CVI – causes of chronic venous insufficiency
CVI is a symptom complex in which there are problems with the lumen of the veins. Usually the vessels have normal lumen. If there are disturbances, the capacity of the veins is significantly reduced. Overload of the venous system leads to impaired blood return, which is manifested by the appearance of symptoms of chronic venous insufficiency.
Impaired venous blood return leads to symptoms of CVI
Is CVI dangerous? Wikipedia states that CVI actively develops and progresses in women 30-50 years old, especially those with a hereditary predisposition. Often, symptoms of CVI appear during pregnancy, when body weight increases significantly.
Among the factors leading to CVI is weak physical activity.
The appearance of CVI is provoked by:
- travel in transport without changing position;
- long static position at the workplace;
- excess weight;
- tendency to constipation;
- staying in the heat for a long time;
- straining when lifting weights.
In addition, CVI can occur with systematic exercise and taking hormonal contraceptives; CVI often occurs during pregnancy.
Treatment
As medical practice shows, most patients diagnosed with chronic venous insufficiency seek medical help only in cases where the disease has caused a number of severe complications, and the treatment will be very complex and long.
Treatment methods include drug and surgical treatment of venous insufficiency, depending on the stage of the disease. Each patient undergoing treatment needs to change their daily routine to include several hours of physical activity. If you are overweight, you need to lose weight.
The first two stages of the disease do not require serious treatment. As a rule, the patient is prescribed medications that increase the tone of the walls of blood vessels - Ginkor-Fort, Detralex. The vein sclerotherapy method is used, in which a drug is injected that stops the process of blood outflow in the damaged vein in order to narrow it.
Detralex
The second – fourth stage is treated with the help of venotonics and antihistamines. If there is a high risk of complications, medications that have an anti-inflammatory effect are prescribed. The choice of medications depends on the individual characteristics of the patient and is prescribed only by the attending physician.
The most severe stages of the disease are 5 and 6, during which ulcers form, and medications with a general and local spectrum of action are prescribed. It is mandatory to treat ulcers daily with decoctions of chamomile and other remedies that have a soothing and disinfecting effect.
Surgical operations are performed only in the last stages of the disease, in the absence of positive dynamics from taking medications. The main types of operations are phlebectomy: removal of the damaged part of the vessel and bypass surgery - complete removal of the vein, and creation of a bypass to ensure blood flow.
CVI - symptoms
CVI may not manifest itself for a long time, but the symptoms that appear significantly affect the patient’s quality of life. The first symptoms are a feeling of heaviness in the legs, very often swelling of the legs and feet appears. Next comes bursting pain. The calf muscles may cramp at night, and the patient experiences a feeling of heat in the lower extremities.
Advanced forms of venous insufficiency - trophic eczema and ulcers
Spider veins and veins begin to appear through the skin, which with varicose veins become noticeable in the form of plexuses, similar to a bunch of grapes. The skin becomes drier and becomes covered with brown “islands” that grow as the disease progresses. Eventually, a trophic ulcer forms in their center.
Causes
Most people on the planet have a genetic predisposition to the disease. In some cases, the development of the disease is associated with age-related changes, since the walls of the veins become less elastic over time, stretch, and the venous valve is not able to ensure tight closure of the lumen.
The main factors that can cause the development of venous circulation insufficiency in the lower extremities:
- Regular intake of medications containing hormones.
- Pregnancy and labor. During the period of bearing a child, the lower limbs and pelvic organs experience excessive stress. The expanding uterus and the increasing weight of the fetus puts pressure on the veins in the pelvis, leading to their compression and provoking stagnant processes.
- Sedentary lifestyle. In people who have a “sedentary” job and do not bother themselves with physical activity, a venous network appears over time, which provokes the development of more serious pathological processes in the circulatory system.
- A position of the body in a lying or sitting position that lasts for hours. In some cases, the patient is recommended to change the nature of his work activity in order to recover from the disease.
- Excess body weight.
- Lifting heavy loads, which is associated with professional activities, is observed among athletes - weightlifters.
- Frequent visits to the steam room, taking hot baths.
CVI - stages of chronic venous insufficiency
The disease has several stages:
- first the venous wall changes;
- valves stop functioning;
- perverted blood flow occurs, leading to venous hypertension;
- varicose veins appear;
- skin pigmentation changes;
- Varicose eczema may appear;
- at this stage, thrombosis often develops, affecting the deep veins;
- complications include thrombophlebitis, pulmonary embolism.
The walls of the veins become more permeable, lymph enters the blood, trophism is disrupted and inflammation occurs (10-15% of cases). The last stage of CVI is a venous trophic ulcer (4% of cases)
Etiology and pathogenesis
Main reasons
Chronic and acute venous insufficiency are often secondary disorders that develop against the background of diseases such as:
- varicose veins in the legs;
- congenital vascular pathology;
- formation of blood clots in deep veins;
- damage to the lower extremities;
- hemodynamic disturbances after recent thrombosis.
Chronic venous insufficiency most often affects people involved in professional sports, obese patients, and women carrying a baby. Congenital pathology and a tendency to CVI are also predisposing factors. Other reasons can also influence the development of chronic venous disorders:
The disease can develop if you take hormonal drugs for a long time.
- long-term use of hormone-containing drugs;
- insufficiently active lifestyle;
- excessive body weight;
- age-related changes;
- constant physical activity.
How is it progressing?
Regardless of the cause of venous insufficiency of the lower extremities, the disease always develops in the same way. Impaired vascular circulation soon provokes an increase in pressure in the lumen of the vein, which expands. Against the background of this condition, valve insufficiency, which is responsible for regulating blood circulation, progresses. If the valves do not close tightly enough, blood begins to move towards the heart and legs. Gradually increasing pressure on the vascular walls leads to a loss of elasticity and increased permeability. Against the background of CVI, progression of arterial insufficiency often occurs.
CVI - Diagnostics
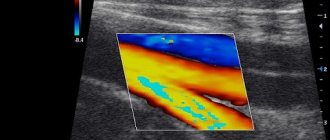
Typically, patients turn to a phlebologist when obvious signs of CVI are visible to the naked eye, and the diagnosis is easy to make. Specialized clinics use ultrasound methods to diagnose CVI:
- the condition of blood vessels is studied;
- assesses how blood flows through them;
- Disturbances in the functioning of venous valves are considered.
Ultrasound scanning gives a complete picture of the causes of CVI
With an ultrasound examination, the doctor receives a three-dimensional image of the vessel, reliable information about its functioning, and can make an objective diagnosis.
Diagnostics
The diagnosis of CVI is established after collecting complaints, objective examination and additional research methods. Patient complaints help to suspect the disease and indirectly determine the severity of the pathology.
During an objective examination, a phlebologist or surgeon evaluates the appearance of the saphenous veins and skin, identifies swelling and pain in the legs, listens to breathing over the lungs and heart sounds.
To clarify the diagnosis, instrumental examination methods are used:
- Duplex ultrasound.
- Doppler ultrasound.
- Phlebography is radiography of veins with a contrast agent.
In most cases, an ultrasound examination is sufficient to make a final diagnosis.
CVI – complications of chronic venous insufficiency
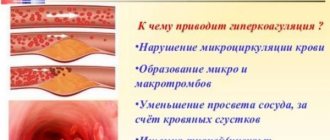
Many patients have a common belief that CVI is not too dangerous, that it is just cosmetic. In fact, disturbances in the venous blood flow of the legs provoke the formation of blood clots. Therefore, CVI has two main complications: thrombosis and thrombophlebitis. In the first disease, the deep veins suffer:
- the affected area acquires a bluish tint,
- tissues swell
- movements are accompanied by pain.
With thrombophlebitis, blood clots form in the superficial veins. Wherein
- the skin turns red;
- Painful lumps form under the skin
- When walking, the patient experiences sharp pain in the legs.
A detached blood clot can clog a large vessel and cause death. Acute manifestations of these diseases are treated only in a surgical hospital. You can see the danger of CVI - photos, the results are on websites on the Internet.
Symptoms of the disease
Let's look at the general symptoms first. It should be remembered that in the initial stages of the disease they appear one at a time and are often “blurred”. The more the disease progresses, the more pronounced the symptoms, and they most often appear in groups. So:
- pain in the legs, feeling of heaviness, fullness;
- spider veins;
- swelling - first passing after rest, then permanent;
- night cramps in the legs;
- dryness, unhealthy shine of the skin, age spots or areas of discoloration;
- trophic ulcers at an advanced stage.
Consultation with a surgeon: when to contact, how is the appointment?
Symptoms of CVI by stage
| Stage | Description |
| 0 | The person is able to work, there are no symptoms, they do not appear after sports and other activities. |
| 1 | Slight pain, heaviness in the legs and swelling at the end of the day, which disappears in the morning, mild cramps. A person is not limited in physical activity and can work at the same pace. |
| 2 | Manifestations of venous insufficiency become pronounced. These are skin pigmentation, dermatological diseases, severe swelling, skin necrosis in some areas. It becomes difficult for a person to work physically or play sports. |
| 3 | Trophic ulcers appear and tissue metabolism is completely disrupted. A person loses his ability to work. |
Symptoms of AHF
Signs of the disease are more pronounced and appear much faster compared to CVI:
- Pain in the legs that increases with movement;
- just below the site of vein blockage there is large swelling;
- difficulties in any physical activity;
- pallor or bluishness of the skin;
- at the site of pathology, skin temperature decreases by 2-3℃;
- body temperature can rise to 40℃;
- increasing pain to unbearable;
- “referring” pain to the groin and pelvis area.
Important! To reduce the likelihood of a blood clot breaking off with subsequent thromboembolism, the patient needs to limit movement. Bed rest is recommended for up to 10 days; the affected leg should be higher than the body.
CVI. How to treat the disease with creams?
Treatment with all kinds of ointments is very common at the household level. Many patients stop treatment at this point. Most ointments only temporarily relieve swelling and pain. CVI – how to treat it? This question is asked by all patients. Such popular remedies as heparin ointment, venoruton, venitan, hepatrombin cope well with the external manifestations of CVI at an early stage, but cannot eliminate its cause. For effective treatment that will give long-term results, a visit to a phlebologist or vascular surgeon is mandatory.
CVI - how to cure without consequences?
This can be done even in difficult cases; treatment of CVI in Moscow can be carried out at a high level. True, then surgery will be needed to restore blood flow in the veins. But in the early stages, conservative treatment of CVI without surgery is sufficient. In particular, elastic compression is used. For this purpose, special medical knitwear is used in the form of stockings, golf, tights (conservative treatment).
When treating CVI, it is very important not to waste time using various ointments that give a local and short-term effect, but to seek help from a qualified specialist.
CVI - treatment at home
Don't be afraid if you are diagnosed with CVI. Treatment with folk remedies will alleviate the situation. For example, venotonic drugs will help. They strengthen the walls of blood vessels, stimulate microcirculation, and quickly relieve the feeling of tired legs and swelling. Patients are also treated with blood thinning medications.
Do you need to relieve the pain of CVI? Treatment with traditional methods:
- Apple vinegar. Twice a day for 30 minutes. Apply gauze soaked in vinegar to your feet for 30 minutes. Keep your legs higher. Reviews about the product are contradictory, but the majority note a positive, weak effect.
- Bell pepper. Dilute a teaspoon of pepper powder in a glass of hot water and drink three times a day. The product stops leg pain and improves blood flow. But CVI does not go away that easily, treatment, the results are still not the same as when treated by a professional phlebologist.
Treatment tactics
Treatment of CVI is carried out by specialists from the field of therapy and surgery. Conservative treatment is prescribed for grades 0–1 of the disease and as maintenance therapy for grades 2–3 of pathology. Surgery is prescribed to radically remove pathologically altered veins and restore normal blood flow in the lower extremities.
Venous insufficiency medications have the following therapeutic effects:
- thin the blood and prevent pathological thrombus formation;
- strengthen the walls of the vessel, reduce its permeability;
- improve venous tone;
- eliminate swelling of the feet and ankles;
- normalize nutrition of leg tissues;
- reduce allergic skin rashes and pain.
Conservative therapy includes the following medications for venous insufficiency:
- venotonics and venoprotectors made on the basis of medicinal herbs (Detralex, Phlebodia, Venarus);
- anticoagulants (Heparin and its derivatives);
- antiplatelet agents (Pentoxifylline, Dipyridamole, Clopidogrel);
- antihistamines (Loratadine, Cetrin);
- antibacterial and antifungal drugs for infection of trophic wounds (Cephalosporins, Tetracyclines, Nystatin);
- nonsteroidal anti-inflammatory drugs (Ibuprofen, Nimesulide);
- local treatment in the form of creams and ointments (Lioton, Venitan, Algipor).
Medicines for venous insufficiency are prescribed by the doctor depending on the degree of CVI and the severity of the disease. Medicines are taken in regular or occasional courses of 2–3 months, on the recommendation of a specialist - in tablets or injections. In case of persistent edema due to venous insufficiency, potassium-sparing diuretics (Veroshpiron, Spironaloctone) are used.
Compression therapy is aimed at maintaining venous tone and includes:
- bandaging the legs with an elastic bandage;
- wearing compression garments (golf, stockings);
- pneumomassage.
Sclerotherapy is a treatment method that involves sclerosing a pathologically altered vein. To do this, a chemical is injected into the vessel, causing a burn to the inner lining (endothelium). As a result, the vein collapses and is cut off from the bloodstream.
The surgical method is performed in several ways. The pathologically altered vein is either ligated or removed using a special probe after applying medical tourniquets. Modern clinics are equipped with endoscopic equipment that allows operations to be performed with minimal tissue damage and a short recovery period.
During conservative treatment and after surgery, exercise therapy is recommended. Regular exercise helps strengthen the muscles of the lower extremities and increase the tone of the venous wall. Swimming, jogging, cycling, and race walking are useful.
The diet is enriched with fresh fruits and vegetables, which supply the body with fibrous fibers as part of fiber to strengthen the venous wall. It is necessary to limit your diet to fatty, spicy, salty foods, which cause thirst and overload the venous system with fluid. A low-calorie diet is indicated for overweight patients. A balanced diet prevents constipation, which reduces the risk of increased intra-abdominal pressure.
Prevention of chronic venous insufficiency
If you perform simple activities every day, the risk of developing CVI is reduced significantly. Even if CVI is discovered, treatment will not be so serious, especially in the early stages.
- You should lead a healthy lifestyle and play sports.
- Follow a diet.
- Wear comfortable shoes and use orthopedic insoles.
- Use elastic compression.
If the first signs of CVI still appear, you cannot postpone a visit to a phlebologist. He diagnoses the degree of CVI. Any delay in time is fraught with complications. Some of them are fatal. If the disease has nevertheless developed to a complex stage, you should not despair. Even complex cases can be cured using modern endovascular surgery, see the photo on our clinic’s website.
What are the dangers of complications?
If venous insufficiency of the lower extremities is not treated for a long time, it leads to serious consequences. Often the disease is complicated by the following pathologies:
- formation of trophic ulcers;
- an inflammatory reaction in the venous walls, resulting in the formation of blood clots;
- eczema;
- erysipelas.
The most severe complication is thromboembolism of the pulmonary artery, due to which the patient may die.
Frequently asked questions from our patients on the Internet
Maria from Arkhangelsk asks: I constantly have swollen legs, how can I restore blood circulation in my legs?
Dear Maria! To restore blood circulation in the legs, you first need to find out the cause of the swelling. As a rule, from a modern point of view, you need to start with an ultrasound duplex scanning of veins and consultation with a phlebologist.
Oksana from Vladimir is interested in: how to identify blood clots in the legs.
Dear Oksana! If you have the slightest suspicion of thrombosis, you should urgently seek medical help. A good diagnosis begins and always includes vascular ultrasound. This technique allows you to accurately determine not only blood clots in the legs, but also the cause of their occurrence. However, the method has a pronounced operator dependence, and it is better to trust professionals in their field.
Maxim from Yekaterinburg is interested in: how to understand that there are blood clots in the veins?
Dear Maxim! Only a specialist can reliably understand that there are blood clots in the veins, or exclude this situation. Thrombosis can be suspected based on the following signs:
- Swelling of the limb.
- Pain and/or redness.
- Feeling of heaviness and fullness in the limb.
- Vein thrombosis has already been previously diagnosed, since blood clots in the veins often recur.
The best solution would be to consult a phlebologist with an ultrasound scan of the venous vessels. You can make an appointment at our center for a consultation at any time convenient for you by phone.
Valentina from Smolensk asks: how to check the veins for blood clots in the legs?
Dear Valentina! You can check the veins for the presence of blood clots in the legs using ultrasound duplex or triplex scanning of the veins of the lower extremities at an appointment with a phlebologist.
Zinaida from Tambov asks: how to treat chronic venous insufficiency at home?
Dear Zinaida! Chronic venous insufficiency should be treated at home only after a good consultation with a specialist who will diagnose and give recommendations. Otherwise, you have a good chance of getting complications from the disease. When you find yourself on websites that colorfully describe how and what to treat at home, remember that most often professional doctors have nothing to do with such recommendations.
Nelly from Ufa asks: how to deal with the symptoms of chronic venous insufficiency?
Dear Nelly! It is better to start fighting the symptoms of chronic venous insufficiency in the legs before these symptoms appear, that is, with prevention: regular physiological exercise, a balanced diet, the use of compression hosiery for excessive loads, air travel. If signs of CVI appear: swelling, heaviness, varicose veins, you should consult a good specialist. This is the only way you can count on success.
PS I do not advise you to treat the symptoms of CVI at home via the Internet.
Alexandra from Tyumen asks: how to quickly relieve pain from chronic venous insufficiency at home?
Dear Alexandra! The appearance of pain with varicose veins is most often a symptom of a developed complication, varicothrombophlebitis or deep vein thrombosis. If pain occurs due to varicose veins, stopping it at home is an extremely dangerous undertaking. It is necessary to quickly seek medical help, possibly calling an ambulance. You can quickly relieve pain with any NSAID, for example, ketoprofen or meloxicam (Movalis). But this is purely a temporary measure.
Maria from Nizhny Novgorod asks: varicose veins have started, what should I do?
Dear Maria! If you have developed varicose veins or there are pronounced signs of varicose veins, you need to contact a professional. The most competent diagnosis and subsequent treatment can be provided to you by specialized centers for the treatment of venous pathology. After the examination, the center specialist will explain to you in detail what and how to do.
Nadezhda from Orenburg is interested in: what is a good prevention of varicose veins on the legs?
Dear Nadezhda! Prevention of varicose veins on the legs includes the following aspects:
- The closest to physiological load on the lower extremities, the involvement of the calf muscles, reducing the time of static load.
- Complete, balanced nutrition.
- For long-term static conditions and air travel, wear compression hosiery of I-II compression class.
Classification
Classification of CVI
The most common classification of chronic venous insufficiency is the following:
- degree 0. In this case, there are no pronounced symptoms of the disease. The patient does not notice any changes. Functionality preserved;
- degree 1. This degree is characterized by the appearance of the first symptoms indicating the presence of a pathological process in the body. The patient feels pain in the lower extremities, a feeling of heaviness and fullness. Soon pronounced, persistent swelling and cramps appear (more pronounced at night);
- degree 2. Swelling does not disappear. On examination, eczema, hyperpigmentation, lipodermatosclerosis are noted;
- degree 3. Trophic ulcers form on the surface of the extremities. This condition is the most dangerous for the patient's health.
There is also an international classification of WHI and CVI - the CEAP system.
Classification of venous insufficiency according to CEAP
According to the clinical picture:
- 0 – there are no visual signs of a person having pathology of the venous vessels;
- 1 – telangiectasia;
- 2 – varicose veins on the legs are visually noted;
- 3 – persistent swelling appears;
- 4 – changes appear on the skin;
- 5 – changes on the skin in the presence of an already healed ulcer;
- 6 - changes on the skin in the presence of a fresh ulcer.
Etiological classification is important, since the treatment of venous pathology largely depends on the causes that provoked chronic circulatory failure.
Etiological classification:
- EC – genetic predisposition;
- ER – unknown cause;
- ES – deficiency develops in a person due to injury, thrombosis, etc.
Anatomical classification according to the CEAP system makes it possible to display the level of the lesion, segment (deep, superficial or communicating), as well as the localization of the pathological process (inferior vena cava or great saphenous vein).
Classification of CVI according to the CEAP system, taking into account pathophysiological aspects:
- chronic insufficiency of venous circulation with reflux symptoms;
- CVI with manifestations of obstruction;
- Combined CVI (combination of reflux and obstruction).
The classification of acute and chronic circulatory failure is used in medical institutions by phlebologists to determine the stage of the disease, as well as its severity. This is necessary to prescribe appropriate effective treatment.