Endarterectomy - what is it?
Endarterectomy is a reconstructive type of surgery that is widely used to correct the consequences of atherosclerosis. Its main goal is to free the lumen of the arteries from fatty deposits that impede blood flow. Blood supply is restored to those areas of the vascular bed that were involved in the pathological process.
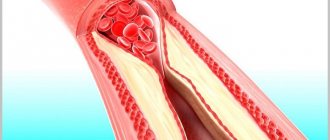
The endothelial lining of blood vessels is normally smooth and even. With the development of atherosclerosis, cholesterol deposits form on the inner lining. As the disease progresses, fatty growths accumulate calcium salts. This helps to increase their size. There is a narrowing of the lumen of the arteries that supply blood to vital organs, which begin to lack oxygen.
In case of extensive damage to the vascular network, in order to avoid ischemia of organ structures, patients are advised to undergo reconstructive surgery. Most often, intervention is performed on the carotid arteries, as well as on the afferent vessels of the lower extremities. Like any operation, endarterectomy has clear indications :
- the lumen of the vascular bed is stenotic by 70% or more;
- there is a history of cerebrovascular accident (the operation is performed to avoid a recurrent stroke in the long term);
- according to instrumental studies, fat deposits are formed according to the type of blood clots;
- layers of lipids are present on the walls of both carotid arteries;
- soft tissue ischemia of the lower extremities was diagnosed.
In addition to these cases, endarterectomy is performed in the absence of the desired effect from conservative therapy. Surgical correction of atherosclerosis is possible when the patient has no contraindications to surgery. These include: the patient’s advanced age, chronic diseases of vital organs in the stage of decompensation, “fresh” myocardial infarction, hemostasis disorders of various origins, neoplastic processes of any localization).
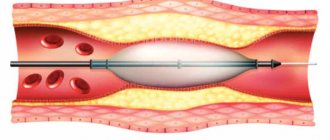
The method of performing the operation depends on its type. With the direct method, the incision begins after the patient is under general anesthesia. After isolating the artery, its wall is cut, and the fatty growth is separated from the endothelium by blunt means. Where the integrity of the vessel has been compromised, angioplasty is performed with a patch made of synthetic material.
The eversion method involves making a transverse incision of the damaged vessel. To get rid of fatty plaques, surgeons use special instruments to turn a section of the vascular bed inside out. Complete excision of the affected area is performed in cases of severe atherosclerosis. A prosthesis made of synthetic material is sewn into place in place of the removed portion of the vessel.
Endarterectomy for obliterating atherosclerosis of the vessels of the lower extremities
Obliterating atherosclerosis of the vessels of the lower extremities is a chronic disease caused by atherosclerotic damage to the vessels involved in the blood supply to the lower extremities. As a result of blockage or narrowing of the vessel, tissue ischemia occurs, accompanied by pain, ulcers form and such a serious complication as gangrene of the lower extremities.
Considering that atherosclerosis is a generalized disease, almost 30% of patients have combined damage to the vessels of the lower extremities and the carotid arteries.
With such a combination of lesions, the question always arises: which vessels to operate on first?
According to current recommendations, if a patient with severe narrowing of the carotid arteries (narrowing more than 70%) has suffered a transient ischemic attack or stroke within the previous 6 months, and he has obliterating atherosclerosis of the vessels of the lower extremities, then surgery on the carotid arteries should be performed before surgery on the carotid arteries. vessels of the lower extremities.
In some cases, the issue of simultaneous surgical correction of changes in two arteries is considered.
In any case, the question of how to remove plaques from vessels with combined damage to the carotid arteries and arteries of the lower extremities is decided only by a surgeon.
Along with the operation of iliofemoral bypass, endarterectomy is used for obliterating atherosclerosis of the legs. It is carried out in a direct, eversion and open way. Surgeons make a choice in favor of one method or another based on the results of examination of patients.
When a patient comes to the therapist with the above complaints, or during tests it turns out that the cholesterol level is significantly higher than normal, a more detailed examination of the blood vessels is required. It includes:
- analysis to determine the lipid profile and blood clotting indicators;
- magnetic resonance angiography;
- computed angiography;
- duplex ultrasound scanning.
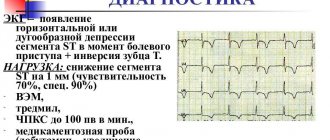
All of the listed diagnostic methods are used only immediately before carotid endarterectomy (plus ECG, EEG, general urine and blood analysis). In other cases, one of the studies is selected. If it turns out that cholesterol plaques have affected the carotid artery, an additional computed tomography scan of the head is performed, which makes it possible to find out how badly the plaque has clogged the carotid artery. If the lumen is narrowed by more than two-thirds, carotid endarterectomy is prescribed.
The operation also has contraindications. These include recent stroke, carotid artery dissection, severe brain disease, plaque mobility, unstable angina, advanced hypertension. The last three contraindications are considered relative, because when the patient’s condition is stabilized, endarterectomy is still performed.
Carotid endarterectomy – removal of atherosclerotic plaques in the carotid artery
The essence of carotid endarterectomy is to restore the patency of the carotid arteries by removing fatty deposits from their lumen. The main goal of this surgical intervention is to restore blood supply to the brain. The most common methods of performing endarterectomy of the carotid arteries are direct and eversion. The surgical technique depends on the severity of endothelial dysfunction in the damaged area of the vascular bed.
Stages of the operation
This kind of intervention is usually carried out under general anesthesia . This is due to the fact that local anesthesia is usually used due to the low number of postoperative complications, as well as the extremely short rehabilitation period. Also, a conscious patient can monitor the operating process and regulate the state of blood flow in the brain.
- In connection with the prevention of infectious complications, the patient's neck is shaved before surgery.
- After administering anesthesia, the surgeon makes a small longitudinal incision on one side of the neck. This is how the carotid artery is detected.
- The specialist clamps the detected carotid artery and stops the blood flow passing through it. During this period of time, blood will flow into the brain from another carotid artery, located on the opposite side of the patient’s neck.
- If the carotid artery is detected and compressed at the site of narrowing, the doctor makes another incision.
- Next, the specialist removes the patient’s atheromatous plaques by scraping the inner wall of the carotid artery.
- After this stage of the operation, the incision on the artery is sutured, and blood flow is restored. A patch can be placed at the site of the incision; it is made from tissue taken from the patient’s vein; it is taken from the leg.
- When completing the operation, the surgeon sutures the wound formed on the neck, then applying a bandage to it. The operation time is 2 hours .
Risks and possible complications of carotid endarterectomy
Complications of this surgical intervention most often include intraoperative bleeding. Damage to cranial nerves can sometimes occur. Because of this, paresis of the branches of the hypoglossal or vagus nerves occurs. Sometimes plaque rupture is possible, which can cause cerebrovascular accident in the patient.
Due to the fact that the operation to remove plaques from the carotid vessels is performed in an open manner, wound complications are possible. They occur when pathogenic microorganisms enter the wound and actively multiply. To avoid this, surgeons prescribe a course of antibiotic therapy to their patients. The drugs are taken at the stage of preparation for the intervention or after it.
Prevention of complications
Sometimes, as with any surgical intervention, the following complications may occur:
- infectious complications of a postoperative wound;
- recurrence of thrombosis after surgery;
- destruction of the blood clot and its migration to the heart, pulmonary artery or other vessels;
- bleeding from the wound early or late after surgery.
Major complications of surgery include stroke, re-formation of plaque (restenosis), myocardial infarction, damage to the nerves of the larynx with difficulty swallowing and paralysis of the vocal cords. Other negative consequences associated with anesthesia and surgical procedures are also possible. The risk of postoperative strokes increases significantly in smokers, patients with a previous stroke, diabetes mellitus or hypertension, with difficult-to-reach localization of vascular plaques, with a significant decrease in the lumen of the paired vessel on the other side.
For some patients, the operation may result in blood poisoning.
- collapse;
- attack of arterial hypertension;
- subcutaneous hematoma in the area of the surgical field;
- sepsis;
- stroke;
- nerve damage.
These conditions develop acutely and require immediate care in the intensive care unit. Therefore, after carotid endarterectomy, the patient remains in the hospital for at least 3 days. The appearance of such signs may be associated with the hemodynamic characteristics of the patient’s body, a stress reaction to surgery, or disturbances during the intervention.
To prevent negative consequences, you need to adhere to certain rules. It is important to take all medications prescribed by your doctor, as they are necessary to restore normal hemodynamics. If carotid endarterectomy of the carotid arteries was performed on the right, you can lie on the left side, when on the left - on the right, so as not to put pressure on the affected area. If you experience fever, chills, dizziness or other negative sensations, you should immediately consult a doctor.
Recovery and life in the postoperative period
Usually the duration of the operation does not exceed 3 hours. After emerging from drug-induced sleep, the patient is transported to the recovery room. The duration of inpatient treatment ranges from 5 to 10 days.
After surgical treatment, patients are prescribed a list of medications. Typically these are antithrombotic and lipid-lowering agents. If you have arterial hypertension, the doctor will describe in detail the regimen of medications that should be taken continuously for a long time. All medications are taken under the supervision of a doctor!
7 days after the intervention, postoperative sutures are removed. The recovery period should proceed without active physical and emotional stress. Patients are advised to adhere to a proper diet, which excludes foods rich in cholesterol. You should definitely take time for walks in the fresh air. 4 weeks after removal of the sutures, the patient should visit the surgeon so that he can assess how the postoperative period is progressing and give further recommendations.
How is cholesterol plaque formed?
Everyone has heard about cholesterol at some point, but not everyone fully understands the seriousness of controlling this indicator. Moreover, slender people are most often mistaken. They are sure that cholesterol means excess weight, i.e. fat, and they are in no danger. But in fact, cholesterol plaques are not cellulite or a double chin at all, but small organic inclusions that form in the blood vessels. They clog the lumen, preventing blood from circulating normally.
The formation of a cholesterol plaque in a vessel begins with damage to its inner layer. The endothelium weakens as a result of a person’s poor nutrition, frequent increases in blood pressure (hypertension), as well as bad habits - smoking and alcohol abuse. Cholesterol is deposited in the pores of the injured wall, which gradually layers and forms into a whole plaque.
Attention! Blood cholesterol levels should be tested at least once a year. Today it is not difficult: there are even compact devices with which you can do rapid tests at home.
Cholesterol may not bother a person until he is 30 years old, while the body is still coping with current problems. After 30 (in some cases earlier), shortness of breath begins, hypertension develops, and memory deteriorates. Depending on which artery is blocked by plaque, various systems and organs suffer.
The most dangerous thing is when cholesterol accumulates in the carotid (carotid) artery, causing a deterioration in blood supply to the brain. This is the development of ischemia and the risk of strokes and micro-strokes. The first sign is ischemic attacks, which are manifested by tingling in the limbs, a sharp deterioration in vision and slurred speech. A person is immersed in this state for several minutes. It indicates a lack of brain nutrition and requires consultation with a doctor.