What to do?
Why is it necessary to combat low hemoglobin?
To prevent symptoms from developing.
Both oncology and its treatment definitely cause a lot of trouble for the patient. If you add the symptoms of anemia to them, then treatment can turn into a nightmare.
What medications can help?
The most common answer to the question: “How to increase hemoglobin in oncology?” – medicines. Unlike diet, they can help at any stage. A few common examples:
Totema, solution for oral administration. Description: the drug consists of iron, copper and manganese. The last two elements improve the absorption of the main substance. Contraindications: allergies to components, hemochromatosis, hemosiderosis, thalassemia, stomach or intestinal ulcers during an exacerbation, intoxication with manganese, copper or lead, age up to 3 months. Price: 440 rub. for 20 ampoules.
Maltofer Fol, chewable tablets. Description: a combination of iron and folic acid. Contraindications: hypersensitivity, gastric or duodenal ulcer. Price: 530 rub. for 30 tablets.
Sorbifer Durules, tablets. Description: iron and ascorbic acid. The latter is extremely useful for immunity, which decreases during chemotherapy. Contraindications: individual intolerance, esophageal stenosis, excess iron in the body, age under 12 years. Price: 380 rub. for 30 tablets.
Aktiferrin, syrup. Description: a combination of iron and serine, which accelerates absorption in the gastrointestinal tract. Contraindications: allergies, severe iron absorption disorders, increased iron content in the body. Price: 210 rub. for 100 ml.
Ferro-Folgamma, capsules. Description: iron, folic acid, vitamin B12. Contraindications: hypersensitivity to components, liver failure, hemosiderosis, hemochromatosis, some types of anemia. Price: 600 rub. for 50 capsules.
Diet
It should be noted that it is possible to increase hemoglobin with the help of diet only in the early stages of cancer.
In addition, before using the diet, you must undergo all tests and consult with a doctor: an unreasonably increased hemoglobin is no better than a decreased one.
Products that raise hemoglobin: apples, nuts, peas, beans, liver, rose hips, currants, cereals (oatmeal, buckwheat). The best way to increase hemoglobin is with pomegranate juice (drink 500 g in the morning, on an empty stomach, for 30 days), but this pleasure is not cheap.
There are no definitely prohibited foods, but very fatty foods and rice (if it dominates the diet) can reduce the amount of iron absorbed.
Sample menu for several days
Day 1:
- Breakfast: 500 g of pomegranate juice.
- Lunch: a plate of cheese soup, pasta with tomato paste and beans (200 g).
- Dinner: green salad, compote (currants, rose hips, cherries).
Day 2:
- Breakfast: 500 g of pomegranate juice.
- Lunch: 200 oatmeal, 150 g boiled chicken, bread.
- Dinner: unlimited apples.
Day 3:
- Breakfast: 500 g of pomegranate juice.
- Lunch: rice soup (plate), stewed liver (150 g).
- Dinner: 100 g of nuts.
What to do to normalize hemoglobin before surgery?
Nothing. Firstly, you cannot eat before the operation, so there is no “food” solution to the problem. Secondly, you should also not take medications on your own before surgery, because this can have a very bad effect on the course of the surgical intervention.
In general, it is better to ask your doctor this question, and if he thinks that it makes sense to raise hemoglobin before surgery, then he will advise the right way.
Other methods
There are 2 methods that doctors use when diet and medications do not help:
- injections of iron into the bloodstream;
- blood transfusion.
Both methods are used for moderate to severe anemia.
Symptoms of pathology
It is easy to determine the level of iron in the blood; all you need to do is take a blood test at a local clinic or diagnostic laboratory. The reason for taking the test may be an examination related to a visit to the doctor or the presence of obvious signs indicating anemia.
The most common symptoms of anemia include:
- Palpitations and difficulty breathing.
- Fainting and dizziness.
- Pain in the head, sensation of tinnitus.
- Feeling of weakness and pain in the muscular system.
- Changes in taste and smell.
- Changes in the structure of nails.
- Thinning, dry hair.
- Paleness and dryness of mucous membranes and skin.
- Prolonged lethargy, apathy, fatigue, depression.
- Low blood pressure, abnormalities in the operation of the VGT system, cold lower extremities.
If the quantitative value of iron has not decreased much, then a person may not even be aware of it. Or he begins to worry about a persistent feeling of fatigue, even after a full night's sleep, although anemia is often accompanied by insomnia.
Such sensations are caused by oxygen starvation of the body due to a lack of iron-containing protein in red blood cells in the blood or a decrease in their number or volume. After all, as you know, it is the red blood cells that are entrusted with one of the most important missions of supplying all organs, systems and tissues of the body with oxygen and the subsequent removal of carbon dioxide.
Symptoms of anemia depend on the level of hemoglobin in the body. When the readings drop to 90, patients experience impaired concentration and memory. If hemoglobin decreases by another twenty units, a person develops shortness of breath, tinnitus, and arrhythmia.
- deformation of the nail plates due to their depletion;
- dry skin and mucous membranes;
- formation of cracks around the oral cavity;
- taste disturbance;
- increase in body temperature.
Cancerous anemia can be diagnosed using a laboratory blood test. Such a study must be carried out repeatedly throughout the course of treatment of the pathology, which makes it possible to assess the dynamics of the development of a cancerous tumor. It is also recommended to monitor your blood sugar levels.
Reasons for decreased hemoglobin in the blood in oncology
Hemoglobin levels may change during cancer for various reasons
It is important to establish the reason for the decrease in protein concentration in each specific case in order to know how to increase hemoglobin and prevent complications of the disease in the future
The cause may be due to internal bleeding. Oncopathology often causes such a complication, especially with the active progression of a malignant tumor or against the background of an adverse reaction from prescribed therapy. Other reasons that may contribute to a decrease in serum hemoglobin levels are also identified:
- gastrointestinal dysfunction resulting from problems with iron absorption;
- spread of metastases to the bone marrow;
- loss of adequate nutrition (with cancer of the stomach, esophagus or intestines), resulting in iron deficiency in the body;
- the use of potent drugs and procedures (chemotherapy or radiation), the adverse reactions of which are a decrease in the ability to form hematopoiesis;
- acute intoxication of the body, due to the constant growth and disintegration of a malignant tumor in the last stages of oncology.
How to increase hemoglobin in newborns?
If a child is diagnosed with low hemoglobin, then there are two options for solving this problem. The first is nutrition (apples, pomegranate, liver, and cattle meat are recommended). The second option is drug treatment. Doctors try to use this method of restoring health only in a critical situation.
There are cases in which pregnant women experience low hemoglobin. In this case, the body is restored with the help of medications or special products. Negative consequences for the body also occur if there is high hemoglobin: the blood becomes thick, internal organs work worse. There is a predisposition to strokes and heart attacks.
In order to normalize hemoglobin levels, you need to review your diet. If this does not help, then you should consult a doctor who will prescribe medication.
How does a blood transfusion occur to restore hemoglobin?
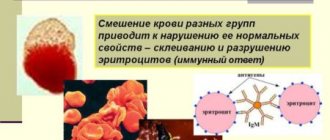
The process of blood transfusion with reduced hemoglobin readings is called blood transfusion in medical terminology. It is carried out only in a hospital setting and under the watchful supervision of medical personnel. Blood is transfused to increase iron levels from a healthy donor to a recipient. The procedure is possible only if the blood type and Rh factor match.
Sequence of mandatory actions during blood transfusion:
- The doctor finds out whether there are good reasons for blood transfusion, and whether there are any contraindications. In this case, collecting an anamnesis is mandatory; it is necessary to find out from the patient whether a blood transfusion medium has previously been transfused to increase hemoglobin, whether allergic reactions or side effects have occurred, the presence of chronic diseases and other individual characteristics of the body that need to be taken into account.
- After laboratory tests of the patient’s personal blood parameters, such as group and Rh factor. Additional confirmation of the initial data will be required on site, that is, in the hospital. To do this, a repeat analysis is carried out in a medical institution, and the indicator is compared with the laboratory one - the data must completely match.
- Select the most appropriate donor red blood cell mass for blood transfusion with low hemoglobin. If there is even the slightest discrepancy in even one indicator, blood transfusion to increase hemoglobin is not permitted. The doctor must make sure that the packaging is sealed, and that the passport contains all the information regarding the number and date of the preparation, the name of the donor, his group and rhesus, the name of the organization of the preparation, the expiration date and the doctor’s signature. The storage duration of donor hematotransfusion composition varies from 20 to 30 days. But even with full compliance with all the indicators during a visual inspection, a specialist should not find any foreign clots or films in it. After a thorough quality check, a repeat analysis is carried out to confirm the group and rhesus.
- Compatibility is checked using the AB0 system, in which the donor’s blood is combined with the recipient’s blood on a special glass.
- To check the compatibility of the Rh factor, two parts of the patient’s serum mass, one part of the donor’s blood, part of the polyglucin, 5 milliliters of saline are added to a special test tube and the reaction is observed while rotating.
- After studying the compatibility data, a biological test is carried out by injecting the recipient with 25 milliliters of donor blood. It is administered three times with an interval of three minutes between injections. At this time, the patient is closely monitored; if the heartbeat and pulse are normal, the face has no signs of redness and general health is stable, then the plasma is allowed for transfusion.
- Blood is not used in its original form; its various components are transfused depending on the intended purpose. If hemoglobin is low, packed red blood cells are transfused. This component of the blood flow is administered by drip at a rate of 40–60 drops per minute. The patient must constantly be under the supervision of a doctor, who monitors his general well-being, pulse, blood pressure, temperature, skin condition, and subsequently enters the information into the medical record.
- At the end of the process, the patient needs rest for two hours. He remains under doctor's supervision for another day, then has his blood and urine tested.
- After the transfusion is completed, approximately 15 milliliters of the recipient's blood serum and the donor's red blood cells are left. They are stored in the refrigerator for about 2 days, if there is a need to do an analysis, in case of complications.
Blood transfusion for anemia is not allowed for everyone, with the exception of people with a rare blood type. Restoration of hemoglobin in them can be carried out only with the use of iron-containing drugs and a special diet, including foods rich in iron.
Is it possible to have surgery with low hemoglobin?
Is it possible to have surgery with low hemoglobin? Any surgical intervention is a kind of stress for the human body.
Anesthesia, violation of the integrity of the skin and possible bleeding during surgery negatively affect the person’s condition, despite the fact that all these actions are aimed at restoring his health.
A normal hemoglobin level plays an important role during surgery, as well as for recovery after it.
Hemoglobin and its functioning in the blood
Blood contains cells of various shapes and colors. Red cells are oval in shape with a depressed middle and are called red blood cells. This is necessary to transport oxygen molecules to the body's cells and carbon dioxide to the lungs.
Inside red blood cells there is a substance that consists of the protein part of globin and the red pigment heme, which contains iron. The interaction of iron with oxygen, which it binds in the lungs for further transportation, gives the blood its red color.
For different age categories, there are different norms for the number of red blood cells in the blood and the composition of hemoglobin in them. Low and high hemoglobin levels are harmful to the body.
Insufficient hemoglobin in the blood causes:
- decreased blood pressure;
- tachycardia with subsequent development of cardiomyopathy;
- drowsiness, weakness;
- anemia;
- change in taste;
- deterioration in appearance;
- liver enlargement;
- swelling of the lower extremities.
Low hemoglobin does not perform the respiratory function of the body and causes oxygen starvation of cells with the subsequent development of pathological abnormalities. In tissues, metabolic processes are disrupted with the appearance of the above symptoms.
Low hemoglobin and surgery
During surgery, it is necessary that the blood test readings are as close to normal as possible. Due to the severe impact on the body, its rapid recovery is important, which is possible with the healthy function of its systems and organs.
In the postoperative period, hemoglobin levels decrease due to various unfavorable factors:
- The loss of blood that occurs during surgery reduces its volume and the quantitative composition of cells in it. The level of red blood cells and hemoglobin also drops. This entails the development of hemorrhagic anemia. Carrying out anesthesia, which can adversely affect various organs and systems of the body. Anesthesia, despite its analgesic function, can cause harm to the patient if its dosage is incorrect, or if the individual characteristics of the patient have not been taken into account. There are some types of anesthesia that affect respiratory function and oxygen transport in the blood.
- Performing abdominal operations on various organs. If this surgical intervention is performed in the gastrointestinal tract, then the process of absorption of various substances changes for the worse. Iron, vitamin B12, folic acid are responsible for hematopoiesis. They do not enter the body in sufficient quantities, which leads to the development of deficiency anemic conditions.
The operation takes into account the risk of bleeding, which can occur due to damage to large vessels, as well as insufficient pressure on them with clamps. This danger is predictable, therefore, if expected blood loss occurs, an immediate blood or plasma transfusion is performed.
Reduced hemoglobin before surgery
Knowing about the problems that can arise during and after surgical interventions, you can understand the reason for the ban on surgery with low hemoglobin.
The postoperative recovery period is also of particular importance. It depends on the state of hemoglobin, therefore, before the start of surgical treatment, a series of examinations are prescribed, which take into account the state of the blood, urine, as well as the functioning of all organs and systems.
Observation of patients during the recovery period gives every reason to assert that the development of an anemic state after surgery increases by half the likelihood of developing serious complications and an unfavorable outcome. Therefore, doctors take into account the ratio of red blood cells to total blood volume - this figure should be at least 30%. This proportion of formed units of blood in its liquid part is called hematocrit.
Hemoglobin concentrations below 100 g/l are a contraindication for surgery. A reduced blood protein level of up to 100 g/l is manifested by mild anemia. Such indicators allow only urgent surgery.
When anesthesia is administered, the anesthesiologist takes into account the development of some life-threatening conditions with reduced hemoglobin:
- a sharp drop in blood pressure;
- deterioration in the activity of the heart muscle;
- deterioration of blood microcirculation;
- change in blood picture.
If there are no emergency indications for surgical intervention, then first of all it is necessary to find out the origin of the reduced hemoglobin level and neutralize it (followed by treatment of anemia).
If hemolytic anemia forms in the body, then its exacerbation begins in the postoperative period. Therefore, if bleeding develops during surgery, there is a possibility that the body will not be able to cope with the load due to the initially low level of hemoglobin in it.
Operation prohibited
Why can't you have surgery if you have low hemoglobin? Before surgery, it is necessary to cure any of the existing types of anemia. However, not all types of this blood disorder respond well to treatment.
When a patient develops hereditary sickle cell anemia, in which the shape of red blood cells and the structure of hemoglobin in them changes, the case is considered a severe and extremely dangerous condition for surgery.
In this case, only blood transfusion before and after surgery, taking into account vital signs, can increase the level of hemoglobin in the blood.
Such anemia is treated symptomatically throughout the patient’s subsequent life.
When carrying out urgent surgical intervention, the following factors must be taken into account:
- available emergency indications;
- risk of blood loss;
- performing surgical treatment of anemia.
In other cases, you first need to increase the hemoglobin level, and only then can anesthesia and surgery be performed. If urgent surgery is required to save a person, and the hemoglobin is below the required unit, then the patient needs to undergo a blood transfusion.
Blood transfusion is the only way to normalize a person’s health status. This procedure can also be called an operation, since there is an intervention in an internal human organ - the blood.
Transplantation of one's own or someone else's blood is carried out in a hospital setting under the close supervision of medical personnel. Transfusion can cause undesirable consequences that are difficult to predict.
They can be very serious, even fatal.
If the body develops deficiency anemia with a lack of iron or vitamin B12, then there is a possibility of developing serious complications during surgical intervention. If planned surgical treatment is planned, then it is necessary to restore blood counts closer to normal. This may take a long time.
It is important to know that patients with a hematocrit level less than 28% before surgery have a high risk of death within 30 days after surgery due to increased wear and tear on the heart muscle.
Treatment of anemic conditions after surgery
The principles of correction of low hemoglobin levels in the postoperative period are not much different from the treatment of other anemic conditions:
- Nutrition with sufficient protein, vitamins and minerals, which are aimed at repaying the deficiency of the missing substances for normal hematopoiesis in the body.
- Iron supplements, vitamin B12 injections.
- Vitamin C, folic acid and digestive enzymes to improve nutrient absorption function.
- Symptomatic treatment of internal organs.
- Blood transfusion for life-long indications.
Therapy for each patient is strictly individual. Therapeutic nutrition must be followed for a long period, and sometimes for life.
In order for hemoglobin to be within normal limits, it must be regularly monitored. Periodic donation of blood for analysis will help to detect anemia in a timely manner and treat it in a timely manner.
Source: https://BolezniKrovi.com/sostav/gemoglobin/operaciyu-pri-nizkom-gemoglobine.html
The importance of hemoglobin for the body
Hemoglobin (Hb) is a protein of the chromoprotein class that contains iron in red blood cells. Provides the transport function of oxygen (O2) throughout all tissues, systems and organs, and transports carbon dioxide. Partially found in plasma. There are approximately 400 million hemoglobin molecules in a red blood cell. In addition to participating in gas exchange, Hb is involved in maintaining the acid-base balance.
WHO has developed recommended standards:
- 110 g/l from six months to five years;
- 115 g/l from 5-11 years;
- from 120 g/l in adolescents 12-14 years old and up to 140 g/l; women 18-70 years old up to 160 g/l;
- from 130 in boys over 14 years old and up to 160 g/l; from 18-75 years to 180 g/l.
The level changes naturally. Reference values must be taken into account. Therefore, at what value of hemoglobin the operation can be performed can only be answered by a doctor.
Anemia and its types
Anemia, as a result of a critical decrease in hemoglobin, occurs in acute or chronic forms. Acute occurs when there is sudden bleeding.
Chronic in the case of gradual development of a pathological condition in which the body adapts to new conditions for oxygen transportation.
In this case, it affects the brain, both the peripheral and central nervous system, heart, muscles, gastrointestinal tract, and organs of the urinary system.
Depending on population groups, there are 3 types of anemia:
- light (lowest rate, children aged 0.5-5 years and pregnant women - 100-109 g/l);
- moderate (the lowest indicator for the same groups is 70-99);
- acute (lowest rate, children from six months to 5 years and pregnant women - less than 70).
The Hb level in the blood must be taken into account in conjunction with elements such as: average erythrocyte volume, average Hb concentration in one erythrocyte, serum iron, hematocrit.
At what Hb value is surgery possible?
During the period of surgical intervention, the human body is exposed to external stress, which affects the number of red blood cells in the blood, as a result of which the Hb level drops. The operation is carried out with tests as close to normal as possible. In the postoperative period, the patient requires recovery, and the hemoglobin level is one of the most important indicators indicating this.
There are a number of reasons why anemia may occur:
- Copious blood loss. The number of red blood cells naturally decreases, resulting in hemorrhagic anemia.
- General anesthesia. During anesthesia, blood pressure is artificially lowered, blood microcirculation is disrupted, and its composition changes.
- Operations on certain organs. For example, in the case of manipulations on the stomach or intestines, the processes of iron absorption are disrupted, and the absorption of folic acid and vitamin B12 slows down.
Therefore, if hemoglobin in the blood is below 100 g/l (mild anemia), then surgery is contraindicated. Moderate and acute anemia requires treatment before surgery. If emergency surgery is required, red blood cell transfusions are used.
How to deal with anemia
Anemia is a condition when red blood cells and their capabilities are insufficient to carry oxygen, and as a result, insufficient satisfaction of physiological needs.
Methods to increase hemoglobin levels:
- Diet (protein diet with sufficient vitamins and minerals). The richest source is red meat and organ meats. And also buckwheat, beans, lemons, cabbage, rose hips.
- Taking medications with di- and trivalent Fe.
- Injections.
- Transfusion of blood plasma or red blood cells.
- Taking vitamin C, hematogen, folic acid, digestive enzymes.
- Complex therapeutic treatment in a hospital.
- Folk methods.
Hemoglobin levels can radically affect a person’s life both in the preoperative period and during the recovery period after surgery. Therefore, if surgical treatment is necessary, it is important to undergo an examination prescribed by a doctor to identify possible risks. If the Hb indicator is not normal, then measures should be taken taking into account the characteristics of the body.
Source: https://krovinfo.com/pri-kakom-gemoglobine-mozhno-delat-operaciyu/
Consequences of transfusions
Low hemoglobin does not always return to normal after a blood transfusion. Moreover, the procedure itself can be very dangerous for the patient. After it, the patient must spend at least a day in a state of absolute rest. On the second day, additional tests will be scheduled, and only if everything is fine, the person can be transferred to the general ward.
The following are considered as negative consequences:
- Muscle pain.
- Hives and other allergic rashes on the body.
- Decrease in blood pressure levels.
- Increased body temperature.
- Severe migraines.
- Swelling of the limbs, nausea, vomiting.
- Interruptions in heart rate.
Almost everyone who is about to undergo this procedure asks the question: is a transfusion dangerous? It is dangerous, therefore all patients are in the hospital until vital signs and hemoglobin levels stabilize.
Consequences and complications of blood transfusion
In approximately 1-2% of cases of the total blood transfusions performed for cancer, complications are likely to develop. The most common complications are the following:
- increased body temperature;
- impaired coordination of movements;
- jump in blood pressure;
- facial redness;
- breathing problems;
- nausea and vomiting;
- hematuria.
If such complications are identified at an early stage, the consequences can be eliminated. Due to the risks, patients are advised to remain in the hospital for 2-3 days after the transfusion.
Why does hemoglobin drop in cancer?
With the emergence and progression of a malignant process, a number of pathological biochemical reactions are activated, leading to changes in the functioning of internal organs and the development of complications. Most often, disorders affect the hematopoietic, immune, cardiovascular, and respiratory systems.
The first diagnostic symptom is a low level of hemoglobin in developing oncology, due to which the disease can be suspected and timely measures can be taken.
Reasons for decreased hemoglobin and red blood cells:
- failure of the red bone marrow due to intoxication with cancer decay products and metastases;
- tumor in the bone marrow, its damage;
- intoxication with decay products of malignant tumors;
- triggering of immunity and excessive synthesis of tumor necrosis factor, interleukin, interferon. Cytokines reduce the lifespan of red blood cells to 90-60 days, when the norm is 120 days;
- internal bleeding associated with a nearby blood vessel and tumor;
- prolonged hemorrhage directly from the neoplasm;
- receiving radiation and chemotherapy. Capable of destroying mature erythrocyte cells, as well as immature precursor cells;
- inhibition of erythropoietin synthesis in the kidneys after aggressive treatment;
- surgical manipulations for excision or removal;
- insufficient nutrition of the patient or complete refusal of food.
Anemia requires additional laboratory and instrumental examinations to establish the root cause of changes in clinical blood test.
Contraindications to blood transfusion
The list of contraindications to blood transfusion includes:
- acute allergy;
- vascular and heart diseases;
- hypertension 3 degrees;
- circulatory disorders;
- pulmonary edema;
- thromboembolism;
- asthma;
- changes in the functioning of the central nervous system.
In case of acute anemia due to the oncological process, the transfusion procedure is carried out without considering contraindications. Health care providers must consider the need to provide means to prevent complications.
Normal quantity
In utero and in babies under one year of age, fetal hemoglobin with a high degree of chemical affinity for oxygen participates in hematopoiesis.
The replacement of the fetal form with the glycolyzed one, inherent in the adult body, begins even before birth and is completed upon reaching one year.
Fetal protein transfers oxygen to tissues worse, so physiological anemia may begin after birth.
A decrease in the level of hemoglobin in the baby’s blood after birth is sometimes associated with a natural sharp increase in blood pressure after childbirth. Suppression of hemoglobin synthesis by the bone marrow occurs.
Do not confuse physiological anemia with iron deficiency, which can appear after four months from birth.
Physiological occurs when the body’s ability to synthesize hemoglobin decreases. And iron deficiency is when there is a lack of iron in the body or poor absorption of it.
What hemoglobin should a newborn, one-month-old and one-year-old child have?
Table of normal hemoglobin readings in an infant born at term.
| Age | Blood level, g/l |
| 1 day | 190-195 |
| Day 3 | 180-186 |
| Day 7 | 182-188 |
| 14 days | 172-177 |
| One month | 135-140 |
| Two month | 110-115 |
| Three months | 114-116 |
| Four months | 120-125 |
| From six months to a year | 122-127 |
With a premature birth, the baby’s body experiences extreme stress, since the transition of fetal hemoglobin to normal has not yet begun. Therefore, he begins to suffer from oxygen starvation.
Naturally, the level of the protein in question in the blood of such children differs from full-term ones.
Table of normal hemoglobin levels in premature infants up to one year old.
| Age (in days) | Blood level, g/l |
| 1 | 188-193 |
| From 2 to 5 | 186-190 |
| From 10 to 17 | 150-155 |
| 23 – 25 | 112-115 |
| 37 – 55 | 89-93 |
The second table presents data for premature babies up to approximately two months, as this is their most vulnerable period.
The considered indicator reaches a minimum value at two months, as in full-term children, but its level is noticeably lower.
From all of the above, the following conclusions can be drawn:
- everyone is born with an increased level of hemoglobin in the blood compared to the average (see tables), regardless of the degree of term;
up to two months in children, the level in the blood decreases due to the presence of the fetal variety, which is very reluctant to part with oxygen.
In premature babies, the value of the indicator drops more sharply than in full-term babies. Such babies should be under the supervision of a doctor to receive the necessary treatment.
After two months of life, the amount of glycated blood begins to increase noticeably.
The consequence of this is an increase in its level to average statistical values (120-130 g/l) by year.
Normal indicators and manifestations of anemia
The hemoglobin level in the blood during cancer indicates the state of the body as a whole during the course of the disease and the degree of effectiveness of the therapy. Sufficient protein content in red blood cells ensures the transport of oxygen to tissues and organs, creating unfavorable conditions for the growth of cancer cells.
The normal value for males is 140 g/l, for females – 120 g/l. Quite often, specialists in the field of oncology do not attach much importance to low numbers, perceiving them as part of the diagnosis, which is fundamentally wrong.
A decrease in hemoglobin levels can have various manifestations:
- weakness, fatigue;
- frequent dizziness;
- pale skin;
- thinness and fragility of nail plates;
- dyspnea;
- pain in the chest area;
- cardiopalmus.
The lack of adequate therapy and timely correction can lead to the development of respiratory and heart failure and disruption of the functioning of the nervous system.
Why is a low level dangerous?
If there is a lack of hemoglobin, the baby’s body experiences oxygen starvation, so low hemoglobin in a one-year-old infant and younger is fraught with:
- decreased immunity;
developmental delay; disruption of the functioning of internal organs, including the brain.
For the formation of hemoglobin you need not just iron and products containing it
It is important that the body can absorb it, that is, synthesize it
Breastfeeding or bottle feeding
Breast milk contains very little iron. The newborn draws iron from its reserves, which it created in the womb.
Mother's milk contains a complex protein - lactoferrin, which promotes almost complete absorption of iron from external sources.
If the mother does not have milk, then this is not a reason for frustration. Modern infant formulas contain iron supplements that are easily absorbed by the baby.
At the same time, he does not even have to completely use up his iron supply.
What to do to increase volume
If an infant's hemoglobin drops, it is necessary to act: for the formation of this protein, of course, iron is needed.
It is the main building material coming from external sources. The body cannot create iron on its own.
And for the complete absorption of microelements, the following substances are necessary:
- glutamic acid and arginine. Scientists have not yet fully understood the intricacies of the issue, but they have found out absolutely precisely: without these substances, iron is not absorbed;
trace elements copper and cobalt. They play the role of catalysts; B vitamins, especially vitamin B12; vitamin C, that is, ordinary ascorbic acid.
Nature has acted very wisely by creating products containing all these substances, except vitamin C. These include nuts.
Peanuts are the leader in the content of both iron and substances that promote its absorption. Then follow sesame and walnuts.
Therefore, a nursing mother, in the absence of gastrointestinal problems, needs to eat 50 g of any nuts every day, washing them down with rosehip decoction or other fruit juice to prevent anemia in herself and her baby.
When asked whether it is possible to increase hemoglobin in a child’s blood with food, Dr. Komarovsky answers:
What to do if you have low hemoglobin: methods of normalization, foods and medications, tips
Very often, when complaining of poor health or during a preventive examination, the attending physician prescribes tests to check the level of hemoglobin in the blood. However, not everyone has an idea of what kind of protein it is, what role it plays in the human body and what to do if hemoglobin is low.
What is hemoglobin and its normal level in the body?
Hemoglobin is an iron-based protein whose main purpose is to combine with oxygen and transport it throughout the body. Moving in the opposite direction, it collects carbon dioxide and carries it through the blood vessels to the lungs, and through them it is expelled. Before you think about what to do if you have low hemoglobin, you need to know the normal level in the blood.
There is an indicator of the hemoglobin norm at which the body functions normally:
- for men, the normal level of hemoglobin in the blood is from 130 to 170 g/l;
- for women from 120 to 150 g/l;
- for pregnant women and women during breastfeeding 120-140g/l;
- for infants up to 3 months 160-240 g/l;
- 3-12 months – hemoglobin decreases significantly and a level of 100-150 g/l is considered normal;
- from the first year of life, depending on the sex of the child, approximate or the same indicators as in an adult are considered the norm.
Causes of anemia
If we talk about the causes of anemia in babies, it is important to emphasize that infants are practically unable to replenish iron-containing protein.
During intrauterine development, the child’s body accumulates hemoglobin, which fully explains its high level at birth; it is more than enough in the first months of life.
However, later its level decreases sharply due to physiological factors.
If this indicator is below the permissible norm, this is most likely due to:
- lack of nutrition;
- congenital anemia;
- various neoplasms;
- bone marrow disease;
- blood loss;
- lack of vitamin B;
- childhood rickets.
If the indicator is significantly higher than normal, this may indicate a congenital heart defect in the child. Sometimes, if surgery is necessary, parents ask whether surgery can be done if there is low hemoglobin. Doctors usually recommend a recovery course if the procedure can be postponed.
The cause of anemia in adults is most often iron deficiency in the body. Perhaps this is due to:
- insufficient consumption of iron-containing foods;
- postoperative period;
- blood loss during menstruation or another nature;
- various types of diets;
- lack of vitamin B12;
- intestinal dysbiosis;
- various diseases, including blood diseases.
Symptoms
The main external manifestations of anemia:
- pallor;
- unhealthy tired look;
- weakness, drowsiness;
- fast fatiguability;
- poor appetite.
If hemoglobin is low, surgery is not performed, since intervention is stressful for the body, which will have complications.
Frequent symptoms are dizziness to the point of loss of consciousness, low blood pressure, depression, headaches, and rapid heartbeat. Cold hands and feet, susceptibility to viral and infectious diseases, as well as muscle pain, often indicate a deficiency of iron in the blood.
Anemia in children
Anemia is most often observed in children in the first years of life; at different stages of development it can be a rather dangerous disease. In a mild form, the disease is almost always observed in small-toothed children; in more severe cases, it requires immediate medical intervention. Therefore, it is important for parents to know what to do if their child has low hemoglobin.
Often the cause of anemia is explained by the intensive development and growth of the child. It is much more difficult for younger children to provide foods with the iron they need for health. Therefore, experts advise introducing complementary foods in a timely manner, feeding them with mixtures containing iron, amino acids and vitamin B12.
Anemia in children is classified into three groups
- Anemia due to major blood loss.
- Iron deficiency and hereditary anemia.
- Hemolytic anemia, the consequence of which is an increased process of blood destruction in comparison with the blood-forming process.
Anemia in pregnant women
What to do with low hemoglobin during pregnancy, and what causes the condition? In 9 cases out of 10, anemia in pregnant women occurs due to a lack of iron, which is fraught with complications during pregnancy and childbirth. If treatment is not started in time, the consequences of the disease can affect the fetus.
During pregnancy, the daily requirement of iron doubles; if the body does not receive it from food or vitamins, it uses up its own reserves.
During the period of bearing and feeding a child, a woman loses about 900 mg of accumulated iron; with a balanced diet, it is replenished within 3.5-5 years.
For this reason, during a second pregnancy earlier than this period, women experience iron deficiency.
Consequences of anemia
Depending on the degree of the disease, the consequences of anemia appear as follows:
- In children with mild anemia, pale and dry skin is observed, and hair becomes dull. In more severe forms, cracks appear on the palms and heels, academic performance decreases, and the child is easily susceptible to infectious and colds. Infants may experience frequent vomiting, anxiety, and poor appetite. Parents are required to know these symptoms and decide in time what to do if their child has low hemoglobin. The consequences of long-term anemia can be a lag in both mental and physical development, in addition, exacerbation of chronic diseases is highly likely.
- In pregnant women, the consequences of anemia can be difficult or premature birth, unfavorable pregnancy, inhibition of fetal development, gestosis, threat of miscarriage, inflammatory processes, congenital anemia in the child.
- In an adult, anemia is reflected in appearance and general well-being. The consequences of anemia manifest themselves in a depressed and depressed state, fatigue, and irritability. External signs include unnatural hair loss, dry skin, brittle nails, cracks in the corners of the mouth.
The effect of walking and regular nutrition on the body
Lack of a normal diet, unbalanced diet, quick snacks and frequent consumption of unhealthy foods lead to anemia. What to do if you have low hemoglobin? Eating foods high in iron from time to time will not improve the situation. It is important to eat properly and nutritiously every day.
Regular walking helps replenish the deficiency and saturate the body with oxygen.
You don’t have to go for a long and long walk; one evening walk every day after dinner or go a couple of stops before work and walk is enough.
After just a couple of weeks, the functioning of the cardiovascular system will noticeably improve, general well-being will normalize, and in addition, this is one of the best ways to prevent anemia.
Treatment with medications
Mild forms of anemia can be successfully treated with special diets that replenish iron deficiency; in case of serious illnesses, the doctor prescribes medication.
If a person is in the postoperative period or is waiting for intervention, then he is wondering whether it is possible to have surgery with low hemoglobin. Doctors usually recommend normalizing blood parameters, and only then proceeding with subsequent treatment.
The most widely used drugs are “Aktiferrin”, “Maltofer”, “Totema”, “Ferlatum”, “Heferol”, “Sorbifer”, “Ferumlek”. These medications are available in liquid form, tablets or injections.
You should not self-medicate, especially for pregnant women. Each individual drug and dosage are selected individually.
When taking a drug containing iron, the following points must be considered:
- as a rule, medications with a high iron content are taken in the late afternoon, before meals;
- Avoid simultaneous use of medications that interfere with iron absorption, for example, Levomycetin or Tetracycline;
- better absorption of iron is promoted by: ascorbic acid, B vitamins, sorbent, vitamin A and E;
- the course of treatment should last at least 1.5 months.
Foods that increase hemoglobin levels
What to do if you have low hemoglobin and can you increase it with food?
You can compensate for iron deficiency by adding foods high in this element to your daily diet:
- lean meat products: pork, lamb, beef liver, tongue, heart, chicken;
- seafood, including red fish and caviar;
- vegetables: beets, carrots;
- fruits: persimmons, apples, dried apricots, pomegranate;
- cereals and beans: buckwheat, bran, lentils, beans;
- berries: black currant, strawberry, blueberry, cherry, gooseberry;
- nuts: peanuts, pine nuts and walnuts.
Regular consumption of these products helps prevent anemia.
Diet and restrictions during treatment
Can I get vaccinated if I have low hemoglobin? Doctors say that it is undesirable (although this is not considered a contraindication), since vaccinations reduce immunity. First you need to cure anemia.
As a treatment for a patient with anemia, a special diet may be recommended to promote recovery and restore the normal level of the indicator.
The diet includes:
- Freshly squeezed juices from pomegranate, apples, carrots and beets with the addition of parsley or dill.
- Compotes and fruit drinks from dried fruits and berries.
- Salads from fresh vegetables, spinach with the addition of crushed nuts.
- Side dishes of steamed vegetables: cauliflower, potatoes, mushrooms.
- Buckwheat and millet porridge.
- The first and second courses of meat are irreplaceable with such a diet: beef, pork, turkey, rabbit and lamb.
- Beef and pork liver significantly saturate the body with iron.
One of the best recipes for raising hemoglobin is a mixture of dried fruits, honey and walnuts. For preparation you will need raisins, dried apricots, nuts and honey in equal proportions. The ingredients are ground through a meat grinder and poured with honey, the resulting mixture is eaten 1 tbsp. l., three times a day before meals.
During the diet, you should avoid or minimize the consumption of certain foods:
- strong coffee and tea, as they flush iron from the body;
- Dairy products and grains interfere with the normal absorption of iron, so they should be consumed at different times from iron-containing foods.
Vaccinations and surgeries for anemia
If the results of a general blood test do not correspond to the norm, then parents worry whether vaccinations are given if they have low hemoglobin. A mild degree of anemia is not a contraindication for vaccination; only a severe form of the disease can be a reason for a medical exemption from vaccination.
Is surgery performed for low hemoglobin? Before any operation, the patient must undergo tests, mainly to establish the level of all indicators in the blood and urine, as well as to determine the condition of the internal organs.
Surgery is a serious stress for the body; the recovery process, which partially depends on hemoglobin, is no less important.
If its level is below the permissible norm, the attending physician will decide to postpone the operation and prescribe iron-containing drugs.
Numerous practice proves that in people with reduced hemoglobin levels, the recovery process is slower, in addition, they are more often susceptible to postoperative complications. Patients with anemia during surgery are at greater risk of bleeding and tolerate anesthesia less well.
A hemoglobin level below 100 g/l is a contraindication for surgery; operations are possible only in emergency cases.
To avoid anemia, adults and children are advised to take preventive measures, spend more time in the fresh air, follow a diet, and eat only healthy foods. It is important to remember that disease is easier to prevent than to cure.
Source: https://FB.ru/article/411025/chto-delat-esli-nizkiy-gemoglobin-sposobyi-normalizatsii-produktyi-i-preparatyi-sovetyi
What changes after a blood transfusion procedure?
Blood transfusion is carried out as a method of restoring the patient’s health in a short period of time. But doctors always use this option as a last resort because such manipulation can have both positive and negative effects on the patient’s body.
Positive changes
The trend in improved transfusiology is to administer to the patient exactly the transfusion medium that is necessary for component therapy.
The injected red blood cell mass allows:
- increase blood volume by supplementing its elements;
- eliminate oxygen starvation;
- ensure normal supply of tissues and cells with oxygen;
- improve the functioning of the body as a whole.
In addition, after a transfusion, immunity is noticeably increased. The patient develops stable resistance to pathogenic microorganisms. The condition that caused the drop in hemoglobin after blood transfusion is easier to treat.
Negative changes
Blood transfusion has both positive and negative aspects. Very often, after a blood transfusion, certain complications develop. This procedure can cause irreparable harm to the patient's health. Therefore, only the doctor determines whether to administer blood elements to the patient or not. Possible consequences of transfusion are divided into three groups.
Jet
Complications manifest themselves as:
- Increased body temperature, up to fever.
- Bleeding resulting from large blood transfusions.
- Hemolytic shock, which develops when the blood of the patient and the donor sample are incompatible.
- Post-transfusion shock. The pathology develops as a result of transfusion of low-quality donor biomaterial.
- Anaphylactic shock to the injected biomaterial.
- Citrate shock. Usually the condition develops due to components of donor biomaterial.
Mechanical
Complications manifest themselves as:
- Rapid expansion of the heart due to intensive administration of red blood cells.
- Embolism that occurs during the penetration of air bubbles into the venous vessels during blood transfusion.
- Increased blood clotting, which increases the risk of blood clots that can clog blood vessels and disrupt the functional activity of internal organs.
Infectious
There are cases of infection during transfusion with blood-contact infections, such as: HIV, hepatitis, syphilis. This is possible due to non-compliance with established storage rules and control periods for donor material. The donor sample must be rechecked 5 months after its donation. But in unforeseen situations, donor blood is used without waiting for a second check. In such situations, a similar type of complication arises.
How to protect yourself from complications
The safe completion of blood transfusion is guaranteed only if all established safety standards that are provided for by this procedure are observed.
They are:
- In a careful reading of the anamnesis. The doctor must find out whether or not a blood transfusion has been performed in the patient's history. If there were surgical operations or childbirth, then the consequences appeared afterwards or not.
- Strict adherence to technique when determining blood group and Rh factor.
- Using the highest quality reagents and appropriate laboratory equipment.
- Carrying out all necessary compatibility tests.
- Monitoring the patient’s well-being until his complete rehabilitation.
According to statistics, the consequences that develop during blood transfusion more often arise due to the inattentive attitude of medical staff and non-compliance with the main rules during the procedure. The slightest mistake can take a person's life.
Indications for blood transfusion
Timely recommended and properly organized transfusion ensures the restoration of the cancer patient’s well-being and helps prevent the development of complications. Medical research has found that whole blood transfusions often activate the process of metastasis in aggressive forms of cancer. This condition reduces the body's resistance and aggravates the prognosis for recovery.
During oncological processes, only individual blood products are infused into patients. Determining the appropriate drug occurs in a particular case. The hemotransfusiologist takes into account the following factors:
- blood type;
- Rh factor;
- the duration of the oncological process and the severity of its course;
- patient's age;
- general well-being.
At stages 3-4 of the tumor process, the patient requires several transfusion procedures. At the initial stage of development of malignancy, one transfusion is sufficient to stabilize the patient. After the intervention, the dynamics of blood parameters are constantly monitored.
With precise selection of the required volumes and components, improvement in well-being is observed 2-3 days after the infusion. Patients note the elimination of weakness and restoration of appetite. The duration of improvement depends on the patient’s baseline indicators. In the later stages of the process, one should not expect long-term normalization of the condition.
It is known that to improve the condition of cancer patients, painkillers containing narcotic components are often used. Blood transfusion is a more acceptable method to eliminate pain due to chronic fatigue.
List of indications for manipulation:
- tumors of the gastrointestinal tract of malignant etiology;
- diseases of the female genital area;
- liver tumor.
The prolonged course of the oncological process provokes changes in important functions and leads to the development of anemia. When the bone marrow of the cross is affected, extensive operations are required, which are always accompanied by significant blood loss. The optimal method to ensure safe restoration of function is the infusion of donor blood products.
Anemia in premature babies
What is anemia in premature babies?
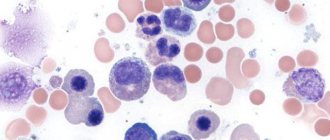
Anemia is a low level of red blood cells in the blood. Red blood cells are responsible for absorbing oxygen in the lungs and delivering it to other organs. A low level of red blood cells in the blood makes it difficult to transport it to other organs, and they do not receive enough oxygen. If anemia is severe, it can lead to serious health problems.
Anemia of prematurity occurs in premature infants. who were born earlier than expected.
Causes of anemia in premature babies
Infants are more prone to anemia because:
Red blood cell production temporarily slows down in all newborns immediately after birth (this is especially noticeable in premature babies); Blood production does not keep pace with the child's growth; Red blood cells have a shorter lifespan in children compared to adults.
Anemia of prematurity can be caused by one or more of the following problems:
Blood loss as a result of: Complications during childbirth; Blood sampling for testing (regular blood tests necessary to monitor the condition of premature babies); Decreased red blood cell production as a result of the following problems: Dietary problems; Some infections, such as rubella or parvovirus, that affect the bone marrow (the bone marrow makes red blood cells); Destruction of red blood cells can occur in the presence of the following diseases: Incompatibility of the blood of mother and child (Rh incompatibility); Hereditary diseases.
Family history of anemia; Complications during childbirth; Blood loss during childbirth; Diseases that require the heart to pump a large volume of blood; Twins with feto-fetal transfusion syndrome; Poor nutrition, especially low levels of iron, vitamin B6 or B12.
Pallor; Slowness; fast or difficult breathing; Difficulty during feeding; Slow weight gain; Periods during which breathing stops.
Diagnosis of anemia in premature infants
The doctor will ask about your child's symptoms and medical history and perform a physical examination. Blood tests will be needed to:
Count the number of red blood cells; Determine how quickly red blood cells are produced; Look for signs of red blood cell destruction; Measure the level of iron and vitamin B in the blood.
The diagnosis will be made based on a blood test. Test results can also help determine the cause of anemia.
Treatment of anemia in premature babies
Treatment will depend on the cause of the anemia. Mild anemia may not require treatment. The doctor will simply monitor the condition of the child’s blood. Blood tests may be necessary to monitor the child's overall health so that deterioration in health can be detected early.
Treatment options for anemia of prematurity include:
Optimizing nutrition for anemia in premature infants
Nutrition plays a big role in treating anemia. The right foods will help your baby's body produce more red blood cells.
Lack of certain nutrients can, on the contrary, hinder the production of red blood cells
Iron is an important component of red blood cells. A few weeks after birth, the baby may be prescribed iron supplements.
Erythropoietin in the treatment of anemia in premature infants
Erythropoietin is one of the hormones in the human body. It stimulates the production of red blood cells. Supplemental erythropoietin may be given to the infant to increase the body's production of red blood cells.
This procedure is often prescribed in addition to special nutrition.
Blood transfusion for anemia in premature infants
In severe cases of anemia, blood transfusions may be required. which will quickly increase the level of red blood cells in the baby’s blood.
Sometimes more than one blood transfusion may be needed.
To reduce the chance of anemia in a premature baby, do the following:
Provide your child with proper nutrition; Get proper prenatal care during pregnancy; Take steps to prevent preterm birth, including: Avoid alcohol, smoking, and drugs; Eat a healthy, balanced diet with plenty of fruits and vegetables; Keep chronic diseases under control.
At what hemoglobin levels can surgery be performed?
Surgery, no matter how simple or complex it may be, is a great stress for the body. Often, the effects of anesthesia or blood loss can have a negative impact on the patient’s well-being. When deciding whether to have surgery, the doctor checks the hemoglobin (Hb) in the blood. The level of the indicator affects the outcome and rehabilitation of the patient.
Hemoglobin: one of the most important elements
Hemoglobin is a specially structured protein that contains iron, which delivers oxygen to all tissues. Both low and high levels are harmful to the body. Its non-compliance with standards leads to:
- decrease in blood pressure;
- tachycardia;
- drowsiness/fatigue;
- anemia;
- changes in the taste of food;
- deterioration of hair/skin condition;
- liver enlargement;
- swelling of the legs.
Surgical intervention affects the decrease in the red blood cell count, which causes hemoglobin to drop. Therefore, test readings should be within or close to the norm of 110-150 g/l. The patient’s recovery process after a serious intervention is extremely important, which is possible with the healthy functioning of organs and systems.
Low Hb: yes or no surgery
When the hemoglobin level is normal, the recovery rate is faster and without aggravating consequences. Before placing the patient on the operating table, the doctor prescribes an examination to understand at what hemoglobin level it is safe to perform the operation. A complete blood count (CBC) is taken to determine the concentration of red blood cells and coagulability.
After surgery on the gastrointestinal tract, the process of absorption of substances worsens. Iron (Fe), vitamin B12, folic acid - are involved in hematopoiesis. Due to their slow absorption by the body, anemia will begin to develop. Therefore, one of the main methods of treatment has become the use of drugs containing these 3 substances.
Attention! If emergency surgery is necessary, on which life depends, then doctors prescribe a blood transfusion to eliminate low hemoglobin.
Before surgery, the specialist calculates the risk of bleeding, which occurs mainly due to damage to large vessels or insufficient pressure on them with clamps. Since this situation can be predicted, the patient is given a plasma transfusion.
At what hemoglobin level is surgery prohibited?
Keeping in mind the complications that are possible during the surgeon’s intervention and in the postoperative period, experts prohibit even simple operations if the patient has low Hb levels. Importance is attached to the rehabilitation period.
How the patient will recover depends on the level of hemoglobin, therefore, before surgical treatment, a series of diagnostic tests are prescribed to check the composition of the blood and urine. Examine the presence of pathologies in organs and systems.
Before surgery, any degree of anemia and other obstructive diseases must be treated.
If hemoglobin levels are 100 g/l or lower, surgery of any complexity is contraindicated. If the patient's Hb level is low, the doctor finds out the cause of this pathology. Then he applies methods to treat anemia. Prescribes a diet and medications containing Fe. In case of emergency surgery, reduced values are allowed, but the doctor still takes into account:
- the prevailing circumstances of emergency treatment;
- risk of blood loss;
- possibility of surgical treatment of anemia.
We must not forget that people with a hematocrit less than 28% risk complications or death in the first postoperative month due to increased wear and tear on the heart muscle.
How to increase hemoglobin
After an operation of any level of complexity, hemoglobin is greatly reduced - this leads to bad consequences (constant fatigue, decreased blood pressure, swelling in the legs, anemia, etc.).
In addition to unpleasant symptoms, a low concentration of red blood cells leads to a decrease in immune function, which increases the risk of complications even with a simple cold.
It is worth consulting with a specialist to promptly identify the problem and find a way to eliminate it.
The most common principles of Hb correction:
- Protein diet. Eating high-protein foods and vitamin-mineral complexes eliminates the lack of substances required for hematopoiesis. Allowed to eat: red meat, offal, seafood, eggs, dairy products. As well as raw fruit/vegetable salads and greens.
- Taking digestive enzymes that improve the permeability of nutrients.
- Treatment of other diseases of internal organs.
- Taking medications containing iron. Additionally, vitamin C is prescribed.
- 2-3 courses of intramuscular injections of vitamin B12.
- Hematogen.
- Folic acid and foods rich in it.
- In case of serious blood loss - blood transfusion. An extreme measure, it is carried out when there is a high risk of losing the patient’s life.
Low Hb is one of the reasons for the bad consequences of being on the operating table: fatigue, dizziness, even loss of consciousness. The cause of this pathology is often an unbalanced, low-quality diet or blood loss. In this case, bleeding can be hidden or obvious. It is important to check your hemoglobin annually to avoid the development of anemia and its complications.
Source: https://sosud-ok.ru/krov/lechenie-krov/pri-kakom-gemoglobine-mozhno-delat-operatsiyu.html
Correction of high white blood cell counts in cancer
The level of leukocytes in oncology increases in many types of leukemia, during which hormonal therapy is prescribed. Taking corticosteroids reduces symptoms and increases bone marrow reserve.
Hormone therapy for severe leukemia can suppress mitotic processes in the lesions, while providing additional resistance to the tumor.
Initially, treatment is carried out in small doses, but if the patient experiences negative dynamics, the administered doses are gradually increased. In severe stages of the disease, as well as in severe hemorrhagic syndrome, treatment is carried out with the maximum permissible doses of steroids.