Parenchymal organs
All human internal organs can be divided into two large groups:
- Cavity;
- Parenchymatous.
With the cavitary, everything is very clear - this is the stomach, intestines, bladder. They have a cavity and a wall supplied with vessels. Bleeding from these organs will only be associated with vascular damage. If the vessel is small, then it is able to contract on its own, narrowing its lumen, and the bleeding will stop. But what are parenchymal organs?
They have a completely different structure:
- Liver;
- Lungs;
- Pancreas;
- Kidneys;
- Spleen.
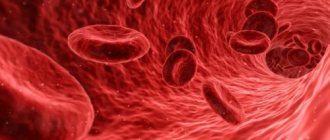
There is no cavity in them, only the main tissue responsible for the function of this organ is parenchyma . It is permeated with many tiny vessels. When a parenchymal organ is damaged, bleeding develops from each of these capillaries.
An unpleasant feature of the parenchyma and its vessels is the inability to contract, stopping the bleeding on its own.
Where are parenchymal organs located?
Reasons for appearance
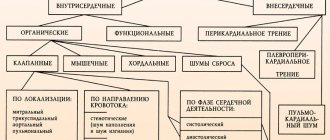
Bleeding, the concept and types, as well as the causes of which depend on the factors affecting the body, is the release of biological fluid (blood) through the vascular bed into the environment or into the body cavity.
The causes of hemorrhage include:
| Type of bleeding | Reason for appearance |
| External | External bleeding occurs as a result of a violation of the integrity of the skin, veins or arteries. Depending on the affected vessels, there are also several types of bleeding. Blood may leak onto the surface of the body from wounds, ulcers and skin tumors. |
| Interstitial | The cause of interstitial bleeding is bruises or fractures, various types of injuries. Also an important factor in the development of interstitial hemorrhage can be pathologies of the cardiovascular system associated with vascular permeability and blood clotting. |
| Intracavity | Intracavitary bleeding is closely related to injury to a parenchymal organ. The disease can also develop due to the pathology of a damaged organ. |
| Pulmonary | Pulmonary hemorrhage is the most dangerous, since during the hemorrhage the biological fluid can completely fill the lung. When the lungs are damaged, there is a lack of air and breathing problems. Pulmonary hemorrhage can result from advanced forms of respiratory system diseases. Congenital defects and pathologies also influence the appearance of hemorrhage. |
| Gastrointestinal | The causes of gastrointestinal hemorrhage are ulcers, colitis, and tumors. Also, vomiting blood can be caused by foods that are contraindicated for a certain disease. |
| Afibrinogenic | The cause of this hemorrhage is severe and lengthy operations on the abdominal and thoracic cavity. Over a long period of time, a lot of fibrinogen is consumed. |
| Postoperative | Postoperative hemorrhages = secondary. They occur when a blood clot is pushed out. |
There is also a classification of bleeding according to the affected vessel. The cause of such hemorrhages is direct trauma to the blood vessels or diseases of the vascular system.
Causes
The development of parenchymal blood loss is preceded by a violation of the integrity of the organ. Rupture of the parenchyma and small capillaries become a direct source of hemorrhage.
Reasons that can lead to damage to a parenchymal organ:
- Injuries;
- Infections;
- Malignant tumors;
- Vascular tumors – hemangiomas.
Abdominal and chest injuries often occur as a result of road traffic accidents. Under the influence of an impact on the dashboard, steering wheel or other parts of the car, a parenchymal organ ruptures. Similar changes occur when the abdominal cavity is injured.
The greatest danger in cases of blunt abdominal trauma is two-stage ruptures. First, blood accumulates under the organ capsule, forming a bruise. At this time, your health does not suffer. Over time, the hematoma grows, overstretching of the organ capsule occurs, it ruptures and symptoms of internal bleeding develop.
An infection such as tuberculosis often affects lung tissue. Certain forms of tuberculosis cause destruction of lung tissue. The cavity that forms is called a tuberculous cavity. Bleeding arising from the cavity is manifested by a strong cough with bloody, foamy sputum.
Cancerous tumors can affect many organs, including parenchymal ones. Growing into the tissue of an organ, the tumor destroys it. At some point, bleeding may occur from the area affected by the tumor.
A large number of vessels that always penetrate the tumor predisposes to this. Bleeding is especially large due to hemangioma, a tumor consisting entirely of blood vessels.
Causes of parenchymal bleeding
Parenchymal organs have a strong blood supply; even minor damage to the capsule can cause massive bleeding. The main cause is injuries - falls from heights, impacts, traffic accidents. In addition to injuries, hemorrhages can be caused by:
- cyst rupture;
- organ compression;
- parasitic lesions;
- infectious diseases (tuberculosis);
- pathological processes in the parenchyma;
- malignant and benign tumors.
Problems with the blood coagulation system further worsen the condition.
Important! The walls of the vessels are fused with the connective tissue membrane, the vessels do not collapse, so stopping the bleeding on your own is impossible.
When exposed to a damaging factor, the surface of the organ begins to bleed profusely. Due to the impregnation of organ tissues, hemorrhages appear. Blood pours into the abdominal or chest cavity, forming hematomas. The simultaneous appearance of hematomas and hemorrhages is possible. Even mild bleeding leads to the development of anemia. Cells and organs begin to suffer from increasing hypoxia. The level of red blood cells and hemoglobin in the blood decreases.
Features of blood loss
Rupture of a parenchymal organ is manifested by bleeding from the site of injury. Blood flowing inside the body is not visible externally. Internal parenchymal bleeding develops.
Blood is responsible for delivering oxygen and nutrients. It ensures normal immunity and maintains blood pressure. The loss of even a small amount of blood results in symptoms of anemia.
Acute blood loss due to parenchymal bleeding is an emergency condition. A lack of circulating blood volume primarily affects blood pressure. It decreases as the blood supply to the vessels decreases. All organs suffer from lack of oxygen. The body tries to the last to maintain nutrition in the most important parts of the body - the brain, kidneys, heart.
The kidneys are one of the first to suffer - with low pressure they are not able to perform their function. The kidneys stop filtering urine, and its production decreases. With severe blood loss, the kidneys completely stop working, and no urine is produced at all.
All other organs also suffer from blood loss. For the brain, this manifests itself as loss of consciousness. For the heart - severe pain and heart rhythm disturbances.
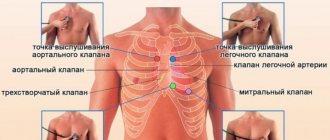
Primary diagnosis
To make a diagnosis of internal bleeding, you need to rely on several factors.
1). Patient history : presence of previous injury or chronic diseases of internal organs - cirrhosis of the liver, various types of leukemia.
2). A thorough examination of the patient : the presence of traces of injury (bruises, abrasions, rib fractures) or signs of disease of the internal organs (yellowness of the skin and mucous membranes and enlarged liver with cirrhosis).
3). Complaints : the appearance of acute pain at the site of suspected bleeding.
First aid measures for arterial bleeding
4). Symptoms of acute blood loss : severe pallor of the skin and mucous membranes, weakness, cold sweat, rapid breathing and heartbeat, decreased blood pressure, loss of consciousness.
Symptoms
Signs of parenchymal bleeding depend on the volume of blood lost. In total, about 7% of body weight in the human body is blood.
Doctors measure the amount of blood lost due to bleeding as a percentage of the total circulating blood volume:
- Up to 10% - light bleeding;
- 10-20% - moderate bleeding;
- 21-30% - heavy bleeding;
- More than 30% - massive, critical blood loss.
Symptoms of parenchymal bleeding are caused by a lack of blood and oxygen starvation of all organs. With severe blood loss, they develop rapidly, within a few minutes. Weak parenchymal bleeding can worsen a person’s condition for a day or more.
The victim is concerned about:
- Severe weakness;
- Dizziness;
- Flashing flashes and black dots before the eyes;
- Loss of consciousness;
- Nausea, vomiting;
- Pain in the area of the affected organ;
- Lack of urine;
- Cold sweat;
- Pale skin.
When you try to feel the pulse, its weak filling and frequency are determined. Doctors call this pulse “thread-like” because it is almost not felt. If there are no pulse waves on the wrist, you should try to determine them on the neck, in the area of the carotid artery. Find out why it is called that.
In a state of severe blood loss, the pulse is maintained only in large arteries such as the carotid artery. But even there it is weak and very frequent.
Blood pressure measurement is mandatory. Values lower than 90/60 mmHg are considered hypotension. Blood loss is always accompanied by low blood pressure.
This is due to poor filling of blood vessels. The lower the pressure, the more frequent and weak the pulse.
The ratio of pulse to upper pressure is called the Algover index. Normally it is 0.5, and with bleeding it increases to one or more. The value of the Algover index indicates the severity of blood loss.
With parenchymal bleeding from the liver, pancreas or spleen, abdominal symptoms can be identified. On palpation, pain in the area of the affected organ is determined. In this same place, the stomach becomes extremely hard. This is due to irritation of the peritoneum by blood pouring into the cavity.
Parenchymal bleeding: signs and first aid
Parenchymal bleeding is when the blood is not released outside, but due to damage to internal organs or in some of their pathologies, flows into the internal cavities of the body (abdominal, pleural).
Types of bleeding
Bleeding is the leakage of blood from blood vessels. Most often it is caused by their damage. This may be a consequence of injury (which happens most often) or the consequences of pathological changes in the body.
Bleeding is usually divided into external, when blood from a damaged vessel flows out through a wound or natural openings, and internal. In this case, blood accumulates in the cavities. The following types of external bleeding are distinguished:
- capillary - occur as a result of superficial damage, blood is released in small quantities, drop by drop;
- venous - occurs as a result of deeper injuries (cut, puncture wounds) and a large amount of dark red blood flows out;
- arterial - the cause is deep injuries in which the wall of the arteries is damaged, while the blood flows out in a pulsating stream and has a bright scarlet color;
- mixed bleeding can also occur with deep injuries, with both arteries and veins bleeding in the wound at the same time.
Internal bleeding can also be classified according to the location of the process. With blows and injuries to the chest, bleeding may occur, in which blood flows into the pleural cavity.
Bleeding in the abdominal cavity can be a consequence of diseases of the organs located in it; in women, it can be caused by an ectopic pregnancy, but most often the cause of internal bleeding in the abdominal cavity is blunt trauma to the abdomen, which is accompanied by rupture of the liver or spleen.
What is parenchyma
Parenchyma is a tissue that forms the basis of many internal organs. Anatomically, it is formed, depending on the task of the organ, by epithelial, nervous, muscle, myeloid or lymphoid tissue.
The peculiarity of these organs is that in each of them the parenchyma forms specialized structures that allow the organ to perform its functions. In the liver these are its lobules, in the kidneys - nephrons, in the spleen - follicles.
It is often difficult to diagnose and therefore may have lost a lot of blood by the time help is given. That is why timely diagnosis and stopping of parenchymal bleeding is a priority task for the surgeon.
The first place among the causes is unconditionally occupied by injury.
Regardless of what caused it - a traffic accident, a blow or a fall from a height - even a minor impact can be enough to cause parenchymal bleeding.
This is due to the fact that even a small tear in the organ capsule (and it is, as a rule, very delicate) is enough to cause the blood vessels that feed the parenchyma and are therefore present in large numbers to become damaged and blood begins to flow into the body cavity.
In addition to injuries, the following pathologies can cause parenchymal bleeding:
- tumors, both malignant and benign;
- infections (tuberculosis);
- pathologies of parenchymal organs (hemangioma);
- parasitic lesions;
- pathology of the blood coagulation system.
The consequence of bleeding in the body can be a hemorrhage (in this case, the gushing blood soaks into the surrounding tissues) or a hematoma. Then a cavity filled with blood forms in the tissue. With parenchymal bleeding, both of these options are possible.
The danger is that the vessels feeding the parenchyma do not collapse due to their structure, which means that bleeding will continue. Even if it is not intense, the symptoms of anemia will still increase, and as a result, the organs and brain will suffer from hypoxia.
With significant blood loss, hemorrhagic shock develops - a serious condition in which blood pressure significantly decreases and signs of multiple organ failure progress.
Despite the obvious danger to the patient’s life, such bleeding cannot always be detected immediately. It often happens that blood loss occurs over a period of time, with virtually no effect on overall well-being.
Parenchymal bleeding in the early stages can be suspected by general weakness, drowsiness, and dizziness. The patient experiences thirst, “sights” and darkening in the eyes, cold sweat. Fainting is possible.
The degree of blood loss can be judged by factors such as pulse, blood pressure and other objective signs.
Moderate blood loss is characterized by an increase in heart rate to 100 beats per minute or higher and a decrease in systolic pressure below 90 mmHg. Art. rapid breathing, pale skin, cold sticky sweat, cold extremities, dry mouth, severe weakness, apathy, adynamia, and lethargy are also noted.
In cases of severe blood loss, systolic pressure drops below 80 mm and the pulse rate may exceed 110 beats per minute. Breathing is shallow, very rapid, yawning, pathological drowsiness, hand tremors, decreased amount of urine output, severe pallor, marbling of the skin, lethargy or confusion, painful thirst, cyanosis of the extremities, acrocyanosis.
Massive internal bleeding is characterized by a decrease in pressure to 60 and an increase in heart rate to 140–160 beats per minute.
Cheyne-Stokes breathing (respiratory movements first deepen and become more frequent, but on the 5th-7th inhalation their intensity begins to decrease, after which there is a pause).
Consciousness is confused or absent, delirium, the skin is sharply pale, sometimes with a grayish tint. Facial features become sharper, eyes become sunken.
In this case, the pressure drops below 60 mm or is not detected at all, pulse contractions are reduced to 2–10 beats, convulsions, agonal breathing are observed, the pupils are dilated, the skin is dry and “marbled.”
As a rule, this condition is irreversible - agony and then death inevitably occur.
Everyone knows very well that very often timely first aid can save a patient’s life. Unfortunately, the same cannot be said about internal bleeding.
Parenchymal bleeding cannot be stopped or reduced with available means; the most important thing that can be done for the victim is to take him to a surgical hospital as soon as possible, that is, call an ambulance.
To prevent the patient’s condition from worsening, before her arrival you can provide the following assistance for parenchymal bleeding:
- give the victim a horizontal position, with legs raised, if hemorrhage into the abdominal cavity is possible, or a semi-sitting position if hemothorax is suspected;
- Apply cold to the area of suspected bleeding.
Note! Patients with symptoms of internal bleeding are strictly prohibited from heating the sore area, inducing vomiting or doing enemas and giving medications that stimulate cardiac activity.
Treatment
To date, the only way to stop parenchymal bleeding is surgical intervention. As a rule, this happens during an emergency operation, before which laboratory tests are performed to evaluate the hematocrit, hemoglobin and red blood cell levels, an ultrasound of the abdominal cavity, and an x-ray.
There are several ways to stop parenchymal bleeding. This:
- organ resection;
- drying out the oil seal;
- electrocoagulation of blood vessels;
- suturing of blood vessels;
- embolization of the feeding vessel;
- use of hemostatic sponges.
Along with stopping bleeding, the most important task is to compensate for blood loss, restore the volume of circulating fluid and improve microcirculation. For this purpose, blood transfusions, plasma and blood substitutes are carried out, as well as administration of a 5% glucose solution and saline solution.
Bleeding even from small vessels poses a danger to human health if they are not noticed and prevented in time. The outpouring of blood from damaged vessels can be both into the external environment and into the cavities of the body.
Suspicion of internal bleeding that has begun requires urgent hospitalization and a full diagnostic examination.
There are different types of bleeding depending on the reasons for their occurrence and the type of vessel from which the blood flows.
First aid measures for bleeding should be started as soon as possible after injury. They consist primarily of stopping bleeding and preventing significant blood loss.
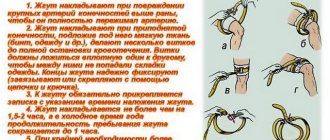
If we are talking about arterial bleeding, the necessary measures to stop the bleeding must be taken immediately, since with this type of bleeding, a significant amount of blood flows out of the wound damage over a short period of time.
Complications
Severe blood loss is scary not only in itself.
Ultimately, it becomes complicated by life-threatening conditions. These pathologies require emergency surgery along with highly qualified care from resuscitators:
- Hemorrhagic shock;
- Disseminated intravascular coagulation syndrome (DIC).
Hemorrhagic shock develops when 30 percent or more of blood is lost. It is manifested by loss of consciousness, almost complete absence of pulse and blood pressure below 60 mm Hg. Treatment for shock is provided in the intensive care unit with the help of transfusions of red blood cells, plasma and colloid solutions.
DIC is a fatal complication of bleeding. Blood loss reaches critical levels, such that the blood loses its ability to clot. Moreover, it can begin to flow not only from the injured area, but also from any organs. Mortality in DIC is high even in an intensive care unit.
Life-threatening blood loss
Massive internal bleeding is characterized by a decrease in pressure to 60 and an increase in heart rate to 140–160 beats per minute. Cheyne-Stokes breathing (respiratory movements first deepen and become more frequent, but on the 5th-7th inhalation their intensity begins to decrease, after which there is a pause). Consciousness is confused or absent, delirium, the skin is sharply pale, sometimes with a grayish tint. Facial features become sharper, eyes become sunken.
Fatal blood loss (as a rule, it is a third of the volume, that is, 1.5–2 liters) is accompanied by the development of a coma. In this case, the pressure drops below 60 mm or is not detected at all, pulse contractions are reduced to 2–10 beats, convulsions, agonal breathing are observed, the pupils are dilated, the skin is dry and “marbled.” As a rule, this condition is irreversible - agony and then death inevitably occur.
First aid
If parenchymal bleeding is suspected, the most important thing is to get it to the clinic. This needs to be done as quickly as possible. Every minute a person loses more and more blood. When more than a third of the circulating blood is lost, bleeding becomes critical. Irreversible changes develop in organs.
The more time passes from the moment of hemorrhage, the less likely it is to have a successful outcome.
You can increase your chances of survival by providing first aid correctly:
- Ice wrapped in a cloth is applied to the area of injury.
- The person sits as comfortably as possible. During transport he is disturbed as little as possible.
- You cannot give any pills, you cannot feed or offer alcohol.
- You can offer a small amount of water or tea.
First steps for parenchymal bleeding
General characteristics of internal bleeding
Such bleeding occurs when the tissues of internal organs are injured. Diagnosis of this condition is usually very difficult.
Most often bleeding occurs:
- due to mechanical damage;
- as a result of neoplasms;
- due to serious illness.
Symptoms may be hidden or mild, so if you suspect the development of such a process, you should immediately contact a specialist. The medical institution will conduct a full examination, which will identify the cause and make prognoses.
Fatal blood loss is approximately 2.5 liters for an adult. In this case, a blood transfusion is performed to save the person's life. Transfusions are performed during surgery and for several days after it. As a result of large blood loss, there is a slow heartbeat, a decrease in red blood cells and other important substances that make up the blood.
The person’s general condition worsens, severe pain appears. The metabolic process is disrupted, the body begins to suffer and experience severe stress. If you have such a problem, you should immediately seek medical help.
Treatment
After the victim is delivered to the clinic’s emergency department, he will be further examined.
Usually these are the most minimal diagnostic procedures that take little time:
- Determination of blood group and Rh factor;
- Determination of hemoglobin;
- Ultrasonography.
Parenchymal bleeding is unable to stop on its own. Almost always, medical care involves surgical intervention. It is started urgently, with little preoperative preparation.
It usually involves transfusions of blood products or solutions to replace the volume of lost blood and raise blood pressure.
There are several ways to stop parenchymal hemorrhage:
- Using a hemostatic sponge;
- Hemming the oil seal;
- Removal of part of an organ;
- Electrical coagulation.
Even an experienced surgeon finds it difficult when the question arises of how to stop parenchymal bleeding. Combinations of methods may be used.
Simultaneously with the operation, hemostatic medications are prescribed:
- Vikasol;
- Etamsylate;
- Aminocaproic acid.
They promote the formation of blood clots in the smallest vessels of the parenchyma. After the hemorrhage stops, the drugs are discontinued. A few more weeks after discharge from the hospital, blood thinning drugs such as aspirin and warfarin are contraindicated for the person.
First aid and surgery
First of all, you should pay attention to the following manifestations:
- presence of abdominal injuries;
- mechanical damage to the chest;
- formation of hematomas and bruises;
- sharp pain in the area of the damaged organ;
- sweat;
- chills and fever;
- cardiopalmus;
- a sharp decrease in pressure.
If you suspect the development of such a condition, the patient should be taken to the hospital as soon as possible, since it is impossible to stop such a process outside the hospital.
Before the doctors arrive, you must:
- Lay the patient down and elevate the legs.
- Cool the suspected area of damage.
When the ambulance arrives, specialists will transport the victim to the hospital and administer medications such as:
- Etamsylate;
- Vikasol;
- Aminocaproic acid.
Medicines will not stop the bleeding, but will improve the patient's condition. In order to maintain pressure, specialists will begin to administer a special solution intravenously.
Once the patient is admitted to the hospital, he will immediately be taken to the operating room where emergency procedures will be performed.
Before performing a surgical intervention, the following measures will be carried out:
- General tests.
- Ultrasound (ultrasound examination).
- X-ray.
If all tests are within normal limits, doctors will perform an emergency operation. Otherwise, diagnostic laparoscopy is performed.
There are several ways to stop such hemorrhage, among them are:
- drying with a special sponge;
- hemming of the omentum;
- amputation of the affected part;
- electrocoagulation;
- sewing using special seams.
During the operation, a blood transfusion is performed, and this procedure is also done several times during the recovery process. In addition, saline solution is infused and maintenance therapy is carried out aimed at preventing the development of DIC syndrome (disseminated intravascular coagulation) and multiple organ failure.
Such bleeding usually becomes a threat to the patient’s life, so it cannot be delayed. The sooner surgery is performed, the better the outcome. With successful surgery, the patient's life can be saved.
Capillary bleeding and first aid
Capillary bleeding is the most common bleeding. It does not pose a threat to human life, since capillaries are the smallest vessels that penetrate all tissues and organs. It has its own distinctive features. The blood flowing from the capillaries has a bright scarlet color, the discharge is not intense, since the pressure in this case will be minimal, and there is no pulsation at all.
First aid algorithm for capillary bleeding
The rules for providing first aid for capillary bleeding are simple.
In this case, there is no need to apply a tourniquet; it is enough to do the following:
- Rinse and disinfect the wound.
The injured area should be tightened tightly, but in such a way as not to disrupt the flow of arterial and venous blood, that is, not too much.
Apply cold to the wound site, which will constrict the blood vessels.
If a person has a superficial wound and no other injuries, then he does not require hospitalization.
Venous bleeding and first aid
Venous bleeding is characterized by the effusion of blood from the veins as a result of their damage. Veins carry blood to the heart from capillaries that supply organs and tissues.
To understand that a person has venous bleeding, you need to focus on the following signs: the blood is dark red or cherry in color. It does not pour out like a fountain, but flows out of the wound slowly and fairly evenly. Even if large veins have been injured and the bleeding is profuse, there is still no pulsation observed. If it does exist, it will be slightly perceptible, which is explained by the irradiation of impulses from a nearby artery.
Venous bleeding is no less dangerous than arterial bleeding. In this case, a person may die not only due to excessive blood loss, but also due to the absorption of air through the veins and its delivery to the heart muscle. Air entrapment occurs when inhaling during injury to a large vein, especially in the neck, and is called an air embolism.
First aid algorithm for venous bleeding
In this case, there is no need to apply a tourniquet and first aid rules boil down to the following:
- If a vein of a limb is injured, it must be raised up. This is done to reduce blood flow to the damaged area.
Then you should begin applying a pressure bandage. For this purpose, there is an individual dressing package. If this is not at hand, then a clean napkin or cloth folded several times is applied to the wound, after which it is wrapped on top with a bandage. You need to put a scarf on top of the bandage.
The place where such a bandage is applied is below the site of injury. It is important to apply the bandage tightly and in a circle, otherwise it will only provoke increased blood flow.
The criterion for assessing the correctness of the actions performed is the absence of bleeding and the presence of pulsation below the wound site.
When there is no clean tissue at hand, you should squeeze the injured limb in the joint as tightly as possible, or squeeze the area just below the blood outlet with your fingers.
In any case, the victim should be hospitalized.
Sometimes, if the bleeding is severe, it cannot be stopped with a bandage alone. In this case, it is advisable to use a tourniquet. It is applied below the wound, due to the way blood is delivered to the heart muscle through the veins.
Gastrointestinal bleeding and first aid
Gastrointestinal bleeding deserves special attention, as it is a life-threatening condition. It is important not to miss the first signs of such blood loss and seek help from a specialist in time. Among them are the following: bloody vomiting with brown impurities, the presence of loose bloody stools, pallor of the skin, increased heart rate with, general weakness accompanied by dizziness, and sometimes loss of consciousness.
First aid algorithm for gastrointestinal bleeding
In order to stop gastrointestinal bleeding, the person must be taken to the hospital.
However, first aid will include the following:
- A person needs complete peace. To do this, it is best to put him in bed.
A cold heating pad or ice pack should be placed on the abdominal area.
You can chop up some ice and give it to the person in small portions to swallow.
Take the victim to the hospital.