Thrombus is a blood clot formed in the lumen of a blood vessel under the influence of internal hemostasis. Formed as a result of pathological effects on the vascular endothelium. Represents a threat to the life and health of the patient. The formation of a clot in the vascular bed is called thrombosis.
A clot is a microscopic formation of irregular shape. Consists of several “components”:
- formed elements of blood;
- platelets;
- fibrin threads;
- plasma proteins.
How is it formed
Damaged vein endothelium triggers processes of internal hemostasis, activating coagulation factors.
Platelets and fibrin are sent to the damaged area. The resulting plug protrudes into the lumen of the vessel and does not cause harm.
Pathological processes occurring in the body, disturbances in blood composition, and other risk factors contribute to the growth of a blood clot.
Formed elements, cell particles and heavy plasma proteins cling to the neoplasm, and fibrin threads glue the cells together, forming a “growth” or clot. Subsequently, the clot can break off and wander throughout the systemic and pulmonary circulation.
Having established itself in a new location, the neoplasm continues to “cling” to blood elements. Blood flows through veins more slowly than in arteries, so clots form very quickly.
Thrombosis interferes with normal blood circulation, negatively affects the venous wall, changes the composition of the blood and contributes to the development of stagnation.
It is impossible to see a blood clot with the naked eye - it is a microscopic formation located in the lumen of a blood vessel.
How to treat thrombosis
A distinctive feature of thrombosis is the constant development of the disease. In other words, the clot never stops growing. It all starts with a microscopic tumor, which becomes larger and larger over time. As a result, the clot begins to create an obstacle to normal blood flow.
When a blood clot is detected in the leg, the symptoms are usually the following:
- pain in the affected area of the leg, which may intensify while walking;
- skin pigmentation;
- swelling of the limb;
- increased body temperature and chills.
In rare cases, the blood clot becomes visible visually. Sometimes you can even feel it under the skin. The area where the large blood clot appeared will have a blue skin color.
With thrombophlebitis of the deep veins in the lower leg area, as a rule, the patient develops a high temperature, the muscles swell, and every lowering of the leg is accompanied by unbearable pain. If you do not contact a specialist in time, the disease will begin to progress and a network of superficial veins will appear, and the skin of the lower extremities will acquire a bluish tint.
In cases where a blood clot develops in the femoral part of the leg, there is swelling of the skin, swelling of veins located close to the surface, as well as severe pain in the affected area. Symptoms such as blue discoloration of the limb and swelling of the veins located in the groin area cannot be excluded. In the case of a blood clot in the femoral vein, a strong increase in body temperature and fever may occur.
Phlebothrombosis, called deep vein thrombosis, is considered a high-risk disease. This can often be found in sick people who have to adhere to bed rest for a long time. Thrombosis may not affect the general condition of a person, but the consequences of a blood clot breaking off can be sad.
Thrombophlebitis is often associated with varicose veins. In this case, it is necessary to carry out diagnostics in time to avoid possible problems. With varicose veins, the presence of a blood clot can often be determined by palpation.
The greatest danger is represented by a blood clot formed on the main vein. In this case, it is very difficult to determine. Most often, the verdict is made only after the blood clot comes off and brings a lot of complications.
Pathology can be recognized only after complications appear. The first symptoms of thrombosis of the veins of the lower extremities are the following:
- feeling of constant heaviness and fatigue in the legs;
- swelling of the tissue;
- the appearance of pain in the legs;
- bluish skin tone;
- increase in the size of veins;
- pain when touching the legs;
- inflammation and enlargement of lymph nodes;
- temperature increase.

Such signs accompany thrombosis of arteries and veins.
This disease is divided into several types. A distinctive feature is the localization of blood clots. Blood clots in the legs located in the arteries are called arterial thrombosis of the lower extremities. This pathology is accompanied by:
- bursting pain;
- decreased sensitivity in the leg up to its complete loss;
- numbness of the limb, decreased tissue temperature in the affected leg;
- in severe cases, limb immobility appears.
If the blood clot is in the superficial veins, a diagnosis of thrombophlebitis (venous thrombosis of the lower extremities) is made. In this case, symptoms include:
- redness of the skin in the vein area;
- changes in the size and density of blood vessels (veins dilate and become denser);
- the appearance of pain during touching.
The first signs of thrombosis of the lower extremities appear weakly; the network of blood vessels does not yet appear on the skin. For this reason, it is extremely difficult to determine the symptoms of blood clot formation with the naked eye. Meanwhile, getting rid of the disease as quickly and effectively as possible is possible only through early detection of thrombosis of the veins in the legs. To do this, each person can conduct self-diagnosis. This procedure will be especially important for people at risk.
One of the first symptoms of a blood clot in the leg is painful veins. This can be checked by palpation. Palpation is carried out in a calm, relaxed state. You should start with the calf muscles, after which you can move higher. During self-diagnosis you should be wary of:
- the appearance of pain when pressing on soft tissues;
- legs look slightly swollen;
- the presence of nodules and compactions in soft tissues;
- slight redness in the area of the veins;
- The skin may be hot in some places.
You can detect signs of vein thrombosis in your leg at an early stage using a test. In medicine, it is called Homans' sign. The test involves dorsiflexing the foot. If pain occurs in the calf muscles, the test for the presence of a blood clot is considered positive. Similar symptoms are present in all patients with deep vein thrombosis.
Another stage of verification is a visual examination of the skin of the legs. When a blood clot forms, the skin around the vein takes on a bluish tint. Having identified such spots on your legs, you should undergo hardware diagnostics as soon as possible.
Under the influence of fast blood flow or some other reasons, a blood clot may move away from the vessel wall. This phenomenon in medicine is called thrombus rupture. From this moment on, the loose blood clot begins to wander through the veins and arteries. At any time, a clot can cause blockage of the lumen of a vessel (thromboembolism). Lack of blood flow in a particular part of the body leads to ischemia and tissue death.
If a blood clot breaks loose, the person needs immediate medical attention. Otherwise, there is a high risk of death. The challenge is to understand the manifestation of this condition in time. Symptoms of a blood clot leaving a vascular wall largely depend on which blood vessel was affected and in which part of the body it is localized.
When arterial blood clots break off in the legs, the following symptoms occur:
- the skin on the leg turns pale;
- local temperature decreases (feet become cold);
- sensitivity is lost;
- lameness occurs when walking;
- later, soft tissues and skin become blue and then black (necrosis occurs).
The complication of thrombophlebitis is accompanied by other first signs; when a blood clot breaks off, it causes:
- redness of the leg (caused by congestion and inflammation);
- severe pain;
- swelling;
- temperature increase.
If thrombosis of the vessels of the lower extremities is detected, the patient must be hospitalized. Not only the effectiveness of therapy, but also a person’s life may depend on the speed and professionalism of doctors.
Depending on the general condition of the patient, the degree of development of the disease and the location of the affected vessel, blood clots in the legs can be treated in several ways.
- Surgical intervention. This measure is an extreme measure and is most often performed in emergency mode.
- Drug therapy. This method is effective for eliminating the disease in the initial stages. With this effect, the blood clot can dissolve.
In addition to treating thrombosis, it is necessary to eliminate the cause of the disease. Otherwise, relapses are possible.
Many people at risk wonder what to do if a thromboembolism occurs. When there is a suspicion that a blood clot has broken off, you should not hesitate to go to the hospital. The first thing you should do is call an ambulance. After the examination, the decision on further actions is made by the doctor (attending) - how to treat thrombosis: with drugs or surgery.

You should not take any medications without a doctor’s recommendation, as this may distort the symptoms.
If a blood clot closes the lumen of a vessel, independent actions aggravate the condition.
You can get rid of blood clots in blood vessels without medications or surgery. This treatment regimen for thrombosis in the legs is prescribed to patients whose disease is at the initial stage of development. In this case, the main requirement is to eliminate the root cause of the disease.
In addition, in order to resolve a blood clot, it is important for a person with this diagnosis to pay attention to their habits:
- Active lifestyle. Regular physical activity helps eliminate blood clots in the veins of the legs.
- Proper nutrition. Excluding fatty, fried, salty and smoked foods from the diet slows down the formation of blood clots.
- Control of blood clotting.
- Bandaging a limb with an elastic bandage.
Unlike drug treatment, such measures do not provide quick results. It will take 1-2 years to cure leg thrombosis.
Medicines
Once a blood clot has been identified, doctors decide on therapy. If the pathology is discovered so late that it makes no sense to rely on independent resorption of the clot, doctors recommend drug therapy. This program uses ointments and tablets for thrombosis. An integrated approach is important:
- For arterial and venous thrombosis, dressings with heparin ointment are often prescribed. This drug promotes the resorption of already formed clots, reduces the production of thrombin and blocks the accumulation of platelets. Under the influence of the ointment, blood vessels dilate and internal inflammation is reduced.
- Antibiotics. If an inflammatory process has begun in the affected vascular bed (in a vein or artery), antibacterial agents are used to treat thrombosis of the vessels of the lower extremities. They block the action of pathological microorganisms and reduce the risk of complications of the disease.
- Anticoagulants for internal use. These drugs have a depressing effect on the blood clotting system. As a result, fibrin fibers and platelets stop layering on the clot. For arterial thrombosis of the lower extremities, Aspirin in small doses is often prescribed as an anticoagulant.
- Intravenous administration of Heparin. This procedure allows you to dissolve blood clots in a leg vessel in a short time, so it is often used for thromboembolism.
- Angioprotectors. To eliminate blood stagnation in the veins, angioprotective drugs are often prescribed. In this case, it becomes easier to cope with the symptoms of thrombosis. Among these drugs for thrombosis: Troxerutin and Hydroxyethylrutoside.
To combat blood clots in the veins of the legs during treatment, it is important to adhere to strict bed rest. In this case, the affected leg is fixed in an elevated position.
Causes
Often localized in the lower extremities. This is primarily due to the increased load on the legs.
Provoking factors are:
- bad habits. Change the composition of the blood;
- old age. Over time, blood vessels lose their former elasticity and become fragile;
- diseases of the endocrine system - especially diabetes;
- sudden weight gain. Increased pressure on the lower limbs;
- hypodynamic lifestyle, or vice versa – excessive physical activity;
- taking medications that affect blood composition;
- professional activity. Standing or sedentary work;
- cardiovascular diseases and poor nutrition.
In people with similar provoking factors, the formation of blood clots occurs several times more often.
The causes of a thickened venous clot include:
- genetic predisposition;
- tumor process of a malignant or benign nature;
- systemic blood diseases that disrupt homeostasis;
- thrombocytosis;
- metabolic disorder;
- hormonal imbalances;
- history of trauma, fractures, abdominal surgery;
- muscle atrophy;
- paralysis;
- the presence of another disease of the vascular system, such as varicose veins;
- purulent processes;
- infectious processes with an increased risk of developing bacteremia.
In combination with provoking factors, the process of thrombus formation accelerates, and new foci appear.
Over time, the clots become heavier and break off completely or in parts with the flow of blood.
A detached blood clot can cause a lot of trouble and cause death.
How exactly does a leg hurt due to a blood clot?
There are several classifications of thrombosis that give an idea of the nature of the pathology.
All types differ in symptoms and approach to treatment. Types of thrombosis:
- primary (phlebothrombosis) can lead to dangerous consequences, characterized by fragile attachment of the blood clot to the wall of the vessel, which is fraught with sudden detachment;
- secondary (thrombophlebitis) is characterized by strong fixation of the clot, a low probability of separation, the pathological process is of an inflammatory nature.
Classification based on the etiological parameter of the disease - the cause of its occurrence:
- congestive thrombosis of the veins in the legs is caused by compression, as a result of which the outflow of blood is disrupted;
- inflammatory thrombosis is caused by injuries, infections, allergies;
- hemostatic thrombosis is observed when blood coagulation functions are impaired.
Classification of thrombosis based on the nature of the connection between the clot and the venous wall:
- occlusive thrombosis (the lumen of the vein is completely closed);
- parietal (there remains a lumen through which blood flow occurs);
- floating thrombosis (large thrombus size, reaching 20 centimeters, this type is especially dangerous with a high risk of rupture);
- multifocal - the formation of clots in different places.
Depending on the nature of the course, the following forms of thrombosis are distinguished:
- spicy;
- subacute;
- chronic.
Complications and prognosis
Acute deep vein thrombosis has a different prognosis depending on the type of clot. The occlusive form of the disease is not dangerous, since the thrombus is tightly attached to the wall of the vessel. Parietal thrombosis is also not dangerous. The only risk is its continued growth and transition to a floating thrombus.
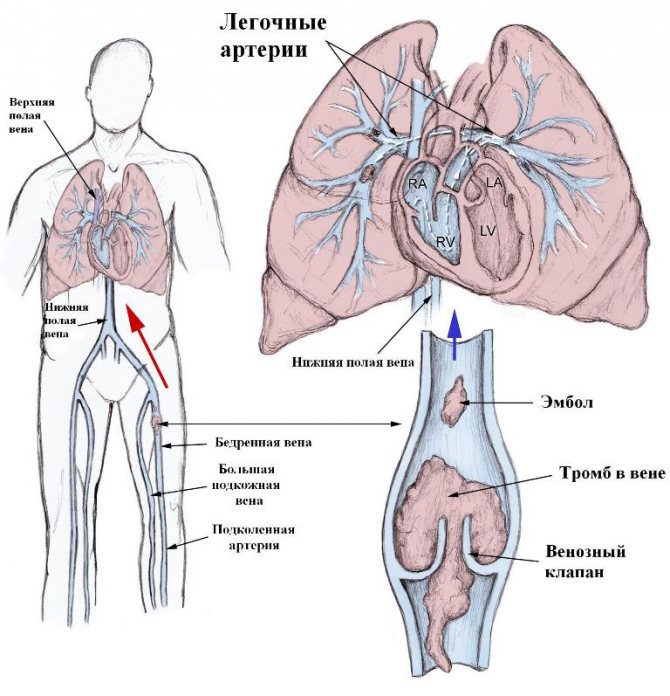
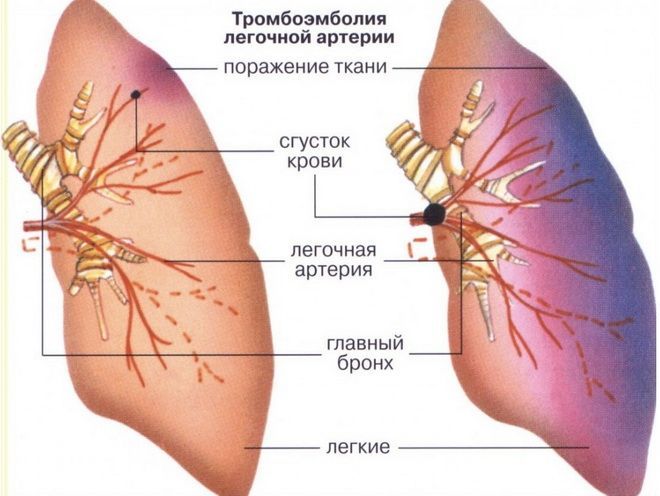
This form of the disease is life-threatening. Pulmonary embolism occurs as a result of part of the blood clot breaking off and reaching the lungs through the bloodstream. Blockage of the pulmonary artery causes the development of acute failure of the respiratory and cardiovascular systems. If a blood clot blocks a small vessel, a pulmonary infarction develops.
Within several years after the illness, many patients, as a result of damage to the walls of blood vessels and valves, develop postthrombotic syndrome, in which there is a high risk of complications in the form of the formation of new blood clots in the veins of not only the lower but also the upper extremities.
Another long-term consequence of the disease is the development of chronic venous insufficiency due to damage to the valves. The increased load on the superficial veins as a result of the redistribution of blood flow leads to their expansion and accelerated development of insufficiency of these vessels.
Inflammatory diseases, eczema, and dermatitis appear on the skin. Typically, trophic ulcers develop; the skin becomes thin and prone to damage.
Rehabilitation after DVT
Rehabilitation of patients after deep vein thrombosis is needed to solve three problems:
- prevention of re-development of the disease;
- prevention of the development of postthrombophlebitis disease;
- compensation of venous outflow.
Main methods of the rehabilitation program:
- regular physical activity;
- time limit for static vertical stay of the body;
- use of compression hosiery.
Rehabilitation is an important process. If you omit it, then the risk of the disease returning in a more complex form is very high.
Doctors emphasize that without a rehabilitation program it is impossible to talk about a complete victory over deep vein thrombosis.
After the illness, the patient enters a period of postthrombophlebitic disease. In the absence of the necessary rehabilitation measures, there is a risk of developing symptoms of chronic venous insufficiency: edema, varicose veins, trophic disorders, as well as the likelihood of recurrent thrombosis. In this regard, it is important to constantly monitor the patient's condition.
A set of rehabilitation measures after deep vein thrombosis:
- course of coagulants;
- use of phlebotonics 1.5 months annually;
- maintaining moderate physical activity;
- eliminating bad habits;
- physiotherapy.
A set of rehabilitation measures allows you to maintain the patient’s quality of life and avoid relapse of the disease.
Signs of deep vein thrombosis
About half of those patients who were found to have blood clots had very few symptoms or none at all.
Although asymptomatic blood clot formation is usually a sign that the thrombosis has not yet reached a serious stage, this is not always the case. Even large blood clots that require immediate surgery may sometimes cause no symptoms at all until the clot breaks off and travels through the bloodstream.
This is one reason why it is extremely important to try to prevent blood clots, especially if you are at risk.
Skin redness
Slight discoloration of the skin in the area of blood clot formation is often one of the first signs. The reason is quite simple: dense collections of blood under the surface of the skin become noticeable as they grow in size.
If you constantly develop red spots on your right and left legs, especially after an injury or surgery, consult a doctor immediately. The great thing about deep vein thrombosis is that they do not go away over time.
Painful swelling may occur at the site of blood clot formation, especially in the ankles and calves. These areas of the body have increased bone and tissue density, which makes it difficult for the body to naturally clear clots that have already formed.
//www..com/watch?v=b6rlWwEK37c
One sign that swelling may be due to a blood clot is that it will not respond to conventional treatments, such as hot or cold compresses. The tumor can also intensify for no apparent reason and appear without external damage.
Fever, itchy skin
The skin near the affected area may be warm and itchy. Sometimes this may be accompanied by tingling and throbbing.
Like other symptoms, they tend to respond poorly to home remedies and get worse over time if left untreated.
Fainting
Fainting and dizziness can occur when the body is unable to naturally dissolve a clot on its own or when it breaks loose and travels to the lungs. In this case, breathing may be difficult.
Dizziness may be most severe if you stand up abruptly after sitting or lying down for a long time (orthostatic hypotension), and due to the nonspecific nature of this condition, many people do not associate it with the possibility of blood clots.
Loss of consciousness is a serious symptom for which you should definitely consult a doctor.
As the blood clot grows, the body will try to get rid of it, and vital organs, such as the heart, will work and pump blood harder, which will lead to an increased heart rate.
Abnormalities in heart function may also indicate that a blood clot has left your leg and traveled to other parts of the body. In this case, other symptoms may appear, for example, sharp stabbing pain in the chest, which intensifies when inhaling.
The course of any pathology leads to the fact that the body's defense systems will work overtime, which can lead to fatigue or exhaustion.
Like many other symptoms of deep vein thrombosis, fatigue can be nonspecific and the underlying cause can be difficult to diagnose. So if you often feel low on energy, it's important to be on the lookout for other symptoms.
The hallmark of weakness associated specifically with blood clots is that you will feel it for no apparent reason.
We suggest that you familiarize yourself with Red dots on the legs
Foot pain
Vein thrombosis can also cause pain in one or both feet.
Because this symptom does not appear directly in the lower leg or thigh area (the typical location of a blood clot), patients often cannot make the connection between the two.
Feet hurt because a blood clot in the leg is restricting or blocking blood flow to the area. As a result, the foot tissues do not receive enough oxygen from the blood, which causes pain.
Calf pain
Quite often, patients mistake this symptom for a muscle cramp or strain, so they ignore it.
The pain caused by deep vein thrombosis is usually most noticeable when you walk and bend your leg.
Skin discoloration
As mentioned earlier, the hallmark symptom of blood clots is persistent redness in the area where they form, but this is not the only skin discoloration that can occur with this condition.
As a result of their formation, the ankles or feet may become pale due to reduced blood flow to the area. As the pathology develops, the affected area acquires a bluish (blue) tint, becomes colder to the touch, and becomes numb.
Deep vein thrombosis has several specific symptoms, but can also be asymptomatic. A problem with blood circulation is indicated by:
- severe swelling at the site of blockage of the vessel;
- changes in skin color, often throughout the entire limb;
- unexpressed pain, which intensifies with load on the legs;
- a noticeably warmer or hotter leg with thrombosis (hyperthermia).
Asymptomatic cases are more dangerous. Due to untimely treatment, the disease can develop into serious complications, causing irreversible consequences.
One of the most striking signs of the rapid development or complication of deep vein thrombosis is local hyperemia. It is impossible to accurately measure the temperature of the leg, but it is tactilely felt that one limb is warmer than the other.
This sign is a reason for immediate hospitalization in order not to miss further complications, in particular pulmonary embolism.
Source: //sitactive.ru/bolyat-veny-nogakh-tromboze/
Classification
Thrombosis occurs in deep and superficial vessels, lower and upper parts of the body.
The pathological process is asymptomatic for a long time, disrupting the circulatory system and deforming the walls of the veins.
There are several types:
- Parietal is the most common type of clot. The thrombus attaches to the endothelium and is held to the membrane by sprouted fibrin threads.
- Oblong is a type of parietal neoplasm. The free edge becomes thinner and gradually peels off, moving with the blood flow.
- Mixed - consists of white and red elements and is capable of movement.
- Central - secured with cords, preventing normal blood supply.
- Occlusion – blocks the vascular bed not partially, but completely. The most dangerous type of thrombosis.
- Obliterative - a formation that blocks a blood vessel by 95%.
All types of blood clots are dangerous because they are capable of breaking away from the endothelium.
How to warn?
Prevention of thrombosis consists of maintaining normal physical activity, getting rid of bad habits and leading a healthy lifestyle. The disease can be triggered by excess weight, smoking and physical inactivity. The patient’s diet is also important, since excessive cholesterol consumption harms blood vessels and aggravates the development of pathology. You need to avoid sitting and exercise your leg muscles, this will help prevent dangerous symptoms of arterial thrombosis.
Why is it dangerous?
The presence of a blood clot in the lower extremities is not always accompanied by clinical manifestations, so a person may not be aware of the existing pathology. Over time, vascular thrombosis leads to irreparable losses.
Having partially blocked the lumen of the vein, the clot prevents normal blood supply to the tissues.
Acute hypoxia develops, mitotic cellular processes stop. Leg pain and fatigue occur. Symptoms appear indicating the development of a pathological process.
A formation that completely blocks the lumen of a vessel entails negative consequences, which, if left untreated, become fatal:
- blood flow disturbance;
- oxygen starvation of cells and tissues;
- pain in the legs increases;
- Due to the usual blood flow, a blood clot can break off and enter the arteries through the main vessels, clogging vital organs.
Lack of therapy leads to loss of functionality, acute hypoxia occurs, and tissues gradually die. Gangrene develops.
Venous thrombosis of the vessels of the legs: from the first signs and prevention to the fight against the disease
Levchenko Lydia, edited by first category doctor Z. Nelly Vladimirovna
Deep vein thrombosis of the lower extremities is a very serious disease, and it is often asymptomatic. But if the symptoms of the disease are not recognized in time and treatment is not carried out, the consequences can be very serious, not excluding death.
With thrombosis of the veins of the lower extremities, blood clots or blood clots form in their cavity, which interfere with the normal movement of blood. Over time, they can clog the venous lumen and even come off. If there is a disturbance in the movement of blood, where the supply is disrupted, then the tissues can die.
If a blood clot breaks away from a vessel, it can end up in the heart, lungs, and other organs. Accordingly, this is dangerous because a stroke, thromboembolism or heart attack may occur, and these diseases lead to sudden death or paralysis.
How to find out if a person has blood clots in the body in the vessels: symptoms, signs
Thrombus
A thrombus is a blood clot that has completely or partially closed the lumen of a vessel, formed due to stagnation of blood in various organs. Thrombosis is a disease in which the presence of blood clots in the human body is confirmed by a doctor.
Important: This diagnosis should only be made by a doctor. If you notice the first signs or symptoms, you should immediately consult a doctor.
So how can you tell if a person has blood clots in their blood vessels? Some symptoms indicate this, but depending on the location of the blood clot in a particular organ, they vary significantly. Signs of blood clots in the body and their location:
- In the brain it can cause dizziness, headaches, and fainting.
- In the lower extremities - swelling, bluish skin, bruising.
- In the heart - pain in this organ, arrhythmias, ischemic heart disease, hypotension, shortness of breath, numbness of the hands.
- In other organs there will also be noticeable disruptions in their functioning.
The very presence of blood clots in the body is usually without symptoms, and the person feels unwell only in the organ where the blood clot is located. The worst thing is a complication, namely the detachment of a blood clot.
Remember: In such cases, there is a high probability of disability and death. The process occurs rapidly, in most cases minutes count - heart attack, stroke, pulmonary embolism, failure of other organs.
In such cases, a person needs urgent medical attention. The administration of necessary medications should be carried out as soon as possible and only by qualified personnel to avoid complications.
Degrees of the disease
Symptoms of limb damage do not appear immediately; they increase as the disease progresses. The clinical picture depends on the degree of disruption of blood flow in the tissues. If the patient does not receive qualified assistance, then thrombosis of the arteries of the lower extremities goes through all stages.
- zero degree – absence of symptoms at rest, pain may occur during sports or physical activity;
- IA - coldness, numbness;
- IB – pain occurs;
- IIA – numbness intensifies, impaired motor function occurs;
- IIB – the leg completely loses sensitivity;
- IIIA – swelling occurs, necrosis begins;
- IIIB – partial muscle contracture;
- IIIB – complete contracture – all muscles of the affected limb become hard and immobile;
- IV – gangrene.
How to determine whether there are blood clots in the legs, is a blood clot in the leg dangerous?
Thrombus A thrombus is a blood clot that completely or partially blocks the flow of blood in the vessels. Thrombophlebitis or thrombosis is the presence of a blood clot in the vessels of the legs. Is a blood clot in the leg dangerous? It all depends on the complexity of the disease and the location of the blood clot. There are diseases associated with the formation of blood clots:
- Thrombophlebitis, thrombosis - causes inflammation and subsequent necrosis of nearby tissues, the temperature of the affected area is usually increased.
- Phlebothrombosis is when one or more blood clots are located in the veins of the lower extremities. With this disease, the temperature of the affected area is normal or the limbs may even be cool.
- Thrombosis can be arterial or venous . The difference lies in the mobility of the formed blood clots. So, in the first case, the probability of mobility of clots is high. In the second, it is practically reduced to zero, due to the lack of pressure and the presence of valves in the veins, which are an additional barrier to the mobility of blood clots.
A blood clot in the leg is dangerous because it poses a health threat. If a doctor diagnoses such a disease, the patient is first prescribed drug treatment, so that the blood clot should resolve on its own. If this does not happen, blood clots are “broken” using modern technologies: laser and other techniques.
How to determine if there are blood clots in the legs:
- A person may suspect this disease if he has swelling and cyanosis, usually of one leg.
- Only a doctor can diagnose the presence or absence of the disease using ultrasound.
- If the diagnosis is confirmed, treatment is prescribed.
Remember: All of the above diseases are dangerous, because if left untreated, they can lead to gangrene, and ultimately the loss of a limb.
In addition, with the blood flow, clots can move to other organs and cause their failure and lead to death.
Treatment
Thrombophlebitis is treated using conservative or surgical methods. The choice of a specific treatment method depends on the stage of the pathological process and the general condition of the patient.
Conservative treatment
Thrombophlebitis takes a long time to treat - at least six months. The patient is prescribed medication (heparin injections). The course of treatment with heparin is 10 days or more. The patient is prescribed thrombolytic and anti-inflammatory drugs.
If thrombophlebitis is severe, the patient is prescribed bed rest for the first week. When the acute stage of thrombophlebitis subsides, the doctor prescribes the patient a course of therapeutic exercises.
Surgery
There are four types of surgical intervention for thrombophlebitis:
- Fogarty catheter. During surgery, a probe is inserted into the veins to remove the clot. The method is used at the initial stage of thrombophlebitis (up to 5 days from the moment of exacerbation of the disease).
- Installation of a vena cava filter in the inferior vena cava. The filter is designed in such a way that it does not allow the blood clot to move through the veins.
- Plication. The task of plication is to stitch the vein with special metal staples.
- Thrombectomy. The most common method of surgical treatment of thrombophlebitis. During the operation, the clot is removed from the vein. In order to prescribe the operation, a mandatory condition must be met: the blood clot occurred no later than 7 days ago. If the thrombus is older, deformations have already occurred on the vein walls and venous valves, which will greatly reduce the effectiveness of the operation.
Source: //AptekaTamara.ru/bolezni/tromb-v-noge-simptomy.html
Symptoms
There are specific symptoms:
- swelling of the limbs;
- soreness and increased fatigue of the legs;
- color change;
- compaction on palpation.
Signs indicating complete blockage of the vessel:
- bluish skin;
- pale skin;
- headache;
- numbness and sensation of “running goosebumps”.
It is not possible to diagnose the disease based on external manifestations.
To do this, a series of diagnostic procedures should be carried out. The determining factor for the presence of a clot is the swelling and glossiness of the leg below the blocked vein.
Signs of the disease intensify gradually, but quickly.
Factors of occurrence
The causes that provoke the development of the disease (ICD code 10 I 80) are divided into 3 factors:
- Thickening of the blood due to changes in its composition.
- Reducing the speed of blood flow.
- Damage to the inner lining of blood vessels.
These factors are diagnosed individually or in combination. They contribute to the development of varicose veins, which is the cause of acute thrombophlebitis.
Vein thrombosis is a rather dangerous disease that can be fatal if a blood clot breaks off and enters the arteries of the lung or heart.
Thrombophlebitis (ICD code 10 I80) develops with forced immobility of a limb (with a fracture).
Thrombosis of the veins of the lower extremities is caused by taking estrogen-containing hormones prescribed for infectious and autoimmune diseases. Oncological diseases provoke thrombophlebitis of the lower extremities. Installation and long-term presence of a catheter in the venous bed and frequent injury to the walls by injections lead to the formation of blood clots.
In 65% of cases, thrombophlebitis is diagnosed in women. The pattern is associated with wearing high-heeled shoes, tight jeans and taking hormonal contraceptives. The cause of the disease may be pregnancy. During this period, physiological activation of coagulation processes occurs, preventing bleeding in the postpartum period, and the inflamed vessel wall leads to the formation of a blood clot. People aged 40-55 years are at risk. At this age, the condition of the body's vascular system deteriorates significantly.
Thrombosis is hereditary. Causative factors include obesity, unbalanced diet, physical activity, smoking and drinking alcoholic beverages.

Deep vein thrombosis has a specific code in the ICD-10 classification – I80
Diagnostic methods
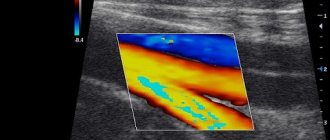
Identifying the location of a blood clot in the legs and determining its type is the main task of diagnosing venous disease.
Modern methods allow you to detect a blood clot:
- duplex scanning of veins;
- radiography;
- angiography;
- installation of a vena cava filter (trap).
Morphological features can be examined using ultrasound diagnostics. A special place in diagnosis is occupied by a coagulogram and determination of the concentration of D-dimer.
Mandatory diagnostics include blood sampling for a general analysis, hemostasiogram, determination of the duration and time of bleeding, and biochemistry.
Once the diagnosis is made, treatment begins immediately.
Blood clot in the leg: causes, symptoms, treatment and consequences
One of the most common types of circulatory disorders in the vessels of the lower extremities is acute venous occlusion. A blood clot in the leg, the symptoms of which indicate a vascular blockage, can provoke a deadly situation associated with the cessation of heart function. It is necessary to call emergency assistance as quickly as possible at the first signs of thrombosis of the veins of the lower extremities.
When a blood clot has formed in the vessels of the legs, it is strictly unacceptable to self-medicate: thrombosis of the lower extremities must be treated by a phlebologist or vascular surgeon
.
Venous blockage
Vascular thrombosis of the lower extremities is a significant risk factor for dangerous thromboembolic complications, regardless of the location of the occlusion. All variants of venous blockage are conventionally divided into 2 types:
- Occlusion in the superior vena cava system;
- Blockage of the vessels of the inferior vena cava.
Blood clots in the veins of the legs are always a lesion of the venous network of the inferior vena cava, when a blood clot forms in the lumen of one of the many vessels. The presence of a blood clot causes blood flow to slow down and the clot's size to gradually increase.
At the first stages of the pathological process there will be no external signs, but as the condition of the lower extremities worsens, the symptoms of the disease appear. It is extremely difficult to recognize a blood clot in deep veins, but when superficial vessels are affected, it is quite possible to determine the presence of a blockage.
You need to know what thrombosis of the veins of the lower extremities is in order to consult a specialist in time and prevent deadly complications.
Deep vein thrombosis of the legs
Variants of occlusal lesions
The basis for thrombotic problems are the following types of vascular diseases:
- Varicose veins of the saphenous veins of the lower extremities;
- Thrombophlebitis affecting superficial or deep vascular trunks;
- Postthrombophlebitic syndrome.
With any type of pathological changes in blood vessels, conditions are created for complete or partial closure of the lumen of the veins. Leg problems are most easily identified by occlusive thrombosis of the great saphenous vein.
Against the background of deep thrombosis of the leg, the severity of symptoms is low. In any case, against the background of varicose veins, one must carefully monitor the external manifestations of the disease, even if there are no signs of vein thrombosis.
Manifestations and symptoms
In each specific situation, it is necessary to monitor the presence of symptoms depending on the disease. Leg thrombosis can be suspected if the following signs are present:
- Leg pain regularly when walking;
- against the background of exercise or at rest, pain in the groin appears in women and men, or discomfort along the inner surface of the thigh;
- swelling of the foot or leg occurs;
- skin color changes, especially in areas of dilated veins;
- body temperature rises.
All types of occlusive vein lesions have their own characteristics: it is important to know what the symptoms of thrombophlebitis are and what are the first signs of thrombosis.
Varicose veins of the legs
Problems with veins most often occur in women. Typical manifestations of the disease include the following symptoms:
- external changes in the skin of the legs associated with the appearance of dilated and tortuous veins;
- pain syndrome of varying severity (from pulling sensations to severe pain after physical activity);
- the appearance of cramps in the lower legs, mainly at night.
In the absence of complications, varicose veins of the legs are a cosmetic problem and a risk factor for thrombosis. It is extremely difficult to independently understand when the situation worsens and what a blood clot on the leg looks like, so if pain appears or worsens, you should immediately consult a doctor.
Complicated varicose veins
The inflammatory process in varicose veins creates conditions for dangerous complications: timely diagnosis of thrombophlebitis of the lower extremities is the main factor in the prevention of severe blood flow disorders in the legs associated with blockage of blood vessels. Thrombophlebitis is characterized by the following symptoms:
- increase in general body temperature;
- maintaining normal temperature of the sore leg;
- bluish tint of the skin due to dilated small saphenous veins;
- severe pain in the legs when moving and at rest;
- tissue swelling.
Detection and treatment of acute thrombophlebitis of the saphenous veins should be carried out in a hospital setting: it is strictly unacceptable to self-medicate using ineffective traditional methods.
Occlusion of the sural veins
The most common location of primary thrombosis of the leg is the system of sural (deep) veins of the leg. Typical signs of a blood clot in the leg are:
- pain of varying severity in the calf area at rest and when touched;
- swelling of the feet and ankles;
- feeling of internal distension of the lower limb after a working day.
Thrombosis of the veins of the lower leg is difficult to identify, therefore, if complaints persist, it is necessary to visit a doctor in a timely manner and conduct a full examination.
Thigh vein thrombosis
Blockage of the great saphenous vein of the thigh is manifested by the following clear signs:
- severe pain, as if the veins in the legs hurt;
- femoral-ankle edema;
- cyanotic skin tone with dilated superficial veins;
- intermittent pain in the groin.
Often, it is the pronounced pain syndrome during thrombosis and the appearance of a tortuous mesh of dilated vessels that helps make an accurate diagnosis.
The highest risk of developing pulmonary embolism occurs when a blood clot forms in the venous plexuses of the pelvis and thigh, so it is necessary to monitor the condition of the vascular system of the lower extremities and carry out preventive therapy in a timely manner.
Diagnostic principles
A vascular surgeon or phlebologist knows how to detect a blood clot and what to do if there is a high risk of thromboembolism. The basis for successful diagnosis is timely contact with a specialist. In addition to a standard examination and special tests, the doctor will order the following studies:
- Laboratory determination of the state of the blood coagulation system using a coagulogram;
- Triplex ultrasound scanning;
- Impedance plethysmography (determining the volume of accumulated venous blood in the vessels of the legs);
- Thermography (assessment of temperature reaction in different parts of the sore leg);
- Phlebography (x-ray contrast method that helps detect leg thrombosis);
- Tomography (CT or MRI) is performed according to indications at the stage of preparation for surgery.
At an appointment with a phlebologist
The purpose of a complete examination is to determine the presence and location of occlusion. In addition, the doctor needs to accurately find out the possibility of complications and the risk of thromboembolism: knowing the dangers of leg thrombosis, it is important to treat thrombosis of the lower extremities, taking into account the sudden deterioration of the condition and the appearance of symptoms of blockage of vital vessels.
Treatment tactics
If an occlusive lesion is detected in the veins of the legs, effective therapy must be started as early as possible. Depending on the type of disease and the severity of blood flow disorders, 2 main treatment methods are used:
- Medication;
- Surgical.
The doctor knows how to treat thrombosis, so you should listen to the specialist and carefully follow all the advice and recommendations of the phlebologist.
Drug treatment
The mandatory and most important tasks of conservative therapy include:
- restoration of vessel patency and improvement of venous blood flow;
- preventing further increase in the size of the formed blood clot;
- prevention of repeated episodes of vein blockage;
- eliminating the risk of blood clot rupture and preventing deadly types of thromboembolism;
- prevention of the chronic form of the disease – postthrombophlebitic disease.
The main and most effective type of medicine is anticoagulants, with which the doctor can reduce the size of the intravascular clot and prevent the risk of dangerous types of thromboembolism. In addition, in complex therapy, droppers with solutions that reduce blood viscosity and various options for vascular drugs are necessarily used.
Surgical treatment
The goal of surgery is to eliminate the occlusion. Thrombectomy is performed through an open approach, but only in emergency situations.
Two options are used: complete thrombectomy and partial (palliative). In some cases, it is necessary to perform a vascular anastomosis to restore normal blood flow in the limb.
For each patient, the doctor will select the treatment method individually.
Planned intervention involves the use of minimally invasive methods performed under the control of venography.
Thrombectomy
Endovascular surgical options (thrombolysis, vena cava filter) help minimize the risk of complications during surgery and successfully remove a clot from the venous system of the legs. In the postoperative period, it is necessary to continue drug treatment, the duration of which can be several months. Medical supervision will be required throughout the entire course of therapy.
Treatment
Thrombosis of the lower extremities is treated in several ways. Therapy depends on the severity of the pathological process and clinical manifestations of the disease.
Drug therapy is the use of drugs with thrombolytic, antispasmodic and anti-inflammatory effects. Therapy is supplemented by oral administration of anticoagulants and steroid glucocorticoids.
The affected limb should be fixed and elevated no more than 25-30 cm.
Surgical methods of treatment:
- excision of the damaged vessel;
- cavity clot removal;
- venous plication;
- setting a trap.
Thrombolysis is the melting of clots using special lysis solutions that are injected into the affected vein.
The most effective method for wandering blood clots is the installation of a vena cava filter, which catches parts of the clots, preventing them from spreading.
The first signs of thrombophlebitis by type (photo)

Based on the location of the source of inflammation, doctors diagnose:
- thrombophlebitis of superficial veins;
- pathology of deep-lying venous vessels (otherwise called phlebothrombosis).
The clinical picture depends on the rate of development of painful signs of thrombophlebitis:
- Acute thrombophlebitis is diagnosed quite rarely, severe symptoms increase and reach a peak already on the 2nd day;
- Subacute course - often observed with damage to deep veins, signs of thrombophlebitis are less intense and develop in waves;
- Chronic thrombophlebitis - foci of inflammation occur periodically, and their localization may change (migrating thrombophlebitis).
Symptoms of thrombophlebitis and their intensity depend on the depth of damage to the venous system and the location of the pathological focus.
Thrombophlebitis of the saphenous veins of the legs

Thrombophlebitis of the saphenous veins of the legs photo 2
Often, damage to the veins of the lower extremities is caused by a long course of varicose veins. Thrombophlebitis of varicose veins can be suspected by the deterioration of the patient's condition. Characteristic features:
- bursting pain in the affected leg, some relief comes from raising the affected limb higher (put it on a chair, raise the leg to the wall in a lying position);
- the appearance of a purplish-cyanotic area above the site of the lesion, the skin below the thrombosis becomes pale;
- the appearance of a venous pattern due to the expansion of veins;
- against the background of a general increase in temperature to 38ºC, the affected limb remains cold.
Prevention
Preventive measures include increased attention to foot health.
If you have a tendency to develop the disease, you should eat right, do special exercises and wear compression garments. For all others, the standard requirements are:
- taking medications and vitamins;
- walking;
- massage and water treatments for feet;
- wearing comfortable shoes and loose clothing;
- quitting smoking and hormonal medications.
Treatment of pathology
The basis of therapy for acute obstruction is surgical intervention. It involves removing the blood clot, and if necrotic tissue changes develop, amputation of the limbs is performed. Drug therapy consists of taking large doses of No-shpa or Drotaverine, which will help eliminate vascular spasm as much as possible. It is also recommended to administer Heparin in high doses. Antiplatelet agents and other agents that reduce the likelihood of blood clots are indicated.
For ischemia, conservative therapy is carried out, which helps to partially increase blood flow in the vessels. For this purpose, direct and indirect anticoagulants are used, antispasmodics and thrombolytics are administered intravenously. It is important to normalize metabolic processes in the body. The use of non-traditional methods in the form of herbal medicine is also recommended.
Drug treatment of thrombosis continues for a long time and is not always effective.
Forecasts
The most dangerous condition is the detachment of a neoplasm. An embolus (part of a detached blood clot) wanders around the blood circulation, damaging the endothelial layer of blood vessels and clogging the main vessels.
When it enters a vein of smaller diameter, the blood clot clogs the vessel, preventing blood supply to tissues or organs. Blockage of the pulmonary artery leads to thromboembolism with subsequent death.
By blocking the vessels of the brain and heart, a stroke and heart attack occur, respectively.
Timely treatment eliminates the occurrence of undesirable consequences and severe complications of the disease.
Causes of blockage
In 95 cases of blockage of the arteries of the lower extremities out of 100, thromboembolism is recorded - thrombosis caused by blood clots (emboli) brought from large vessels - and atherosclerosis. In this case, the “culprit” in the formation of a blood clot is almost always the heart (diseases: atherosclerotic cardiomyopathy, mitral stenosis, extremely rarely - acute myocardial infarction, septic endocarditis, cardiosclerosis - post-infarction or diffuse).
Only in 5 cases out of 100, emboli are formed due to atherosclerotic plaques and aortic aneurysm; even less often, the cause can be thrombosis of the pulmonary artery or the formation of a malignant tumor in the lungs.
Other probable causes of arterial embolism of the lower extremities include:
- artificial heart valve installed in the patient;
- thyrotoxic cardiopathy;
- atrial fibrillation.
There are only 3 causes of thrombosis of the arteries of the lower extremities:
- Reduced blood flow speed. This is observed with arterial hypotension, as well as after operations.
- Violation of the integrity of the artery. Moreover, if the outer shell of the vessel is damaged, there is nothing to worry about. The process of enhanced thrombin production is triggered only when the intima, the inner lining of the vascular bed, is damaged.
- Acceleration of the blood clotting process. Occurs with thrombophilia and erythremia.