Causes of the disease
The direct cause of the condition is acute or chronic blood loss resulting from external or internal bleeding:
- Injuries. When large arteries and veins are damaged.
- Surgery. During surgery, there is a risk of large blood loss due to emergency situations.
- Ulcers of the gastrointestinal tract. Bleeding in this case is not uncommon. The complexity of diagnosis is complicated by the fact that the processes occur inside the body. It is difficult for a person ignorant of medicine to recognize the signs of the disease, so sometimes patients are admitted to the hospital in serious condition and not everyone can be saved.
- Impaired hemostasis. The biological function of the system is to maintain optimal fluid and coagulability of the blood to avoid unnecessary blood loss. If there is a failure in the direction of decreased platelet production, hypocoagulation develops, which leads to spontaneous bleeding.
- Gynecological problems. An acute condition is observed during ectopic pregnancy, when the fallopian tube ruptures; during difficult childbirth; with uterine bleeding. Symptoms of chronic anemia appear with heavy menstruation. Newborns suffer from birth injuries and placental bleeding.
- Liver pathologies. Diseases - cirrhosis, hepatitis, tumors - of the organ cause an increase in pressure in the portal vein, which leads to rupture of the altered veins of the esophagus.
- Lung diseases. A complication of a respiratory disease, when blood, bright scarlet, liquid, sometimes with clots, comes out through the respiratory tract.
- Weakness of the vascular walls occurs with genetic pathologies, lack of vitamin C, radiation sickness, and leukemia.
- Tumors. Hypohemoglobinemia is detected in cancer of internal organs, since the process is accompanied by tissue destruction and hidden blood loss.
- Chronic hemorrhoids. The disease is characterized by the release of fresh blood during exertion and defecation.
- Worm infestation. When parasites are in the lungs, bleeding is present in half of the cases; In the intestines, roundworms, sticking to the walls, damage the mucous membrane.
Due to pathologies and injuries accompanied by blood loss, its volume in the vascular bed decreases. There is a lack of cells containing hemoglobin. And since red blood cells are responsible for the delivery of oxygen, oxygen starvation occurs in the body.
The human body is able to restore up to 500 ml of blood without damage; the disease develops if blood loss exceeds this figure. The loss of half the volume of fluid in the vessels leads to inevitable death.
Etiology and pathogenesis
Hemorrhagic anemia develops when the number of red blood cells or hemoglobin sharply decreases due to prolonged bleeding. Pathology is extremely rarely diagnosed as an independent pathology. As a rule, it is mistaken for a symptom of some disease.
Various factors can trigger the development of anemia. Sometimes they occur against the background of chronic diseases or due to unforeseen circumstances that cause rapid, massive blood loss. These include:
- injuries with large blood loss (rupture of myocardial walls, aortic aneurysm, spleen);
- internal hemorrhages;
- extensive erosions and ulcers;
- fragility of blood vessels;
- operations;
- blood composition disorder.
In women, the causes may be heavy discharge during menstruation, ectopic pregnancy, or injuries received during childbirth. In newborns, anemia can cause placental bleeding and birth trauma. In them it can occur even with excessive sampling of biomaterial during laboratory tests.
In older and middle-aged children, the main cause of anemia is often helminths. They attach to the walls of the gastrointestinal tract, injuring the body and causing microbleeding.
The chronic form is caused by long-term, frequent losses of small volumes of blood. This happens with diseases:
- digestive tract;
- kidney;
- hemorrhoids;
- coagulation disorders (DIC syndrome, hemophilia);
- oncology.
Interesting! Lack of hemoglobin may be due to an increase in the permeability of capillary walls during leukemia, radiation sickness, or an infectious process. Vitamin deficiencies also have a strong effect, especially ascorbic acid, because it helps in the absorption of iron obtained from food.
Main symptoms
Classification of anemia in case of blood loss is carried out according to the degree of development of the condition, distinguished:
- Spicy. Massive blood loss occurs due to injuries and damage to large vessels, with internal bleeding.
- Chronic. Secondary iron deficiency anemia (IDA) gradually develops as a result of diseases.
- Congenital. When the fetus suffers due to blood loss.
Consequently, in patients with posthemorrhagic anemia, symptoms differ depending on the degree of development of the process and the severity of the condition.
Acute form
In acute pathology, the clinical picture progresses rapidly; vascular insufficiency is observed as a result of a sharp depletion of the riverbed. With the onset of blood loss, the following is noted:
- hypotension,
- dizziness and tinnitus,
- tachycardia and shortness of breath,
- pallor of the skin and mucous membranes,
- severe weakness and dry mouth,
- cold sweat,
- nausea.
If there is damage to the gastrointestinal tract, the stool becomes dark in color and the temperature may rise.
If blood loss is significant, hemorrhagic collapse develops. The pressure drops sharply to critical levels - thread-like pulse, shallow and rapid breathing. Muscle weakness is observed up to the cessation of motor activity, vomiting, convulsions and loss of consciousness are possible. Lack of blood supply causes oxygen starvation in organs and systems, death occurs due to respiratory and cardiac arrest.
Chronic form
If posthemorrhagic anemia develops slowly, the symptoms are not so pronounced, since adaptation mechanisms are activated. Signs of the chronic form resemble IDA, since minor bleeding leads to iron deficiency:
- dry skin and painful pallor,
- face is swollen
- hair loss and dullness,
- brittleness and thickening of the nail plate,
- increased fatigue and dizziness,
- heart rhythm disturbance,
- sweating
When the hemoglobin concentration drops to 70 g/l or lower, some patients experience low-grade fever. Patients complain of a feeling of numbness and changes in taste preferences. The severe stage is often accompanied by stomatitis and rapidly developing caries.
Stages (degrees) of the disease: mild, moderate, severe
Depending on the intensity of blood loss, there are several stages, or degrees of severity, of posthemorrhagic anemia.
Determining the severity of the disease plays a critical role in planning further treatment. For example, mild anemia may not require drug therapy, while severe anemia is an absolute indication for immediate hospitalization of the victim.
Stages of posthemorrhagic anemia - table
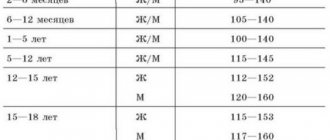
| Degree/Stage | Hemoglobin content in blood, gram/l. | Pulse rate, beats/min. | Systolic (upper) blood pressure, mmHg. |
| Light | 90 and above | Up to 80 | Above 110 |
| Average | 70–90 | 80–100 | 90–110 |
| Heavy | Less than 70 | More than 100 | Below 90 |
Diagnostic methods
When making a diagnosis of posthemorrhagic anemia, the basis of measures includes studying the patient’s medical history, a set of laboratory and instrumental studies. To identify the cause of anemia, you will need to consult a surgeon, hematologist, gastroenterologist or gynecologist. As a basic examination and to clarify the duration of blood loss, tests are carried out to determine the degree of anemia, a blood test is taken:
- General. Indicates a decrease in erythrocyte mass, their hemoglobin saturation, and platelet volume.
- Biochemical. The hemogram gives a detailed idea of the blood elements, their morphology and ratio to the volume of fluid. The study determines an increase in manganese, the enzyme alanine aminotransferase, a decrease in calcium and copper.
Urinalysis gives an initial idea of the state of the urinary system and the functioning of the body. To diagnose the site of internal bleeding, examination methods are used:
- Stool is collected to detect parasitic infestation and occult blood.
- Fibrogastroscopy is required to find out whether bleeding is present in the gastrointestinal tract due to an ulcer or a disintegrating tumor.
- Colonoscopy is an examination of the surface of the colon from the inside, allowing to detect a violation of the integrity of the mucosa.
- Bleeding of hemorrhoids and fissures in the rectum is detected using sigmoidoscopy.
- A chest x-ray is performed to detect traumatic injuries and hemorrhages in the lungs and esophageal-aortic region.
- Ultrasound of the abdominal cavity and organs located in the pelvis reveals the accumulation of blood due to injuries. In women, the method diagnoses rupture of the fallopian tubes during ectopic pregnancy and the condition of the uterus during vaginal bleeding.
- Electrocardiography shows the degree of disturbances in the functioning of the heart associated with lack of blood and hypoxia.
- For women, a gynecological examination is required.
Bone marrow examination is carried out in complex cases when the cause of anemia cannot be identified by conventional methods. Puncture samples taken show the activity of the red brain, trephine biopsy reveals the replacement of hematopoietic cells with adipose tissue.
Types of posthemorrhagic anemia
Anemia from blood loss, or posthemorrhagic anemia, is a deficiency of red blood cells in the plasma resulting from excessive blood loss. In clinical practice, two forms of the disease are known: acute and chronic. The first develops with a single injury to the body, causing rapid loss of a large volume of blood. The reasons for this condition may be:
- phlebeurysm;
- ectopic pregnancy;
- hemophilia;
- pulmonary infarction;
- coagulopathy;
- leukemia;
- extensive injuries;
- tumor formations;
- parasitic diseases;
- consequences of surgical interventions;
- severe forms of pulmonary tuberculosis;
- ulcers of the digestive tract.
Leukemia is one of the causes of anemia
Chronic anemia is possible with small but frequent blood losses, leading to a gradual decrease in the number of circulating red blood cells. The causes of the pathology coincide with those in an acute condition, but differ in the less intense impact on the body.
One of the main reasons for the wide spread of posthemorrhagic anemia in the recent past was the fashion for bloodletting. According to the latest data, it was this procedure that accelerated the death of Mozart. Having fallen ill in 1791, the composer was subjected to a treatment that was innovative at that time, as a result of which he lost about two liters of blood and died in less than a month.
Treatment with drugs and folk remedies
For posthemorrhagic anemia, the main goals of treatment are to identify the source of blood loss and stop the bleeding. For external injuries, apply a tourniquet and bandage. If necessary, vessels and damaged tissues and organs are sutured and resection is performed.
In case of massive blood loss, measures are carried out in the hospital:
- To restore blood supply and hemodynamics, a transfusion of canned blood and plasma is performed. When hemoglobin is below 8%, plasma substitutes are used: “Hemodez”, “Polyglyukin” or “Reopoliglyukin”. The blood transfusion procedure is carried out promptly, since a quarter of the blood loss is fraught with the death of the patient. The volume of infused fluid in this case exceeds blood loss by a maximum of 30%.
- Transfusion of red blood cells is necessary to restore oxygen transport; with rapid loss, its amount can be half a liter.
- Shock is treated with Prednisolone.
- To restore the acid-base balance during treatment, electrolyte and protein compounds are administered intravenously: albumin, glucose, saline.
- Iron is replenished by such drugs as Ferroplex, Feramide, Conferon, Sorbifer Durules. They are taken orally or by injection.
- Microelements are prescribed: cobalt, copper and manganese, as they increase the absorption of iron.
For prolonged bleeding:
- In the case of severe chronic anemia, transfusion is carried out in a small volume.
- To eliminate the symptoms of functional disorders in the heart, liver, and kidneys, therapeutic measures are used.
- For better absorption of Fe, iron-containing products, vitamins C and B groups are prescribed.
- Sometimes surgery is recommended.
The regimen and duration of drug treatment are individual in each specific case. Restoration of the normal picture is observed after one and a half or two months, but the patient takes the medicine for up to six months.
Classification of the disease
There are 2 types of posthemorrhagic anemia:
Acute red cell deficiency involves a sharp decrease in hemoglobin. This form of posthemorrhagic anemia occurs due to blood loss due to trauma or surgery, when a person loses 1/8 or more of the total volume.
Stages of development of the acute form
Doctors distinguish several stages in the development of acute posthemorrhagic anemia:
- Reflex-vascular stage. It is accompanied by the following status indicators:
- decreased blood pressure;
- pallor of the skin and mucous membranes;
- rapid heartbeat;
- spasm of peripheral vessels;
- lack of oxygen;
- removal of plasma from vital organs;
- compensatory return of blood to the heart.
- The hydremic stage occurs 3–6 hours after the start of bleeding and lasts 2–3 days. This happens:
- the flow of fluid from the interstitial areas into the blood vessels;
- increased synthesis of the hormone aldosterone, responsible for fluid retention in the body;
- stimulation of water retention in the body;
- plasma dilution;
- decreased levels of hemoglobin and red blood cells.
- The bone marrow stage (iron deficiency) occurs with progressive bleeding after 4–5 days. At this stage there are:
- insufficient oxygen supply to tissues;
- growth of reticulocytes (young forms of red blood cells) with a low hemoglobin content.
Features of chronic posthemorrhagic anemia
In chronic anemia, there is a small but periodically constant loss of blood over a long period of time. This form is observed in a number of diseases:
- oncology and neoplasms of the gastrointestinal tract;
- peptic ulcer;
- bleeding from varicose hemorrhoidal veins of the rectum;
- erosive processes in the mucous membrane of the esophagus;
- increased bleeding of gums (periodontitis and gingivitis).
Diet and traditional treatment
To restore the body after treatment of posthemorrhagic anemia and replenish hemoglobin, a specific diet is used. Its goal is to provide the body with vitamins and elements, so nutrition should be balanced and high in calories, but with a minimum amount of fat.
- The patient's diet requires the presence of foods containing iron, such as lean meat and liver.
- For enrichment with microelements, valuable amino acids and protein, fish, cottage cheese, and eggs are recommended.
- Suppliers of vitamins are vegetables and fruits, natural juices.
Loss of fluid is replenished by consuming water (at least 2 liters per day). To restore strength and support the body, you can also use folk recipes:
- Rose hips are brewed and drunk instead of tea; you can add strawberry leaves.
- When you lose strength, mix honey (200 ml), Cahors (300 ml) and aloe juice (150 ml). Take a spoon before meals.
- Mix 30 g of chicory juice in a glass of milk and drink it a day.
- Squeeze the juice from radishes, beets and carrots (1:1:1), pour into a dark glass container, cover with a lid and simmer in the oven for 3 hours. The liquid is drunk on a spoon before meals for a course of 3 months.
When blood loss occurs, the immune defense suffers and the body becomes susceptible to infection, so infusions or decoctions based on echinacea, ginseng, lemongrass or marshmallow will help to strengthen and restore the system.
Stages of pathology development
The pathogenesis of the acute clinical form is characterized by the manifestation of 3 stages of anemia:
- The first stage is vascular reflex. At this stage, the body's defense mechanisms are activated, accompanied by the opening of anastomoses. At the same time, blood pressure decreases significantly, shortness of breath appears, heart rhythm is disturbed, and the skin turns pale.
- The second stage is hydremia. The composition of the plasma changes, the vessels are filled with fluid coming from the cell tissues. The concentration of red blood cells and hemoglobin in the blood decreases significantly.
- The third stage is changes in the bone marrow. Characteristic disturbances occur on days 3–5. Iron levels are exceptionally low. This situation requires long-term treatment - up to three months.
The chronic form develops over a long period - from several weeks to a year or more. It is rightfully classified as an iron deficiency manifestation of pathology. Symptoms differ significantly from those of acute anemia.
Among the most expressive signs:
- dry and pale skin;
- swelling;
- dull hair, brittle nail plates;
- active sweating, indicating weakness;
- increased heart rate;
- borderline temperature (37 °C).
The lack of timely therapeutic measures to eliminate prolonged bleeding leads to depletion of the body's compensatory forces, as a result of which the preconditions for hemorrhagic shock develop.