Causes of thrombosis of the veins of the lower extremities
Deep vein thrombosis is a condition in which a blood clot enters one of the deep veins of the lower extremities, hips, or pelvis. The clot blocks circulation through the veins that carry blood from the lower body to the heart. Deep vein thrombosis of the lower extremities (symptoms are the same in men and women) occurs in 1-2 people out of 1000 per year.
The disease and premature death from it are more common in low- and middle-income countries than in high-income countries. Primary thrombosis is called phlebothrombosis, and the risk of its occurrence is higher in women. Thrombophlebitis or secondary, more often occurs in men as recurrent thrombosis.
Three factors can lead to the formation of a blood clot:
- Damage to the inside of a blood vessel as a result of injury or surgery.
- A change in normal blood flow, including unusual turbulence, partial or complete blockage of blood flow.
- Hypercoagulation, a condition in which the blood thickens greatly.
The development of the disease is influenced by genetic, environmental and behavioral factors. The most common causes of the disease are surgical interventions and malignant neoplasms.
Causes of venous thrombosis:
| Medical | Drug use | Behavioral |
| Age | Oral contraceptives | Obesity |
| Extensive surgery | Postmenopausal hormonal drugs | Abuse of UV rays |
| Neurosurgery | Chemotherapy | Excessive alcohol consumption |
| Orthopedic surgery | Psychotropic drugs | Physical passivity |
| Prostatectomy | Use of thalidomide | Physical stress in old age |
| Malignant neoplasms | Corticosteroid use | Excessive caffeine consumption |
| Prolonged bed rest | Hard physical work | |
| Arthroscopy | ||
| Lupus |
The strongest factor is cancer, in which the possibility of developing thrombosis increases 50 times, and some types of operations. Moderate risk factors are medications, lifestyle, and lack of natural anticoagulants.
Pathophysiology
More than a century ago, Rudolf Virchow described 3 factors that are critical for the development of venous thrombosis: (1) venous stasis, (2) activation of blood coagulation, and (3) venous injury. These factors became known as the Virchow triad.
Venous stasis can result from anything that slows or obstructs the flow of venous blood. This leads to an increase in viscosity and the formation of microthrombi, which are not washed away by fluid movement; the resulting clot can then grow and multiply. Endothelial (intimal) blood vessel injury may be internal or secondary to external injury. This may be the result of accidental injury or surgical insult. A hypercoagulable state may occur due to a biochemical imbalance between circulating factors. This may result from an increase in circulating tissue activating factor combined with a decrease in circulating plasma antithrombin and fibrinolysins.
Over time, refinements have been made in the description of these factors and their relative importance in the development of venous thrombosis. The origin of venous thrombosis is often multifactorial, with the components of Virchow's triad taking on different significance in individual patients, but the end result is early thrombus-endothelial interaction. This interaction stimulates local production of cytokines and promotes the adhesion of leukocytes to the endothelium, which promote venous thrombosis. Depending on the relative balance between activated coagulation and thrombolysis, thrombus propagation occurs.
Decreased contractility of the venous wall and dysfunction of the venous valve contribute to the development of chronic venous insufficiency. Increased ambulatory venous pressure causes various clinical symptoms of varicose veins, lower extremity edema, and venous ulceration.
Development of thrombosis
Thrombosis is a homeostatic mechanism by which blood clots or thickens, a process critical to establishing hemostasis after injury. It can be initiated through several pathways, usually consisting of a cascade of enzyme activation that enhance the effect of the initial triggering event. This complex of events leads to fibrinolysis or dissolution of blood clots. The balance of trigger factors and enzymes is complex. Microscopic thrombus formation and thrombolysis (dissolution) are continuous events, but with increased stasis, procoagulant factors, or endothelial damage, the coagulation-fibrinolysis balance may promote pathological obstructive thrombus formation. Clinically significant deep vein thrombosis is the persistent formation of a macroscopic thrombus in the proximal deep veins.
For the most part, the coagulation mechanism consists of a series of self-regulating steps that lead to the formation of a fibrin clot. These steps are controlled by a number of relatively inactive cofactors or zymogens, which, when activated, promote or accelerate the coagulation process. These reactions usually occur on the phospholipid surface of platelets, endothelial cells or macrophages. Generally, the onset of the coagulation process can be divided into 2 different pathways, the intrinsic system and the extrinsic system.
The extrinsic system works by activation by tissue lipoprotein, which is usually released as a result of some kind of mechanical damage or trauma. The internal system usually includes circulating plasma factors. Both of these pathways combine at the level of factor X, which is activated to form factor Xa. This, in turn, promotes the conversion of prothrombin to thrombin (factor II). This is a key step in clot formation because active thrombin is required to convert fibrinogen into a fibrin clot.
Once a fibrin clot has formed and performed its function of hemostasis, the body has mechanisms to restore normal blood flow by lysing fibrin deposits. Circulating fibrinolysins perform this function. Plasmin digests fibrin and also inactivates coagulation factors V and VIII and fibrinogen.
There are three natural anticoagulant mechanisms that prevent inadvertent activation of the clotting process. These include heparin-antithrombin III (ATIII), thrombomodulin protein C and protein S, and tissue factor inhibition pathways. When injury occurs or when surgery is performed, circulating ATIII decreases. This enhances the coagulation process.
Congenital risk factors
Venous thromboembolism is a multifactorial disease in which hereditary and acquired causes are involved. The most prominent genetic factors in the development of thrombosis are the deficiency of natural anticoagulants, protein C, protein S and antithrombin.
Reasons that increase the risk of developing the disease include:
- Deficiency in the body of antithrombin, a protein that prevents excessive formation of blood clots.
- Disturbance of homeostasis.
- Congenital pathologies in the circulatory system.
Causes
Numerous factors, often in combination, contribute to deep venous thrombosis (DVT). They can be classified as acquired (eg, drug, disease) or congenital (eg, anatomical variant, enzyme deficiency, mutation). A useful categorization may be an acute precipitating condition versus a chronic condition, as this difference influences the duration of anticoagulant therapy.
Common causes of DVT are associated with increased venous congestion due to immobilization or central venous obstruction. The immobility can be as brief as that experienced during a transcontinental airplane flight or during surgery under general anesthesia. It may also be expanded, for example, during hospitalization for pelvic, hip or spine surgery, or due to stroke or paraplegia. People in these circumstances require monitoring, prevention, and treatment if they develop DVT.
Decreased blood flow due to increased blood viscosity or central venous pressure
Increased blood viscosity can reduce venous blood flow. This change may be due to an increase in the cellular component of the blood in polycythemia rubra vera or thrombocytosis or a decrease in the fluid component due to dehydration.
Increased central venous pressure, mechanical or functional, can reduce blood flow in the veins of the leg. Massive impact on the iliac veins or inferior vena cava due to neoplasm, pregnancy, stenosis, or congenital anomaly increases resistance to outflow.
Anatomical Variations Contributing to Venous Stasis
Anatomical variations that result in a reduced or absent inferior vena cava or iliac veins may contribute to venous stasis. In case of thrombosis of the iliac bones, the main anatomical contributor is identified in 60-80% of patients. The most well-known anomaly is compression of the left common iliac vein at the anatomical intersection of the right common iliac artery. The vein usually passes under the right common iliac artery during its normal course.
In some people, this anatomy causes compression of the left iliac vein and can lead to streaking or webbing, subsequent congestion, and DVT of the left leg. The reasons are poorly understood. Compression of the iliac vein is also called May-Thurner syndrome or Cockett syndrome.
Variants of the inferior vena cava are rare. Abnormal development is most often identified and diagnosed using cross-sectional imaging or venography. The embryological evolution of the inferior vena cava occurs from the enlargement or atrophy of the paired supracardinal and subcardinal veins. Abnormal embryological development may result in the absence of normal cava. These changes may increase the risk of symptoms because small vessels may be most susceptible to obstruction. In patients under 50 years of age suffering from deep venous thrombosis, the incidence of oral abnormalities reaches 5%.
A double or duplicated inferior vena cava results from a lack of atrophy in part of the left supracardinal vein, resulting in a duplication of the structure to the left of the aorta. A common form is the partially paired inferior vena cava, which connects the left iliac and left renal veins. When cavalet interruption, such as filter placement, is planned, these alternative paths must be considered. Alternatively, the inferior vena cava may not develop. The most common alternative route for blood flow is the azygos vein, which enlarges to compensate. If venous stenosis is present in the communication of the iliac veins and azygos veins, back pressure can lead to insufficiency, congestion, or thrombosis.
In rare cases, neither the inferior vena cava nor the azygos vein develops, and the iliac veins drain through the internal iliac collaterals into the hemorrhoidal veins and the superior mesenteric vein into the hepatic portal system. The hepatic venous drainage into the atrium is open. Because this pathway involves small hemorrhoidal vessels, thrombosis of these veins can cause severe acute swelling of the legs.
Inferior vena cava thrombosis is rare and is an unusual result of deep venous thrombosis of the legs unless an inferior vena cava filter is present and a large embolism in the cava is stopped, resulting in obstruction and expansion of the thrombosis. Common causes of oral thrombosis include tumors involving the kidney or liver, tumors invading the inferior vena cava, compression of the inferior vena cava by an extrinsic mass, and retroperitoneal fibrosis.
Mechanical vein injury
Mechanical damage to the vein wall appears to be an additional stimulus for venous thrombosis. Hip arthroplasty patients associated with femoral vein manipulation represent a high-risk group that cannot be explained by immobilization alone, with 57% of thrombi occurring in the affected femoral vein rather than the usual site of stagnation in the calf. Endothelial injury can convert normal antithrombogenic endothelium to prothrombotic endothelium by stimulating the production of tissue factor, von Willebrand factor, and fibronectin.
Injury may be obvious, for example due to trauma, surgery or iatrogenic injury, but they can also be obscure, for example due to distant deep vein thrombosis (possibly asymptomatic) or minor (forgotten) trauma. Previous DVT is a major risk factor for further DVT. The increased incidence of DVT in acute urinary tract or respiratory infections may be due to inflammation-induced changes in endothelial function.
Common risk factors for deep vein thrombosis
The presence of risk factors plays an important role in assessing the likelihood of DVT before testing. In addition, transient risk factors allow for successful short-term anticoagulation, whereas idiopathic deep vein thrombosis or chronic or persistent risk factors require long-term therapy.
The following factors were significantly and independently associated with an increased risk of VTE, most of which were asymptomatic and diagnosed by venography of both lower extremities:
- Presence of an acute infectious disease
- Age over 75
- cancer
- History of previous VTE
The most common risk factors are obesity, previous VTE, malignancy, surgery and immobility. Each occurs in 20-30% of patients. Hospitalized and nursing home patients often have multiple risk factors and account for half of all DVTs (with an incidence of 1 per 100 population). Obesity also appears to increase the risk of failure to reverse anticoagulation with prothrombin complex concentrate in patients with intracranial hemorrhage.
The single most powerful risk marker remains a history of DVT, as up to 25% of acute venous thromboses are observed in such patients. Pathologically, remnants of previous thrombi are often found in samples of new acute thrombi. However, recurrent thrombosis may actually result from primary hypercoagulable states. Disturbances in the coagulation cascade are the direct result of discrete genetic mutations in the coagulation cascade. Deficiency of protein C, protein S, or antithrombin III accounts for approximately 5-10% of all cases of DVT.
Age has been well studied as an independent risk factor for the development of venous thrombosis. Although there is a 30-fold increase in incidence from 30 to 80 years of age, the effect appears to be multifactorial, with more thrombogenic risk factors occurring in older adults than in those under 40 years of age. Venous stasis observed in immobilized patients and paralyzed limbs also contributes to the development of venous thrombosis. Autopsy studies have correlated the duration of bed rest with the incidence of venous thrombosis: 15% of patients in these studies die within 7 days of sleep and more than 80% in those who die after 12 weeks. In stroke patients, DVT is found in 53% of the paralyzed limbs, compared with only 7% on the normal side.
Malignant neoplasms are observed in 30% of patients with venous thrombosis. Thrombogenic mechanisms include abnormal coagulation, as evidenced by 90% of cancer patients having some abnormal coagulation factors. Chemotherapy may increase the risk of venous thrombosis by affecting the vascular endothelium, coagulation cascades, and tumor cell lysis. The incidence has been shown to increase in those patients who undergo longer courses of treatment for breast cancer, from 4.9% over 12 weeks of treatment to 8.8% over 36 weeks. In addition, DVT complicates 29% of surgical interventions performed for malignant neoplasms.
Postoperative venous thrombosis varies depending on a variety of patient factors, including the type of surgery performed. Without prophylaxis, general surgery typically has a DVT rate of about 20%, whereas orthopedic hip surgery can occur in up to 50% of patients. The nature of orthopedic diseases and diseases, injuries, and surgical repair or replacement of hip and knee joints predisposes patients to the occurrence of VTE disease. These complications are predictable and result from changes in the natural balance mechanisms of various disease states.
Based on radiolabeled fibrinogen, about half of lower extremity blood clots develop during surgery. Perioperative immobilization, coagulation disorders, and venous injury all contribute to the development of surgical venous thrombosis.
Genetic factors
Genetic mutations in the coagulation cascade represent groups at highest risk for developing venous thrombosis. Genetic thrombophilia has been identified in 30% of patients with idiopathic venous thrombosis. The primary deficiencies of the coagulation inhibitors antithrombin, protein C and protein S are associated with 5-10% of all cases of thrombosis. Altered procoagulant enzyme proteins include factor V, factor VIII, factor IX, factor XI, and prothrombin. Resistance of procoagulant factors to the intact anticoagulant system has also recently been described, with the recognition of the factor V Leiden mutation representing 10-65% of patients with DVT. Under conditions of venous stasis, these factors can accumulate in areas prone to thrombosis, where mechanical damage to the vessels has occurred, stimulating the endothelium to become prothrombotic.
Acquired risk factors
Thrombosis can develop based on acquired factors that are associated with diseases, medications and surgical interventions. Combined oral medications containing estrogen and progestin increase the likelihood of developing the disease by 2-4 times, especially for young women
The prevalence of obesity is increasing worldwide and is a factor in the development of thrombosis. With increased weight, the heart begins to work harder to pump blood, and the additional load leads to limited cardiac function.
Other reasons contributing to the development of thrombosis:
- age after 45 years;
- chronic lung diseases;
- liver diseases;
- varicose veins of the legs;
- early heart attacks;
- diabetes;
- complications during pregnancy;
- fractures of the leg bones;
- smoking;
Deep vein thrombosis of the lower extremities can be an acquired cause, for example due to smoking.
- long period of bed rest.
Treatment
The main goals of treatment for deep vein thrombosis (DVT) are to prevent pulmonary embolism, reduce morbidity, and prevent or minimize the risk of developing postthrombotic syndrome.
Anticoagulation has been the mainstay of drug therapy since the introduction of heparin in the 1930s. Other anticoagulant drugs have subsequently been added to the treatment armamentarium over the years, such as vitamin K antagonists and low molecular weight heparin (LMWH). Recently, mechanical thrombolysis has become increasingly used as endovascular therapy increases. Absolute contraindications to anticoagulant treatment include intracranial bleeding, severe active bleeding, recent brain, eye, or spinal cord surgery, pregnancy, and malignant hypertension. Relative contraindications include recent major surgery, recent cerebrovascular accident, and severe thrombocytopenia.
Immediate symptoms of DVT often resolve with anticoagulants alone, and the rationale for intervention is often a 75% reduction in long-term risk of PTS. Systemic IV thrombolysis once improved the rate of thrombotic vein recanalization; however, it is no longer recommended due to the increased incidence of bleeding complications, slightly increased risk of death, and modest improvement in PTS. The lack of a significantly reduced incidence of PTS after systemic thrombolysis (40–60%) likely reflects the inadequacy of the relatively low threshold volume of thrombus removal considered successful.
Thrombolytic therapy is recommended (systemic over catheter-directed therapy) in hypotensive patients with acute VT. When thrombolysis is contraindicated due to a high risk of bleeding, surgical thrombectomy or direct catheter-based thrombolysis is considered.
The risk of bleeding with systemic thrombolysis is similar to that of catheter-directed thrombolysis, and the risk of PTS may further reduce the risk. However, whether catheter-directed thrombolysis is preferable to anticoagulation has not been studied. Adding percutaneous mechanical thrombectomy to intervention options may make decision making easier because recanalization can be achieved more quickly than before and with a reduced lytic dose; therefore, the risk of bleeding may be reduced.
Symptoms
Deep vein thrombosis of the lower extremities includes symptoms:
- Red or discolored skin on the leg.
- Feeling of warmth in the affected area.
- Pain in the leg, which begins in the calf area, is felt in the form of cramps.
Thrombosis can occur without obvious symptoms.
Types of acute thrombosis
Thrombosis of the lower extremities at the site of blockage formation is divided into the following types:
- Proximal (in the popliteal region, along the deep vein of the thigh);
- Distal (with damage to the sural veins in the calf muscles).
If a patient has deep vein thrombosis, treatment cannot be started without establishing the type of thrombosis.
According to the degree of progression, they are distinguished:
- Phlebothrombosis is the initial stage of the disease, when the clot is slightly attached to the inside of the vessel.
- Thrombophlebitis - at this stage, inflammation begins in the veins and the blood clot is fixed more tightly.
Acute thrombosis is divided by type of blood clot, location, and origin.
- Proximal acute thrombophlebitis forms in the femoral vein and vessels of the popliteal region. Characterized by pain in the lower limb. In the projection of the affected vein, severe pain is felt and pronounced swelling is visible. Sometimes the first clinical manifestation of thrombosis is pulmonary embolism.
- With distal thrombosis, the calf veins are affected. Pain is moderate or absent. Swelling is usually not pronounced.
- The ileofemoral form of thrombosis develops in the area of the femoral and iliac vessels. Pain is felt in the calves, groin area, and inner thigh. Severe swelling develops from the groin, spreading to the toes. On palpation, thrombophlebitis manifests itself as severe pain in the projection of the great vessels of the thigh and leg. Thrombophlebitis often forms in the femoral vein, less often in the popliteal or gastrocnemius. A rare localization of thrombus formation is the inferior vena cava.
According to the etiology, thrombosis differs into inflammatory, associated with existing inflammation of soft tissues (thrombophlebitis), congestive, with compression of blood vessels, varicose veins, and associated with thrombophilia.
Diagnostics
By analyzing only the composition of the blood, the doctor cannot accurately determine the development of the disease. But almost all people who have a blood clot in their deep veins develop elevated levels of D-dimer in their blood. Normally it should be 243 ng/ml, for pregnant women - 644 ng/ml.
If thrombosis is suspected, differential diagnosis is carried out with a number of certain diseases:
- Thrombophlebitis, spontaneous or recurrent, of superficial veins.
- Injuries, ruptures, increased muscle tone.
- Chronic venous insufficiency caused by varicose veins and obesity.
- Swelling of the paralyzed leg, which occurs with paralysis.
- Cellulite with redness of the skin and increased temperature in the affected areas.
- Elephantiasis and lymphostasis.
Other methods are also used to make an accurate diagnosis.
Physical examination
When collecting anamnesis, before sending for an instrumental examination, the doctor must hear all complaints indicating the development of the disease and take into account the patient’s condition.
For example:
- the presence of dull or aching pain when walking or at rest;
- heaviness in the calf muscles, leg fatigue;
- development of edema in the lower leg or along the entire surface of the leg;
- combination of pain with swelling;
- primary or secondary thrombosis;
- history of bleeding disorders;
- taking oral contraceptives;
- pregnancy in the present or recent past.
Physical or clinical examination of the patient is carried out in vertical and horizontal positions. Palpation is also carried out to identify pain in the projection of the vascular bundle in the leg. Often the disease is asymptomatic, which is typical for people on long-term bed rest.
Functional tests
If necessary, functional samples are taken to determine the condition of the saphenous vein, the patency of the deep veins, and the discharge of blood from the deep veins to the superficial.
Homans' sign
The doctor’s task is to confirm or reject the diagnosis of venous thrombosis. For this purpose certain tests are carried out. One of the characteristic signs is Homans' sign - pain in the calf muscles when dorsiflexing the foot. It is checked with the patient lying on his back on the first day from the onset of the disease.
Moses test
Moses' symptom is determined by the presence of pain when the lower leg is compressed in the anteroposterior direction. There is no pain when pressing on the lower leg from the sides.
Lowenberg test
The symptom of the disease is confirmed by the presence of pain in the lower leg muscles at a pressure of up to 150 mm Hg. Art., created by the sphygmomanometer cuff. The cuff is placed on the middle third of the leg.
Opitz-Ramines test
The Opitz-Ramines diagnostic test is one of the variations of the previous diagnostic technique. The sphygmomanometer cuff is placed on the lower third of the thigh, pumping air to 160-150 mm Hg. Art.
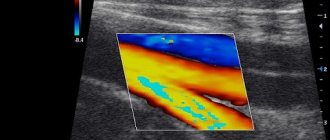
Ultrasound diagnostics
Using high-frequency sound waves, large proximal veins can be visualized and a thrombus, if present, can be detected. But in some cases, a blood clot that appears in small veins is not always visible.
Doppler ultrasound is prescribed as an initial step in deep vein screening. If the results are normal, a repeat test is scheduled after 6-8 days.
To accurately monitor the patient's condition, a series of studies are carried out at intervals of 7 days.
In case of poor visibility, radiopaque venography using MRI is prescribed.
Signs of thrombosis
DVT usually develops in the deep vein in the calf below the knee.
Typical symptoms:
- Pain and tenderness in the lower leg.
- Swelling of the lower leg.
- Color and temperature changes of the lower leg. Blood bypasses the blocked veins and is directed to the external veins. The lower leg becomes hot and red.
Sometimes there are no symptoms, and deep vein blood clots are only diagnosed if a complication such as pulmonary thromboembolism occurs.
Typical symptoms
Treatment of venous thrombosis of the lower extremities
Deep vein thrombosis of the lower extremities, the symptoms of which are confirmed by a doctor, determines the goals of treatment:
- normalization of blood flow in the lower extremities;
- preventing the development of ascending thrombosis in the pelvic and inferior vena cava;
- preventing the development of pulmonary embolism;
- preventive measures to prevent relapses;
- restoration of the patient's performance;
- reducing the level of disability of patients.
Drug therapy
If thrombosis develops in the acute stage, the drug Heparin is used, and subsequently doctors recommend switching to Warfarin to prevent the risk of re-development of thrombosis.
In some cases, thrombolysis is prescribed to prevent the development of thrombosis in the femoral veins. Most patients with thrombosis of the leg and thigh are successfully treated with low molecular weight heparin in an outpatient setting.
When a patient is hospitalized, standard heparin is prescribed intravenously as first-line therapy:
- for treatment: 450 units per day, calculated per 1 kg of weight;
- for prevention: 5000 units 2-3 times a day.
Instead of heparin, drugs included in the heparin group may be offered:
- Nadroparin.
- Adreparin.
- Enoxaparin.
- Tinzaparin.
The calculation of the administered drug is carried out by the doctor based on general indications and the degree of the disease. In addition to non-drug treatment, doctors recommend daily use of compression bandages, stockings, and tights.
Stockings for compression must be selected strictly according to size and it must be remembered that after 6 months the knitwear stretches and loses elasticity. Compression is strictly necessary during the first weeks after the development of the disease, but in the future it must be used for 1-2 years.
Thrombolysis
Thrombolytic therapy is aimed at restoring blood flow in the vessels due to the lysis of a blood clot, or the dissolution of cells under the influence of drugs. To prevent a split blood clot from entering the lungs, thrombolytic therapy is performed, which destroys the blood clot.
Using a catheter, drugs such as streptokinase, a muscle plasminogen activator, are injected directly into the site of the blood clot. The administration of drugs is carried out under x-ray control.
Installation of a vena cava filter
For patients whose body cannot accept anticoagulants, a vena cava filter is prescribed to prevent the risk of recurrent thrombosis. It is inserted into the inferior vena cava and allows for thrombolysis.
The filter is a specially manufactured mesh on a frame, which is inserted into the lumen of the vena cava to retain all particles larger than 4 mm. Thus, venous blood passes freely through the filter, and large blood clots are retained. The stuck blood clots are then dissolved using medications.
Surgery
Surgical methods are necessary when there is a threat of gangrene in the extremities, shock and systemic hypoperfusion. The decision to perform an operation by doctors is made immediately in case of ascending thrombosis and a high risk of developing thromboembolism in the pulmonary artery.
Types of operations performed:
- Phlebectomy, removal of varicose veins.
- An operation that eliminates the discharge of blood from deep veins.
- Stitching of veins.
- Extravasal correction of venous valves.
Traditional medicine recipes
Before starting treatment with home remedies, you should consult your doctor to prevent spontaneous bleeding. This is especially important when taking prescribed anticoagulants. Ginger helps in the treatment of thrombosis.
The natural salicylate in its composition blocks vitamin K and thins the blood:
- It is beneficial to drink ginger tea 2-3 times a day. For this, 1 tbsp. l. The chopped root is boiled and then infused in 2 glasses of water. You can add honey to ginger tea if desired.
- Fresh ginger can be added to prepared cooking dishes or chewed a few pieces throughout the day.
Cayenne pepper promotes better blood circulation, strengthens arteries and capillaries:
- Add 1/3 tsp to a glass of spinach juice. pepper, salt and drink 1-2 times a day.
- You can add pepper to an ointment or gel used to relieve pain in leg muscles.
Turmeric has a thinning property, improves blood circulation, helps prevent the formation of blood clots:
- Boil ½ tsp. spices in a glass of milk. Cool, add 1 tsp. honey. Drink 2 times a day.
A healthy vegetable, garlic, prevents the formation of blood clots, improves blood circulation, lowers blood pressure:
- Eat 2 cloves of garlic every day on an empty stomach.
- Garlic oil, prepared at home, can be used to massage the affected areas of the legs to reduce swelling and relieve pain.
Garlic Butter Recipe:
- Pass a head of peeled garlic through a press.
- Place the mixture in a sterilized jar and add any vegetable oil. Covered with a lid, the mixture is infused for 2 weeks in a warm place.
- The mixture should be stirred daily, then strained and the oil is ready for use. It is stored in a dark place at room temperature.
Fish oil containing omega-3 fatty acids helps the body well. They have fibrinolytic properties that prevent the formation of arterial blood clots. You can get healthy fat by eating salmon, pumpkin seeds, flax seeds, walnuts, or special supplements containing Omega-3.
Diet
To prevent the development of thrombosis, you should adhere to a healthy diet. This will help reduce weight, the risk of developing diabetes, cholesterol levels, which lead to disruption of the cardiovascular system, and subsequently to thrombosis.
Criteria to be followed in nutrition:
- Limit your intake of foods containing unhealthy fats and sodium.
- Avoid sweet and processed foods.
- Eat more fruits and vegetables.
- Include whole grains in your menu, as well as foods low in fat but rich in protein.
To maintain weight, it is advisable to reduce the portions of consumed foods.
Scientists suggest comparing a portion of food consumed at one time with certain items:
| Products | What should the portion be? |
| Fish or chicken | The size of the eaten piece, no more than a deck of cards |
| Fresh fruits or vegetables | The size of the eaten fruit, no more than a tennis ball |
| Potatoes, rice or pasta | A serving should be no more than 1 scoop of ice cream |
| Cheese | The piece should be the size of your thumb |
The size of the plate on which the dish is served also helps control appetite. It should not be life-size, but smaller. Half of its volume should be vegetables, ¼ should be protein, and the rest should be a grain or starchy product. You should control the alcohol you drink; it not only adds calories, but also has a detrimental effect on the cardiovascular system.
Preventive measures to eliminate thrombosis
After a major operation, thrombosis of the blood vessel is a one-time event.
However, some people who develop blood clots after surgery are still likely to have thrombosis - for example, if you have blood clotting problems or continue to be immobilized or immobile. As mentioned above, you may be prescribed to take anticoagulants (warfarin, usually) for a long time. Your doctor will tell you about this.
Other remedies that may help prevent formation or
Leg compression sleeves
recurrence of thrombosis:
- If possible, avoid long periods of immobility, such as sitting in a chair for many hours . If you are able, get up and walk more often. The best thing you can do is to do a half-hour or hour walking marathon every day in the fresh air. The goal is to stop the accumulation of blood in the extremities and improve blood circulation in the body and blood supply to the legs. Regular exercise for the calf muscles also helps. You are required to do some calf exercises even when you are sitting.
- Major operations are a risk of blood clots forming in the blood vessels - especially operations on the hip, lower abdomen, and legs . You may be given an anticoagulant, such as heparin injections, right before surgery to help prevent thrombosis.
- Several new drugs are now available and used to prevent thromboembolic diseases (DVT and PE) after joint replacement surgery, especially the hip or knee.
- Rivaroxaban and dabigatran etexilate are used in situations where preoral tablet administration rather than injection is required.
- Also, during a long operation, an inflatable sleeve that is connected to a pump can be used to create compression . You also have the right to use compression stockings and wear them in the hospital.
- The new drug Fondaparinux sodium (Arixtra) may be prescribed in some cases as an injection to prevent thrombosis in surgical patients or immobile medical patients in the hospital.
- When you have a long journey by plane, train, car or bus, you are required to take frequent short walks along the aisle . Try training your calf muscles while you sit in a chair. (You can do this by moving your ankle joints in a circle; place your feet in a tiptoe position and alternately lift your toes off the floor, keeping your heels on the ground, and vice versa.) Stay hydrated, stop drinking alcohol and sleeping pills. If you have previously had a blood clot, you should see your doctor for advice before you go on a long trip or fly.
- People who are overweight have an increased likelihood of developing blood clots in the deep veins . Therefore, to reduce your risk, you should try to reduce your weight.
Finally
- The most significant factor in the formation of hepatic thrombosis is immobility, especially during or after surgery.
- If you have major surgery, you will usually be given medications such as heparin injections to prevent blood clots (called thromboprophylaxis).
- The most serious complication of blood clot thrombosis is pulmonary embolism (PE or pulmonary embolism PE), some part of the clot breaks off and travels to the lungs, which can lead to death.
- Persistent symptoms may remain after thrombosis.
- With treatment, the risk of more than two complications is significantly reduced.
- Treatment includes anticoagulants (warfarin, usually), compression stockings, leg elevation, and staying active.
- Prevention is very important if the risk of breast thrombosis is increased - for example, during long operations or when you are planning travel and long trips.
How to survive if a blood clot breaks off? (video)
Complications and prognosis
The blockage causes severe pain and swelling in the affected leg. A blood clot can cause inflammation called thrombophlebitis, but complications are less common. Severe complications occur when a clot is released (embolized) and travels through the bloodstream, causing blockage of blood vessels in the lungs.
Pulmonary embolism occurs when a blood vessel in the lung is blocked by a blood clot, usually coming from a lower limb. This can be life-threatening.
It is important to monitor for symptoms of pulmonary embolism and contact your doctor if they occur:
- sudden shortness of breath;
- chest pain or discomfort that gets worse with deep breathing or coughing;
- rapid pulse;
- cough with bloody discharge;
- dizziness leading to fainting.
Deep vein thrombosis of the lower extremities, the symptoms of which can cause a complication in the form of postthrombophlebitis syndrome, develops within 1.5-2 years in 65% of patients who had primary thrombosis.
Signs:
- Persistent swelling of the legs.
- Change in skin color on the legs.
- Pain in the area of blood flow.
- Wounds on the skin of the leg.
In 25% of patients who have not consulted a doctor, thromboembolism occurs within 5 years. About 10-15% of them are fatal. With active therapy, the mortality rate is reduced by 10 times.
Other complications:
- Bleeding due to rupture of a varicose vein.
- Dermatitis, eczema.
- Trophic ulcers.
What is the characteristic of venous thromboembolism?
Thrombosis is the obliteration of a blood supply vessel by a blood clot (thrombus).
An embolism is when a blood clot dislodges from its site of formation and travels with the blood until it becomes lodged in a narrow spot in a blood vessel in other areas of the body. Such a blood clot is called an embolus.
Pulmonary embolism or pulmonary embolism (hereinafter referred to as PE or PE) is when a blood clot breaks away from the site of its formation (usually a leg vein) and clogs the lumen of one of the blood vessels in the lungs. Pulmonary embolism is also part of a group of diseases known as venous thromboembolism.
Rehabilitation
During the postoperative period, weakening of the legs and muscles occurs. Recuperation is an important step on the path to recovery. Significant improvement occurs 7-10 days after the start of blood thinning, but during this period the patient enters a qualitatively new state. To prevent relapses, you should change your lifestyle, diet and physical activity.
Advice for patients who have had deep vein thrombosis:
- Do not interrupt anticoagulant therapy, which can be very long. Such therapy is not carried out in courses; it must be continuous.
- Elastic compression is indicated for all patients who have suffered from the disease. This should be taught in the hospital, how to properly bandage a leg with elastic bandages.
- To prevent hyperkeratosis, which can develop due to wearing bandages, you should treat your feet with nourishing creams and gels at night.
- Avoid microtraumas in the legs and mycotic lesions.
- Carry out hygienic procedures by pouring hot and cold water over each leg daily for a vascular tonic effect.
- Limit all types of hair removal that are accompanied by heating the legs, laser, mechanical or electrical influence.
- Exclude foods containing vitamin K from the menu: coffee, liver, sorrel.
- Try not to sit or stand for more than 1 hour, so as not to strain your muscles.
- Regular walking will improve blood circulation and eliminate venous congestion. You should start by walking slowly for 3-5 minutes, at intervals of 3 minutes. for relax. The criterion for the ability to walk will be a feeling of fullness in the leg or pain. After one month, you can increase the duration to 1 hour. This training should continue for 2 years.
- Return to physical activity is possible one month after surgery.
- In the first 4 weeks after surgery, it is not recommended to travel by air. Low pressure in the aircraft cabin activates the blood clotting mechanism and there is an increased risk of thrombosis.
Why does blood thicken and thrombus formation occur in the deep veins of the legs?
Typically, blood that flows quickly through the veins and does not thicken. Walking promotes blood flow in the veins of the legs because the muscles compress the veins as they move.
- Sometimes DVT occurs for no apparent reason. There are the following components that can increase the risk of blood clots in the deep veins: Immobility , which causes slow blood flow in the veins. If the blood in your veins flows slowly, the risk of blood clots is much higher.
- Surgery , when the patient is under anesthesia for an hour to an hour and a half, is also the most common cause of thrombus formation in the deep veins. Your legs are at rest when you are under anesthesia because the muscles in your body are temporarily paralyzed. Blood flow in the leg veins may become very slow, making clot formation more likely at this time. Some types of operations (in particular, operations in the pelvic or leg areas) significantly increase the risk of hepatic thrombosis.
- Any illness or injury that causes immobility increases the risk. For example, a leg being in a hard cast after a fracture. People who are admitted to intensive care are at increased risk of developing thrombosis, for a variety of reasons, but mainly because they are very ill and secondly because they are immobile (they may be drowsy from the anesthetic drugs) .
- Long-distance travel by plane, train or bus (car) may slightly increase your risk . This happens because in these conditions a person mostly sits for a long time and does not move.
- Damage to the inside of the vein increases the risk of a blood clot. Vein thrombosis can lead to damage to the inner surface of the vein. If you have this pathology, then you have an increased risk of complications in the future. Certain diseases, such as vasculitis (an inflammatory condition of the vein walls) and certain medications (such as chemotherapy) can destroy the vein and increase the risk of creating blood clots in the veins. Damage to a vein can also occur at the site of a needle puncture. This can happen after IV treatment in hospital (when an intravenous catheter is inserted into a vein). Addicts who inject drugs such as heroin damage their veins, increasing the risk of blood clots. This happens if they inject drugs into the legs or groin.
- Conditions that cause excessive blood clotting (thrombophilia) and may increase the possibility of thrombosis. Some conditions can lead to increased blood clotting. For example, nephrotic syndrome and antiphospholipid syndrome. Some genetic conditions can also cause blood to clot quickly. Example: An inherited blood disorder such as the Leiden mutation can cause blood clots in the deep veins. If you have a close relative in your family who was or is suffering from DVT, then you are more likely to develop blood clots in the deep veins
- Birth control pills and hormone replacement therapy (HRT) medications, which contain estrogen, can significantly increase blood clotting. The likelihood of blood clots in the deep veins in women taking these medications is slightly increased.
- People with cancer or heart failure are at increased risk of thrombosis . Sometimes DVT occurs in a person who has not yet been diagnosed with cancer. Researchers are still searching for the cause of blood clots in the deep veins, a major cause of which may be cancer.
- Age. Older people tend to move much less than younger people, so their risk of thrombosis is higher.
- Pregnancy also increases the likelihood of developing the disease. One in 1,000 pregnant women was diagnosed with a DVT while they were expecting or within six months of giving birth.
- Obesity also increases the risk
- Men tend to develop blood clots in the deep veins more often than women.
- Dehydration most often leads to DVT. In fact, the blood becomes more viscous and the tendency to form clots increases.
Probability of thrombosis (according to Wells)
How often is thrombus formation found in deep veins?
Experts estimate that DVT occurs in one in 1,000 people each year.
Treatment of thrombosis (video)
Lifestyle
Deep vein thrombosis of the lower extremities, the symptoms of which are described earlier in the article, suffered at any age, requires changes in lifestyle.
For example:
- Stop smoking and drinking alcohol.
- Lower your blood pressure by eating less sugar and salt.
- Lose weight.
- Avoid prolonged sitting to avoid blood stagnation.
- During the day, do exercises for your legs several times, lifting them, stretching your calves.
- Walk daily, swim once a week, if possible.
- Avoid wearing tight clothing, especially in the lower body area.
- Wear compression stockings or underwear, especially during the postoperative period.
- Drink plenty of fluids throughout the day.
- Consult your doctor about taking birth control.
Deep vein thrombosis of the lower extremities is a common disease that affects people of all ages and affects health for many years.
Information about the prognosis and treatment options are always individual and depend on many symptoms. Doctors are doing everything possible to improve the quality of life of patients with postphlebitic syndrome, but people should also be more attentive to their health.
Author: Belyaeva Anna
Article design: Oleg Lozinsky
How to recognize the disease?
Venous and arterial thrombosis can be detected using Doppler ultrasound and venography. Various functional tests are of great diagnostic importance.
These include the Homans, Pratt, and marching tests. To identify subacute or acute deep vein thrombosis, Lowenberg's sign can be determined.
To do this, a blood pressure cuff is placed above the knee. Pressure of 80 or 100 mm Hg.
Art. causes pain in the limb. A healthy person has no pain.
A marching test is often carried out. For this purpose, bandaging is done from the fingers to the groin area.
The patient is asked to walk for a few minutes. Then the bandage is removed.
If there is thrombosis, bursting pain appears. Diagnosis of the disease also includes an interview, an external examination, a coagulogram, and a general blood and urine test.
Additional diagnostic methods include duplex scanning and radionuclide testing. A mandatory research method is rheovasography.
At the same time, the filling of the tissues and vessels of the lower extremities with blood is assessed.
Complex of medical procedures
So, how does modern medicine propose to treat thrombosis of the lower extremities?
When determining the diagnosis, the following is carried out for thrombosis of the veins of the lower extremities:
- drug therapy using anticoagulative drugs that reduce blood clotting factors;
- injection of a clot-dissolving substance into a vein;
- surgical removal of a blood clot;
- installation of vena cava filters in a vein.
Conservative treatment
The main goals of conservative treatment are to suppress subsequent thrombus formation , eliminate the inflammatory process and the attachment of the blood clot to the walls of the vessel , as well as the impact on tissue metabolism.
During drug treatment, the doctor prescribes anticoagulant drugs to the patient, which reduce blood clotting and reduce the risk of re-formation of blood clots. The most common drug is heparin and its derivatives.
Surgery
Only floating blood clots are subject to surgical intervention . In severe types of venous thrombosis of the lower extremities, which provoke the risk of tissue necrosis, surgical removal of the thrombus is appropriate.
This operation is venous thrombolectomy. In places where there are dangerous floating blood clots, vena cava filters are implanted for this purpose. This method helps people who cannot use anticoagulants.
However, the serious condition of the patients, due to the nature and scale of the primary surgical intervention, does not allow this procedure to be used in every case.
Methods and techniques of surgical operations in such patients are the subject of debate.
Some doctors adhere to femoral access to the main veins. Others prefer combined access , i.e. combination of femoral and laparotomy access to the inferior vena cava. The degree of surgical intervention in patients with thrombosis of the lower extremities depends on the degree of damage to the deep veins, the patient’s condition, etc.
What is deep vein thrombosis and why is it dangerous?
Deep vein thrombosis is a pathological condition in which a blood clot forms in the deep veins of the arms or legs. In order to understand the causes of thrombosis and the dangers this process poses, you need to know some features of the anatomy and physiology of our body.
- The walls of arteries contain a thin layer of smooth muscle that allows these vessels to change the width of the lumen, increasing their elasticity and ability to withstand the high blood pressure created by the heart. Thanks to this structure, arterial blood is delivered to the most remote corners of the human body. Veins do not have a muscle layer in their walls, so they do not in any way affect the speed of blood flow back to the heart. Venous blood moves towards the heart thanks to the work of skeletal muscles, which contract during movement, compress the veins and push blood through them. Thus, the greatest flow of blood through the veins occurs while we are engaged in physical activity.
- There are two types of veins in the arms and legs: superficial and deep. Superficial veins lie under the skin and are clearly visible in the form of dark, tortuous strands. The deep veins are located deep within the muscles of the upper and lower extremities. Blood can pass from the superficial veins to the deep veins through small perforating (perforating) veins. Superficial and perforating veins have special valves that ensure one-way blood flow only in the direction of the heart.
A piece of a blood clot can break off and begin to move towards the heart and lungs, and this is life-threatening
- The formation of a blood clot in the deep venous system of the arms or legs is not dangerous in itself. A life-threatening situation occurs when a piece of a blood clot or the entire blood clot breaks off and begins to move with the bloodstream towards the heart. Through the right atrium and right ventricle, the thrombus enters the pulmonary artery system and blocks its lumen. Pulmonary embolism very often ends in death. Therefore, the main goal of diagnosis and treatment of deep vein thrombosis is the prevention of pulmonary embolism.
- Superficial vein thrombosis is practically not dangerous from the point of view of thromboembolism, since the venous valves in the perforating veins do not allow blood clots to penetrate into the deep vein system.
Thrombosis prevention and treatment
If a person is at risk of developing thrombosis, it is necessary to be constantly monitored by the attending physician. Certain medications may be prescribed to prevent the disease. If we are talking about treatment, then it involves the simultaneous fulfillment of several conditions:
- It is necessary to thin the blood. To do this, patients take medications that contain acetylsalicylic acid. You should only select medications together with a doctor: acting on your own is dangerous to your health and life.
- It is important to strengthen blood vessels. To do this, you need drugs with active ingredients, including vitamin C. These products include a dietary supplement - a complex of venotonic vitamins and plant extracts “Normaven”. It helps maintain the strength and elasticity of blood vessels.
- Blood purification is required (with the help of special medications). All these measures help prevent the development of the disease.
Read also: Varicose veins in the groin area in women
Everyday preventive measures
In order to prevent thrombosis, it is necessary to follow simple measures to prevent this disease, which relate to our daily life.
Rejection of bad habits
It's no secret that bad habits themselves negatively affect the functioning of the entire body. People who often drink alcohol and also smoke cigarettes put their blood vessels at great risk.
If thrombosis has already begun or to prevent the disease, also avoid drinking strong tea or coffee.
Constant movement
Leading a sedentary lifestyle is unacceptable if you already have problems with blood clots. Moderate physical activity will also be an excellent prevention of their formation.
If you are the owner of a quiet office profession, then in your free time from work you need to lead an active lifestyle. Try to walk more, you can also do swimming or yoga.
Travel behavior
If you have a long journey in a car or plane that cannot be avoided, do everything possible to prevent vascular disease.
To prevent blood clots from forming after such events, it is necessary to purchase a pack of elastic bandages in advance. Also remember to drink enough water along the way.
Thermal impact
If you are serious about preventing heart and vascular diseases, then you should avoid almost all thermal manipulations.
Frequent visits to the bathhouse or sauna are unacceptable. Sudden changes in temperature provoke vasospasm, which causes blood clots to form. You should not test your body’s strength, increasing the risk of blood clots.
Read also: Thrombosis of mesenteric vessels of the intestine clinic
Doctor's examinations
Among patients who have already encountered the problem of blood clots, it is customary to visit a phlebologist for prevention 2 to 4 times a year.
This is done to ensure that there are no relapses of the disease, and you also need to try to detect small blood clots that appear in time.
It is possible that the patient will be advised to take folic acid or similar medications as a preventative measure. Anticoagulants and antiplatelet agents also have a good effect.
Taking vitamins
In order to prevent the formation of blood clots in blood vessels, it is necessary to maintain the correct vitamin balance in the body.
What to do if you can’t replenish your supply of vitamins through food? Your doctor will recommend special medications that you need to take to prevent blood clots from bothering you. If a person is suspected of thrombosis, he will be prescribed vitamins E and B.
Folk prevention
You can prevent excessive blood thickness, as well as subsequent blood clots, with the help of herbal decoctions made from natural ingredients.
Both eating berries and preparing a drink from them brings human blood to its physiological state. Healthy ingredients include cranberries, black currants, blackberries, viburnum berries, and sea buckthorn.
Tea made from raspberries and blueberry leaves has gained great trust in alternative medicine.
Drinking a drink of ginger and lemon in the morning will bring great benefits. As an alternative, you can use clover tincture.
These drinks effectively cleanse veins and blood vessels, preventing painful plaques from settling on their walls.
Another effective preventive remedy is topical creams or tinctures for drinking from chestnut fruits.
You can significantly improve blood circulation through the vessels with the help of birch buds, raspberry and linden leaves, sweet clover or hawthorn. Dill is also very popular in this regard. Before you start using any product, you must obtain the approval of your doctor.
The specialist will tell you which dosage will be most correct for you, as well as how long treatment should be carried out. It also wouldn’t hurt to conduct a home test for sensitivity to the components of the product. To do this, apply a small amount to your wrist or elbow.
Today, increased thrombus formation is a real problem for patients at risk. If prevention of blood clots is not carried out, the patient may even face death. Thrombosis prevention needs to be communicated to the masses of the public.
People definitely need to know how to protect themselves from blood clots and this insidious disease in general. Stagnation of blood in the vessels negatively affects the functioning of the heart, and over time can lead to a heart attack. A specialist can explain in detail how to prevent the formation of blood clots in your case. As a rule, with a proper lifestyle and sports activity, the patient does not require medications.
Methods for diagnosing the patency of deep veins
Upon examination, dilation, thickening and swelling of the veins are detected. Then the doctor conducts functional tests to determine the functioning of the valve apparatus of the venous network:
- Applying a tourniquet to the thigh of an elevated limb. With thrombosis, the veins below the ligation quickly fill up after moving to a standing position.
- When you cough, at the junction of the saphenous vein and the femoral vein, reverse blood flow is felt in the form of a push.
- Marching test - the limb is wrapped in an elastic bandage, the patient with thrombosis after walking feels fullness, pain, and the veins under the skin do not collapse.
The diagnosis can be confirmed using instrumental research methods:
- Ultrasound with Doppler sonography - a thrombus is detected, slowing of blood movement, narrowing of the lumen of the vessel, motionless valves, an expanded area to the site of blockage.
- Phlebography reveals initial signs and fresh blood clots, the degree of microcirculation disturbance.
Phlebography in the diagnosis of thrombosis