The muscle that controls the rate of contraction of the heart is called the myocardium. And when physicochemical and biochemical processes are disrupted in it, this means that dystrophic changes occur in the myocardium.
Important! If you detect such changes at an early stage of your development, they can be avoided.
Myocardial damage of any nature is manifested primarily by modifications of myocytes. Dystrophy accompanies all major cardiac pathologies, for example:
- ischemic disease;
- vices;
- inflammatory processes.
It is this that is the basis of heart failure, which occurs in heart diseases. Diffuse dystrophic changes in the myocardium begin their development gradually; the cause of this may be insufficient nutrition of the muscle layer.
Signs of myocardial dystrophy can be different and are determined by the type of underlying disease, its duration and prevalence.
over a long period of time, the disease may not particularly manifest itself, but there have been cases when athletes die during acute physical overexertion. It is found that due to excess calcium ions, contracture of cardiomyocytes develops. Sometimes pathology is detected not by symptoms, but by functional studies. The most common symptoms are pain in the left chest (cardialgia), conduction and heart rhythm disturbances, as well as heart failure.
The unpleasant sensations that arise can be aching or stabbing, and often have no connection with physical activity. However, this does not mean that pain cannot intensify after overstrain of a psychological or physical nature. A decrease in the ability of the heart muscle to contract is manifested by tachycardia, excessive fatigue and weakness. When dystrophic changes in the left ventricular myocardium worsen, heart failure is complicated by stagnation in the pulmonary and systemic circulation. In addition, non-inflammatory fluid may accumulate in the pleural or abdominal area, and passive movement in the joints is limited.
Types and causes of pathological processes of the myocardium
Dystrophic processes occurring in the middle layer of the heart muscle can be classified according to etiology. They can occur when:
- acute and chronic anemia;
- vitamin deficiency, nutritional disorders;
- endocrine metabolic disorders;
- endogenous and exogenous intoxication;
- diseases of the neuromuscular system;
- extreme physical stress;
- pregnancy;
- kidney damage, electrolyte disturbances.
Moderate dystrophic changes in their course can be acute and chronic. In special cases, the outcome may be myodystrophic cardiosclerosis. The pathological process can spread in a diffuse or focal manner. Most often, diffuse changes develop with inflammation of the muscle layer and the formation of connective tissue that replaces its fibers. Interesting! During the studies, uniform damage is detected in such areas as the atrium, interventricular septum and ventricles.
Changes in the myocardium on the ECG: what does it mean and what can it mean?
An electrocardiogram is commonly used to detect abnormal heart rhythms and investigate the cause of chest pain. And it happens that after the test the doctor tells the patient that he has recorded myocardial changes on the ECG. What does this wording mean? This is a signal that the heart muscle is undergoing changes. And the doctor’s task is to find out their character. They can be caused by age (for example, myocardial changes are very common in children and the elderly), or by an inflammatory disease. Or perhaps it’s due to intense sports activities. Athletes experience thickening of the myocardial walls. This condition even received a special term - “athletic heart”.
Three types of changes can occur in the entire cardiac muscle or in any part of it:
- metabolic;
- diffuse;
- dystrophic.
The most common are diffuse moderate changes in the myocardium. What it is? This is a uniform damage to all parts of the heart muscle. Possible causes are an inflammatory process in the myocardium or problems with the exchange of water and salt. Or there may be a consequence of taking medications such as cardiac glycosides.
Moderate metabolic disorders in the myocardium are usually associated with high loads and irritants, including hypothermia, excess weight, and stress. If stimuli are applied irregularly, the myocardium returns to normal.
Sometimes moderate dystrophic changes in the myocardium are detected on the ECG. What does the difference in energy consumption by the body and its flow to the heart mean?
Diabetes mellitus (DM) is a major metabolic disorder and currently affects more than 250 million people worldwide. The number of people with diabetes is projected to increase to 350 million by 2030. This pathology often causes moderate changes in the myocardium. We have already found out what this is, it remains to find out what the consequences of neglecting the ECG results can be.
If you do not pay attention to changes in the myocardium, accompanied by unpleasant symptoms, this can lead to the development of coronary heart disease, chronic cerebral ischemia and cardiomyopathy. What is chronic cerebral ischemia? In short, it is a gradual deterioration in cerebral blood flow. A frequent “companion” of this disease is stroke.
Symptoms that should prompt you to see a doctor:
- Dyspnea.
- Arrhythmia.
- Painful sensations in the heart area.
- Regular and unexplained fatigue.
How to deal with moderate myocardial changes:
- Try to lose excess weight.
- Treat old (chronic) diseases.
- Do not overcool or overheat.
- Do not subject yourself to great nervous and physical tests.
- Donate blood for hormones and blood sugar levels.
What to do if changes in myocardial function are detected? Be sure to make an appointment with a cardiologist and, together with your doctor, develop a set of health measures.
Diagnostic changes
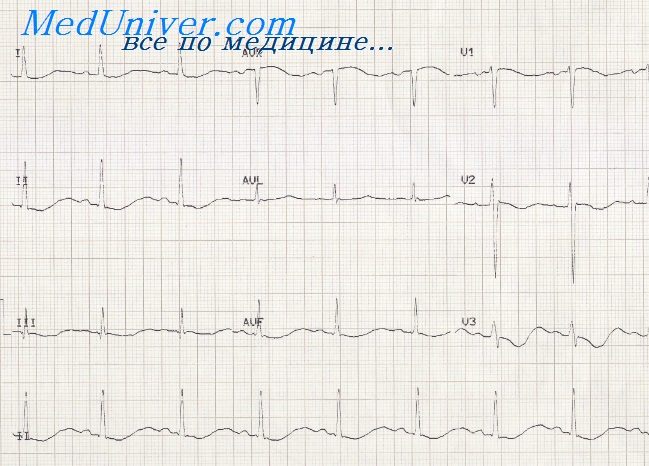
It cannot be said that dystrophic changes in the myocardium on the ECG have special characteristics that contributed to the diagnosis. For this reason, the result is valuable if it is supplemented by patient complaints, examination data and laboratory tests.
Research plays an important role in diagnosis. An electrocardiogram or Echo-CG makes it possible to distinguish diffuse changes from focal ones, which are a consequence of a heart attack or rheumatism. Diffuse pathology is noted in all leads on the ECG, while focal pathology is observed in one of the two. The doctor can recognize rhythmic changes, conductivity features, and an increase in the volume of some sections.
Uncharacteristic ultrasound reflections are noted throughout the myocardial tissue. You can also detect dilatation of some parts of the heart, an increase in the mass and volume of the myocardium, and insufficient motor activity. This also includes additional manifestations of reduced contractility.
Treatment tactics
Treatment begins with taking into account the results of the ECG. In specific cases of this disease, pathogenetic mechanisms take place, the characteristics of which determine further therapy.
Treatment involves more than just treating the underlying disease. Medicines that improve metabolic processes and eliminate electrolyte disturbances are indicated. The doctor may resort to therapy that includes anabolic steroids. Non-steroidal anabolic drugs and vitamins U, E, B are also actively used. In some cases, substances containing calcium, potassium or magnesium are indicated. In order to have a beneficial effect on maintaining muscle function, cardiac glycosides are used, but in minimal doses.
Any disease can be prevented, and metabolic dystrophic changes in the myocardium are no exception. First of all, it is necessary to start with identifying the underlying disease and its treatment, which caused such changes. It is also important to protect the patient from risk factors. The main ones are:
- acute and chronic illnesses;
- disruptions in the schedule of nutrition, work and rest.
Even moderate dystrophic changes in the myocardium can affect the quality of life, so it is worth avoiding psycho-emotional effects on the body whenever possible, normalizing the daily routine, and most importantly, giving up bad habits, if any. In order to cure the disease, or even better to prevent it, strive to adhere to physical and psychological peace.
infocardio.ru
Prevention
The use of traditional medicine is not allowed! Neither for treatment nor for prevention. The only thing a person can do in the fight against cardiac pathology, besides medical treatment, is to monitor their lifestyle and, if necessary, change it. Recommended:
- Elimination of negative factors: strength training, diets and fasting (vegetarianism), harmful production and pills (avoid self-medication).
- Visiting sanatoriums, consuming enough water rich in vitamins and minerals (especially potassium, magnesium, calcium).
- Observe the work and rest regime, do not overexert yourself (physically, intellectually and psychologically).
If you constantly monitor your condition and undergo an examination by a doctor, the risks are reduced.
- Engage in regular but feasible sports and therapeutic exercises.
- Regular medical examinations and timely treatment of any inflammation or infections in the body.
- Check your heart regularly with an electrocardiogram.
Dystrophic changes in the myocardium on an ECG can be detected in the early stages, when the process is still reversible.
From this video you will learn about the features of treatment of myocardial dystrophy:
Reasons for development
Myocardial dystrophy is always a secondary disease that occurs against the background of another pathology and (or) the action of toxic substances.
| Group of factors | Specific reasons |
| Toxins | Alcohol Narcotic drugs Overdose of cardiac drugs Poisons Hazardous substances Chemotherapy drugs with cardiotoxic effects Nonsteroidal anti-inflammatory substances |
| Dyshormonal and endocrine (dishormonal myocardial dystrophy occurs) | Pheochromocytoma – neoplasm of the adrenal glands Thyrotoxicosis (increased activity of thyroid hormones) Diabetes Antiphospholipid syndrome - destruction of own lipids on cell walls
|
| Food | Extreme obesity Significant weight loss (cachexia) or weight loss over a very short period of time
|
| Physical agents | Blunt chest injuries in the projection of the heart Vibration Radiation Weightlessness |
| Infections | Tonsillitis Syphilis HIV infection |
| Gastrointestinal | Any types of hepatitis Liver failure Atrophic gastritis |
| Storage diseases | Amyloidosis – accumulation of amyloid in organs Wilson-Konovalov disease - accumulation of copper in cells Mucopolysaccharidosis – excessive deposition of mucopolysaccharide Glycogenosis – accumulation of excess glycogen in the kidneys, liver, heart |
| Diseases with impaired renal filtration | Glomerulonephritis – degeneration of kidney tissue Myeloma is a tumor of blood cells Chronic compartment syndrome - occurs when a part of the body gets caught under a heavy object |
| Family hereditary diseases affecting the neuromuscular system | Progressive neuromuscular dystrophy - degeneration of muscle fiber cells into connective tissue Spinal amyotrophy – degeneration of spinal cord cells into inactive connective tissue Paroxysmal myoplegia – attacks of muscle weakness Myasthenia gravis – progressive loss of muscle strength |
| Other | Neurogenic pathology – neuroses, dystonia Physical overexertion Anemia – decreased hemoglobin levels |
Stages and symptoms of the disease
Myocardial dystrophy develops in stages. Each stage of the process has its own symptoms, corresponding to the degree of disruption of biochemical processes in the tissues of the heart. In addition to these manifestations, patients have complaints inherent to the underlying disease - the cause of myocardial damage.
The first, or neurohumoral, stage
- Variable, indistinct, weak painful sensations in the projection of the heart. They occur against the background of emotional or physical stress. There is no pain at rest.
- Moderate fatigue after usual exercise.
- There may be a slight loss of body weight.
- Patients feel well and can do their usual activities.
- There are no changes in the study of myocardial function.
Second, or stage of organic change
Third, or stage of heart failure
- Shortness of breath, sharply worsening when lying down. In the extreme stage, patients can only sleep lying down.
- Severe weakness, progressive fatigue from any work.
- Inability to perform usual activities and physical activities.
- Loss of body weight.
- Increased heart rate.
- Violation of the rhythm of myocardial contractions.
- Swelling of the feet and legs.
- Moist wheezing in the lungs when breathing.
- Significant changes in research.
Treatment of dystrophic changes in the myocardium
Dystrophic changes in the myocardium From the moment of birth, it is common for a person to feel the rhythm of the heart, which is perceived by him as the heartbeat of life itself. The functionality of the heart muscle, which has no breaks or days off, is truly unique. The main task of this organ is the continuous pumping of blood throughout the body.
However, there are cases when pathological changes occur in the muscle tissue of the heart associated with disruption of biochemical processes. This disease is called dystrophic changes in the myocardium. We will consider below what consequences this process entails for the functioning of the body and the functioning of the heart.
The muscles of the human heart wall, thanks to extremely complex heterogeneous, autogenous and neurohumoral processes in the body, are capable of generating a bioelectric impulse from biochemical processes into mechanical energy responsible for creating rhythmic movements of the heart. And the consequences of changes in the balance of the body, first of all, result in changes in the myocardium of the posterior and lower walls of the ventricle of the heart. They may be cardiac pathologies, hormonal imbalances, or the consequences of a viral infection.
When metabolic processes in the heart muscle are disrupted, the production of energy compounds decreases and toxic substances accumulate. This leads to the development of myocardial dystrophy. It is accompanied by pain in the heart, tachycardia and arrhythmia, fatigue, and shortness of breath. For treatment, drugs are used that improve myocardial nutrition, normalize rhythm and blood circulation. Read this article
Depending on the damaging factor, cardiac muscle dystrophy occurs:
- nutritional (eating disorders, beriberi disease, scurvy);
- dishormonal;
- diabetic;
- anemic;
- catecholamine (adrenal hyperfunction);
- thyrotoxic (excess of thyroid hormones);
- tonsillogenic;
- alcoholic;
- toxic;
- mixed.
And here is more information about fatty degeneration of the myocardium.
With thyrotoxicosis, the formation of energy compounds (ATP, creatine phosphate) decreases, and protein metabolism changes. In this case, an excess of hormones activates the work of the sympathetic nervous system. In patients, the pulse and blood circulation accelerate, and the volume of blood released per minute increases. The heart works under high load conditions, and not enough energy is produced for this.
Symptoms are associated with various forms of arrhythmia: tachycardia, extrasystoles, atrial flutter. Long-term hyperfunction of the thyroid gland leads to weakness of myocardial contractility, heart pain, shortness of breath, edema and congestion in the liver. Hormone deficiency slows down the rate of metabolic processes, leads to fluid retention in myocardial cells, increased sodium and decreased potassium levels. Patients experience a rare heart rhythm, impulse blockade, constant dull and aching pain in the heart, and dizziness.
Alcoholism
It has been proven that daily consumption of 60 - 80 ml of ethyl (3 bottles of beer or 200 ml of vodka, 5 glasses of wine) after 7 - 8 years is guaranteed to lead to myocardial dystrophy. In case of liver dysfunction, stress overload, infections, this period is reduced to 2 years or occurs when taking smaller amounts of alcoholic beverages.
Toxic form
Appears with prolonged treatment with hormones (Hydrocortisone, Prednisolone, Betamethasone, Dexamethasone) or non-steroidal anti-inflammatory drugs (Ibuprofen, Indomethacin), cytostatics (Methotrexate, Cyclophosphamide), antibiotics (Doxorubicin, Tetracycline), antidepressants, tranquilizers. Acute poisoning is caused by carbon monoxide, phosphorus salts or arsenic acid, chloroform. Manifestations of toxic myocardial dystrophy are:
- pain in the heart - aching, stabbing;
- hot flashes, sweating or chills with cold extremities;
- low exercise tolerance, severe weakness;
- headache;
- arrhythmia - tachycardia, extrasystoles, attacks of atrial fibrillation, atrial fibrillation, conduction block;
- swelling in the legs, accumulation of fluid in the pericardium, abdominal cavity;
- cough, attacks of shortness of breath or suffocation;
- heaviness and pain in the liver.
Myocardial dystrophy develops with frequent sore throats. Accompanied by severe pain in the heart area, constant weakness, a feeling of irregular rhythm, and sweating. Patients often have elevated body temperature to subfebrile levels (37.1 - 37.4 degrees), difficulty breathing, pain in muscles and joints.
In athletes
If the hemoglobin content in the blood drops to 85 g/l and below, then all tissues of the body experience oxygen starvation. The reason for this may be iron deficiency, destruction of red blood cells, trauma, tumors, chronic bleeding (peptic ulcer, hemorrhoids, uterine), intravascular coagulation syndrome (DIC). Symptoms of anemic dystrophy of the heart muscle:
- pale skin,
- frequent dizziness,
- increased heart rate,
- pulsation of the arteries of the neck,
- dyspnea,
- tachycardia.
Low estrogen levels and fluctuations in hormone levels lead to the development of dystrophic changes in the heart muscle in the form of pressing pain, often radiating under the shoulder blade or to the left arm, tingling or discomfort in the heart area. Increased symptoms are observed during periods of hot flashes, sweating and rapid heartbeat. With concomitant arterial hypertension, the likelihood of developing heart failure cannot be excluded.
To restore metabolic processes in the heart muscle, it is necessary to normalize hormonal levels and blood composition, treat infections, intoxication and anemia, completely stop drinking alcohol and smoking, and avoid physical and emotional stress. Drug therapy includes:
- vitamin complexes (Neurorubin, Milgamma);
- lipoic acid (Tiogamma turbo, Espa-lipon);
- antioxidants (Vitamin E, Nicotinamide, Selenium);
- antihypoxants (Cytochrome, Mexidol, Corvitin);
- potassium and magnesium salts (Panangin, Magne B6, Kalipoz prolongatum);
- antiarrhythmic (Atenol, Breviblok, Cordarone);
- cardiotrophic agents (Riboxin, Potassium orotate, Preductal, Carnitine, ATP, Cardonate);
- adaptogens (ginseng tincture, Pantocrine);
- diuretics (Trifas, Veroshpiron), cardiac glycosides (Digoxin), ACE inhibitors (Prenesa) for heart failure.
Diagnostics
The difficulty in making the correct diagnosis for myocardial dystrophy lies in the absence of changes during examination at the first stage of the process. At this stage, only the underlying disease can be identified, for which secondary myocardial dystrophy is typical.
| Examination method | Characteristic changes |
| Inspection by system | Enlarged heart size with a shift to the left Irregular pulse (sinus arrhythmias) |
| Auscultation (assessment of heart murmurs by ear) | Moderate muting of tones at all points Weakness of the first tone at the cardiac apex Weak systolic murmur |
| Electrocardiography (ECG) | Sinus arrhythmia (extrasystole, increased or decreased heart rate) Low voltage of the ventricular complex Partial bundle branch blocks Impaired repolarization (recovery after contraction) of the heart |
| ECG with drug tests (potassium, beta blockers) | Improvement of pathological changes |
| Velergometry (ECG under physical activity) | There is no increase in the volume of blood ejected during contraction Decreased exercise tolerance Inability to fully perform the required load |
| Ultrasonographic examination (ultrasound) | Heart enlargement Expansion of the cavities of the heart chambers at the third stage of the disease Decrease in the volume of blood released during myocardial contraction in the phase of organ dysfunction |
| Scintigraphy with Thallium 201 | Impaired passage of potassium and sodium ions through the cell wall Pathology of myocardial metabolic processes |
| Magnetic resonance imaging (MRI) with radioactive phosphorus | Decrease in the amount of energy reserves of cardiac muscle cells Change in pH (acidity) of the cellular fluid |
| Biopsy (tissue sampling) of the myocardium with histochemical analysis | Pathology of enzymatic metabolism in heart tissue Destruction of myocardial fibers Changes in organ cells |
The most accurate diagnostic method is the sampling of myocardial tissue, but given that the procedure requires cardiac puncture, the indications for it are extremely limited. A biopsy is performed only in difficult diagnostic situations when myocardial dystrophy cannot be established by other methods.
Diagnosis of myocardial dystrophy

The diagnosis of “myocardial dystrophy” is always only an addition to the main diagnosis. In cases where there are clear signs of myocardial dystrophy, but the cause that caused them is unclear, a thorough search for the underlying disease is necessary.
Differential diagnosis of myocardial dystrophy is usually carried out with myocarditis, myocardial or atherosclerotic cardiosclerosis, coronary heart disease, and neurosis. An accurate diagnosis is often made by excluding possible heart diseases. The main criterion that makes it possible to assert that myocardial dystrophy has developed is to identify its cause.
The most common method of examining patients is electrocardiography, which provides sufficient information for the initial manifestations of cardiac dystrophy.
- The doctor at the functional diagnostics office determines metabolic changes, conduction disorders (blockades) and rhythm by the nature of the teeth when deciphering.
- During auscultation, one can indirectly suspect the onset of pathology by dull heart sounds.
- Histological studies are carried out in a living person extremely rarely. It is possible to take material for a biopsy for differential diagnosis with a tumor.
- Magnetic resonance imaging shows the degree of energy deficiency of the heart muscle.
Unlike acute myocardial infarction, biochemical blood samples do not show signs of tissue breakdown (transaminases, creatine phosphokinase, lactate dehydrogenase) and leukocytosis.
Treatment methods
Myocardial dystrophy refers to diseases that can be completely cured provided that the underlying cause of the pathology is stabilized, but only if the disease has not entered the phase of cardiac failure. In this case, it is only possible to improve the quality and prolong the patient’s life.
Treatment consists of several main areas that must be carried out simultaneously.
Elimination of the causative factor
The main direction of therapy. It is necessary to eliminate the primary disease or causes that caused pathological changes in the heart muscle. The possibility of complete restoration of the myocardium depends on how effective these measures are.
Toxic and dyshormonal myocardial dystrophy respond well to treatment; diseases with genetic transmission (neuromuscular diseases) or associated with excessive accumulation of substances in the cells of internal organs are more difficult to influence.
Dystrophy due to physical overstrain requires the abolition of stress, and neurogenic myocardial dystrophy requires high-quality psychological assistance and sedatives.
Infectious myocardial dystrophies require antibacterial treatment and elimination of the source of infection. For tonsillitis, it is necessary to remove the tonsils during a cold period, otherwise there will be no effect from the treatment.
Alcoholic dystrophies respond to treatment very slowly, the process takes many months and sometimes years. A prerequisite is a complete abstinence from drinking any form of alcohol.
Impact on energy and metabolic processes
Complexes of drugs are used to increase protein synthesis, resistance to free radicals and restore normal electrolyte balance in the myocardium:
As well as means for improving the nutrition of myocardial tissue and increasing its resistance to low oxygen levels:
Significant weight loss is an indication for enteral (oral) replacement support through the introduction of high-calorie nutritional media:
- nutrizon,
- nutridrink,
- resource.
Improved heart function
Medicines are used to maintain and restore normal function of the heart muscle:
Treatment
Dystrophic changes in the heart muscle respond well to treatment. Treatment is carried out in three areas:
- therapy of the underlying pathology;
- normalization of myocardial metabolism;
- symptomatic drugs.
The underlying disease must be treated by appropriate specialists: for ischemic disease - a cardiologist; diabetes mellitus, thyroid dysfunction – endocrinologist; anemia - hematologist.
To normalize metabolism, anabolic hormones “Nerobol”, “Retabolil”, “Riboxin”, vitamin preparations - B, U, E, as well as potassium, magnesium, calcium are prescribed. For ari, “Metoprolol”, “Cordarone”.
Symptomatic treatment includes painkillers and sedatives. Sedatives have a good effect on neurotic and vegetative manifestations.
Forecast
Myocardial dystrophy can be completely restored if the cause of the disease is treatable and therapy is carried out before the onset of severe cardiac dysfunction.
In the case of severe cardiac output impairment, the prognosis is unfavorable - patients die within 1–2 years, even with treatment. Without therapy, patients do not survive for years.
Myocardial dystrophy can occur in an acute form, quickly leading to impaired cardiac function, and cause sudden death (athletes during or immediately after training). In this case, a lack of oxygen occurs in the myocardium, the electrolyte composition of the cells changes and the conduction of excitation through the conduction system is disrupted - the heart stops.
okardio.com
Stages and types
Myocardial dystrophy has a 3-stage course.
- The compensatory stage leads to swelling of the lower extremities, disturbances in heart rhythm, and the appearance of shortness of breath.
- The subcompensatory stage leads to increased symptoms, an increase in the size of the heart and liver, a decrease in the flow of blood into the vessels, and congestion in the lungs.
- The decompensatory stage, in which degeneration of the heart muscle is observed, the symptoms are clearly expressed and the pathological processes in the heart become irreversible.
Forms of dystrophy
By type, depending on the degree of damage to the heart muscle, diffuse, fatty, dyshormonal, ischemic, granular, and focal dystrophy are distinguished.
- Diffuse dystrophy develops against the background of an inflammatory process in the heart muscle, leading to a decrease in oxygen supply, thickening of the muscle layer, swelling, and thrombus formation. Lack of oxygen supply to the heart muscle can lead to complications: the development of leukocyte diabetes, myocardial ischemia, genetic changes in cardiomyocytes, heart failure, which often becomes the cause of death for patients.
- Acute focal ischemic dystrophy of the myocardium occurs without any special symptoms and the main thing is not to start the process. If you suspect or experience pain, burning in the heart area, shortness of breath, dizziness, you should urgently consult a doctor, undergo an ultrasound of the heart, suggested instrumental studies to visualize the affected areas of the muscle layer and prescribe timely treatment.
- Fatty degeneration of the myocardium leads to the accumulation of fat droplets in the cells of the muscle layers, their increase in size, destruction of mitochondria, stretching and flabbiness of the muscle cavity, clay-yellow tint of feces, accumulation of fatty cardiomyocytes, which inevitably leads to disruption of cellular metabolic processes, destruction of lipoproteins in the heart cells. The main causes of development are alcohol intoxication, heart and blood diseases, hypoxia and vascular stenosis.
- Dystrophy of the middle layer of the heart muscle develops more often in athletes, when the number of heart beats exceeds more than 200 beats/m, the muscles do not have time to completely relax, internal muscle tension occurs, blood circulation is impaired, oxygen supply to organs and vessels decreases, and anaerobic glycolysis develops during milk ejections. acids into cells in reserve in large volumes.
- Dishormonal dystrophy is more common in women aged 55-60 years against the background of hormonal imbalance during menopause, when tissues and muscles begin to experience oxygen starvation, metabolism manifests itself, estrogen levels decrease, the synthesis of fatty acids is activated in the bloodstream, the muscle layer becomes flabby, and the skin becomes flabby. with a lack of oxygen - pale and swollen. During development in men, testosterone synthesis is disrupted.
- Ischemic dystrophy of the cardiac myocardium is the most dangerous form as a result of coronary crisis and heart failure. If left untreated, it can lead to the development of myocardial ischemia. Dystrophy has many different subtypes depending on the factors - provocateurs that provoked development.
- Dystrophy of the left ventricle of the heart leads to a decrease in the thickness of the muscle layer, the appearance of a number of clinical symptoms in the patient: weakness, feeling, fatigue, disturbances in the rhythm of the heart and intermittent work, pain, shortness of breath, decreased performance, increased fatigue, and a general deterioration in well-being. Urgent treatment is required, otherwise heart failure, cerebral hemorrhage and necrosis of the heart muscle are guaranteed.
What is myocardial dystrophy, and what consequences does it entail?
With myocardial dystrophy, secondary damage to the heart muscle and other pathological disorders occur. For the most part, this pathology develops as a result of complications of heart disease, which affect the nutrition of the myocardium.
The result of the development of dystrophy is low muscle tone, which creates favorable conditions for the development of heart failure. This pathology develops due to oxygen starvation of the myocardium. Tissues may atrophy or even die.
All changes that occur in the heart as a result of the development of myocardial dystrophy are reversible. That is why it is so important to identify the problem in a timely manner and undergo a comprehensive examination. Previously, the risk group included people over 40 years of age, but now there is a tendency to lower this age limit.
There are several forms of myocardial dystrophy. This classification is based on root causes and symptoms:
- The ischemic form develops as a result of lack of oxygen. In some cases, a blood clot may be present in the arteries.
- Focal myocardial dystrophy is caused by disturbances in arterial circulation. This form of pathology can occur without symptoms, and even heart attacks in some cases pass without obvious signs.
- Fatty degeneration of the myocardium develops diffusely against the background of small amounts of fat deposited in cardiomyocytes. As the pathology develops, fat grows and replaces the entire cytoplasm. The cause of this pathology is a lack of proteins and vitamins in the body, which should be supplied with food.
- The dishormonal form occurs against the background of hormonal disorders. More typical for women who have reached menopause. It also often accompanies gynecological diseases. In men, it can be diagnosed due to disturbances in the process of testosterone production.
- The toxic variety is typical for people with alcohol addiction. It can also occur in athletes as a result of physical stress and disturbances in blood circulation.
- Left ventricular dystrophy is not an independent disease; it occurs solely against the background of the development of another pathology.

We figured out what myocardial dystrophy is and even looked at its main varieties, so we can safely move on.
Why does the disease develop?
Heart tissue - diagram
Provoking factors that can affect the functioning of the heart and lead to myocardial damage include:
- acute poisoning of the body with drugs, alcohol, nicotine, other medications, in particular hormones
- high doses of radiation
- stress
- depression
- increased physical activity, when dystrophy is often diagnosed in athletes
- poor meager nutrition and prolonged fasting, inevitably leading to exhaustion of the body
- active overload
- diabetes
- carbon monoxide intoxication
- hypertension anemia
- liver diseases
- cardiac pathologies
- chronic diseases that can lead to changes in blood composition and metabolic disorders
- disorders in the gastrointestinal tract, in particular in the heart
Myocardial dystrophy often develops due to excessive physical exertion, stress, poor nutrition, and moral overload of one’s own body.
Why does dystrophy occur?
There are three groups of reasons:
- Heart pathologies – coronary disease, angina pectoris, myocarditis.
- "Non-heart" diseases.
- A special group is athlete's dystrophy.
The heart receives everything it needs from the blood flowing through the coronary arteries. Coronary artery disease and angina pectoris lead to narrowing of the lumen of blood vessels and poor blood supply. Against this background, ischemic dystrophy develops.
Non-heart diseases include:
- anemia;
- avitaminosis;
- diabetes;
- thyrotoxicosis;
- infections;
- intoxication;
- thyrotoxicosis (Graves disease);
- menopause in women;
- excessive alcohol consumption.
During physical activity, when the heart rate reaches 200 beats, there is no diastole, and energy resources are depleted. These changes are often observed in professional athletes.
During physical activity, when the contraction frequency reaches 200 beats, there is no diastole, and energy resources are depleted. These changes are often observed in professional athletes.

The reasons for the progression of the disease are quite varied
Based on anatomical characteristics, they are distinguished:
- local damage;
- widespread lesion.
How does dystrophy manifest?
Myocardial dystrophy - symptoms
Symptoms may not manifest themselves for a long time. A person considers himself healthy and does not consult a doctor. Over time, dystrophy progresses and inevitably leads to heart failure. Patients develop:
- dyspnea
- pain in the heart and sternum
- hypertensive syndrome
- tingling fingers
- attacks of tachycardia
- cardiopalmus
- weakness and fatigue
- fever and redness of the face
- increased sweating
- feeling of lack of air
- cardiac cough
- lack of energy and strength, which indicates the rapid development of heart failure.
Stitching pain in the heart area sometimes becomes simply unbearable. Symptoms with the development of dystrophy no longer go away without a trace, becoming intrusive, permanent and, of course, dangerous to human life. If the signs have become pronounced and appear even at rest, then most likely there is heart failure and the lack of timely treatment will ultimately lead to a stroke or myocardial infarction.
The main thing is not to miss the primary signs. But the patient often does not attach much importance to the appearance of short-term shortness of breath, fatigue and weakness. But if they become daily and constant, then this is a clear signal that a pathology is developing in the body that requires urgent eradication when:
- there is a dull or aching pain in the heart area
- heart rhythm is abnormal
- decreased blood pressure
- lower limbs swell
- there is a feeling of lack of air, signs of ascites, hematomyelia
- there is severe weakness in the arms and legs, asthenia
- Chronic tonsillitis developed against the background of heart pain
- sweating increases at night
- increased fatigue, nervousness
- often feel dizzy
- sleep is disturbed.
If your weight decreases sharply, pain radiates to your left arm, and you feel unwell due to low blood pressure, then you need to sound the alarm, consult a doctor and undergo an examination.
Diagnostics
Diagnosis begins with finding out the medical history, complaints and a complete examination of the patient. The main diagnostic methods include:
- Ultrasound, MRI of the heart
- radiography
- Cardiography to listen to heart murmurs
- electrocardiography to detect abnormalities in the activity of the heart, regardless of the level of disease development
- Doppler examination to determine the degree of asymmetry and expansion of the cavities of the heart
- ECG for cardiac arrhythmia
- additional tests for excess catecholamines in heart tissue.
Clinical manifestations
There are three groups of symptoms:
- Signs of myocardial dystrophy.
- Manifestations of the underlying disease.
- Heart failure clinic.
The first signs are shortness of breath, fatigue, and weakness. Over time, pain appears in the chest area. The pain is temporary. Low blood pressure and swelling are also considered symptoms of the development of the disease, but they can also indicate pathologies such as extrasystole, tachycardia, and atrial fibrillation.
If concomitant diseases are present, the clinical picture may vary. In anemia, myocardial metabolism suffers if hemoglobin is below 80 g/l. Manifested by tachycardia, chest pain, shortness of breath. In the clinic of thyrotoxicosis, a “bouncing” pulse, shortness of breath, and high pulse pressure predominate. Hormonal metabolic disorders in the myocardium develop during menopause. They are accompanied by vegetative disorders: redness of the face, a feeling of heat, increased sweating. Alcoholic cardiopathy manifests itself in the form of a feeling of lack of air and rapid heartbeat. Cardiac dystrophy, which occurs against the background of angina, is manifested by chest pain and shortness of breath.

The main symptoms include: high fatigue
The combination of symptoms of dystrophy and the underlying disease complicates clinical diagnosis and requires the use of more complex instrumental and additional research methods.
How is the treatment carried out?
Treatment of myocardial dystrophy
Doctors believe that the disease is completely reversible if treatment is started in a timely manner. The main thing is to direct the course towards:
- change in metabolic processes
- elimination of heart failure
- improvement of conduction processes and electrolyte metabolism by intravenous administration of magnesium, potassium salts, vitamins B6 and anabolic hormones to replenish the heart muscle
- elimination of disturbances in protein metabolism.
Drug treatment consists of prescribing to the patient:
- pyridine nuclides
- cardiac glycosides for obvious heart failure to improve electrolyte balance and replenish potassium salts (Panangin, Cardin, Asparaginate)
- drugs to improve metabolic processes and stabilize electrolyte metabolism
- anabolic steroids to stimulate protein metabolism in the body and tissue repair
- non-steroidal drugs (potassium orotate, inosine, panangin)
- vitamin complexes to restore and improve the functioning of the heart muscle
- beta blockers
- cardiac glycosides for heart failure, rhythm disturbance.
Diabetes mellitus leads to myocardial dystrophy, so the patient may additionally be referred to an endocrinologist for hormone replacement therapy with drugs containing:
- iron (erythropoietin)
- magnesium, cardiotropic drugs (magnesium orotate, Panangin, Magnerot, Cardiomagnyl, folic acid)
A complex disease - myocardial dystrophy and complex treatment including a course of physiotherapy, massage, medicinal baths, as well as nutrition with a complete refusal of spicy foods, strong coffee, tea, alcohol and smoking. It is important to completely reconsider your lifestyle.
Post-rehabilitation period
Patients diagnosed with myocardial dystrophy are advised to resort treatment, balneotherapy, physiotherapy, treatment of thyroid diseases, taking iron vitamins for severe anemia, sedatives if the disease is caused by stress and emotional experiences. It is important to normalize metabolism and maximally support the body, in particular the heart muscle, with vitamins and minerals, so diversify your diet and walk more in the fresh air.
Patients during treatment, as well as in the post-rehabilitation period, will undergo a planned ultrasound and ECG of the heart in order to prevent further progression of the pathology and activation of inflammatory processes in the structures of cardiomyocytes.
Based on the fact that myocardial dystrophy develops due to the presence of any disease, the best preventative measure is its treatment.
Taking vitamins and microelements will help strengthen the general condition of the body and prevent weakening of the immune system. In addition, in order to prevent the occurrence of diseases, it is necessary to undergo an annual medical examination.
Thus, the best prevention of diseases is an attentive and caring attitude towards your own health. Myocardial dystrophy is a disease whose existence may not be known until a certain point. But if you listen to yourself and your own body, pay attention to even the slightest deviations from the normal state, you can easily avoid serious diagnoses by getting rid of the disease at the initial stages of its development.
med-advisor.ru
Causes of the disease
There are several main factors that can become a catalyst for the occurrence of this disease. These include:
- insufficiently fortified diet, which can cause anemia;
- birth defects;
- hypertension;
- diseases that provoke a malfunction in the body’s metabolic processes, the most common of which is diabetes;
- powerful effects on the liver of harmful toxic substances;
- imbalance of hormones in the body resulting from diseases of the thyroid gland.
In addition, in addition to all of the above, regular overstrain of the heart during sports also leads to the occurrence of modifications of the myocardium. Basically, in people with active physical activity, dystrophic changes in the myocardium in the left ventricle are found.
Stages and symptoms of the disease
Symptoms such as shortness of breath, rapid heartbeat even at rest, and increased fatigue gradually develop. There is no pain in the heart area, but many patients report some discomfort.
As the pathology develops, the symptoms intensify. Shortness of breath and tachycardia are accompanied by a cough, especially at night.
Dystrophic changes in the heart muscle occur in three stages:
- The myocardium wears out. The patient experiences symptoms such as heart pain and heavy breathing. The level of physical endurance is significantly reduced. No changes can be seen on the electrocardiogram.
- The initial stage of deterioration of contractile function. Symptoms such as arrhythmia, swelling of the extremities, and shortness of breath occur. The cardiogram shows minor changes.
- Contractile function is greatly reduced. The tone of the heart muscles decreases. The patient is accompanied by symptoms such as swelling, constant pain in the heart, shortness of breath, and fatigue. All changes are clearly visible on the ECG.
Diagnosis, treatment and prevention
Diagnosis of dystrophic changes in the myocardium begins with a detailed questioning about the patient’s complaints and condition. Particular attention is focused on the profession and finding out whether the patient was involved in sports. After this, the doctor prescribes an electrocardiogram, ultrasound examination of the heart and thyroid gland, and MRI. If a hormonal system disorder is suspected, a blood test is prescribed to determine the level of necessary hormones.
An ultrasound of the heart indicates its size and pathological changes. Sometimes, for a more detailed study of the heart muscle, a biopsy is prescribed. Using a special instrument, the chest is pierced and a piece of tissue is pinched off, which is examined under a microscope.
Types of pathological changes
The classification is:
- Dyshormonal myocardial dystrophy.
- Dysmetabolic myocardial dystrophy.
- Myocardial dystrophy of mixed origin.
- Myocardial dystrophy of complex genesis.
Dyshormonal myocardial dystrophy occurs as a result of hormonal imbalances. The disease usually affects women during menopause and men with testosterone production disorders.
This type of disease in women develops at an accelerated pace, therefore it is recommended that after 45 years of age undergo preventive examinations in order to identify changes in the myocardium as early as possible.
Myocardial dystrophy of the metabolic type is not considered by most doctors to be a separate type of disease - these are dystrophic changes as a result of metabolic disorders.
This may happen if:
- a person lacks vitamins and minerals;
- protein metabolism in tissues is disrupted.
A disease of mixed origin occurs as a result of the presence of low hemoglobin, vitamin deficiency, endocrine disorders, that is, the pathological process begins under the influence of several factors. Such diffuse-dystrophic changes lead to deformation of the myocardium, stretching of its cells and a decrease in the thickness of the septum.
Diffuse-dystrophic changes of complex genesis develop under the influence of external factors:
- alcohol abuse;
- smoking;
- addiction;
- endocrine and metabolic disorders;
- poisoning of the body.
Treatment of myocardial dystrophy
In some cases, it even helps normalize heart function.
Treatment of myocardial dystrophy is carried out using the following drugs:
- Metabolic agents. They reduce changes in the heart muscle, eliminate symptoms, and improve the patient’s well-being.
- Antioxidant drugs. They prevent lipids from oxidizing in the heart muscle cells. Thanks to this, cell membranes are not damaged and harmful substances do not penetrate into them.
- Calcium channel antagonists. A high calcium content in the cells leads to relaxation of the heart muscle tissue, which disrupts its energy supply and damages the cell structure. Therefore, these drugs are indispensable in the treatment of myocardial dystrophy if the patient does not suffer from heart failure.
- Stabilizers of lysosomal membranes. They stop the penetration of an enzyme into cells that destroys protein.
- If there is a lack of salts in the heart muscle, potassium supplements may be prescribed. They make up for the shortage.
- Beta blockers are used to make stress have less of an impact on the heart. They are especially often prescribed if the patient suffers from hypertension, arrhythmia or tachycardia.
- Antihypoxants. Such drugs eliminate the lack of oxygen in the heart muscle.
Lifestyle with myocardial dystrophy
Following your doctor's recommendations will significantly improve your well-being and speed up your recovery.
The patient must correctly distribute physical activity.
It is advised to adhere to the following rules:
- Sleep at least eight hours a day and rest for at least an hour during the day.
- Light physical exercise is helpful. It is better if you do them every day, but excessive load is contraindicated. This may make the condition worse.
- It is advisable to perform breathing exercises, swim, walk several kilometers, and ride a bicycle.
- If during physical activity your heart begins to hurt, weakness and shortness of breath appear, you need to take a break until your health returns to normal.
- It is not advisable to be in extremely high or low temperatures. Heat speeds up the heartbeat and increases the load on the heart muscle, while cold leads to vasospasm and poor circulation.
- It is important to avoid stress and nervous tension. You can use sedatives of herbal origin, for example, valerian or motherwort. It is useful to do meditation and auto-training. This helps many people calm down.
- You need to stop drinking alcohol and smoking. They increase the load on the heart and negatively affect the course of the disease.
A disease such as myocardial dystrophy also requires proper nutrition. It is necessary to exclude coffee, fatty, spicy foods, smoked foods and spices, and rich broths from the diet. It is healthy to eat more vegetables, fruits, dairy products, berries, baked meats and low-fat fish.
Dystrophic changes in the myocardium are quite treatable; the main thing is to consult a doctor in time before irreversible processes begin.
We recommend reading:
serdce1.ru