What are tumor markers?
Let’s imagine a theoretical situation - the doctor gave a referral for tumor markers, now we won’t even find out which ones.
- What feelings does the patient experience after receiving such a referral and awaiting the result?
- What emotions will the number on the form cause if it is outside the norm?
- Horror, fear, despair. Do we need them?
How accurate are tumor markers and when should their level be determined? We will use data only from very serious sources: statistics from the World Health Organization and international recommendations developed by the National Academy of Clinical Biochemistry (NACB, USA) and the European Group for the Study of Tumor Markers (EGTM), of course, with adaptation to Russian reality.
Tumor markers are certain substances that are detected in biological fluids of the body (most often we are talking about blood serum); tumor markers can also be detected in extracts or paraffin blocks of tissue. An ideal marker should have two characteristics:
- sensitivity - that is, the percentage of positive results in people with a tumor;
- specificity - that is, the percentage of healthy people in whom the test gives a negative result.
Ideal would be 100% sensitivity and 100% specificity. In this case, the tumor marker must be characteristic of a specific type of tumor.
Unfortunately, such markers have not yet been discovered, so there is always room for error, both in the direction of a false diagnosis and in the direction of false peace of mind.
Reasons for an increase or decrease in the CYFRA 21-1 tumor marker
In diagnostics, there are two criteria by which we evaluate any study - sensitivity and specificity. Markers can be highly sensitive but low specific. This suggests that their increase may depend on a number of reasons completely unrelated to cancer.
For example, the ovarian cancer marker CA 125 can be elevated not only in tumors or inflammatory diseases of the ovaries, but, for example, in liver dysfunction, inflammatory diseases of the cervix and the uterus itself.
Often, with liver dysfunction, carcinoembryonic antigen (CEA) increases. Thus, the values of tumor markers depend on a number of processes, including inflammatory ones, that can occur in the body.
It happens that a slight increase in the tumor marker serves as the beginning for the start of a whole series of diagnostic procedures, up to such a harmless study as positron emission tomography (PET/CT), and as it turns out later, these procedures were not at all necessary for this patient.
The question of what causes the deviation from the norm of this marker interests many. In clinical practice, the tumor marker cyfra 21-1 is most often elevated due to the development of the diseases listed above.
In addition, the appearance of elevated values may be influenced by a common cold or the patient’s violations in preparation for this test. It is considered more dangerous if the patient underwent surgery to resection an organ affected by cancer and cyfra 21-1, a tumor marker of epithelial tissues, decreased to reference values, and after a short time the antigen levels suddenly began to increase again. This situation indicates the beginning of a relapse of the disease.
What tumor markers do we know?
The list of known tumor markers tends to infinity. Most of them are very specific and unknown to general practitioners. Most often, doctors who do not specialize in the management of patients with cancer are interested in the following.
- PSA (prostate-specific antigen) is an antigen characteristic of prostate tissue. Its level in the blood increases in both malignant and benign prostate diseases. In addition, the PSA level may be elevated after injury, palpation, mechanical irritation of the gland, or ejaculation on the eve of the test.
- CA125 is an antigen present in normal endometrial tissue. It enters the bloodstream only if natural barriers are damaged. Its blood level may double during menstruation and in cases of endometriosis. A significant increase in the level of CA125 occurs in ovarian cancer (in 80% of cases) and cancer of other organs of the female reproductive system, tumors of the breast and pancreas, rectum, stomach, lungs and liver. Among benign diseases, inflammatory diseases of the female reproductive system, hepatitis, cirrhosis and autoimmune diseases lead to an increase in the level of this marker.
- CA15-3 is an antigen most characteristic of tumor cells from the mammary gland; its level can also increase in malignant tumors of other locations (stomach, liver, pancreas and organs of the female reproductive system). In addition, its level increases in benign diseases of the mammary glands and in autoimmune processes.
- CA19-9 is an antigen that is produced by pancreatic carcinoma cells, less commonly by stomach tumors (the second most important marker of these tumors), liver and breast tumors. Among benign diseases, hepatitis and cirrhosis, cholecystitis and cystic fibrosis lead to an increase in its level.
- CA242 is a marker of malignant tumors of the gastrointestinal tract; it is mainly increased in tumors of the pancreas, intestines and stomach, but can also be increased in benign diseases of these organs.
- CEA (aka PEA - carcinoembryonic antigen) is found in some tissues of adults in very small quantities. During tumor processes, the concentration of CEA in the blood increases significantly. An increase in the concentration of this marker occurs in colorectal cancer, lung, breast or pancreatic cancer, metastases of malignant tumors to the liver, bone tissue, prostate and ovarian tumors. Moreover, an increase also occurs in benign diseases of the intestines, liver and lungs, especially in heavy smokers.
Now let's find out in what cases it is worth carrying out such an analysis.
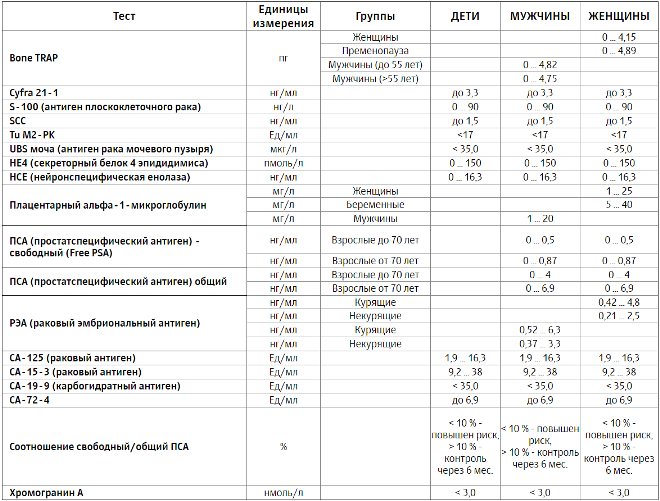
Norms of blood test parameters for tumor markers
The table shows the norms of the most commonly determined tumor markers. In different laboratories, depending on the research method and the accepted units of measurement, normal values may differ.
Norms of blood test parameters for tumor markers
| Index | Reference values |
| Alpha fetoprotein (AFP) | Men and non-pregnant women – up to 2.64 IU/ml pregnant women – 23.8–62.9 IU/ml (depending on the stage of pregnancy) |
| Carcinoembryonic antigen (CEA) | Men – up to 3.3 ng/ml non-smokers, up to 6.3 ng/ml smokers women – up to 2.5 ng/ml non-smokers, up to 4.8 ng/ml smokers |
| Ovarian tumor marker CA-125 | Up to 35 U/ml |
| Breast tumor marker CA 15-3 | Up to 32 U/ml |
| Pancreatic tumor marker CA 19-9 | Up to 37 U/ml |
| Prostate-specific antigen general | Up to 4 ng/ml |
| Human chorionic gonadotropin (hCG) common beta subunit | Men – up to 2.5 U/l Women – up to 5 U/l |
The most common tumors
Quite often people are afraid of cancer in general. But it’s impossible to be tested for all diseases, so let’s look at WHO statistics and find out which tumors claim the most lives among Russian residents.
Men
- Cancer of the trachea, bronchi and lungs - 27.8%
- Stomach tumors - 12.55%
- Colon and rectal cancer - 11.8%
- Prostate cancer - 7.7%
- Tumors of the mucous membranes of the mouth and oropharynx - 5.0%
- 35.3% accounted for deaths from all other types of tumors
Women
- Breast tumors - 17.8%
- Tumors of the rectum and colon - 16.5%
- Stomach tumors - 10.9%
- Cancer of the trachea, bronchi and lungs - 6.8%
- Pancreatic tumors - 5.9%
- 42.2% accounted for deaths from all other types of tumors
Now let's look at the possibilities of using tumor markers to identify and treat people with these tumors.
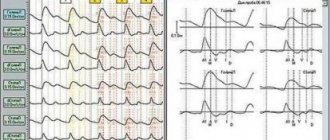
Cancer of the trachea, bronchi and lungs
Markers that can be used to determine prognosis for lung cancer are HSE, PEA and CYFRA21.1. NSE (neuron-specific enolase) is characteristic of only one type of this cancer, small cell. For other types of lung cancer, PEA and CYFRA21.1 are used. None of these markers can be used for diagnosis, since their specificity is very low (in other words, quite a lot of false positive results are detected with low sensitivity of the method). However, these markers are necessary to assess the results of treatment when comparing their levels before the start of therapy and during treatment. They can also be used after surgery to detect relapse.
Breast tumors
Breast tumors are the most common cause of death among all female deaths from cancer. A feature of these tumors is good treatment results in the early stages, so timely detection is very important. In breast cancer, CEA and CA15.3 are of greatest importance. It has been proven that in women who have undergone radical treatment, an increase in CA15.3 almost always indicates a relapse of the disease. The dynamics of the levels of this marker during treatment reflects the effectiveness of the chosen method of therapy. However, given the low specificity of CA15.3, its use for breast cancer screening is not recommended.
What are the main risk factors for developing cancer?
The main risk factors include working in hazardous industries, smoking, frequent (more than three times a week) and long-term consumption of alcohol, daily consumption of red meat, constant consumption of food that has been heat-treated, frozen and sold in ready-to-eat form.
Such foods are poor in fiber, vitamins and other substances necessary for humans, which can lead to an increased risk of, for example, breast cancer. Smoking is one of the most common and dangerous risk factors - it leads not only to lung cancer, but also to cancer of the esophagus, stomach, bladder, head and neck tumors: laryngeal cancer, cancer of the buccal mucosa, tongue cancer, etc.
For skin cancer and melanoma, as we already mentioned, the risk factor is sun exposure to the point of sunburn.
Long-term use of hormonal drugs, such as hormone replacement therapy, for more than 5 years and not under medical supervision, can lead to an increased risk of breast cancer and uterine cancer in women, so the use of such drugs should be carried out under the strict supervision of a mammologist and gynecologist.
As we mentioned above, viruses can also be a risk factor, including oncogenic types of the HPV virus, which lead to genital cancer and oral cancer. Some non-carcinogenic viruses may also be risk factors.
For example, hepatitis B and C viruses: they do not directly cause liver cancer, but lead to the chronic inflammatory disease of the liver - hepatitis, and after 15 years, a patient with chronic hepatitis B and C may develop hepatocellular cancer.
No not always. The number of tumor markers contained in the blood may increase slightly with the development of cysts, benign tumors, infectious or inflammatory diseases, and even after a common cold.
Tumors of the rectum and colon
If colorectal cancer is detected at an early stage, the five-year survival rate after treatment reaches 90%, this is a very good indicator in oncology. The most common marker of this type of tumor is CEA. However, here too in the expert recommendations we see a picture similar to the previous ones. The dynamics of CEA can be used to identify progression after treatment; this marker is especially important for identifying progression after removal of metastases from the liver. But its definition is not used to screen for colorectal cancer.
Prostate tumors
In Russia, PSA determination is used to screen for prostate cancer during the annual clinical examination of men over 50 years of age. In the USA and European countries, it is also recommended to determine this marker for all men over 50 years old, and with a family history - from 40–45 years old. However, when relying on the test results, there are several interesting facts about this marker to consider.
- PSA is informative only in combination with a digital rectal examination.
- When donating blood for analysis, appropriate preparation is required.
- When assessing the result, it is necessary to use age norms.
- Men over 75 years of age are not prescribed such screening, since treatment of non-clinical forms of prostate cancer only worsens the prognosis for life.
- Research data published in 2011 confirmed that early detection of prostate cancer through screening had no effect on specific life expectancy in the long term.
Therefore, even such a specific and familiar marker as PSA loses its position in early diagnosis.
Decoding the results
An increased level of the HE4 tumor marker can also be observed in other cancers. This fact must be taken into account when deciphering the results. A relatively high concentration of marker protein can indicate lung cancer, kidney failure, kidney fibrosis (a chronic inflammatory process that leads to excessive growth of the connective tissue of the kidneys, which leads to the appearance of scars).
A reliable examination result can be obtained regardless of the phase of the patient’s menstrual cycle.
How long to expect results
The results of the analysis can be obtained within two days from the date of its delivery. This is very important, especially for timely detection of a tumor and prompt consultation with a doctor if cancer is suspected. The study is almost irreplaceable when the disease is asymptomatic. It makes it possible to cure the patient and improves the prognosis of recovery.
Marker standards
HE 4, like any tumor marker, has a range of values that correspond to the norm. The norm for women depends on age. Thus, for patients under 40 years of age, the reference value of glycoprotein is no more than 60 picomoles/liter; from 40 to 49 years – the indicator should be no more than 76 picomoles/liter; from 50 to 59 years – no more than 74 picomoles/liter; from 60 to 69 years – up to 83 picomoles/liter; from 70 years – no more than 104 picomoles/liter.
Increased values
The reasons for increased indicators may be:
- ovarian cancer (this occurs in 9 cases out of 10);
- breast oncology;
- cancer of the endometrium (inner mucous membrane) of the uterus;
- lung cancer (extremely unlikely).
The gene responsible for the production of ovarian tumor markers is often found in mutated cells. Therefore, an increased level of such proteins in the body with a high degree of probability may indicate the presence of cancerous tumors.
The most common symptoms of ovarian cancer:
- “false” urge to urinate, a feeling that the bladder is not completely emptied. Such symptoms are due to the fact that the tumor puts pressure on the bladder;
- irregular menstrual cycle;
- vaginal discharge containing blood;
- digestive disorders such as bloating, constipation, loss of appetite;
- the presence of pain during sexual intercourse;
- pain in the abdominal area (stomach);
- general weakness, lethargy, drowsiness;
- reduced level of performance;
- the appearance of mental disorders such as neuroses and depression.
The ovary may stop functioning completely in the later stages of the disease. In this case, any treatment methods will be ineffective.
If the tumor marker concentration is elevated, an urgent visit to an oncologist is necessary. The doctor will prescribe additional examinations and select a treatment regimen. Possible treatments include either chemotherapy or surgery to remove the cancer. The results of the course of treatment can be judged only a month after its start. In accordance with the data obtained, the doctor can timely adjust the plan for treatment procedures.
A favorable outcome is considered to be the absence of metastases and the return of test results to a level corresponding to standard indicators. If the values are still elevated, a change in the patient's treatment plan is necessary.
Low performance
Reduced tumor marker values are a variant of the norm. They can confirm the woman's health. However, for some forms of oncology, the described analysis will not be informative. These are the following types of cancer.
- Germinogenic. It appears in those cells that were formed during the girl’s intrauterine development. This disease can appear at almost any age. This is a fairly rare type of tumor. Surgery and chemotherapy are effective and lead to complete recovery of the patient.
- Mucoid. This type of malignant neoplasm affects the mammary glands. This tumor occurs with a frequency of 2 to 5% of the total number of breast cancers. When the disease is detected at the second stage, the mortality rate is no more than 5%; at the third stage, death is expected in 23% of cases. This once again speaks to the importance of timely diagnosis.

The HE4 tumor marker remains normal in the described forms of cancer. To exclude an oncological diagnosis, it is necessary to calculate the ROMA 2 index. Patients are often recommended to undergo an ultrasound examination, undergo additional tests, and use alternative diagnostic methods.
When the analysis is wrong
Tumor markers such as HE 4 are not absolute indicators of cancer. It is possible to obtain false positive results in the following cases:
- in the presence of cystic fibrosis - a hereditary genetic disease characterized by severe malfunctions of the respiratory system;
- for infections of the genitourinary system;
- with kidney or liver failure;
- in the presence of cysts (benign tumors filled with fluid);
- if fibroids are present, they are benign tumors of the uterus.
If there is a suspicion of cancer, but the test does not confirm its presence, the test must be taken again after a month.
Tumors of the female reproductive system
Tumors of the female reproductive system account for approximately 10% of deaths from malignant tumors. They were not included in our initial list, since in WHO statistics they are divided by tumors of individual organs (tumors of the endometrium, cervix, ovaries, etc.).
Among them, ovarian cancer claims the most lives among women. For differential diagnosis between benign and malignant processes when identifying pathological formations in the pelvis, CA125 can be used. This marker is used for further monitoring of treated patients, and its levels are used over time to assess the effectiveness of therapy. The CA125 test is not recommended by experts for screening women without any complaints. However, this study should be performed every 6 months in conjunction with pelvic ultrasound in women with a high hereditary predisposition - in the presence of mutations in the BRCA1 and BRCA2 genes.
Popular types of cancer
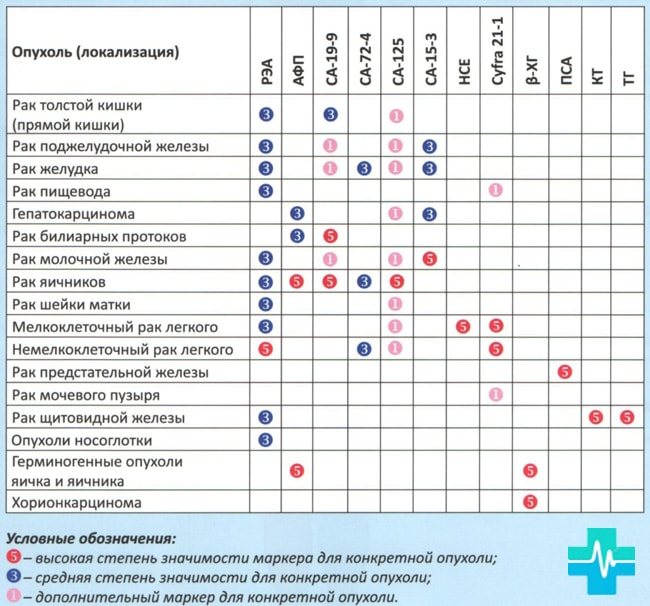
Markers have properties that differ for different reasons. The main one is highly sensitive and specific. But there are also secondary species. They are used together with the main ones and together give a result that is more accurate. Additional is used to determine relapse.
This substance is divided according to its origin:
- receptors;
- hormones;
- enzymes;
- oncofetal.
Oncofetal indicators usually include a larger number of oncological indicators. Such structures are found in huge quantities only in embryonic tissue; they play a very important role in the formation of a child.
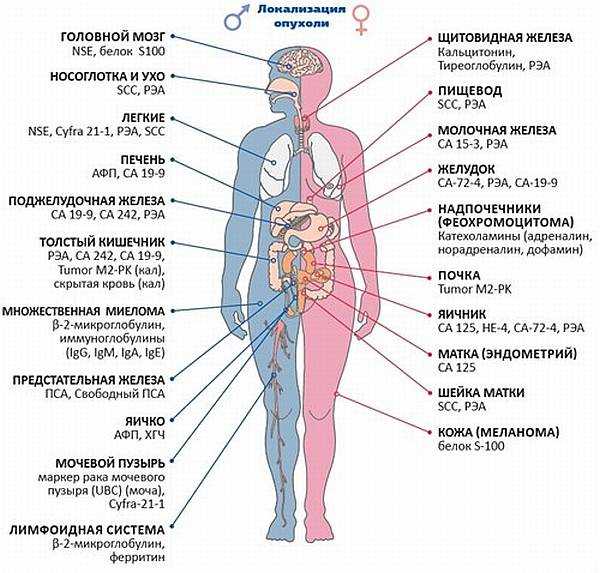
There are also tumor markers that help find the location of the tumor.
- Chest – CA15-3, CEA.
- Testicles – VHCG, AFP.
- Ovaries – CA125, CA19-9.
- Uterus – CA 19-9, CA 125.
- Liver –AFP.
- Intestines – CA 19-9, CA 125.
- Leather – S 100.
- Prostate gland – PSA.
- Bladder – TPA, Cyfra 21-1.
- Pancreas – CA 19-9, CA 72-4.
Some of the indicators may exceed the norm. But it is difficult to accurately determine the presence of cancer from them. For example, CEA is produced in the tissue of the embryo, and is present in small quantities in an adult; it is this substance that is sensitive to a large number of oncologies.
Usually, when taking tests, the doctor prescribes several tumor markers at once. The fact is that several antigen indicators can indicate one disease at once, just as one marker can be isolated from cancerous tissues of different organs.
- The main one is a tumor marker, which is highly sensitive and can detect a tumor in the early stages, but can belong to different tissues.
- Secondary - a marker with low sensitivity, but a narrower specialization. Usually, several secondary markers are used at once along with the main one for more accurate results.
Mainly used are oncofetal tumor markers or proteins that are mostly found in the tissues of the embryo. They are necessary for the normal construction of internal organs and the growth of the child in the womb. An adult should have less of these proteins.
| Tumor location | Onomarkers |
| Brain | NSE, protein S100 |
| Nasopharynx and ear | SCC,REA |
| Lungs | NSE, CYFRA 21-1, REA, SCC |
| Liver | WUA, CF 19-9 |
| Pancreas | Tumor marker CA 19-9, CA242, CEA |
| Colon | REA, SA 242, SA 19-9, Tumor M2-PK |
| Multiple myeloma | B-2 Microglobulin, Immunoglobulins (igG, igM, igA, igE) |
| Prostate | PSA, Free PSA |
| Testicle in men | Tumor marker AFP (AFP), tumor marker hCG, CA 125 |
| Bladder | Bladder Cancer Marker - UBC, Cyfra 21-1 |
| Lymphoid system | B-2 microglobulin, firritin |
| Thyroid | Calcitonin, Thyroglobulin, CEA |
| Esophagus | SCC, REA |
| Breast | SA 15-3, REA |
| Stomach | Antigen Ca-72-4, REA, CA-19-9 |
| Adrenal glands (Pheochromocytoma) | Catecholamines (adrenaline, norepinephrine, dopamine) |
| Bud | Tumor M2-PK |
| Ovaries in women | SA 125, NE-4, SA 72-4, REA |
| Uterus (Endometrium) | CA 125 |
| Cervix | SCC, REA |
| Skin (Melanoma) | Protein S-100 |
| Gallbladder | SA 19-9 |
| Name | Most specific marker | Other markers | Purpose of the study | Use for early stage/screening diagnostics | The need for additional diagnostic methods |
| Bladder cancer | BTA, NMP22 | CEA, CA 125, CA 19 9 | Monitoring treatment, detecting relapses | No | (cystoscopy, biopsy, cytological examination of urine) |
| Breast cancer | CA15 3, CEA | CA 27.29 | Treatment control | No | (mammography, tomography, biopsy) |
| Rectal cancer | SEA, SA 19 9 | — | Monitoring treatment, detecting relapses, assessing prognosis | No | (colonoscopy, sigmoidoscopy, feces for occult blood) |
| Liver cancer | AFP | — | Diagnostics, treatment control | No Yes | (biopsy, ultrasound, tomography) |
| Lungs' cancer | CEA, NSE | TPA | Monitoring treatment, detecting relapses | No | (X-ray studies, tomography) |
| Melanoma | TA 90, SU 100 | — | Metastasis, progression | No | (biopsy) |
| Ovarian cancer | CA 125 | SA 72-4, LASA-P, AFP | Monitoring treatment, detecting relapses | No/screening for high-risk groups | (ultrasound, biopsy) |
| Pancreas cancer | SA 19 9 | PAP, PSMA | Monitoring treatment, detecting relapses | No | (ultrasound, tomography) |
In 2/3 of patients, AFP alpha-fetoprotein often increases, which is a tumor marker of liver cancer and increases as the tumor process grows. In addition, this liver tumor marker increases in acute and chronic hepatitis, and sometimes in ovarian or testicular cancer, but this category of patients accounts for no more than 5%.
With the development of multiple myeloma or lymphomas, beta - 2 - microglobulin is determined and it is this tumor marker that is prognostic for survival.
The presence of CA 15 3 and CA 27.29 indicates breast cancer, but at the initial stage of the disease they exceed the norm slightly. As it progresses, the rate increases.
CA 125 indicates ovarian cancer and is elevated in most patients; it is this tumor marker of ovarian cancer that allows a preliminary diagnosis to be made at the stage of medical examination. But it can also be elevated in other gynecological diseases or lung cancer, as well as in cancer survivors.
CA 19 9 is characteristic of damage to the pancreas, as well as with the effectiveness of treatment. This marker may increase in cases of intestinal or bile duct cancer.
Depending on their importance for the diagnosis of tumors, the following types of tumor markers are distinguished: primary, secondary and additional. For example, to detect ovarian cancer, CA 125 is the main tumor marker, HE4 is the secondary antigen, and the concentration of AFP and CEA is additionally examined.
Tumor markers are distinguished by origin:
- Immunological - tumor antibodies (cancer antigen) These include markers CA 125, CA 72-4 and CA 19-9.
- Hormones. In the diagnosis of malignant neoplasms, determination of the levels of ACTH, hCG, TSH, thyroglobulin and thyrocalcitonin is used.
- Enzymes – acid phosphatase and lactate dehydrogenase (LDH).
- Metabolic products: creatinine, free DNA, hydroxyproline and polyamines.
- Blood plasma proteins: ferritin, ceruloplasmin and β2-microglobulin, as well as protein products of tumor cell breakdown.
- Receptors - estrogen and progesterone.
In connection with the association with organs, tumor markers are identified:
- for mammary glands – CA15-3, Cyfra 21-1, CEA;
- for ovaries - CEA, CA125, AFP, CA 19-9 and BHCG;
- for the uterus - SCC, Cyfra 21-1, CA 19-9, CEA, CA 19-9, CA 125;
- for the prostate gland – PSA and FPSA;
- for testes – BHCG and AFP;
- for the large intestine and rectum - CEA, CA 125 and CA 19-9;
- for the pancreas - CEA, CA 72-4 and CA 19-9;
- for the liver – AFP and CEA;
- for stomach CA 72-4, CEA and CA 19-9;
- for the esophagus - CEA and Cyfra 21-1;
- for the thyroid gland – CEA and NSE;
- for lungs - NSE, CEA, CYFRA 21-1, CA 125 and CA 19-9;
- for the bladder – TPA, CEA and Cyfra 21-1;
- for leather – S 100.
What tumor markers should women take? If we are talking about the pathology of the reproductive organs, then women are recommended to determine tumor markers that are associated with the uterus, ovaries and mammary gland. When it comes to identifying diseases of other organs, the list of recommended tests does not depend on gender.
Based on the location of detection, the following tumor markers are identified:
- humoral - their level is determined in the blood, urine and cerebrospinal fluid;
- tissue - determined by histochemical research methods directly in the tumor tissue.
Based on their chemical structure, the following tumor markers are distinguished:
- carbohydrate determinants of glycoproteins;
- glycoproteins;
- saccharides;
- polypeptides;
- glycolipids;
- immunoglobulins;
- polyamines.
To date, experts know about 200 compounds. However, in practice, about 20 are used for research. This is because most of them do not have sufficient specificity.
Do I need to take tumor markers? The answer is clear: yes. An increased level of tumor marker is a guide to action - a malignant neoplasm must be excluded. If cancer is detected at a preclinical stage, then treatment will be more successful, and the prognosis for life and recovery will be more favorable.
The value of determining the level of tumor markers depends on the degree of its association with a certain histological type of tissue and organ. Thus, calcitonin can detect medullary thyroid cancer, PSA/PAP indicates prostate cancer, and NSE is found in small cell lung cancer.
The following tumor markers have relatively high organ specificity:
- CA 125 in case of ovarian cancer;
- CA 15-3 for breast cancer;
- CA 19-9 in pancreatic cancer.
Tissue organ-specific antigen (TPA) and carcinoembryonic antigen (CEA) do not have organ specificity. Their level will be elevated in case of malignant neoplasm of any organ. Cardiofetal antigens are classified into a separate group.
When determining cancer, the main thing is to decipher the results of the tests. In 2/3 of patients, an increase in AFP alpha-fetoprotein is observed, which indicates the presence of liver cancer. The indicator begins to increase as the tumor develops.
When the analysis for tumor markers is deciphered, if lymphoma and myeloma are observed, beta-2 microglobulin increases. The presence of CA27-29 and CA 15-3 indicates breast cancer, but in the first stage of such oncology, its excess of the norm is minimal. Indicators begin to increase as the disease progresses.
Speaking about what the CA 125 marker is, it indicates the presence of ovarian cancer; it is this analysis that makes it possible to determine the disease at the examination stage, making a preliminary diagnosis. However, its increase is possible if a woman has another gynecological disease or lung cancer.
When are tumor markers really needed?
Determination of most tumor markers is important and should be used in the presence of clinical manifestations of a tumor and its instrumental confirmation for differential diagnosis or monitoring the effectiveness of therapy.
Testing for tumor markers should not be used as a screening test. However, this does not mean that the marker does not contribute to the early detection of tumors, but only that such an examination does not improve the prognosis of the average group of people. However, no one can say how it will affect the life of a particular person.
It is extremely important that any examination is prescribed by a doctor who has sufficient knowledge and can interpret the test result for the benefit of the patient. This will help not only maintain health, but also avoid stressful situations and unnecessary material expenses.
Features of the analysis
The patient usually has to be tested for tumor markers several times: this is not a single procedure, but a series of tests that are prescribed when the presence of a tumor is suspected and allow one to make a prognosis regarding its development.
The test is necessarily preceded by preparation, since there are a number of factors that can cause a slight increase in tumor markers even in a healthy person, which significantly complicates the diagnosis.
Preparing for the study is quite simple. Three days before the procedure, the patient must stop drinking alcohol, as well as fatty and spicy foods and any “heavy” dishes.
A blood test for tumor markers is always taken from a vein, the procedure must be carried out on an empty stomach, so the last meal should be no later than 8 hours before it starts.
Immediately before the study, smoking is prohibited, as this may affect the results.
READ Factors that cause lymphocytes to be elevated in the blood
The optimal time to donate blood is considered to be the morning (between 7 and 11 a.m.), since at this time tumor markers can be studied in as much detail as possible.
Video:
A few days before the examination, it is advisable to stop taking any medications, but if this is not possible, then you must notify the doctor about this.
It is also necessary to warn the doctor about previous examinations that the patient underwent during the week before the examination. This is especially important if MRI, ultrasound, or CT were performed, as they can significantly distort the results.
Patients donating blood for PSA (tumor markers of the prostate gland) should abstain from sexual intercourse a week before the test, as well as from any procedures that include effects on this organ: massage, transurethral ultrasound, digital examination, etc.
During the procedure, the patient must be calm, so it is worth coming to the test in advance to sit for a while and normalize the nervous system. It is better to avoid physical activity 3 days before the procedure.
Since there are usually several tests for tumor markers, it is better to do them all in one laboratory - this way you can get the most adequate results.
Proper preparation is very important for this type of research, as it directly affects its accuracy.
The process of donating blood is no different from a regular test: the doctor takes material from a vein, and the result is usually ready within a few hours.