A pathology such as arterial insufficiency of the lower extremities can be present in a latent form in any modern person leading a sedentary lifestyle. The fact is that arterial insufficiency in the chronic form of the disease does not lead to any visible manifestations. Typically, the first symptoms of peripheral vascular damage appear in the later stages of the disease. The existing classification of arterial insufficiency of the lower extremities includes several stages. One of them is an asymptomatic course with hidden pathological changes in muscle tissue at the level of myocytes.
Acute lower extremity ischemia can occur suddenly and lead to the appearance of severe clinical signs within a few minutes. Modern classification of lower extremity ischemia allows us to clarify the etiology of this process and indicate a potential cause. Depending on the stage of arterial insufficiency, it is possible to provide conservative pharmacological assistance or prescribe emergency surgical intervention.
Classification of chronic arterial insufficiency (ischemia) of the lower extremities
Taking into account the fact that chronic arterial insufficiency is a syndrome caused by changes in the anatomical structure and function of the arteries of the extremities, we considered it necessary to dwell in more detail on the methodology for examining patients due to the high frequency of this disease: it is known that intermittent claudication is observed in 5% of the world's population. The classification of chronic limb ischemia used allows us to identify the stage of the pathological process and the degree of morphological changes in tissues.
According to the modern classification of arterial insufficiency, the asymptomatic stage is characterized by damage (usually atherosclerotic) to arteries without hemodynamically significant stenoses or with minor changes in regional hemodynamics that do not cause clear clinical manifestations of chronic limb ischemia. In this case, a fairly high frequency of combined lesions of two or more arterial systems and the presence of other concomitant cardiovascular pathology are of important pathogenetic significance, which can contribute to the deterioration of locomotor function and the appearance of symptoms in the limb.
According to the classification of chronic arterial insufficiency, intermittent claudication characterizes the stage of subcompensation - the main symptoms appear during physical activity. At this stage, morphological changes in the arteries are significant and sufficient to cause distinct hemodynamic changes, the essence of which boils down to the suppression of the parameters of volumetric blood flow velocity and perfusion pressure in the arteries distal to the focus of the obliterating lesion.
The subcompensation stage according to the classification of chronic ischemia of the lower extremities develops due to a discrepancy between the delivery of oxygen and the tissue needs for the required amount for energy production. As you know, all living cells constantly need adenosine triphosphoric acid (ATP) to maintain their own vital activity and viability. This minimum energy intake is referred to as basal ATP intake (resting 0.5 µmol/g tissue/min).
Physical activity leads to a multiple (tens of times) increase in ATP consumption - in this case we are talking about the functional volume of ATP consumption. Skeletal muscles generally have a high need for ATP and are quite sensitive to its deficiency. Due to the fact that there are practically no reserves of ATP in myocytes (and when ATP synthesis in the muscles ceases, its reserves are depleted in a few seconds), cells require a continuous influx of both metabolites (as substrates of respiration) and oxygen ( as the final acceptor in oxidation reactions). If their intake into cells is insufficient, ATP synthesis decreases; This state is called hypoenergetic.
I79* Lesions of arteries, arterioles and capillaries in diseases classified elsewhere
I79.0* Aortic aneurysm in diseases classified elsewhere
I79.1* Aortitis in diseases classified elsewhere
I79.2* Peripheral angiopathy in diseases classified elsewhere
I79.8* Other lesions of arteries, arterioles and capillaries in diseases classified elsewhere
Diseases of arteries, arterioles and capillaries (I70-I79)
I70 Atherosclerosis
- arterial
- arteriovascular
- vascular
endarteritis deformans or obliterans senile:
- arteritis
- endarteritis
Excl.: cerebral (I67.2) coronary (I25.1) mesenteric (K55.1) pulmonary (I27.0) The following supplementary classification to indicate the presence or absence of gangrene is provided for optional use with appropriate subcategories in I70.
I70.0 Atherosclerosis of aorta
I70.1 Atherosclerosis of renal artery
I70.2 Atherosclerosis of arteries of extremities
I70.8 Atherosclerosis of other arteries
I70.9 Generalized and unspecified atherosclerosis
I71 Aortic aneurysm and dissection
I71.0 Dissection of the aorta
I71.1 Thoracic aortic aneurysm, ruptured
I71.2 Thoracic aortic aneurysm, without mention of rupture
I71.3 Abdominal aortic aneurysm, ruptured
I71.4 Abdominal aortic aneurysm, without mention of rupture
I71.5 Thoracoabdominal aortic aneurysm, ruptured
I71.6 Thoracoabdominal aortic aneurysm, without mention of rupture
I71.8 Aortic aneurysm of unspecified site, ruptured
I71.9 Aortic aneurysm of unspecified site, without mention of rupture
I72 Other aneurysm and dissection
- aorta (I71.-)
- arteriovenous NOS (Q27.3)
- arteriovenous NOS acquired (I77.0)
- ruptured (I60.-)
dissection of:
- coronary artery (I25.4)
- precerebral artery, congenital (nonruptured) (Q28.1)
I72.0 Aneurysm and dissection of carotid artery
I72.1 Aneurysm and dissection of artery of upper extremity
I72.2 Aneurysm and dissection of renal artery
I72.3 Aneurysm and dissection of ilioartery
I72.4 Aneurysm and dissection of artery of lower extremity
I72.5 Aneurysm and dissection of other precerebral arteries
- carotid artery (I72.0)
- vertebral artery (I72.6)
I72.6 Aneurysm and dissection of vertebral artery
I72.8 Aneurysm and dissection of other specified arteries
I72.9 Aneurysm and dissection of unspecified site
I73 Other peripheral vascular diseases
I73.0 Raynaud syndrome
I73.1 Thromboangiitis obliterans [Buerger]
I73.8 Other specified peripheral vascular diseases
- simple
- vasomotor
Erythrocyanosis Erythromelalgia
I73.9 Peripheral vascular disease, unspecified
I74 Arterial embolism and thrombosis
- embolic
- thrombotic
Excl.: embolism and thrombosis:
- basilar (I63.0-I63.2, I65.1)
- carotid (I63.0-I63.2, I65.2)
- cerebral (I63.3-I63.5, I66.9)
- complicating: abortion or ectopic or molar pregnancy (O00-O07, O08.2)
- pregnancy, childbirth and the puerperium (O88.-)
I74.0 Embolism and thrombosis of abdominal aorta
I74.1 Embolism and thrombosis of other and unspecified parts of the aorta
I74.2 Embolism and thrombosis of arteries of upper extremities
I74.3 Embolism and thrombosis of arteries of lower extremities
I74.4 Embolism and thrombosis of arteries of extremities, unspecified
I74.5 Embolism and thrombosis of iliatric artery
I74.8 Embolism and thrombosis of other arteries
I74.9 Embolism and thrombosis of unspecified artery
I77 Other disorders of arteries and arterioles
I77.0 Arteriovenous fistula, acquired
I77.1 Stricture of artery
I77.2 Rupture of artery
I77.3 Arterial fibromuscular dysplasia
I77.4 Coeliac artery compression syndrome
I77.5 Necrosis of artery
I77.6 Arteritis, unspecified
- aortic arch [Takayasu] (M31.4)
- cerebral NEC (I67.7)
- coronary (I25.8)
- deformans (I70.-)
- giant cell (M31.5-M31.6)
- obliterans (I70.-)
- senile (I70.-)
I77.8 Other specified disorders of arteries and arterioles
I77.9 Disorder of arteries and arterioles, unspecified
I78 Diseases of capillaries
I78.0 Hereditary haemorrhagic telangiectasia
I78.1 Naevus, non-neoplastic
- NOS (D22.-)
- blue (D22.-)
- flammeus (Q82.5)
- hairy (D22.-)
- melanocytic (D22.-)
- pigmented (D22.-)
- portwine (Q82.5)
- sanguineous (Q82.5)
- strawberry (Q82.5)
- vascular NOS (Q82.5)
- verrucous (Q82.5)
I78.8 Other diseases of capillaries
I78.9 Disease of capillaries, unspecified
I79* Disorders of arteries, arterioles and capillaries in diseases classified elsewhere
I79.0* Aneurysm of aorta in diseases classified elsewhere
I79.1* Aortitis in diseases classified elsewhere
I79.2* Peripheral angiopathy in diseases classified elsewhere
I79.8* Other disorders of arteries, arterioles and capillaries in diseases classified elsewhere
Add a comment Cancel reply
List of classes
Excluded: autoimmune disease (systemic) NOS (M35.9)
disease caused by the human immunodeficiency virus HIV (B20 - B24) congenital anomalies (malformations), deformations and chromosomal disorders (Q00 - Q99) neoplasms (C00 - D48) complications of pregnancy, childbirth and the postpartum period (O00 - O99) certain conditions arising in the perinatal period (P00 - P96) symptoms, signs and abnormalities identified during clinical and laboratory tests, not classified elsewhere (R00 - R99) trauma, poisoning and some other consequences of external causes (S00 - T98) endocrine diseases, nutritional disorders and metabolic disorders (E00 - E90).
Note. All neoplasms (both functionally active and inactive) are included in class II. The corresponding codes in this class (for example, E05.8, E07.0, E16-E31, E34.-) can, if necessary, be used as additional codes to identify functionally active neoplasms and ectopic endocrine tissue, as well as hyperfunction and hypofunction of the endocrine glands, associated with neoplasms and other disorders classified elsewhere. Excluded: certain conditions arising in the perinatal period (P00 - P96), some infectious and parasitic diseases (A00 - B99), complications of pregnancy, childbirth and the puerperium (O00 - O99), congenital anomalies, deformities and chromosomal disorders (Q00 - Q99 ), diseases of the endocrine system, nutritional disorders and metabolic disorders (E00 - E90), injuries, poisoning and some other consequences of external causes (S00 - T98), neoplasms (C00 - D48), symptoms, signs and deviations from the norm identified in clinical and laboratory studies, not classified elsewhere (R00 - R99). Chapter IX Diseases of the circulatory system (I00-I99)
Excluded
: diseases of the endocrine system, nutritional disorders and metabolic disorders (E00-E90) congenital anomalies, deformations and chromosomal disorders (Q00-Q99) some infectious and parasitic diseases (A00-B99) neoplasms (C00-D48) complications of pregnancy, childbirth and postpartum period (O00-O99) certain conditions arising in the perinatal period (P00-P96) symptoms, signs and abnormalities identified during clinical and laboratory tests, not classified elsewhere (R00-R99) systemic connective tissue disorders (M30- M36) trauma, poisoning and some other consequences of external causes (S00-T98) transient cerebral ischemic attacks and related syndromes (G45.-)
This chapter contains the following blocks
: I00-I02 Acute rheumatic fever I05-I09 Chronic rheumatic heart diseases I10-I15 Hypertensive diseases I20-I25 Ischaemic heart diseases I26-I28 Pulmonary heart disease and diseases of pulmonary circulation I30-I52 Other forms of heart disease I60-I69 Cerebrovascular diseases I70 -I79 Diseases of arteries, arterioles and capillaries I80-I89 Diseases of veins, lymphatic vessels and lymph nodes, not elsewhere classified I95-I99 Other and unspecified disorders of the circulatory system
source
1st, 2nd and 3rd degrees of chronic arterial insufficiency (ischemia) of the lower extremities
Depending on the degree of chronic arterial insufficiency, energy metabolism in muscle fibers is disrupted. Thus, arterial insufficiency of the 1st degree does not lead to significant changes. And arterial insufficiency of the 2nd degree already makes the work of the muscles of the lower extremities difficult. With the 3rd degree of arterial insufficiency, intermittent claudication already occurs and typical clinical signs may appear.
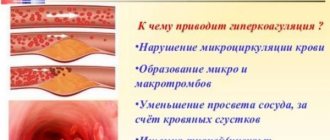
A hypoenergetic state develops with chronic arterial insufficiency of the lower extremities (spasm, thrombosis, stenosis), which is clinically manifested by ischemia and pain. Thus, in stage II (stage of illness) of chronic ischemia of the lower extremities, characterized by an initial decrease in blood supply to skeletal muscles, at rest the amount of incoming metabolites and oxygen is sufficient for the synthesis of ATP and is able to compensate for the basal volume of energy consumption. However, during physical activity (during which there is even a slight compensatory increase in blood flow), the volume of these substrates becomes insufficient for the production of ATP.
In grades III and IV chronic limb ischemia, united by the term “chronic critical ischemia,” the level of delivery of substrates for ATP synthesis is insufficient, resulting in not only a sharp decrease in functional, but also a significant inhibition of basal ATP consumption. In addition, a drop in perfusion pressure with severe ischemia of the lower extremities triggers a cascade of local microcirculation disorders. And with the addition of a local infection, the release of bacterial toxins and a response to an infectious agent, microcirculation and metabolic disorders in ischemic tissues are significantly aggravated.
Prevention
To protect yourself as much as possible from the development of blood clots, first of all you should completely stop smoking . It is necessary to either completely exclude or minimize the amount of salt from the diet, as well as all foods high in cholesterol. These are sausages and semi-finished products, butter, potatoes, cream and full-fat sour cream, canned food, fatty meat and lard, fast food, egg yolk and red caviar.
Regular physical activity prevents congestion that causes venous insufficiency and helps avoid obesity, which leads to atherosclerosis.
Sharp pain, tingling or a feeling of numbness in one of the limbs is a reason to immediately contact a phlebologist. Considering the degree of threat of this disease, immediate control of thrombosis at the initial stage increases the chances not only of saving the limb, but also life in general.
ICD-10 Category: I74.4
Acute arterial insufficiency (ischemia) of the lower extremities
In addition to chronic, there is acute arterial insufficiency, which develops as a result of any sudden decrease in blood supply to the limb and creates a potential threat to its viability. The causes of acute limb ischemia are thrombosis (40%), embolism (37%), thrombosis of prostheses and areas of endovascular interventions (up to 15%), as well as thrombosis of peripheral artery aneurysms and arterial trauma.
Due to the fact that patients often do not pay attention to the symptoms of the disease, not associating them with diseases of the vascular system, and therefore do not always report them to the doctor, during the survey it is necessary to ask a standard set of questions, which allows identifying symptoms of the disease that are significant for diagnosis, but to which the patient himself may not pay due attention.
Find out if he has:
- Changes in muscle development and symptoms when walking such as weakness, soreness, numbness in the muscles of the lower extremities (buttocks, thighs, calf muscles)
- Discomfort in the legs at rest or when straining
- Symptoms indicating poor healing or non-healing of wounds in the legs and feet
- Pain in the legs (feet), which depends on the position of the body (standing, lying down)
- Abdominal pain triggered by food intake, and whether the patient has noticed a recent change in body weight (loss)
- Closest first-degree relatives diagnosed with an abdominal aortic aneurysm
- Indications for the presence of hypertension with high diastolic blood pressure
- Transient or permanent neurological impairment, visual changes, history of ischemic stroke
The patient should be asked whether he has had any episodes of migratory thrombophlebitis of the superficial veins (thromboangiitis obliterans), or whether he has been exposed to chronic intoxication (nicotine, alcohol). In addition to atherosclerosis as the main cause of acute ischemia of the lower extremities, there are other nosologies that contribute to the gradual occlusion of arteries: diabetes, lipid metabolism disorders, hypertension, increased levels of homocysteine and a serum marker of systemic inflammation (C-reactive protein - CRP), hyperfibrinogenemia, chronic renal failure.
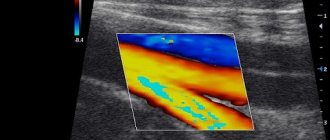
During an objective examination, if acute arterial insufficiency of the lower extremities is suspected, attention is paid to the color of the skin and the severity of trophic disorders, which directly depend on the stage of arterial insufficiency of the affected limb.
Thus, a leg raised at an angle of 45° in a lying patient suddenly turns pale, and the color of the limb lowered onto the bed is restored later than after 10 s (normal value). The skin of patients with obliterating diseases of the arteries of the lower extremities loses its elasticity and becomes dry. The nail plates of the toes of the affected foot (especially the first and fifth toes) become dark, dull, brittle, uneven and deformed. Less often, the nails become thinner, and more often they become noticeably thicker.
As a result of subungual hyperkeratosis, they take on an ugly shape - they become sharply curved, grow in the form of a mushroom, or bend downwards. In some cases, these characteristic changes remain unnoticed by the attending physician, who is inclined to explain these changes as a manifestation of epidermophytosis.
With more significant circulatory disorders, hair growth stops and hair loss occurs, and atrophy of the muscles of the lower leg and thigh of the affected limbs is noted.
In a number of patients with stages III and IV of acute arterial insufficiency of the limb, swelling of the distal parts of the limb is observed. At the stage of trophic disorders, there is increased vulnerability of the tissues of the affected limb. Even after minor injuries, abrasions, bruises, wounds when caring for nails, and sometimes for no apparent reason, cracks and deep ulcerations occur. Appearing in the most distal parts of the limb, they are often accompanied by severe pain.
Symptoms of vascular ischemia of the lower extremities
Pain in the affected limb is the first sign. The pain syndrome is especially pronounced during embolism. A feeling of numbness, coldness, and paresthesia are pathognomonic symptoms of ischemia of the lower extremities; in almost all cases, pallor of the skin is detected. Subsequently, a bluish tint appears, with severe ischemia of the o. Noteworthy are the symptoms of limb ischemia, such as a decrease in body temperature, most pronounced in the distal parts, and a disorder of superficial and deep sensitivity: from a slight decrease to complete anesthesia. Sensory impairment always occurs as a “stocking”.
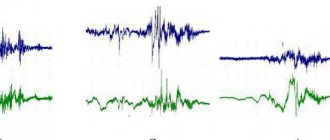
The absence of arterial pulsation distal to the occlusion is the only clinical sign of vascular ischemia of the lower extremities, allowing the localization of an embolus or thrombus to be determined.
Careful palpation determination of the pulsation of the arteries of the limb will help to determine (quite accurately) the proximal level of acute vascular occlusion without any instrumental research methods. Detection of systolic murmur allows one to suspect stenotic lesions of proximally located vessels.
Impairment of active movements in the limb is characteristic of severe ischemia and manifests itself in the form of a decrease in muscle strength (paresis) or lack of active movements (paralysis) first in the distal and then in the proximal joints, up to complete immobility of the limb. The proximal border of ischemic disorders depends on the level of occlusion and the degree of ischemia of the limb. Pain on palpation of ischemic muscles is observed with severe ischemia and is an unfavorable prognostic sign. Pain in the calf muscles is more common, and with high occlusion - in the thigh muscles.
Description of the disease
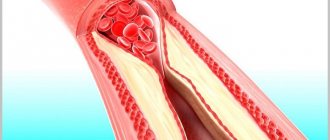
Atherosclerosis of the lower extremities is a disease that affects the endothelium (inner lining) of the blood vessels of the legs. This happens due to an imbalance in lipid metabolism. The main cause of both atherosclerosis of the aorta and leg arteries is a persistently and long-term elevated level of bad cholesterol in the blood. According to the international classification, atherosclerosis of the arteries of the legs has a code according to ICD 10: 170.2.
Plaques in blood vessels in the lower extremities
The disease manifests itself mainly in adulthood and old age, but its laboratory signs can be detected much earlier. Atherosclerosis can develop in the body for decades without showing any symptoms. The main arteries are most often affected. Gradually, the lumen of the vessel is closed by cholesterol plaques, and atherosclerosis takes on a wall-occlusive form. What's so special about her? In this clinical case, sclerotic masses mixed with lipids block the vascular lumen by more than half.
Simultaneously with this, destructive processes occur in the capillary sections of the circulatory system. Due to the occlusion of small collateral arteries, the trophism of the feet and joints is disrupted, and the clinical picture of the disease is formed.
Critical ischemia of the arteries of the lower extremities
Muscle soreness is a precursor to subfascial edema. Subfascial swelling of the leg muscles is a sign of severe ischemia of the arteries of the lower extremities; it is characterized by extreme density and does not extend above the knee joint. It can be total, covering all the muscles of the lower leg, or limited to the anterior or posterior group of muscles. Muscle contracture is the most dangerous symptom of critical ischemia of the lower extremities, which indicates the beginning of necrobiotic phenomena.
There are:
- Distal (partial) contracture , in which passive movements are impossible only in the distal joints;
- Total (complete) contracture , in which movements are impossible in all joints of the limb, which is in a state very similar to rigor mortis.