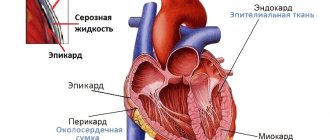
The heart is one of the vital organs of the human body. Only well-functioning work and structural features of the organ make it possible to fully provide nutrition to the tissues of organs and systems. The organ is a muscle consisting of three layers: endocardium, myocardium, epicardium. The first and last are thin layers covering the myocardium (a group of striated muscle fibers) on the inner and outer sides. The heart has four chambers, including the left and right ventricles, as well as the left and right atria. Each camera performs its own significant functions. They are separated from each other by the right ventricular and interatrial septa. There are valves that prevent blood from flowing back. The complex anatomical structure allows for continuous pumping of blood, delivering nutrition to all organs and systems of the human body.
LIST OF ABBREVIATIONS
AVU - atrioventricular node
GB - hypertension
https://www.youtube.com/watch?v=66wJNSCiNps
GI - ventricular index
IHD - coronary heart disease
ICM—myocardial blood supply index
LVI - left ventricular index
RVI - right ventricular index
IF - Fulton index
IEF - epicardial fat index
L - mass of the free wall of the left ventricle
LV - left ventricle
LOA - left circumflex artery
LPS - left atrium
MK - mitral valve
MP—mass of the interventricular septum
IAS - interatrial septum
MS - heart mass
ORP - volume-weight indicator
OVPL - volume-weight indicator of the left ventricle
OVPP - volume-weight indicator of the right ventricle
P - mass of the free wall of the right ventricle
PA - right heart artery
RV - right ventricle
LAD - anterior interventricular artery
MVP - mitral valve prolapse
RSA - right atrium
RVHS - separate weighing of parts of the heart
ROBL - left ventricular reserve volume
RVV - right ventricular reserve volume
SAU - sinoauricular node
SI - cardiac index
TC - tricuspid valve
FC - fibrous ring
NMR - net heart mass
EF - epicardial fat
EIT - electric pulse therapy
L - perimeter of the coronary artery
S—total area of the lumen of the arteries of the heart
Right atrium: description, normal performance, diagnosis and treatment of diseases
The human heart is represented by four chambers: atria and ventricles (right and left). The side walls of the cavities form the characteristic outlines of the organ on x-ray photographs. The right atrium (RA) is the smallest chamber located at the base (top) of the heart. The RA cavity is connected to the right ventricle through the atrioventricular junction and the tricuspid valve. The coronary groove serves as the boundary between the departments on the outer surface, which is poorly visualized due to the massiveness of the pericardium (the pericardial sac).
The atrium cavity is not designed for a large one-time volume of blood, so the thickness of the walls is 2-3 mm (five times less than that of the ventricle). A sufficient number of muscle fibers and the functionality of the valves avoid overload.
The anatomical structure of the right atrium is represented by a hexagonal cubic chamber. Characteristics of the main landmarks and elements of each of the walls are in the table:
- The openings of the upper and lower PV are at the boundaries with the front and rear walls.
- The Lover's mound is located between the points of confluence of blood vessels. In the prenatal period, the formation serves as a valve that regulates the direction of flow.
- Under the opening of the lower PV is the Eustachian valve (tissue protrusion), which extends to the edge of the fossa oval in the form of a Chiari network (plates with fenestrae - “holes”)
Vessels of the right atrium
Cardiomyocytes of the RA are supplied with blood by the right coronary artery, which starts from the aortic sinus and lies in the designated coronal sulcus. Along the way, the vessel gives off branches:
- to the sinoatrial node (the main pacemaker of the heart);
- atrial (2-6), which supply the ear and nearby tissues;
- intermediate branch (nourishes the bulk of the myocardium).
The outflow of venous blood from the myocardium of the right atrium occurs in two ways:
- Through the coronary veins, the fluid enters the coronary sinus of the left part of the diaphragmatic surface of the heart. The length of the sinus is 2-3 cm and opens into the cavity of the RA at the confluence of the inferior vena cava.
- Direct outflow from small-caliber vessels (the group of “right atrial veins” of Viessen-Tibizia) into the chamber cavity.
The lymphatic system of the right heart is represented by three networks:
- deep (subendothelial);
- intermediate (myocardial);
- superficial (subepicardial).
The spent lymph from the local system enters large vessels, on the way of which there are regional nodes.
Histology
The collection of venous blood from the entire body and its direction into the pulmonary circulation requires a specific structure of the walls of the right atrium. The histological structure of the PP is presented in the table:
- the inner protective lining of the heart;
- smooth surface prevents thrombus formation;
- formation of the tricuspid valve (from the connective tissue plate) in the area of the atrioventricular opening
- contractile function at the time of myocardial systole;
- secretion of natriuretic peptide (a hormone responsible for the excretion of sodium from the body in urine)
- separation of the heart from the pericardial cavity;
- synthesis of pericardial fluid for easy sliding of the chamber in the cavity of the pericardial sac
All chambers of the heart are enclosed in an external cavity formation of connective tissue - the pericardium (pericardial sac).
1Important diagnostic method
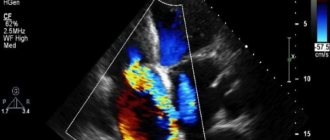
Ultrasound examination of the heart
Echocardiographic examination of the cardiovascular system is a very important and also quite accessible diagnostic method. In some cases, the method is the “gold standard”, allowing one or another diagnosis to be verified. In addition, the method makes it possible to identify hidden heart failure that does not manifest itself during intense physical activity.
Clinical and morphological classification of pericardial diseases
The examination of the heart begins with an assessment of the pericardium, which consists of two layers: fibrous, which passes into the adventitia of large vessels, and serous. The serous is divided into parietal, adjacent to the fibrous, and visceral (epicardium), forming a pericardial cavity containing 30-75 ml of clear yellowish fluid.
The pericardium is tightly fused to the tendon center of the diaphragm. On the lateral sides the pericardium borders on the pleura; behind – with the descending aorta, esophagus, spine; in front - with the sternum and ribs.
There are oblique and transverse sinuses of the pericardium (Fig. 2, 3). The oblique sinus (sinus obliquus Halleri) is located between the right and left pulmonary veins, the posterior surface of the left atrium and the posterior wall of the pericardium. The transverse sinus (sinus transversus pericardii) is formed in front by the pulmonary artery and aorta, behind by the inferior vena cava and atria, and above by the pericardium. It is open on the right and left.
The outer layer of the pericardium is supplied with blood by the internal thoracic (mainly from a. pericardiacophrenicae), superior phrenic, intercostal, bronchial and mediastinal arteries, in the anterior fold of the pericardium, in the area of entry and exit of large vessels, anastomosing with the system of coronary arteries supplying the epicardium. In critical situations, these anastomoses create additional blood supply to the myocardium.
Venous outflow is carried out through the veins accompanying the arteries of the same name.
The outflow of lymph from the pericardium goes to the upper anterior mediastinal, sternal, diaphragmatic, bronchopulmonary and paraesophageal lymph nodes.
When pathological changes in the pericardium are detected, from our point of view, it is advisable to use the clinical and morphological classification of E.E. Gogin (1979) (see Table 1). The most common pathology of the pericardium is fibrinous pericarditis, which occurs in rheumatism and other collagen diseases, tuberculosis, uremia, in acute myocardial infarction, as a component of Dressler's syndrome, in cardiac trauma, including surgery.
In the last three conditions, the presence of pericarditis is considered as an autoimmune reaction: in acute myocardial infarction - to necrosis of muscle fibers (Dressler's syndrome), during surgery, trauma - to blood in the pericardial cavity, damage to the integrity of the pericardium (postpericardiotomy pericarditis).
Table 1
(according to E.E. Gogin)
I. Pericarditis
The left atrium (LA) is an anatomical section (chamber) of the heart that receives arterial blood from the pulmonary veins and pumps it into the left ventricle. Pathological abnormalities that develop in the LA are the basis for some common diseases. The resulting disturbances change blood circulation parameters and significantly affect the quality and duration of people’s lives.
The structure of the left atrium, like the right, is similar to an irregular cube.
Chamber walls:
- The anterior one protrudes and forms the left ear, which is adjacent to the pulmonary trunk on the left.
- Rear.
- Upper.
- Internal - takes part in the formation of the interatrial septum. It has a thinner part that corresponds to the oval fossa.
- The lower one forms the basis of the left ventricle.
- Outdoor.
The LA wall is thinner than the right one. The inner surface of the auricle is lined with pectineus muscles, the rest of the atrium is smooth.
Four pulmonary veins drain into the LA (two from each lung):
- Top right.
- Bottom right.
- Top left.
- Bottom left.
They carry arterial blood from the lungs. The openings of these veins are located on the posterior wall of the left atrium and do not have valves.
Function
Main functions of the left atrium:
- Depositing. The chamber is a container that receives blood from the pulmonary veins.
- According to the pressure gradient, it conducts blood into the left ventricle after the mitral valve opens.
- Helps complete filling of the left ventricle through its contraction.
- When the atrium walls stretch, the pressure rises, which stimulates the formation of natriuretic peptide (NUP). The biologically active substance reduces circulating blood volume and blood pressure. It has been proven that NUP prevents the development of cardiac hypertrophy.
- There are many baro- and mechanoreceptors located in the LA. The former respond to an increase in central venous pressure, which in turn leads to the activation of the latter, which contribute to the development of tachycardia (accelerated heartbeat).
Camera parameters are measured using echocardiography (EchoCG), a non-invasive ultrasound research method.
Normal dimensions of the left atrium in adults:
- cavity size – 8-40 mm;
- anterior-posterior – 1.3-3.7 cm;
- width: front – 1.2-3.1 cm, back – 1.4-3.3 cm;
- height – 1.5-3.9 cm;
- wall thickness – 1.5-2 mm;
- thickness of the interatrial septum – 0.7-1.2 cm;
- weight – 15-25 g (5.6-9.2% of the total).
The volume of the cavity (the amount of blood that fits in the atrium) is 110-130 cm3.
Blood pressure: 2-4 mm Hg. Art. in diastole and 9-12 mm Hg. Art. at systole.
In addition, the adequacy of filling with blood from the pulmonary veins, the uniformity of contraction of muscle fibers of all walls and the direction of blood flow in different phases of the cycle are assessed.
The main methods that can be used to determine the condition of the left atrium include: electrocardiography (ECG) and echocardiography (EchoCG).
The function of the left atrium on the ECG is assessed by the P wave in leads I, II, aVL, V5, V6.
This method allows you to see:
- Atrial hypertrophy (thickening of the walls). Signs on the cardiogram: increased height and bifurcation of P in I, II, aVL, V5, V6 (the so-called “P - mitrale” - raising the second part of the tooth); negative or biphasic P, P duration is more than 0.1 s.
Hypertrophy is the basis for the occurrence of atrial fibrillation (fibrillation). On the ECG it is expressed by: absence of the P wave, the presence of chaotic f-waves (especially in II, III, aVF, V1, V2), irregular ventricular rhythm.In addition, the proliferation of muscle fibers contributes to the appearance of sinus tachycardia - an increase in the number of impulses arising in the sinoatrial node. On the ECG, the P wave is normal, the RR distance is shortened.
- Atrial dilatation (an increase in the size of the cavity against the background of a thinning of the wall) can be suspected using an electrocardiogram only in the presence of arrhythmias.
EchoCG signs
EchoCG or ultrasound (ultrasound) determines the size and performance of the left atrium, which makes it possible to diagnose hypertrophy and dilatation of this section.
The method is used to diagnose coarctation of the aorta, mitral and aortic valve defects, cardiac tumors (myxomas), the presence of which affects the size and function of the left atrium.
Signs of dysfunction of the left atrium are called overload (hyperfunction). The condition is based on hemodynamic tension of the walls by resistance or volume.
Prolonged load on the muscle mass of the myocardium of the chamber first causes hypertrophy of the fibers. However, depletion of energy reserves and progression of pathology contribute to muscle atrophy, and the atrium begins to dilate.
Characteristic clinical symptoms:
- fatigue;
- dyspnea;
- interruptions in heart function;
- pain in the heart area;
- decreased endurance to physical activity.
Acute conditions Long-term diseases
|
|
ECG signs of overload: increased height and duration of P (mostly its second phase) in V1, V2, sometimes negative P in V1.
LA overload most often leads to its hypertrophy or dilatation. During an objective examination (using percussion), pathology can be suspected by the upward displacement of the upper border of the heart.
Treatment always depends on what pathology led to overload and, as a consequence, to hypertrophy or dilatation. If we are talking about acute conditions, then they are treated by doctors according to emergency care protocols in each case. Long-term, chronic diseases are treated with lifelong medication, and many require surgical intervention.
If the above conditions are not treated, there is a high risk of a number of dangerous complications:
- severe heart failure;
- cardiac asthma;
- atrial fibrillation.
conclusions
The left atrium is the part of the heart that is often susceptible to pathological changes. They, in turn, lead to very serious diseases with complications and rhythm disturbances.
For example, atrial fibrillation is the leading cause of ischemic strokes.
Therefore, if during a routine examination a patient is found to have LA overload or hypertrophy, further detailed diagnostics are recommended.
The following sources of information were used to prepare the material.
Which Vessels Enter the Right and Left Atrium
The heart is the center of a closed cardiovascular system, pumping blood through the vessels. Its work allows it to provide cells with oxygen and nutrients, remove carbon dioxide and metabolic products from them, and also respond to damage, inflammatory processes and the penetration of bacteria, viruses and other microorganisms.
Some vessels flow into the right atrium, others into the left. Thus, all the venous (waste) and oxygenated arterial blood in the lungs enters the heart.
The human heart is a 4-chamber “pump” of 2 atria and 2 ventricles
Blood is pushed out from the other 2 chambers of the heart - the ventricles. Venous blood goes to the pulmonary lobes along the pulmonary trunk from the right ventricle, and oxygenated arterial blood from the left ventricle enters the aorta.
In this article, we will briefly consider which vessels enter the left atrium and what flows into the right atrium. In fact, we will talk about the end of the systemic and pulmonary circulation of the human cardiovascular system.
The functions of the first circle are listed in the introduction above, but the small closed circle between the heart and lungs, in addition to heat transfer, faces only one global task - gas exchange: freeing the blood from carbon dioxide and saturating it with oxygen.
Vessels draining into the atria of the heart
Vessels flow into the right atrium, through which venous blood flows with a high content of CO2 and waste. They close the large circle of blood circulation.
There are two such veins:
- Inferior vena cava . It is the largest venous vessel, which is often called the venous trunk. “Waste” blood from the legs, tissues and organs located in the pelvis and abdomen is collected here.
- Superior vena cava . It is a short trunk formed by two brachiocephalic venous vessels. It opens with an orifice into the right atrial chamber at the level of the third right rib. Venous blood from the arms, head, tissues and organs of the chest flows here.
The thickness of the upper and lower hollow venous vessels flowing into the heart is different, since they experience different loads. In addition, there are gender differences in the topographic and anatomical characteristics of the thickness of their walls.
For your information. Histological maturity of the tissue of the walls of the inferior and superior vena cava occurs at the age of 10, and starting from the age of 70, there is a gradual reduction in the number and atrophy of circularly located smooth muscle cells.
By the way, answering the question: “What vessels flow into the right atrium?” – we should remember the lymphatic system. Its ducts connect into trunks, which open into veins located near the clavicular bones.
Thus, venous blood flowing in the area between the mouths of the lymphatic trunks and the superior vena cava has the highest degree of bactericidal activity.
Veins draining into the atria of the heart
Paired vessels flow into the left atrium, closing the pulmonary circulation:
- The two left (superior and inferior) pulmonary veins drain oxygenated blood into the left atrium. Their mouths are located vertically, one above the other, and are located in the left posterolateral region of the wall of the atrial chamber. The upper vessel collects blood from the upper lobe of the left lung, and the lower left pulmonary vein, respectively, from the lower lobe of the left lung.
- The two right (superior and inferior) pulmonary veins drain blood into the left atrial chamber of the heart from the right lung. The length of these vessels is greater than that of the left pulmonary veins, since before they enter the posterior wall of the left atrium near the interatrial septum, they still pass through the thickness of the posterior wall of the right atrium (pictured below).
The thickness of the walls of the vessels that flow into the left atrium is almost the same in men and women. However, there are also differences. The thickness of the wall between the orifices and the diameter of the superior venous vessel are greater in women, and the diameters of both inferior pulmonary veins are greater in men.
Location of the pulmonary veins
We also note that during intrauterine development the pulmonary circulation does not work. Oxygen-enriched blood comes from the mother through the umbilical vein and is drained through the umbilical arteries of the placenta.
The pulmonary circulation, starting with the pulmonary column and ending with the pulmonary veins, begins to function immediately after birth, as soon as the baby takes his first breath.
Congenital defects
The most common anomalies in the development of blood vessels flowing into the atria of the heart are:
- The presence of 2 hollow superior or 2 hollow inferior veins, instead of one. It is rare, but the location of the inferior vena cava to the right of the spine occurs. Typically, these defects do not affect health and do not require surgical correction.
- Anomalous pulmonary venous drainage (APVD). This pathology is an unnatural entry of these vessels not into the left, but into the right atrium, which occurs in various combinations. The total proportion of such anomalies is 3% of all congenital heart defects. These defects require surgical treatment. The type of operation and timing depend on the type of ADLV (see below).
To diagnose ADLV, the doctor will prescribe a set of examinations, including: ECG, echocardiography, MRI, CT, atrio- and ventriculography, as well as many other instrumental studies.
Options for partial and one of the total (in the center) anomalous pulmonary vein drainages
ADLV can be partial or complete (total). In the first case, 1 or 2 pulmonary veins flow into the right atrium instead of the left one and, in most cases, such an anomaly is accompanied by an atrial septal defect.
Partial ADLV causes cyanosis, shortness of breath, frequent pneumonia, weakness, pain in the heart, and retarded physical development. The pathology requires surgery according to indications.
Patients with ADPV can live up to 30 years before dying due to cardiac arrest due to heart failure or pulmonary infection.
For your information. In addition to atrial or ventricular septal defect, ADLV is often accompanied by other developmental defects. Among them: tetrado of Fallot, coarctation of the aorta, Turkish saber syndrome, truncus arteriosus, abnormalities in the development of the gastrointestinal tract and genitourinary system.
Total ADPV are congenital pathologies in which all 4 pulmonary venous vessels open separately not into the left atrium, but into the right atrium. Often there are options when they all connect into one common collector vessel, flowing either into the coronary sinus, or into the superior or inferior vena cava.
Children with total ADLV defects are born full-term, and the body, although with difficulty, copes with this situation for several days (months). However, the health condition is critical from the very first day, and it is necessary to perform reconstructive surgery as quickly as possible.
Diseases
Among the pathologies of vessels flowing into the atria acquired during life, the most common are:
- obstruction of the upper or lower hollow venous vessels flowing into the right atrial chamber, caused by thrombosis or a tumor process;
- pulmonary vein stenosis;
- obliterating endarteritis of the pulmonary venous vessels.
All these diseases cannot be treated conservatively and require surgical intervention.
And as a conclusion, we suggest watching a video that tells in more detail about the largest vein in the human body, the Inferior Vena Cava, which flows into the right atrium.
Source: https://Cardio-help.ru/anatomiya/vpadayut-v-pravoe-predserdie-688
2Ejection fraction
Healthy ejection fraction and pathological (less than 45%)
Ejection fraction (EF) has important diagnostic value, as it allows assessing the systolic function of the LV and right ventricles. Ejection fraction is the percentage of blood volume that is expelled into the vessels from the right and left ventricles during systole. If, for example, from 100 ml of blood 65 ml of blood entered the vessels, as a percentage this will be 65%.
Left ventricle. The normal left ventricular ejection fraction for men is ≥ 52%, for women – ≥ 54%. In addition to the LV ejection fraction, the LV shortening fraction is also determined, which reflects the state of its pumping (contractile) function. The norm for the shortening fraction (SF) of the left ventricle is ≥ 25%.
Right ventricle. The normal ejection fraction for the right ventricle (RV) is ≥ 45%.
3Sizes of heart chambers
Chambers of the heart
The dimensions of the heart chambers are a parameter that is determined in order to exclude or confirm overload of the atria or ventricles.
Left atrium. The normal left atrium (LA) diameter in mm for men is ≤ 40, for women ≤ 38. An increase in the diameter of the left atrium may indicate heart failure in the patient. In addition to the LA diameter, its volume is also measured. The normal LA volume in mm3 for men is ≤ 58, for women ≤ 52. LA size increases with cardiomyopathies, mitral valve defects, arrhythmias (heart rhythm disturbances), and congenital heart defects.
Right atrium. For the right atrium (RA), as well as for the left atrium, the dimensions (diameter and volume) are determined by echocardiography. Normally, the diameter of the PP is ≤ 44 mm. Right atrium volume is divided by body surface area (BSA). For men, the normal ratio of PP/PPT volume is ≤ 39 ml/m2, for women - ≤33 ml/m2.
ECHO Cardiography (ultrasound of the heart)
Left ventricle. The ventricles have their own parameters regarding their sizes. Since the practicing physician is interested in the functional state of the ventricles in systole and diastole, there are corresponding indicators. Main size indicators for the left ventricle:
- Diastolic size in mm (men) - ≤ 58, women - ≤ 52;
- Diastolic size/PPT (men) - ≤ 30 mm/m2, women - ≤ 31 mm/m2;
- End-diastolic volume (men) - ≤ 150 ml, women - ≤ 106 ml;
- End-diastolic volume/BSA (men) - ≤ 74 ml/m2, women - ≤61 ml/m2;
- Systolic size in mm (men) - ≤ 40, women - ≤ 35;
- End systolic volume (men) - ≤ 61 ml, women - ≤ 42 ml;
- End-systolic volume/BSA (men) - ≤ 31 ml/m2, women - ≤ 24 ml/m2;
Indicators of diastolic and systolic volume and size may increase with myocardial diseases, heart failure, as well as with congenital and acquired heart defects.Myocardial mass indicators
- LV myocardium (heart muscle) mass (men) - ≤ 224 g, women - ≤ 162 g;
- Myocardial mass of the LV/ASA (men) - ≤ 115 g/m2; women - ≤95 g/m2;
- Thickness of the posterior wall of the LV in mm (men) - ≤ 10, women - ≤ 9;
The mass of the LV myocardium may increase as its walls thicken (hypertrophy). The cause of hypertrophy can be various diseases of the cardiovascular system: arterial hypertension, mitral and aortic valve defects, hypertrophic cardiomyopathy.
Right ventricle. Basal diameter - ≤ 41 mm; End diastolic volume (EDV) RV/APT (men) ≤ 87 ml/m2, women ≤ 74 ml/m2; End systolic volume (ESV) RV/APT (men) - ≤ 44 ml/m2 , women - 36 ml/m2; Pancreatic wall thickness - ≤ 5 mm.
Interventricular septum. The thickness of the IVS in men in mm is ≤ 10, in women – ≤ 9;
Left and right atrium: structure and openings of the atria
Right atrial hypertrophy (RAH) is the term for enlargement of this part of the heart. Let us recall that venous blood, collected in large vessels from throughout the body, enters the right atrium. The right atrium communicates with the right ventricle.
Between the atrium and the ventricle is a tricuspid valve, which prevents blood from flowing back from the ventricle into the atrium. From the right ventricle, venous blood enters the pulmonary circulation through the pulmonary artery, where it is enriched with oxygen, and then enters the right side of the heart and from there to the aorta.
HPP manifests itself as thickening of the wall of the right atrium, and then expansion of its cavity. It occurs when the atrium is overloaded with blood pressure or volume.
In this article we will introduce the reader to the causes, main symptoms and principles of diagnosing right atrial hypertrophy.
Causes
Congenital malformations such as tetralogy of Fallot can lead to right atrial hypertrophy.
Right atrium pressure overload is characteristic of tricuspid valve stenosis. This is an acquired heart defect, in which the area of the opening between the atrium and the ventricle decreases. Tricuspid valve stenosis may be due to endocarditis.
With another acquired heart defect, tricuspid valve insufficiency, the right atrium experiences volume overload. In this condition, blood from the right ventricle, when it contracts, flows not only into the pulmonary artery, but also back into the right atrium, causing it to work under overload.
The right atrium is enlarged in some congenital heart defects. For example, with a significant atrial septal defect, blood from the left atrium enters not only the left ventricle, but also through the defect into the right atrium, causing its overload.
Congenital heart defects accompanied by the development of HPP in children - Ebstein's anomaly, tetralogy of Fallot, transposition of the great vessels and others. Right atrium overload can occur quickly and manifest primarily on the electrocardiogram.
This condition can occur during an attack of bronchial asthma, pneumonia, myocardial infarction, or pulmonary embolism. Subsequently, with recovery, the signs of HPP gradually disappear.
Sometimes electrocardiographic signs of HPP appear when the heart rate increases, for example, against the background of hyperthyroidism. In thin people, electrocardiographic signs of HPP may be normal.
Symptoms and complications
GPP itself does not cause any symptoms. The patient is only concerned about signs associated with the underlying disease. When chronic pulmonary heart disease develops, this may include shortness of breath with light exertion and at rest, especially when lying down, coughing at night, and hemoptysis.
If the right atrium ceases to cope with the increased load, signs of circulatory failure in a large circle appear, associated with stagnation of venous blood in the body. These are symptoms such as heaviness in the right hypochondrium, an increase in the size of the abdomen, swelling of the legs and anterior abdominal wall, the appearance of dilated veins in the abdomen and others.
Source: https://cordiacardio.ru/aritmii/uvelichenie-pravogo-predserdiya.html
EPICARDIAL FATTY FIBER
Epicardial fatty tissue (EF) is more pronounced above the right ventricle, along the coronary sulcus. Normally, the mass of the EF in men is up to 38.3 g, in women – up to 33 g, depending on gender, age, body weight and pathology. A more accurate criterion for cardiac obesity is the EJ index (IJE, A.M. Lifshits, 1979) - the ratio of fiber mass to heart mass (see.
application - a map of separate weighing of parts of the heart, RHF). The value of IEF in men is higher than 25%, and in women higher than 33% indicates cardiac obesity, usually with general obesity and dyshormonal myocardial dystrophies. Extreme degree of cardiac obesity – lipoma capsularae cordis. Among other diseases, IEL is statistically significantly higher in hypertensive patients. In addition, the mass of EF increases with age.
4Valves
Heart valves
To assess the condition of the valves in echocardiography, parameters such as valve area and mean pressure gradient are used.
- Aortic valve. Area - 2.5-4.5 cm2; average pressure gradient{amp}lt; 5 mmHg The area of the aortic valve decreases if stenosis develops. In severe aortic stenosis, the area of the aortic valve (AV) narrows to 1 cm2. The pressure gradient depends on the degree of narrowing of the AV, as well as on the blood flow through it. With the development of aortic stenosis, the average pressure gradient increases to 50 mmHg.
- Mitral valve (MV). Area - 4-6 cm2, average pressure gradient{amp}lt; 2 mmHg Transmitral flow E/e, -{amp}lt; 8, transmitral flow: E/A 1-2. Narrowing of the mitral valve opening indicates the development of stenosis. Transmitral flow in ultrasound diagnostics is used to assess the filling function of the LV and left atrium. Normally, transmitral flow is characterized by the presence of two waves - peak E (early phase of ventricular filling) and peak A (atrial systole). Using these indicators, left atrial filling pressure is calculated and the severity of diastolic dysfunction and the degree of increase in LV diastolic pressure are assessed.
Anatomy of the human heart. Simple and affordable
The heart is one of the most romantic and sensual organs of the human body. In many cultures, it is considered the seat of the soul, the place where affection and love are born. However, from an anatomical point of view, the picture looks more prosaic.
A healthy heart is a strong muscular organ about the size of its owner's fist. The work of the heart muscle does not stop for a second from the moment a person is born until death.
By pumping blood, the heart supplies oxygen to all organs and tissues, helps remove waste products and performs part of the body’s cleansing functions. Let's talk about the features of the anatomical structure of this amazing organ.
Anatomy of the human heart: historical and medical excursion
Cardiology, a science that studies the structure of the heart and blood vessels, was identified as a separate branch of anatomy back in 1628, when Harvey identified and presented to the medical community the laws of human circulation. He demonstrated how the heart, like a pump, pushes blood through the vascular bed in a strictly defined direction, supplying the organs with nutrients and oxygen.
The heart is located in the human thoracic region, slightly to the left of the central axis. The shape of the organ can vary depending on the individual structural features of the body, age, constitution, gender and other factors.
Thus, dense, short people have a more rounded heart than thin and tall people.
Its shape is believed to be approximately the circumference of a tightly clenched fist, and its weight ranges from 210 grams for women to 380 grams for men.
The volume of blood pumped by the heart muscle per day is approximately 7–10 thousand liters, and this work is carried out continuously! The amount of blood may vary due to physical and psychological conditions.
Under stress, when the body needs oxygen, the load on the heart increases significantly: at such moments it is able to move blood at a speed of up to 30 liters per minute, restoring the body’s reserves.
However, the organ is not able to constantly work for wear and tear: during moments of rest, blood flow slows down to 5 liters per minute, and the muscle cells that form the heart rest and recover.
Structure of the heart: anatomy of tissues and cells
The heart is classified as a muscular organ, however, it is a mistake to believe that it consists of muscle fibers alone. The heart wall includes three layers, each of which has its own characteristics:
1. Endocardium
- This is the inner shell lining the surface of the chambers. It is represented by a balanced symbiosis of elastic connective and smooth muscle cells.
It is almost impossible to outline clear boundaries of the endocardium: as it becomes thinner, it smoothly passes into the adjacent blood vessels, and in particularly thin places of the atria it fuses directly with the epicardium, bypassing the middle, most extensive layer - the myocardium.
2. Myocardium
- This is the muscular frame of the heart.
Several layers of striated muscle tissue are connected in such a way as to quickly and purposefully respond to excitation that arises in one area and passes through the entire organ, pushing blood into the vascular bed.
In addition to muscle cells, the myocardium includes P-cells capable of transmitting nerve impulses. The degree of myocardial development in individual areas depends on the scope of functions assigned to it. For example, the myocardium in the atria is much thinner than the ventricular myocardium.
In the same layer there is a fibrous ring, which anatomically separates the atria and ventricles. This feature allows the chambers to contract alternately, pushing blood in a strictly defined direction.
3. Epicard
- superficial layer of the heart wall. The serous membrane, formed by epithelial and connective tissue, is an intermediate link between the organ and the cardiac sac - the pericardium. The thin transparent structure protects the heart from increased friction and promotes the interaction of the muscle layer with adjacent tissues.
On the outside, the heart is surrounded by the pericardium, a mucous membrane otherwise called the cardiac sac. It consists of two leaves - the outer one, facing the diaphragm, and the inner one, tightly adjacent to the heart. Between them there is a fluid-filled cavity, which reduces friction during heart contractions.
Chambers and valves
The heart cavity is divided into 4 sections:
- right atrium and ventricle filled with venous blood;
- left atrium and ventricle with arterial blood.
The right and left halves are separated by a dense septum, which prevents the two types of blood from mixing and maintains one-way blood flow.
True, this feature has one small exception: in children in the womb, there is an oval window in the septum, through which blood mixes in the cavity of the heart.
Normally, by birth this hole is closed and the cardiovascular system functions as in an adult. Incomplete closure of the oval window is considered a serious pathology and requires surgical intervention.
Between the atria and ventricles, the mitral and tricuspid valves are located in pairs, which are held in place by tendon threads. Synchronous contraction of the valves ensures one-way blood flow, preventing the mixing of arterial and venous flow.
The largest artery of the bloodstream, the aorta, departs from the left ventricle, and the pulmonary trunk originates in the right ventricle. To ensure that blood moves exclusively in one direction, semilunar valves are located between the chambers of the heart and the arteries.
Blood flow is ensured by the venous network. The inferior vena cava flows into the right atrium, and the pulmonary veins, respectively, into the left.
Anatomical features of the human heart
Since the supply of oxygen and nutrients to other organs directly depends on the normal functioning of the heart, it must ideally adapt to changing environmental conditions, operating in a different frequency range. Such variability is possible due to the anatomical and physiological characteristics of the heart muscle:
- Autonomy implies complete independence from the central nervous system. The heart contracts from impulses produced by itself, so the work of the central nervous system does not affect the heart rate in any way.
- Conduction consists of transmitting the generated impulse along the chain to other parts and cells of the heart.
- Excitability implies an instant reaction to changes occurring in the body and outside it.
- Contractility, that is, the force of contraction of fibers, is directly proportional to their length.
- Refractoriness is a period during which myocardial tissue is inexcitable.
Any failure in this system can lead to a sharp and uncontrollable change in heart rate, asynchrony of heart contractions, even fibrillation and death.
Phases of the heart
To continuously move blood through the vessels, the heart must contract. Based on the stage of contraction, there are 3 phases of the cardiac cycle:
- Atrial systole, during which blood flows from the atria into the ventricles. In order not to interfere with the flow, the mitral and tricuspid valves open at this moment, and the semilunar valves, on the contrary, close.
- Ventricular systole involves the movement of blood further to the arteries through the open semilunar valves. At the same time, the flap valves close.
- Diastole involves filling the atria with venous blood through the open leaflet valves.
Each heartbeat lasts approximately one second, but during active physical work or during stress, the speed of impulses increases due to a reduction in the duration of diastole. During proper rest, sleep or meditation, heart contractions, on the contrary, slow down, diastole becomes longer, so the body is more actively cleansed of metabolites.
Anatomy of the coronary system
In order to fully perform its assigned functions, the heart must not only pump blood throughout the body, but also itself receive nutrients from the bloodstream.
The aortic system, which carries blood to the muscle fibers of the heart, is called the coronary system and includes two arteries - the left and the right.
Both of them depart from the aorta and, moving in the opposite direction, saturate the heart cells with useful substances and oxygen contained in the blood.
Conduction system of the heart muscle
Continuous contraction of the heart is achieved due to its autonomous operation. An electrical impulse that triggers the process of contraction of muscle fibers is generated in the sinus node of the right atrium with a frequency of 50–80 beats per minute.
It is transmitted along the nerve fibers of the atrioventricular node to the interventricular septum, then through large bundles (branch branches) to the walls of the ventricles, and then passes to smaller Purkinje nerve fibers.
Thanks to this, the heart muscle can contract progressively, pushing blood from the internal cavity into the vascular bed.
Lifestyle and heart health
The condition of the entire body directly depends on the full functioning of the heart, so the goal of any sane person is to maintain the health of the cardiovascular system. In order not to encounter cardiac pathologies, you should try to exclude or at least minimize provoking factors:
- being overweight;
- smoking, drinking alcohol and drugs;
- irrational diet, abuse of fatty, fried, salty foods;
- elevated cholesterol levels;
- inactive lifestyle;
- ultra-intense physical activity;
- a state of persistent stress, nervous exhaustion and overwork.
Knowing a little more about the anatomy of the human heart, try to make an effort to give up destructive habits. Change your life for the better, and then your heart will work like a clock.
Source: https://www.oum.ru/literature/anatomiya-cheloveka/anatomiya-serdtsa-cheloveka/
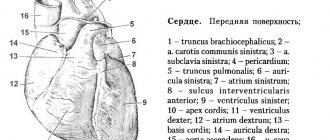
HEART SHAPE AND SIZES
Chambers of the heart
It is known that the shape of the heart depends on age, gender, body type and pathology. In newborns it is close to spherical, and by the age of 12 it approaches oval. In men and hypersthenics it is cone-shaped, in women and asthenics it is oval. In case of hypertension, aortic valve damage, pulmonary artery stenosis, the heart is cone-shaped. With stenosis of the atrioventricular orifices, the heart is oval and rounded due to the expansion of the atria.
When describing the heart, the following definitions of shape are used: 1 - conical, 2 - narrow-conical, 3 - wide-conical, 4 - blunt-conical, 5 - cylindrical, b - oval, 7 - spherical, flattened. (Fig. 4).
Palpation of the heart sometimes provides very valuable information, especially in the early stages of myocardial infarction and the presence of aneurysms. In ischemic zones, when it is still difficult to visually outline the focus, the elasticity of the myocardium has already been lost. The shape and size of the heart are uninformative compared to relative organometric indices (see below for separate weighing of parts of the heart - RVHS).
5Vessels
Blood vessels of the heart
Pulmonary artery. The diameter of the pulmonary artery (PA) is ≤ 21 mm, the acceleration time of the PA is ≥110 ms. A decrease in the lumen of the vessel indicates stenosis or pathological narrowing of the pulmonary artery. Systolic pressure ≤ 30 mm Hg, mean pressure ≤ 20-25 mm Hg; An increase in pressure in the pulmonary artery that exceeds acceptable limits indicates the presence of pulmonary hypertension.
Inferior vena cava. The diameter of the inferior vena cava (IVC) is ≤ 21 mm; An increase in the diameter of the inferior vena cava can be observed with a significant increase in the volume of the right atrium (RA) and a weakening of its contractile function. This condition can occur with narrowing of the right atrioventricular orifice and with tricuspid valve (TC) insufficiency.
More detailed information about the remaining valves, large vessels, and calculations of indicators can be found in other sources. Here are some of them that were missing above:
- Ejection fraction according to Simpson is the norm ≥ 45%, according to Teicholz - ≥ 55%. Simpson's method is used more often because it is more accurate. According to this method, the entire LV cavity is divided conditionally into a certain number of thin disks. The EchoCG operator makes measurements at the end of systole and diastole. The Teicholtz method for determining ejection fraction is simpler, but in the presence of asynergic zones in the LV, the obtained data on ejection fraction are inaccurate.
- The concept of normokinesis, hyperkinesis and hypokinesis. Such indicators are assessed by the amplitude of the interventricular septum and the posterior wall of the LV. Normally, fluctuations of the interventricular septum (IVS) are within the range of 0.5-0.8 cm, for the posterior wall of the LV - 0.9 - 1.4 cm. If the amplitude of movements is less than the indicated figures, they speak of hypokinesis. In the absence of movement - akinesis. There is also the concept of dyskinesia - wall movement with a negative sign. With hyperkinesis, indicators exceed normal values. Asynchronous movement of the LV walls may also occur, which often occurs with intraventricular conduction disorders, atrial fibrillation (AF), and an artificial pacemaker.
Importance of the right atrium
The human right atrium, due to its anatomical structure, allows for continuous blood flow after contraction of the ventricle. Achieved through the following aspects:
- There is a constant flow of venous blood, so the walls of the chamber are quite thin, which allows the organ to stretch and prevent the chamber from overflowing and increasing pressure;
- The walls of the right atrium have a thin layer of muscle tissue. This feature does not allow the chamber to contract completely, which also ensures transit flow of venous blood;
- The contraction, in turn, is very weak, which prevents the backflow of blood and does not interfere with its correct flow;
- Continuous circulation is also ensured due to the absence of inlet valves at the mouth of the vena cava. To open them would require increased pressure, which is not available in this part;
- The presence of atrial volume receptors plays an important role in maintaining blood flow. These include low pressure baroreceptors. Their job is to send a signal to the hypothalamus when the pressure in that part decreases. The hypothalamus responds in turn by releasing vasopressin. During ventricular contraction, pressure increases.
The above functions of the right atrium ensure constant blood flow and circulation. If the pressure did not periodically increase, thanks to baroreceptors, then the flow of blood would be in jerks, and not constant.
HEART MASS
Heart mass (MC) depends on gender, age (see Table 2), mass, body surface area, height, and pathology and is therefore very inaccurate as an indicator of myocardial hypertrophy.
table 2
| Age | Indicators of heart size and mass | |||
| Length(cm) | Width(cm) | Thickness(cm) | Weight (g) | |
| Newborn | 2,9-3,1 | 3,8-4,0 | 1,7-1,8 | 16-23 |
| 1 year | 4,9-5,0 | 5,9-6,1 | 2,9-3,0 | 52-56 |
| 3 years | 5,4-5,5 | 6,2-6,6 | 3,1-3,3 | 68-71 |
| 5 years | 5,7-6,5 | 6,4-7,3 | 3,4-3,6 | 88-94 |
| 7 years | 6,2-7,0 | 7,3-7,6 | 3,3-3,5 | 107-110 |
| 9 years | 6,2-7,3 | 7,1-8,2 | 3,4-3,5 | 129-138 |
| 11 years | 7,4-7,7 | 8,0 | 3,4-3,5 | 154 |
| 13 years | 7,8 | 8,2-8,3 | 3,7-3,8 | 203-212 |
| 15 years | 8,2-8,3 | 8,7-8,8 | 3,9 | 224 |
| adults | 10-15 | 8-11 | 6-8,5 | 236-234 |
https://www.youtube.com/watch?v=DrI-_tTZHQI
Normal values of heart mass according to different authors vary widely. Our experience has shown that to assess hypertrophy it is advisable to use the criteria of A.M. Lifshitz (1984): normal heart weight in men is from 273 to 374 g, in women - from 236 to 325 g. Myocardial hypertrophy is stated when the heart weight is more than 380 g .
The superior vena cava and its system - characteristics, functions - About the veins
Superior vena cava syndrome (SVVC), or cava syndrome, is a group of characteristic symptoms caused by a violation of the outflow of venous blood from the neck, head, upper extremities and other organs of the upper body.
Usually a consequence of other diseases, mainly lung cancer. It is more common in men aged 35 to 60 years.
Basic information
Venous blood from all organs and tissues of the human body flows to the right half of the heart (venous) through two large venous trunks: the superior and inferior vena cava. Bypassing them, only the cardiac veins flow directly into the right atrium.
The human superior vena cava (SVC) is a short, valveless vein (up to 8 cm long). It is located in the anterior mediastinum and includes a number of large vessels. The superior vena cava carries venous blood from the upper part of the body to the heart.
This is a thin-walled vessel that is surrounded by relatively dense structures (trachea, aorta, bronchi, chest) and chains of lymph nodes along its entire length. The superior vena cava collects used blood from organs located above the diaphragm, and the inferior vena cava - below the diaphragm.
The physiological pressure in it is low, which can lead to mild blockage due to various lesions of the structures surrounding it.
Developmental anomaly
There is a congenital anomaly - the left superior vena cava, which is accessory to the right. It is formed during the period of intrauterine development of the fetus and accounts for 2 to 5% of congenital heart defects.
If the right SVC is missing and only the left one is present, the coronary sinus may become huge due to excessive blood flow into it.
Sometimes the left superior vena cava may drain into the left atrium. Then surgery is necessary.
Superior vena cava system
To understand the causes of the syndrome, you need to understand how the ERV functions.
The superior vena cava system consists of vessels that collect venous blood from the neck, head, upper extremities, and also through the bronchial veins from the lungs and bronchi.
Vessels that are part of the SVC system:
- veins of the arms and shoulder girdle (subclavian vein, deep and superficial veins of the arms);
- veins of the chest (esophageal, pericardial, bronchial and mediastinal veins);
- veins of the neck and head (anterior, internal, external jugular veins);
- some veins extending from the walls of the abdomen (azygos and semi-gypsy veins).
The veins that carry blood are very close to the heart. When the heart chambers relax, they seem to be attracted to it. This creates strong negative pressure in the system.
There are several tributaries of the superior vena cava. The main ones are the left and right brachiocephalic veins. They are formed as a result of the confluence of the internal jugular and subclavian veins and do not have valves.
Also a tributary of the SVC is the azygos vein. Starting in the abdominal cavity, it absorbs blood from the chest organs and intercostal veins. Equipped with valves.
The superior and inferior vena cava drain into the ventricle and right atrium. Oxygen-poor blood is pumped into the atrium as it relaxes. From there it enters the ventricle. Then to the pulmonary artery to get enough oxygen. Then the blood returns to the left side of the heart through the venous vessels. From there it will go to all organs.
If the patency of a vein is impaired, a compensatory function is performed by anastomoses (connections between vessels) that connect the basin of the superior and inferior vena cava.
But compensation of blood flow in the SVC cannot be completely ensured even by the large number of existing collaterals (bypass paths).
Etiology of cava syndrome
There are 3 types of pathology that provoke the development of superior vena cava syndrome:
- SVC thrombosis.
- Malignant neoplasm on the wall of the superior vena cava.
- Compression of the vein from the outside.
Malignant tumors that are most often (up to 90% of cases) complicated by cava syndrome:
- small cell, squamous cell lung cancer (most often right-sided);
- gastrointestinal cancer;
- breast cancer (with metastases);
- melanoma;
- lymphoma;
- sarcoma.
Other causes leading to superior vena cava syndrome:
- retrosternal goiter;
- sarcoidosis;
- traumatic and spontaneous thrombosis;
- idiopathic fibrous mediastinitis;
- constructive pericarditis;
- mediastinal teratoma;
- post-radiation fibrosis;
- purulent mediastinitis;
- tuberculosis, syphilis and other infectious diseases;
- silicosis;
- blood clot formation from a long stay of the catheter in the SVC.
Clinical manifestations
The severity of various symptoms of cava syndrome is influenced by:
- level of the SVC lumen;
- the degree of compression;
- speed of development of pathological processes.
The clinical course can be slowly progressive (with compression) or acute (with blockage).
The main symptoms of superior vena cava syndrome:
- swelling of the upper body and face;
- shortness of breath even at rest;
- nausea;
- cough;
- hoarseness of voice;
- cyanosis;
- noisy, wheezing breathing due to swelling of the larynx (stridor);
- fainting;
- difficulty breathing and swallowing;
- dilation and swelling of the veins of the upper body.
Less commonly, the following symptoms occur:
- suffocation (due to swelling of the larynx);
- lacrimation, tinnitus, double vision (due to disruption of the ocular and auditory nerves);
- bleeding (nasal, pulmonary, esophageal).
In very rare cases, during the acute course of superior vena cava syndrome, intracranial pressure increases and cerebral edema occurs, which can lead to hemorrhagic stroke and death.
Diagnostic measures
Diagnosis begins with a physical examination by a doctor. Based on its results, it identifies clinical indicators, the manifestation of symptoms and the degree of their intensity and establishes possible causes of the disease.
To clarify the nature of the blockage and its localization, additional instrumental studies are prescribed. The most informative of them are:
- chest x-ray in different projections;
- phlebography;
- computed tomography, MRI.
Additional diagnostic methods include:
- bronchological studies;
- Doppler ultrasound of the carotid and supraclavicular veins;
- consultation with an ophthalmologist (to determine eye disorders characteristic of cava syndrome).
Having all the diagnostic results in hand, the doctor determines treatment tactics.
Treatment
General treatment measures for patients are:
- bed rest (head should be elevated);
- low salt diet;
- constant oxygen inhalation.
Based on the causes of development and rate of progression of superior vena cava syndrome, optimal therapy is selected, most often aimed at relieving symptoms.
It is very important to determine the initial process that causes cava syndrome, that is, to establish the main diagnosis. And only in case of a threat to life and very severe disorders is it permissible to begin treatment without installing it.
The treatment methods used for superior vena cava syndrome are divided into conservative and surgical.
Conservative methods
Depending on the manifestation of symptoms, a different approach is required:
- for airway obstruction, tracheostomy, oxygen inhalation, and tracheal intubation are used;
- if there is a lack of air, a stent is installed through the skin;
- for cerebral edema, glucocorticosteroids and diuretics, anticonvulsants are used (if required);
- for malignant neoplasms - radiation therapy and chemotherapy;
- for thrombus, fibrinolytic drugs are prescribed.
If there is no effect from conservative treatment or worsening is observed, surgical intervention is performed.
Surgical methods
When the superior vena cava is compressed from the outside, radical decompression (tumor removal) is performed. If this is not possible, surgery is performed for the purpose of palliative care. In these cases, the patient may be prescribed:
- stenting (installation of a self-expanding metal stent through the skin);
- thrombectomy (removal of a blood clot);
- bypass (internal or external);
- external decompression;
- endoprosthetics;
- endovascular angioplasty through the skin.
Kava syndrome is a symptom complex that complicates the course of many diseases affecting the mediastinum.
Thus, good prognosis is impossible without successful primary therapy. Only removing the root cause will help stop the pathological process. In the acute course of the syndrome and in the presence of an oncological factor, the prognosis is unfavorable.
Therefore, if these symptoms occur, you should immediately contact a specialist and conduct a full medical examination.
Source:
Superior and inferior vena cava
The vena cava form the basis of the venous system and consist of two trunks - the superior and inferior veins, which collect blood from the entire human body and flow into the heart.
Anatomy of the vena cava
The upper one is located in the chest cavity, namely in its upper part. It is formed by the fusion of two veins - the brachiocephalic veins (right and left).
It originates at the level of the first rib to the right of the sternum, goes down, flows at the level of the third right rib into the right atrium. It is adjacent to the right lung, and the aorta passes to the left of it.
Behind the superior hollow is the root of the right lung, at the level of the second right rib it is covered by the pericardium. Before its entrance into the pericardial cavity, two veins flow into it: the azygos and the accessory hemi-unpaired.
The inferior vena cava begins in the abdominal cavity. It is formed at the confluence of the iliac veins, goes up, deviates to the right from the aorta towards the diaphragm.
https://www.youtube.com/watch?v=vFcC5tMGDP0
It is located in the retroperitoneal space behind the internal organs.
Through an opening in the diaphragm it is directed into the chest cavity, from there it goes to the pericardium and flows, like the superior hollow, into the right atrium. The following veins drain into the IVC:
- hepatic;
- diaphragmatic lower;
- adrenal gland right;
- renal;
- right ovarian or testicular;
- lumbar
The inferior vena cava is usually divided into three sections: infrarenal, renal and hepatic.
Vena cava diseases
The main pathology of the vena cava is their complete or partial obstruction (occlusion), due to thrombosis or tumor. The pathological conditions that develop in connection with this are called superior vena cava syndrome and inferior vena cava syndrome.
SVC syndrome
This pathology develops against the background of thrombosis or compression of the superior vena cava, as a result of which the venous outflow from the neck, head, shoulder girdle, and upper torso is disrupted. The syndrome is more often observed in men from 30 to 60.
Impaired patency of the SVC is associated with the peculiarities of its location, structure and low venous pressure. The superior vena cava is equipped with a system of anastomoses that perform a compensatory function in case of obstruction of the main vessel, but they are not able to completely replace it.
Reasons for development
There are three main causes of the syndrome:
- extravasal compression;
- tumor growth;
- blood clot formation.
In most cases, SVC syndrome is caused by malignant tumors, such as:
- lung cancer (usually right-sided);
- lymphoma;
- metastases into the mediastinum in breast, testicular, and prostate cancer;
- lymphogranulomatosis;
- sarcoma.
In addition, there may be other reasons:
- benign tumors;
- infections (syphilis, tuberculosis and others);
- aortic aneurysm;
- constrictive pericarditis;
- fibrous mediastinitis.
SVC syndrome can develop in case of vein thrombosis, which often occurs during prolonged catheterization or if there is a pacemaker in it.
Symptoms
The severity of symptoms depends on how severely the blood circulation is impaired, as well as on the speed of development of the SVC syndrome. Its course can be either chronic (in case of compression and tumors) or acute (in case of thrombosis).
The pathology is characterized by three signs: cyanosis of the skin, swelling, dilated saphenous veins on the face, neck, arms and upper torso.
In addition, manifestations of superior vena cava syndrome include:
Another article:How to remove veins on the legs using folk remedies
- chest pain;
- cough;
- dyspnea;
- attacks of suffocation;
- hoarse voice;
- swelling of the larynx and noisy wheezing;
- difficulty swallowing:
- bleeding (nasal, esophageal, pulmonary) caused by increased venous pressure;
- headache, noise in the head;
- confusion;
- drowsiness;
- convulsions;
- decreased vision, lacrimation, rapid eye fatigue;
- tinnitus, auditory hallucinations, hearing impairment.
Source: https://agent003.ru/metody-lecheniya/verhnyaya-polaya-vena-i-ee-sistema-harakteristika-funktsii.html