When did they start using
The procedure involves introducing a large amount of thrombolytic drugs into the body. They will help resolve blood clots and restore blood circulation.
The use of this technique for heart attacks began in 1980. At first it related to experimental medicine. Only after repeated confirmation of its effectiveness did the therapy begin to be widely used to resuscitate people after an acute attack.
Previously, tests were carried out on animals. This made it possible to improve the method and determine what effect the drugs used have on the composition of the blood, and identify possible adverse reactions and complications.
The procedure began to be carried out abroad only in 1995. And in the CIS, thrombolysis has been used only for the last ten years.
Very often, the procedure is performed by emergency doctors in order to stop the pathological process in time.
Progress of the procedure
Thrombolytic therapy for a heart attack is carried out either by emergency doctors or in the intensive care unit. After the patient is admitted to the hospital, all preparatory measures must be carried out within an hour. During this time, the patient must be examined for concomitant diseases and the presence of contraindications to the procedure.
Myocardial infarction is a dangerous pathology in which every minute can save a person’s life. When performing thrombolysis, the doctor should adhere to the following recommendations:
- Before administering thrombolytic drugs, urinary catheters are installed;
- During the first days after treatment, catheters should not be inserted into large arteries;
- During the day, any intramuscular injections are prohibited;
- When selecting a dosage, the patient’s weight should be taken into account.
Age is not a contraindication for the use of thrombolytics. The less time has passed since the onset of the attack, the greater the effect of the therapy. This is due to the fact that fresh blood clots have a softer consistency and are more easily absorbed.
Over time, they become denser, which makes the treatment process much more difficult.
For thrombolytic therapy use:
- Puroplase is a recombinant prourokinase.
- Alteplase. This is a fibrin-specific antigen. It is administered after 4 hours.
- Tenecteplase. The drug is used for management in the prehospital period.
Also, during the treatment process, Actilyse is often used in the following dosage:
- During the first three hours, a string injection of 15 mg of Actilyse is administered. After this, 50 mg is administered by infusion. After an hour for 60 minutes - another 35 mg of the substance. Do not administer more than 100 mg of the drug.
- If treatment takes place within 6 to 12 hours, then first 10 mg is administered by string method, then 59 mg is administered by infusion. Then 10 mg are administered every half hour until the total dosage reaches 100 mg.
The doctor who performs the procedure must strictly follow the instructions.
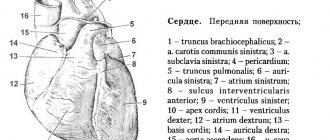
Understanding the reasons for the development of myocardial infarction will help to understand why thrombolysis is necessary. This attack develops due to thrombosis of a blood vessel. The lumen through which blood moves is blocked. This condition is caused by a blood clot that forms when a cholesterol plaque ruptures.
Attention! Myocardial infarction in many cases leads to death caused by cardiac arrest. Even if the person remains alive, the main heart muscle does not recover fully. As a result, a person experiences the consequences of a heart attack throughout his life.
Whether doctors will be able to save life or not largely depends on the methods used in the first hours after the attack. Thrombolysis during a heart attack has contraindications, although in general the procedure helps to urgently restore blood circulation and stop the process of death of heart cells.
A little history
Thrombolysis for myocardial infarction began to be used after the 1980s. At first, this procedure was experimental. Only after its effectiveness was proven did the technique become widely used.
Animal trials were performed before thrombolysis was performed on humans. Such studies have made it possible to improve the technique and more accurately determine how drugs administered during the procedure affect the composition of the blood, what adverse reactions may occur, and how to correctly calculate the dosage.
Only after 1995 this procedure began to be used in some foreign clinics. In the countries of the former CIS, thrombolysis has been carried out only for the last 10 years.
It is important to begin treatment of a heart attack as soon as possible after the attack develops. The therapeutic window for thrombolysis is the first 3 hours after the onset of the disease. Although therapy can be continued for the next 6 hours and the benefits are maintained, the results are not as pronounced and complications occur more frequently.
Because this procedure must be performed immediately after a heart attack, it often has to be performed by an ambulance crew. When visiting your home, doctors must have the right drug to begin properly treating acute myocardial infarction.
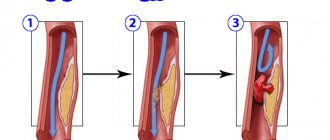
Thrombolysis is a process aimed at dissolving a blood clot formed in a blood vessel. In the body of a healthy person, it occurs constantly, preventing the formation of small blood clots. The dissolution process occurs with the help of special enzymes.
If large blood clots have formed, the body is unable to dissolve them on its own. At best, a small hole may appear in the clot, but this is not enough for normal blood circulation.
We suggest that you familiarize yourself with Medicines for thrombophlebitis of the lower and upper
As new blood clots form, nutrition to vital organs deteriorates, and the risk of heart attack (death of heart muscle cells) increases. If nothing is done, necrosis begins in the tissues, and muscle contraction worsens, which can lead to sudden cardiac arrest.
Important! Thrombolysis is carried out by doctors in a hospital or emergency room. The essence of the method is to administer drugs that can dissolve a blood clot in the shortest possible time.
Timely thrombolysis can stop myocardial infarction, protecting most of the heart muscle. The procedure fully restores blood supply and nutrition to heart cells.
Not only thrombolysis helps doctors save the life of the injured person and restore blood circulation in the vessels. Some other methods also give a similar effect. Studies have shown that timely thrombolysis:
- promotes a speedy recovery;
- reduces length of hospital stay;
- increases the chances of maintaining working capacity after a heart attack.
The patient is recovering from an attack and the procedure performed
Although during a heart attack the diseased cardiovascular system fails, it is possible to restore its functioning. If qualified doctors do this, the result is guaranteed.
Indications for thrombolysis are limited. The procedure is prescribed by a doctor, or the decision to perform it is made by the ambulance team. Thrombolysis is performed in the following cases:
- with a heart attack in the first hours after the attack;
- if the myocardium has not died, the pain persists, and there is no Q wave in the ECG, the procedure is indicated within 12 hours;
- with idioventricular rhythm;
- if a heart attack is suspected.
In most cases, thrombolysis brings good results. The person survives, and the infarction does not spread to the rest of the myocardium.
Contraindications
However, there are contraindications to the use of thrombolytic therapy. Most of them are associated with the risk of bleeding.
conclusions
Thrombolytic therapy is included in the list of standard measures when providing care to patients with acute coronary syndrome at the prehospital stage. The use of TLT in the first hours from the onset of AMI symptoms can save patients with potentially necrotic myocardium, improve left ventricular function and reduce the mortality rate from AMI. The risk of rethrombosis (re-occlusion) is reduced by the combination of thrombolysis with heparin therapy and long-term use of Aspirin.
The following sources of information were used to prepare the material.
With early (up to 3 hours) thrombolysis
Similar effectiveness was noted for the intracoronary method (done only in specialized cardiology departments) and the intravenous systemic method (carried out in an ambulance during transportation, in any department of a hospital hospital or at home). The latter has fewer side effects (less often causes CABG and dangerous arrhythmias). Thus, in England, 50% of all trombonesis is performed at home (in 2/3 of cases - in the first 2 hours).
How it works
Thrombolysis drugs for myocardial infarction dissolve a blood clot formed in the vascular bed. Under normal conditions, small blood clots in the body are dissolved under the influence of special enzymes. But if they are too large, then the body cannot cope with this situation on its own. In this case, the vessel becomes blocked and a heart attack develops.
Drugs used during thrombolytic therapy can quickly dissolve blood clots and stop infarction. Thanks to this, most of the myocardium will be preserved. The procedure can completely restore the process of blood circulation and nutrition of heart cells.
Thrombolytics lead to:
- maintaining the function of the ventricles to pump blood;
- reducing the risk of developing an aneurysm;
- reducing the affected area;
- restoration of electrical conduction of the heart muscle.
The drugs will not only form a lumen in the vessel at the site of the blockage, but will also completely dissolve the blood clot and restore normal blood flow.
It was also determined that the effect of the drugs depends on the time of administration. If thrombolysis is carried out within the first three hours after the onset of an attack, this will reduce the risk of death by 25%; if thrombolytics are administered after 6 hours, the chances of mortality are reduced by 18%.
The sooner blood flow is restored, the less extensive myocardial damage there will be.
Kinds
Depending on the timing of thrombolysis, the procedure may be:
- selective;
- non-selective.
In the first case, the drugs are administered during the first six hours from the onset of acute circulatory disorders. The main feature of the non-selective technique is the implementation of resuscitation measures during the first three hours.
Depending on the method of drug administration, thrombolysis occurs:
- local. If an examination was carried out in a hospital setting using equipment for intravascular administration, diluting agents are brought as close as possible to the affected area;
- systemic. It is used when there is no information about the location of the blood clot that caused the myocardial infarction. The drugs are administered in the usual way into a vein.
Contraindications to thrombolysis in myocardial infarction
Indications for thrombolysis in myocardial infarction are quite limited. The decision about whether such treatment is necessary is made in the ambulance or in the hospital. The procedure is practiced in the following cases:
- during the first few hours of a heart attack;
- if the death of the heart muscle has not occurred and the pain does not stop, the results of electrocardiography show the presence of a Q wave, then treatment can be carried out within the first twelve hours;
- in the presence of idioventricular rhythm;
- if an attack of acute circulatory disorder in the heart muscle is suspected.
Most often, timely use of thrombolysis gives good results. If the lesion does not affect most of the heart muscle, then the chances of survival are high.
But there are also contraindications to thrombolysis in myocardial infarction. This is due to the high probability of severe blood loss with:
- open bleeding in the gastrointestinal tract;
- hemorrhagic stroke;
- surgical interventions that have been performed recently;
- childbirth;
- traumatic brain injuries.
In these cases, treatment with thrombolytic drugs cannot be performed. Caution, it should be used when:
- aortic dissection;
- repeated attacks of heart attack;
- circulatory disorders in the brain;
- stomach ulcer;
- injuries;
- liver damage in the form of hepatitis or cirrhosis;
- glomerulonephritis;
- pregnancy;
- individual intolerance to certain thrombolytic agents.
We invite you to familiarize yourself with Medicine for VSD: what drugs and remedies to take for vegetative-vascular dystonia, treatment in Moscow
Most doctors refuse to perform thrombolysis if, shortly before the attack, the patient underwent eye surgery, especially with the use of laser technologies.
Thrombolysis for myocardial infarction helps restore blood supply to the heart muscle caused by blockage of the coronary arteries. The drugs used during the procedure dissolve blood clots.
The effectiveness of therapy reaches 95% when started in a timely manner. Despite many positive qualities, this treatment also has contraindications, to identify which an examination is performed.
Therapy is carried out in the cardiology department.
Indications for thrombolysis in myocardial infarction are:
- the most acute period of cardiac necrosis (in the first 6 hours after the attack);
- small focal lesions of the heart muscle, accompanied by severe pain and the appearance of a Q wave on the cardiogram (in this case, thrombolytics are administered within 12 hours after the onset of the acute phase of the infarction);
- severe heart rhythm disturbance;
- acute disruption of the blood supply to the heart muscle.
Absolute contraindications to the administration of thrombolytics include pathological conditions characterized by an increased risk of blood loss:
- active bleeding (including recent gastrointestinal bleeding);
- exacerbation of peptic ulcer of the stomach and duodenum;
- acute nonspecific colitis;
- acute, acute and subacute stages of hemorrhagic stroke;
- major surgical interventions;
- early postpartum period;
- previous subarachnoid hemorrhages;
- severe traumatic brain injuries.
Relative contraindications are:
- suspected coronary artery dissection;
- brain pathologies not included in the list of absolute contraindications (disorders of the blood supply to brain tissue suffered during the last 2 months);
- fresh injuries to the head, chest, abdominal and pelvic areas;
- history of internal bleeding;
- multifocal myocardial infarction, accompanied by severe cardiosclerosis;
- chronic peptic ulcer disease in remission;
- hemorrhagic syndrome;
- severe liver pathologies (cirrhosis, cancer, hepatitis);
- glomerulonephritis;
- blood clotting disorders (with hemophilia and other diseases of the hematopoietic system);
- severe arterial hypertension that is difficult to treat;
- diabetic vascular lesions;
- suspected pregnancy;
- oral anticoagulants for a long time;
- recent vascular puncture;
- laser vision correction performed within the last 2 months;
- prolonged pauses in breathing;
- history of allergic reactions to thrombolytics;
- extensive burns.
Thrombolysis for a heart attack is carried out as follows:
- An hour before the start of the procedure, the patient is placed in intensive care. Here an emergency examination is carried out to assess vital signs.
- Choice of thrombolytic. The use of 1st generation drugs (Fibrinolysin and Streptokinase) is justified only in the absence of more effective drugs. They slowly dissolve blood clots, and over time, the effectiveness of such thrombolytics decreases. Urokinase and Alteplase have a faster action. They do not cause allergic reactions and can be administered even 6 hours after the onset of an attack.
- Administration of thrombolytics. The drug is injected into the artery as a jet. The initial dose depends on the severity of vascular blockage and the condition of the patient’s body. The first stage of thrombolysis lasts 3 hours, after which they proceed to drip administration of the drug. The total dose of Alteplase should not exceed 100 mg.
Within 24 hours after completion of the procedure, it is prohibited to catheterize large vessels and give intramuscular injections. The effectiveness of treatment is determined using x-ray examination of the coronary vessels. The procedure helps evaluate the rate of thrombus dissolution, the patency of large arteries and the nature of blood flow.
The indication for thrombolysis is myocardial infarction with pathological Q waves and the ability to administer a thrombolytic in a time frame that allows hope for an improved prognosis.
A number of studies, however, have shown that survival increases when thrombolytics are administered at a later date - up to 24 hours from the moment of coronary artery occlusion.
Therefore, in certain cases, for example, with wave-like pain syndrome, you can resort to thrombolysis within 24 hours after the onset of the first symptoms.
So, indications for thrombolysis:
- ST segment elevation of more than 1 mm (0.1 mV) in two or more adjacent leads (for example, II, III, aVF)
- ST segment depression and increased amplitude of R waves in leads V1-V2 (signs of infarction of the posterior wall of the left ventricle)
- Newly diagnosed left bundle branch block Timing of thrombolytic administration:
- Less than 6 hours after pain onset: maximum effectiveness
- More than 12 hours: less effective, but if chest pain persists, thrombolysis is indicated
The main contraindication to thrombolysis is the increased risk of bleeding. Patients who have previously received streptokinase or anistreplase should not be reintroduced to either drug due to the risk of allergic reactions.
Old age is not a contraindication to thrombolysis: although in most cases it is carried out before 75 years of age, thrombolytics should be used at an older age, if there are no contraindications and severe concomitant diseases.
We invite you to familiarize yourself with Drugs for varicose veins: a review of drugs for varicose veins
So, contraindications to thrombolysis:
- Major surgery or injury in the previous 6 weeks
- Bleeding from the gastrointestinal tract or urinary tract in the previous 6 months
- Blood clotting disorders
- Suspicion of acute pericarditis, dissecting aortic aneurysm
- Resuscitation lasting more than 10 minutes
- History of intracranial tumors or brain surgery
- Acute cerebrovascular accident in the previous 6 months
- Severe arterial hypertension (BP {amp}gt; 200/120 mm Hg. Art.)
- Pregnancy
In specialized centers, an alternative to thrombolysis is primary balloon coronary angioplasty (often with stent placement). It has the greatest advantage in cases of contraindications to thrombolytics, cardiogenic shock and extensive anterior myocardial infarction.
Myocardial infarction in itself is not an indication for surgical treatment of coronary artery disease, however, in case of post-infarction angina and a positive result of a stress test performed before discharge, coronary angiography is indicated to decide on subsequent coronary bypass surgery or balloon angioplasty.
The main goal of treatment for myocardial infarction is to restore coronary blood flow in the infarct-related artery. This is achieved by using thrombolytic agents: streptokinase, streptodecase, urokinase, tissue plasminogen activator (tPA).
- The use of thrombolytics is the standard treatment for acute myocardial infarction.
- Indications for thrombolytic therapy:
- A typical anginal attack lasting more than 30 minutes and necessarily corresponding ECG changes:
- ST segment elevation in at least 2 leads and/or
The duration of the pain syndrome (myocardial infarction) is no more than 6 hours, but if anginal pain persists and the acute stage of myocardial infarction according to the ECG is up to 12 hours. The best results are achieved within the first 4 hours.
- If thrombolytic therapy is carried out in the first hour, then 51% of the myocardium is saved, within the 2nd hour - 26%, within
- 3 hours - only 13%.
- Contraindications to thrombolytic therapy:
- Bleeding, hemorrhagic syndrome.
Cerebral hemorrhage, ischemic stroke (up to 3 months old).
Allergy to thrombolytics.
Gastric ulcer and 12 s.c. in the acute stage.
- Age 75 and older.
- Fresh severe injuries, operations or “abdominal” biopsies.
- Uncontrolled hypertension BP {amp}gt; 180/100.
- Pregnancy or conditions after childbirth.
- Diabetic hemorrhagic retinopathy.
- Chronic or acute renal failure.
- Tooth extraction no earlier than 14 days.
- Prolonged cardiopulmonary resuscitation.
- The use of thrombolytics for small focal infarction and unstable angina is not justified, since their effectiveness in these conditions has not been proven.
1.0 million - 1.5 million IV drip per 100.0 ml of physiological solution for 30 minutes.
1.5 million as a bolus.
1 million IV infusion – 1 hour.
- 30 mg over 2-3 minutes
- tPA (tissue plasminogen activator
- Bolus 15 mg, then infusion 0.75 mg/kg/min over 30 minutes, then 0.5 mg/kg/min over 1 hour
- Before the administration of streptokinase, prednisolone 60 - 90 mg is administered.
Over three years, 21 systemic thrombolysis (ST) was performed with Streptokinase at a dose of 1.5 million. Unfortunately, the amount of the drug is not enough, but there are more than 70% of patients with contraindications for CT.
- Hemorrhages: intracranial and systemic.
- With the introduction of streptokinase, the risk is 1%, with tPA (tissue plasminogen activator) - 1.3%.
- Prevention of bleeding: correct choice of indications, do not perform intramuscular injections, do not perform central venous catheterization.
Thrombolytic therapy and its side effects
Thrombolysis for myocardial infarction is the procedure for administering special drugs that eliminate clots (thrombi) in blood vessels. Many cardiologists do not dare to perform it, since bleeding (from micro to serious internal) may occur afterwards.
However, thrombolysis is often necessary to save a person's life. A competent person should know about the intricacies of the procedure, the drugs used and possible complications.
Who may need thrombolysis
Everyone knows what myocardial infarction is. The first associations are a formidable cardiac pathology, for which one should not hesitate to seek medical help. In the sixties of the last century, heart attacks claimed lives with shocking frequency: mortality exceeded 45% of cases.
Nowadays, when there are intensive care units with special equipment, the number of deaths has almost halved. Thrombolytic drugs have become the main link in resuscitation therapy. Thanks to them, the upper threshold of death from a heart attack does not exceed 7%.
The fact is that thrombosis is the key cause in 94% of attacks. Often its development occurs against the background of rupture of atherosclerotic plaques.
The goal of doctors is to restore the patency of the blocked vessel as quickly as possible and reduce the spread of myocardial infarction.
Reperfusion (resumption of normal blood flow) helps prevent expansion of the infarct zone and minimize a number of other dangerous consequences.
If thrombolytic drugs are administered within the first twelve hours, mortality rates are significantly reduced.
More about blood clot resolution
Eliminating the clot helps restore blood flow in the vessel. The thrombolysis procedure, carried out at the moment when the clot has just formed, saves an impressive part of the heart cells from death.
The thrombolytic agent is administered intravenously at minimal speed. Streptokinase is considered one of the most accessible and widespread drugs. Despite this, doctors do not recommend repeated administration of it, as side effects in the form of allergies may occur.
Methodology for the thrombolysis procedure
The thrombolysis procedure is carried out with an approved series of drugs that promote the transformation of bulk plasminogen into an enzyme that destroys blood clots (plasmin). The goal is to free the artery bed and restore its capacity.
Medicine, as they say, has stepped forward. And if previously the optimal effect was considered to achieve at least some patency, today thrombolytic therapy for myocardial infarction helps restore adequate blood flow, limit the spread of pathology, preserve left ventricular function and guarantee a favorable prognosis.
When should the procedure be performed?
Typically, cardiologists who offer the thrombolysis procedure emphasize that this must be done within the first hour after the blood clot has formed. This measure allows you to avoid deaths from heart attacks and deaths within a year after the attack.
Timely administration of thrombolytics helps to avoid destruction of the septum separating the ventricles, ventricular arrhythmias and cardiogenic shock.
Late administration of thrombolytics
The period when cardiac “tissue” can be saved varies from one to three hours. However, you can reduce the likelihood of death if you start therapy and within three to six. A thrombolysis procedure performed after six to twelve hours is considered less effective, but still not useless, especially if the pain syndrome persists.
Thrombolysis brings good results when it comes to anterior infarction (extensive myocardial trauma). In any case, this procedure gives additional chances of survival (regardless of the age of the victim).
Indications for thrombolysis
Indications for the thrombolysis procedure are:
- suspicion of a heart attack (anginal syndrome is pronounced, lasts more than thirty minutes);
- there is a blockade of the electrical conduction system of the heart (in particular, the left bundle branch).
The standard period of time between symptoms becoming apparent and the first measures being taken is usually twelve hours.
Contraindications for the procedure
Despite all the positive spectrum of action, thrombolysis also has a number of contraindications. They are divided into absolute and relative.
| Internal bleeding that has occurred within the last fourteen days | Any surgical intervention or traumatic brain injury that occurred within two weeks |
| Elevated blood pressure (above 200/100) | Symptoms of hemorrhagic diathesis in response to the thrombolysis procedure |
| Traumatic brain or other injuries, surgery in the last couple of weeks | Known or suspected diabetes mellitus |
| Peptic ulcer of the stomach in the active phase | Liver or kidney problems (liver or kidney failure) |
| Cardiologists suspect hemorrhage in the pericardial region | |
| Suspicion of aortic aneurysm | |
| An allergic reaction to a drug that is planned to be used for thrombolysis | Use of anticoagulants for six months |
Methods for assessing the effectiveness of therapy
Using coronography, which is similar to an X-ray for the circulatory system, you can make sure that the thrombolysis procedure is not a layer-by-layer washing away of a clot (thrombus), but the appearance of holes in it. At the same moment, the blood clot is restored. The method is effective when thrombolytics act faster than thrombus restoration.
Unfortunately, sometimes victims of a heart attack experience a secondary formation of a blood clot.
The effectiveness of therapy can be assessed using a cardiogram and standard blood tests.
A sign of positive dynamics is considered to be a decrease in pain. Angiography is performed within one and a half hours after the start of the thrombolysis procedure. Basically, it demonstrates that arterial patency has increased.
Thrombolytic therapy is assessed using a special scale. It shows how much blood circulation has been restored:
- A zero degree indicates that the contrast agent is not visible below the level affected by thrombosis, and there is no blood flow.
- The first degree indicates that there is a weak blood flow that is not able to fill the artery.
- The second degree speaks in favor of the fact that there is a slow blood flow.
- The third degree indicates that there are no more problems with patency, adequate blood flow has been restored.
The effectiveness of thrombolysis involves several factors. The most important thing is to start therapy as early as possible. We recommend reading the article about myocardial infarction and its consequences. From it you will learn about the symptoms and causes of the problem, diagnostic methods, therapy and possible complications.
Complications after thrombolysis
It is precisely because thrombolytic therapy has many pitfalls that doctors are afraid of it. Side effects may appear if the drug and method of trobolysis are selected incorrectly, as well as if absolute or indirect contraindications are not taken into account.
| It occupies a leading place in the list of possible complications: from twenty to sixty percent of patients who have had a heart attack have encountered it | |
| Coronary artery reocclusion | Occurs in fifteen to twenty percent of cases. The course is often asymptomatic. To prevent this complication, a solution of nitroglycerin and heparin is administered. |
| Traditionally, it is corrected by the rate of administration of thrombolytics. | |
| Allergy to thrombolytic drugs | Requires immediate termination of the procedure. And depending on how severe the symptoms are, the use of antihistamines, hormonal therapy, bronchodilators and adrenaline (if the patient has anaphylactic shock). |
| Intracranial hemorrhage | This diagnosis is one of the major obstacles to the introduction of thrombolytic drugs becoming a generally accepted measure. |
| A complication typical for mature patients with an uncontrolled increase in blood pressure and numerous neurological diagnoses. The administration of thrombolytics is contraindicated for these people. |
Effective thrombolysis, unfortunately, cannot guarantee the elimination of ischemia and recurrent infarction in the future. In addition, the administration of thrombolytics does not exclude recurrent thrombosis with the development of a heart attack.
The introduction of drugs, as they say, is a “double-edged sword”: on the one hand, effective help, on the other, dangerous complications. However, when life hangs in the balance, it is best to trust the experts.
Source: https://CardioBook.ru/thrombolizis-pri-infarkte-miocarda/
Efficiency mark
The degree of effectiveness of thrombolytic therapy is assessed using coronary angiography. Thanks to this study, a decrease in the size of the blood clot and the degree of patency of the coronary vessels are determined within 30 minutes after the start of treatment. In some cases, repeated thrombus formation is detected.
The results of thrombolysis are assessed using electrocardiography and blood tests, as well as using a special scale from zero to three:
- with zero efficiency, there is no blood flow and the contrast agent is located below the site of blood clot formation;
- blood circulation is weak, due to which the arterial bed is not completely filled through small holes in the thrombus;
- blood flow is slowed down, partial filling of the bed is observed;
- the lumen of the artery was completely filled with a contrast agent, which indicates that the thrombus has completely resolved and the patency of the vessel has been restored.
Thanks to timely treatment, the risk of developing cardiogenic shock and other consequences can be reduced.
Complications
In rare cases, thrombolysis is accompanied by the development of complications. Some patients experience bleeding after administration of the drug. At the same time, hematocrit and hemoglobin quickly decrease. A blood test shows a decrease in platelet count. If this happens, then treatment is stopped and other methods are used.
Every tenth patient experiences a sharp decrease in blood pressure. Recovery of the condition is noticed after cessation of therapy.
The prognosis after thrombolysis for a heart attack is favorable in most cases. The procedure significantly increases the chances of recovery.