrusion of the heart wall), rhythm disturbances, cardiogenic shock with pulmonary edema, cardiac rupture, myocarditis;
- restoration of physical activity (including professional) to the highest possible levels;
- psychological preparation of the patient for life after a heart attack, the mood for long-term rehabilitation;
- reducing the risk of recurrent cardiovascular events, including stroke.
Definition
Acute myocardial infarction - signs of cardiomyocyte necrosis in clinical conditions suggesting the presence of acute myocardial ischemia.
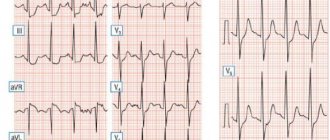
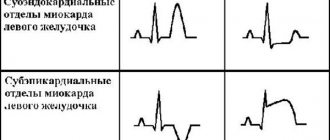
Acute coronary syndrome with persistent ST segment elevations is recent clinical signs or symptoms of myocardial ischemia in combination with the presence of persistent (lasting more than 20 minutes) ST segment elevations in at least two adjacent ECG leads. Includes myocardial infarction with persistent ST segment elevations and unstable angina.
First recommendations
Physical therapy is the most important stage in restoring the physical activity of a person who has suffered a heart attack. The start time of exercise therapy is prescribed by the doctor depending on the degree of myocardial damage and the patient’s condition.
In case of moderate severity of the pathology, gymnastics is started already on the 2-3rd day; in case of severe pathology, it is usually necessary to wait a week. The basic principles of restoring the patient’s physical activity boil down to the following steps:
- the first few days require strict bed rest;
- on days 4-5 the patient is allowed to take a sitting position with his legs dangling from the bed;
- on day 7, if the situation is favorable, the patient can begin to move close to the bed;
- after 2 weeks it will be possible to take short walks around the ward;
- from 3 weeks after an attack, it is usually allowed to go out into the corridor, as well as go down the stairs under the supervision of an instructor.
The distance the patient travels should increase every day.
After increasing the load, the doctor must measure the patient’s blood pressure and pulse. If the indicators differ from the norm, the load will need to be reduced. If recovery is favorable, the patient may be referred to a cardiac rehabilitation center (sanatorium), where he will continue his recovery under the supervision of professionals.
Preventive measures
A person who has had a heart attack is at risk of recurrence of the disease. It is extremely important for the patient to undergo a medical examination in a clinical setting and undergo tests. Be sure to measure your blood pressure and pulse. A detailed blood test is performed twice a year.
In more than 70% of all patients, there is a mental disorder, so it is important to regularly visit a psychologist to correct the emotional state of health. The use of alcoholic beverages and drugs is strictly prohibited. The patient must constantly monitor his weight, preventing it from increasing.
Regarding sexual life, it is worth noting that many medications that are used during the rehabilitation period negatively affect sexual health in both women and men. It is worth limiting some bed positions during sex. You should not use poses that require you to bend forward.
A heart attack is a serious heart disease with a large number of complications, but even with this diagnosis, subject to all rehabilitation and prevention measures, you can lead a full life, the quality of which will depend only on the patient.
Rehabilitation methods
Treatment and restoration of the body after a heart attack requires an integrated approach. Basic rehabilitation methods:
- taking pharmaceutical drugs;
- dosed physical activity;
- diet;
- following the basic principles of a healthy lifestyle.
First of all, you need to give up smoking and drinking alcohol. Toxins contained in alcohol and nicotine have the following negative effects on the body:
- contribute to an increase in the level of “bad” cholesterol (low-density lipoproteins);
- cause vascular spasms;
- lead to surges in blood pressure;
- provoke the development of arrhythmia or tachycardia.
After a heart attack, these manifestations are especially dangerous, as they can cause a second attack and sudden death of a person.
Medicines are used at all stages of therapy. Upon admission to the hospital, the patient is prescribed medications aimed at reducing the load on the myocardium, preventing thrombus formation, relieving pain, and eliminating the panic fear of death.
For this purpose, drugs from the following pharmaceutical groups are used:
- analgesics;
- thrombolytics;
- tranquilizers;
- anticoagulants.
During the post-inpatient and maintenance periods of rehabilitation, funds are selected individually, depending on the consequences that occur.
More often used:
- beta blockers;
- antiplatelet agents;
- statins to prevent the development of vascular atherosclerosis;
- nitro drugs for angina attacks;
- antiarrhythmic drugs;
- antihypertensive drugs;
- decongestants.
Attention: medications should only be taken as prescribed by your doctor!
You cannot stop taking medications or change the dosage on your own. This can provoke the development of life-threatening complications.
Properly selected physical activity is one of the necessary conditions for recovery. According to research, regular exercise reduces mortality in the first year after a heart attack by 25%.
The development of an acceptable set of exercises should be carried out by a physiotherapist. You can exercise at home or in a physical therapy room.
After a heart attack, gymnastics helps:
- strengthen the myocardium;
- increase the contractility of the heart muscle;
- normalize blood circulation;
- reduce cholesterol levels;
- minimize the likelihood of blood clots.
Example of a set of exercises:
- sit on a chair, straighten your back, close your knees, lower your arms. As you inhale, alternately raise your arms, and as you exhale, lower them;
- bend your arms at the elbow joints and perform rotational movements. First clockwise, then counterclockwise;
- in a sitting position, spread your arms to the sides. As you inhale, pull your left (then right) leg to your chest with your hands, and as you exhale, return to the starting position;
- place your palms on your waist and bend to the sides;
- stand up straight, hands on your waist, feet shoulder-width apart. Rotate your body to the right and left;
- walk in place for 15 minutes.
The load should be increased gradually. Even if you feel well, intense training after a heart attack is contraindicated.
Attention: if pain occurs in the heart area (including mild tingling), you should stop charging immediately, take nitroglycerin, and consult your doctor.
You need to start training 1.5-2 hours after eating. Constantly monitor your heartbeat. Immediately after exercise, the pulse should not exceed 120 beats per minute; after a five-minute rest, return to normal values.
Nutrition
Compliance with a special diet is necessary to restore full functioning of the myocardium and prevent recurrent attacks.
During the first few days in the hospital, the patient is given small portions only of lean soups and pureed foods without salt. This reduces the strain on the damaged heart muscle.
After discharge, the list of permitted foods and their volume increases, but some restrictions remain for life.
You will have to completely eliminate from use:
- any fatty meat;
- sausages;
- spicy seasonings;
- pickles;
- smoked meats;
- margarine;
- chips;
- semi-finished products;
- salo;
- cakes;
- fast food.
It is necessary to limit the consumption of legumes, eggs, offal, fatty cheese, and sweets. The basis of the diet should be:
- vegetables. Various types of cabbage are especially useful. It is better to bake potatoes unpeeled and, if possible, eat them with their jackets;
- lean meat;
- fruits;
- low fat dairy products;
- greenery;
- sea fish;
- cereals;
- nuts (include in the menu regularly, but little by little);
- whole wheat bread;
- berries;
- vegetable oils.
Jelly, puree, pudding, and sherbet are suitable as desserts. It is good to replace strong tea and coffee with sugar-free juices, fruit drinks, and mineral water. You need to drink 1-1.5 liters of liquid per day.
Nutrition should be balanced, contain sufficient amounts of proteins, fats, and carbohydrates.
Attention: strict diets for cardiac pathology are contraindicated!
To normalize weight, it is enough to reduce the calorie content of dishes. You can control your performance by measuring your waist. For men, the circumference should not exceed 94 cm, for women – 80 cm.
Physical rehabilitation of post-infarction patients is carried out in stages, with a gradual increase in loads and constant monitoring of functional capabilities. Methods of adaptation of organs and systems (cardiovascular, respiratory, musculoskeletal), as well as psychological support, are used comprehensively.
Rehabilitation means:
- physical therapy (physical therapy);
- sanatorium-resort rehabilitation in specialized cardiological boarding houses;
- educational program in organized schools for patients with coronary heart disease (CHD);
- drug treatment depending on the patient’s condition, circulatory disorders;
- physiotherapy;
- psychological rehabilitation.
The recovery program is selected based on the patient’s diagnosis: the extent of the infarction (transmural or small focal), localization (apex, wall, septum), and concomitant diseases are taken into account.
| Clinical group | Main features |
| First (easy) |
|
| Second (moderate) |
|
| Third (heavy) |
|
The patient's clinical team determines the overall and phased duration of rehabilitation.
To select exercises for physical rehabilitation, the functional state of the body systems is assessed. To do this, test loads are carried out:
- 6-minute walk test: the patient needs to walk the greatest distance in 6 minutes without starting to run;
- bicycle ergometry - on an exercise bike with a given power;
- treadmill test - walking on a treadmill.
Depending on the symptoms that arise, the types of responses presented in the table are distinguished.
| Criterion | Physiological | Intermediate | Pathological |
| Fatigue | Moderate | Pronounced, disappears in less than 5 minutes | Expressed with a long recovery period |
| Dyspnea | No | Minor | Expressed |
| Chest pain | No | Episodes, self-limiting | Strong, requires nitroglycerin |
| Blood pressure and pulse | Within normal limits for load level | Infrequent disturbances with recovery within 5-10 minutes | Exceeding the limit for a long time, requiring more than 10 minutes of rest |
| ECG changes | No |
|
|
Depending on the patient’s response, stage of rehabilitation and severity, programs of different levels are selected.
Exercises of the exercise therapy program 1 (the first 2-4 days of rehabilitation with the starting position lying down):
- flexion and extension of the fingers and toes (6-8 times);
- while inhaling, bend your forearms, spread your elbows to the sides, while exhaling, straighten your arms along your body (2-3 times);
- alternate bending of the legs at the knees, without lifting the feet from the bed (4-6 times);
- turn your hands with your palms down: as you inhale, reach for your knees, tensing the muscles of your torso and legs, as you exhale, relax (2-3 times);
- lower your legs bent at the knees alternately to the right and left sides (4-6 times);
- alternately stretch your hands to your legs bent at the knees (3-5 times).
Between exercises you need to pause for 10-30 seconds to restore breathing.
Approximate exercise therapy complex 2 (from 4 to 12 days of rehabilitation in hospital, starting position – sitting):
- back straight, hands on knees: as you inhale, touch your shoulders with your hands, spread your elbows to the sides, as you exhale, return to the starting position (6-8 times);
- as you inhale – arms forward and up, as you exhale – lower them (3-5 times);
- move your feet back and forth without lifting them off the floor (10-15 times);
- while inhaling, spread your arms to the sides, while exhaling, return to the starting position (6-8 times);
- arms bent at the elbows at the waist: turn your head alternately to the left and right (5-10 times).
Rehabilitation after myocardial infarction at home (physical therapy 3) can be carried out using special mobile applications to monitor exercise performance.
Rehabilitation of patients in sanatoriums after a heart attack is carried out with a stable condition and expansion of motor activity to walking 500 meters.
The main goal of sanatorium-resort recovery (up to 2 months after a heart attack) is to stimulate compensatory mechanisms for the further transfer of the patient to the outpatient stage.
Complications of myocardial infarction
Complications of a heart attack
Aggravating moments can arise both in the acute period, already in the hospital, and in the most acute period - in the first minutes of the development of cardiomyocyte necrosis.
In the modern world, it is generally accepted that life after a myocardial infarction should include the continuation of one’s work activity, albeit with some restrictions. Most people can return to their previous jobs quite well after three or four months of quality rehabilitation.
And, nevertheless, it is important to understand that each person is strictly individual; for some, such a return to nervous work is completely unnecessary. And for many people, subsequently returning to a job they love may be the most important part of fully regaining their former quality of life.
Of course, only a gradual return to work is considered the optimal approach. For example, you can start with half a working day and go to work every other day. Of course, you should start only with the easiest duties. In addition, it is recommended to include several additional periods of rest if excessive fatigue is noticed.
Some patients consider the best option after a heart attack to be the so-called early retirement. At the same time, it is very important that such a decision is made by the patient himself without pressure from relatives and only for the right reasons, and not at all out of fear of a recurrence of the attack.
The acute period of myocardial infarction is characterized by the development of cardiogenic shock and acute failure. These varieties represent the earliest complications of a heart attack and are among the most dangerous for humans during the acute period of development of the disease.
Heart failure is a very common complication that occurs immediately after a heart attack, and the severity of the resulting failure depends on the extent of damage to the heart muscle. If the deficiency develops in a severe form, a person experiences cardiogenic shock. This complication is characterized by a decrease in the pumping function of the myocardium, which occurs as a result of necrotic phenomena occurring in the thickness of the muscular layer of the heart. Most often, complications of this severity develop in elderly women and patients with diabetes.
Treatment of complications that arise during the acute period consists of taking medications containing nitroglycerin and ACE inhibitors. In addition, the course of treatment includes taking vasopressor drugs and drugs with diuretic properties. The use of endovascular techniques involves the use of angioplasty and intra-aortic balloon counterpulsation. Sometimes, in special cases, surgical treatment is used.
Early complications develop in the first minutes, hours or days after an attack. These include:
- Cardiogenic shock.
- Pulmonary edema.
- Acute heart failure.
- Conduction and rhythm disturbances, ventricular fibrillation is especially common.
- Blood clot formation.
- Cardiac tamponade occurs due to a rupture of the heart muscle wall (this is rare).
- Pericarditis.
In addition, myocardial infarction is dangerous due to its late complications, which develop in the subacute and post-infarction period of the disease. As a rule, they occur approximately 3 weeks after the attack occurred. These include:
- Dressler's syndrome or post-infarction syndrome.
- Thromboembolic complications.
- Cardiac aneurysm.
- Chronic heart failure (CHF).
Let's consider the most severe complications of myocardial infarction.
Left ventricular AHF develops more often, i.e. myocardial damage occurs in the area of the left ventricle. This is a very serious complication. It includes cardiac (heart) asthma, pulmonary edema and cardiogenic shock. The severity of AHF depends on the volume of the affected area.
As a result of cardiac asthma, the perivascular and peribronchial spaces are filled with serous fluid - this leads to a deterioration in metabolism and further penetration of fluid into the lumen of the alveoli. This liquid mixes with the exhaled air to form foam.
Cardiac asthma is characterized by an abrupt onset, usually at rest, often at night. The patient feels an acute lack of air. It becomes a little easier in a sitting position. In addition, there are:
- Pale skin.
- Swelling.
- Cyanosis.
- Cold sweat.
- Moist rales are heard in the lungs.
A characteristic difference between cardiac asthma and bronchial asthma is the fact that inhalation is difficult. Whereas in the case of bronchial asthma, on the contrary, the patient experiences difficulty in exhaling.
If in such a situation urgent measures are not taken and the patient is not hospitalized to provide qualified assistance, pulmonary edema develops.
With this complication of a heart attack, there are difficulties with the heart muscle pumping the required volume of blood. As a result, all organs suffer from lack of nutrition and oxygen supply. This pathology manifests itself as swelling and shortness of breath, sometimes even at rest. With CHF, the patient should lead an exceptionally healthy lifestyle.
At the same time, in patients with acute myocardial infarction, signs of ischemia of the heart muscle may increase and the size of the infarction may increase. With unstable angina, progression of symptoms or development of myocardial infarction is possible.
- The best way to recover from hypertension (quickly, easily, healthy, without “chemical” drugs and dietary supplements)
- Hypertension is a popular way to cure it at stages 1 and 2
- Causes of hypertension and how to eliminate them. Tests for hypertension
- Effective treatment of hypertension without drugs
In most patients with acute myocardial infarction, blood pressure remains normal or decreases. With moderate or severe hypertension, the question arises of quickly lowering blood pressure to avoid increasing the size of the infarction.
With unstable angina, the pressure usually rises during an ischemic attack, and after the attack, it usually normalizes or returns to its original level. If, despite therapy with antianginal drugs (eg, nitrates, propranolol or analgesics), angina attacks persist, then rapid reduction of blood pressure to baseline levels, preferably with intravenous nitroglycerin, is necessary to prevent the development of a heart attack and eliminate symptoms.
The use of beta blockers, ACE inhibitors and sodium nitroprusside is also effective. The latter can cause “steal syndrome”, and therefore it is more advisable to use it in cases where hypertension is resistant to other drugs.
Reducing blood pressure in patients with acute coronary syndrome is of auxiliary importance. It is necessary to take emergency measures to restore coronary (cardiac) blood flow: thrombolysis, heparin therapy, angioplasty, coronary artery bypass grafting.
You can learn in detail about all the medications that are mentioned in this note in the article “Medicines for the treatment of hypertensive crisis.”
- Complicated and uncomplicated hypertensive crisis: how to distinguish
- When a hypertensive patient needs urgent hospitalization
- Stroke - a complication of hypertensive crisis - and how to treat it
- Complication of hypertensive crisis: heart failure
- Aortic aneurysm is a complication of hypertensive crisis
- How to treat hypertensive crisis in pregnant women, after surgery, with severe burns and when withdrawing clonidine
Nutrition rules
During the rehabilitation process, great importance is given to the patient’s proper nutrition. Diets may be different, but they all have common principles:
- reducing the calorie content of food;
- limiting fatty, flour and sweet foods;
- avoidance of hot and spicy foods;
- minimum salt consumption – no more than 5 g per day;
- the amount of fluid consumed should be about 1.5 liters daily;
- meals should be frequent, but in small portions.
What should you eat after a heart attack? The diet must include foods containing fiber, vitamins C and P, polyunsaturated fatty acids, and potassium. The following foods are allowed:
- low-fat meat;
- fruits and vegetables, except spinach, mushrooms, legumes, sorrel, radishes;
- vegetable oils;
- vegetable soups;
- compotes and juices without sugar, weakly brewed tea;
- bran and rye bread, porridge;
- lean fish;
- dairy products without fat;
- omelette.
You will need to give up:
- fatty meat;
- natural coffee;
- fresh bread, any baked goods;
- eggs, fried or boiled;
- marinades, pickles, canned food;
- cakes, chocolate, pastries and other sweets.
Stages of post-infarction rehabilitation
The effectiveness of restoring a person’s adaptive capabilities depends on the adequacy of the loads at different periods. In general cardiac rehabilitation there are three main stages:
- early;
- outpatient;
- remote.
The duration of the stages differs for each person depending on the clinical situation.
Early
The early period involves rehabilitation of the patient in a hospital setting in various departments.
- Intensive care and resuscitation department (no more than 3 days for uncomplicated cases). The patient is allowed to make body turns in bed, head movements and low-amplitude movements with the limbs. The exercise complex 1 is performed exclusively under the supervision of a therapeutic exercises instructor. The greatest attention is paid to the psychological side of recovery: conversations are held about the disease, the methods of treatment and rehabilitation used, and further modification of lifestyle.
- Cardiology department (10-14 days). The patient's motor mode expands to walking around the ward and riding a wheelchair along the corridor. A set of exercise therapy exercises 2 is used; if the patient’s reaction is positive, exits into the corridor are allowed.
- Inpatient stay at a specialized sanatorium or resort (up to 1.5-2 months). The main focus is the return of the patient to normal life, participation in an educational program for patients, and physical procedures.
Physical activity is severely limited due to the need to form an adequate scar at the site of necrotic myocardium, which will be able to maintain hemodynamic parameters at sufficient levels.
Outpatient
In foreign sources, the rehabilitation period after hospitalization is called the recovery phase. The average duration is 6-8 weeks, during which the patient is under the supervision of specialists from a clinic or outpatient center.
Main areas of work with patients:
- restoration of the patient’s physical capabilities;
- preparation for professional activity;
- secondary prevention of cardiovascular accidents and late complications.
During this period, the patient is offered to use rehabilitation methods in a clinic setting (physiotherapy, bicycle ergometry).
The duration of this phase of patient rehabilitation implies lifelong adherence to the doctor’s recommendations regarding:
- physical activity;
- rational nutrition: such patients are recommended to follow a Mediterranean diet low in animal fats;
- giving up bad habits;
- adequate work activity (return to low-intensity work is possible 2 months after a heart attack).
In Russia, outpatient recovery involves regular visits to a local physician, as well as other doctors. In foreign countries, government programs provide a 21-day stay for patients in hospitals at specialized centers once a year.
Pre-infarction state
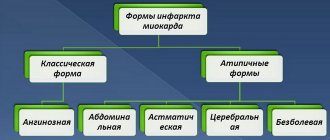
To avoid becoming a victim of an unexpected heart attack, it is important to know the symptoms of a pre-heart attack. These are the so-called harbingers of impending danger. Acute myocardial infarction often develops according to the scenario of increasing angina (pain or discomfort behind the sternum). As a rule, the symptoms of typical angina disappear after the patient takes nitroglycerin. If the remedy does not help, and angina pectoris intensifies, then we can talk about an approaching heart attack. This condition is called unstable angina. In this case, it is better for the patient to change his plans and call an ambulance. Unstable angina manifests itself in several ways.
- Pain in the sternum radiates to the collarbone and arm.
- Painful sensations may be accompanied by a burning sensation (abdominal syndrome).
- Weakness and cold sweat appear.
- The pulse quickens.
- The patient feels panicky.
In some cases, there may be no pain, a type known as atypical pre-infarction syndrome. Its symptoms are dizziness, causeless
Physical activity and sex life
The return to physical activity begins in the hospital setting. After the condition has stabilized, the patient is allowed to perform small physical exercises, first passive (just sitting in bed), then more active.
Restoration of simple motor skills should occur within the first few weeks after the attack.
From the 6th week, patients are usually prescribed physical therapy, exercise on an exercise bike, walking, climbing stairs, light jogging, and swimming. The load should be increased very carefully.
Physical therapy is very important in rehabilitation after a heart attack. Thanks to special exercises, you can improve blood circulation and restore heart function.
Exercise therapy is prescribed only if the patient’s condition is satisfactory and the recovery period is favorable.
People who have had a heart attack can do household chores depending on the functional class of the disease. Patients of the third class are allowed to wash dishes, wipe dust, the second class are allowed to do minor housework, but they are prohibited from sawing, working with a drill, or washing clothes by hand. For first class patients, the possibilities are almost unlimited. You just need to avoid working in an awkward body position.
Patients can begin sexual activity a month to a month and a half after the attack. The possibility of sexual contact will be indicated by the preservation of normal pulse and blood pressure even when ascending to the 2nd floor.
Basic recommendations for sexual intercourse:
- Nitroglycerin tablets should always be prepared nearby;
- It is recommended to have sex only with a trusted partner;
- the room temperature should not be too high;
- poses should be chosen that will not cause excessive physical stress - for example, poses in a vertical position are not recommended;
- do not drink alcohol, fatty foods and energy drinks before sexual intercourse, and do not take hot baths.
Potency enhancing products should be used with extreme caution. Many of them negatively affect the functioning of the heart.
If such a drug causes an attack of angina, it is strictly forbidden to swallow nitroglycerin - the combined effect of these drugs usually sharply reduces blood pressure and often leads to death.
Myocardial infarction was previously considered a disease of older men, but now the pathology is increasingly being registered among the working population. Impaired cardiac function significantly impairs the patient's quality of life.
Thanks to new methods of diagnosis, treatment and early rehabilitation, patients who have suffered a myocardial infarction can live to a ripe old age by following simple recommendations:
- systemic drug therapy, most often Aspirin, statins, nitrates;
- regular physical activity: morning exercises, dosed walking 3-4 times a week for 1 hour;
- weight loss (the required level is calculated by the doctor using the Quetelet index);
- Mediterranean diet;
- optimistic attitude towards a full recovery.
Recovery after a myocardial infarction at home is the most important stage for the patient, since the quality of life depends on the consistency of exercise and adherence to recommendations.
Pre-infarction state
To avoid becoming a victim of an unexpected heart attack, it is important to know the symptoms of a pre-heart attack. These are the so-called harbingers of impending danger. Acute myocardial infarction often develops according to the scenario of increasing angina (pain or discomfort behind the sternum). As a rule, the symptoms of typical angina disappear after the patient takes nitroglycerin. If the remedy does not help, and angina pectoris intensifies, then we can talk about an approaching heart attack. This condition is called unstable angina. In this case, it is better for the patient to change his plans and call an ambulance. Unstable angina manifests itself in several ways.
- Pain in the sternum radiates to the collarbone and arm.
- Painful sensations may be accompanied by a burning sensation (abdominal syndrome).
- Weakness and cold sweat appear.
- The pulse quickens.
- The patient feels panicky.
In some cases, there may be no pain, a type known as atypical pre-infarction syndrome. Its symptoms are dizziness, causeless
shortness of breath and insomnia. In some cases, gastrointestinal disorders are noted:
If the patient and those around him, with the symptoms described above, do not take any measures, then the syndrome will intensify and go directly into myocardial infarction. The pain in the sternum intensifies many times over, the person turns pale and, in severe cases, loses consciousness.
If signs of unstable angina occur, clinical recommendations for the patient are to avoid any physical activity. You need to drink nitroglycerin, take a supine position and wait for the doctor to arrive. The room where the patient is located must have access to fresh air.
Habits
People who smoke are much more susceptible to various heart diseases. Smoking causes spasms of the heart vessels, as well as oxygen starvation of the heart muscle. During the rehabilitation period after a heart attack, it is necessary to completely stop smoking, and to prevent relapses, you will need to make every effort to quit this addiction forever.
With the issue of drinking alcohol, everything is not so radical, but moderation will still be required. During the rehabilitation period, you need to give up alcohol completely, and then adhere to a strict dosage. The maximum permitted dose of pure alcohol per day is: men – 30 ml, women – 20 ml.
Where to undergo recovery: list of centers and institutions
In Russia there are many resorts and health centers specializing in cardiac pathologies. The choice of the necessary institution is carried out depending on concomitant diseases, geographic location and financial capabilities of the patient.
The most popular cardiac rehabilitation centers in the country:
- Kislovodsk (Stavropol Territory) is a balneoclimatic resort from the group of Caucasian mineral waters;
- sanatorium named after Kirov (Crimea);
- rehabilitation center named after. Herzen (Moscow region);
- sanatorium "Zvezdny" (Krasnodar region), which also treats patients with pathologies of the respiratory system, digestion, kidneys, and skin;
- rehabilitation center of the clinic named after. N.I. Pirogova deals with seriously ill patients after a heart attack and complex operations on blood vessels and the heart;
- sanatorium "Electra" (Irkutsk);
- sanatorium-preventorium "Salyn" (Bryansk region).
It is necessary to select an institution for rehabilitation among proven, certified sanatoriums that offer specialized medical services.
Terminology
A bare metal stent is a stent that is a steel frame made of biologically inert material.
Myocardial infarction without persistent ST is a myocardial infarction in which in the early stages of the disease there are no persistent (lasting more than 20 minutes) ST segment elevations on the ECG.
Myocardial infarction with a Q is a myocardial infarction with the appearance of pathological Q waves in at least two adjacent ECG leads.
Myocardial infarction without a Q is a myocardial infarction when pathological Q waves on the ECG have not formed.
Coronary artery bypass surgery is a bypass operation that improves blood flow distal to a hemodynamically significant stenosis in the coronary artery. Depending on the technique, it includes aortocoronary, mammary-coronary and other types of bypass surgery.
Acute coronary syndrome is any group of clinical signs or symptoms that suggest acute myocardial infarction or unstable angina.
Acute necrosis of cardiomyocytes is an increase and/or decrease in the blood levels of biomarkers of myocardial necrosis (preferably cardiac troponin), which at least once exceeds the 99th percentile of values in healthy individuals.
Primary percutaneous coronary intervention is a method of reperfusion treatment of acute coronary syndrome with persistent ST segment elevations on the ECG, when the first measure to restore the patency of the coronary artery is percutaneous coronary intervention.
“Prepared” percutaneous coronary intervention is a method of reperfusion treatment of acute coronary syndrome with persistent ST segment elevations on the ECG, in which a full or half dose of a fibrinolytic is administered before primary percutaneous coronary intervention, sometimes in combination with a glycoprotein IIb/IIIa blocker. Currently not recommended.
“Rescue” (“saving”) percutaneous coronary intervention is urgent percutaneous coronary intervention after unsuccessful thrombolytic therapy.
A drug-eluting stent is a stent from the surface of which an antiproliferative substance is released, which prevents the formation of neointima and thereby helps reduce the severity of restenosis processes.
Thrombolytic therapy is a method of reperfusion treatment of acute coronary syndrome with persistent ST segment elevations on the ECG, when medicinal restoration of occluded coronary patency is carried out using parenteral administration of a fibrinolytic drug, usually in combination with antiplatelet agents and an anticoagulant.
A pharmaco-invasive approach is a method of reperfusion treatment of acute coronary syndrome with persistent ST segment elevations on the ECG, when thrombolytic therapy is carried out and in the next 24 hours all patients undergo diagnostic coronary angiography with the intention of stenting the infarction-related stenosis.
Percutaneous coronary intervention is the restoration of blood flow in a stenotic area of the coronary artery using the percutaneous insertion of the necessary devices. Includes percutaneous balloon angioplasty, coronary stenting and other less common techniques. Typically, unless otherwise specified, percutaneous coronary intervention refers to coronary stenting.
Medical and medical supervision
Treatment with medications plays a leading role in preventing possible relapses. In the post-infarction period, the following drugs are prescribed:
- Means for reducing blood viscosity: Plavix, Aspirin, Tiklid.
- Drugs for the treatment of arrhythmia, angina pectoris, hypertension (depending on what disease led to the development of a heart attack): beta-blockers, nitrates, calcium antagonists, angiotensin-converting enzyme inhibitors.
- Drugs for the prevention of atherosclerosis: fibrates, statins, bile acid sequesters, nicotinic acid.
- Preparations for improving metabolic processes in tissues: Solcoseryl, Actovegin, Mildronate, Piracetam.
- Antioxidants: Riboxin, vitamin E.
In addition, annual monthly courses of multivitamin complexes can be prescribed, which will help strengthen the body and prevent the harmful effects of external factors on the state of the cardiovascular system.
Psychological rehabilitation after a heart attack
Recovery largely depends on the attitude of the patient himself. It can be difficult for an elderly person to return to normal life after a heart attack. The attack always occurs suddenly. Long-term treatment, a sharp restriction of activity, and the inability to perform everyday tasks lead to serious changes in the psyche.
The patient becomes irritable, capricious, and loses stress resistance. Some patients experience a strong fear of a second “blow” and refuse to make any movements, delaying the recovery process. Others, on the contrary, underestimate the seriousness of the situation, neglect clinical recommendations, and provoke a new heart attack.
The support of loved ones and the feeling of the importance of one’s existence are especially important for a person during this period. Additionally, the help of a psychiatrist may be required. The specialist will help the patient realize that illness is not a death sentence and will prevent the development of neurosis and depressive states.
Restoring the body after a cardiovascular disease is a complex and lengthy process that requires constant medical supervision. If it is not possible to provide full-fledged home care, it is better to undergo the first stages of treatment in a specialized institution. Competent rehabilitation after a heart attack in a boarding house for the elderly significantly reduces the time required for a person to return to normal life.
A person who has survived a heart attack is often susceptible to depression. His fears are well founded - after all, the attack could happen again. Therefore, in the post-infarction period, psychological rehabilitation is given a special place.
The main goals of psychotherapy are the prevention of neuroses, normalization of mental state, elimination of phobias and sleep problems.
To eliminate the patient’s fears, relaxation techniques and motivation to work are taught.
The psychologist usually works with the patient’s relatives. Often, after a heart attack, they begin to consider the patient disabled, surround him with excessive care and try to limit his physical activity - this attitude has a bad effect on the patient’s psychological state and makes it difficult for him to return to a full life.
Additional Tips
To prevent recurrence of a heart attack, the patient must avoid nervous and physical stress. During the first days he must remain in bed. If you experience shortness of breath while lying down, it is better to be in an elevated state.
Physical therapy exercises are prohibited in case of severe arrhythmia, high body temperature, low blood pressure and heart failure.
If the patient has renal failure or severe heart failure, intracranial hematomas and increased bleeding, some drugs may be contraindicated for him - for example, Mannitol. A number of diagnostic examinations can negatively affect the patient’s condition. For example, coronary angiography is performed only before surgical treatment.