Author: Svetlana Viktorovna Shishkanova, head of the independent veterinary laboratory “Poisk”, St. Petersburg.
Leukogram
(leucogramma; leuko- + Greek gramma - record) or
leukocyte formula
is the percentage of different types of leukocytes, determined by counting them in a stained blood smear under a microscope. The leukogram gives an idea of the balance between the production of leukocytes in the bone marrow, their distribution in the vascular system and emigration from the blood vessels into the tissues. There are two methods for calculating the leukogram: manual (using a stained blood smear under a microscope) and automatic (using a hematology analyzer). In veterinary medicine, the manual counting method is considered the most accurate compared to the automatic method. The manual method allows not only to differentiate different types of leukocytes, but also to determine changes in cell morphology, the appearance of neutrophil toxicity, the presence of atypical cells, cell aggregates, and blood parasites. When examining a stained blood smear, a laboratory doctor must remember the uneven distribution of leukocytes in the smear: lymphocytes take a central location, neutrophils take a marginal location, and therefore, when calculating the leukogram, it is necessary to capture both the central and marginal zones of the smear.
When interpreting the leukogram of a German shepherd, we see pronounced leukocytosis and relative lymphopenia; in the Yorkshire terrier, on the contrary, moderate leukopenia and relative lymphocytosis. However, if we compare the absolute values of lymphocytes of both dogs, they will be the same and correspond to the normal variant. The percentage of leukocytes is needed only to calculate absolute numbers. A leukogram with only the percentage of leukocytes can mislead the veterinarian. The absolute value is calculated by multiplying the percentage of cells of a given type by the total number of leukocytes in the animal and dividing by 100. Approximately focusing on the percentage of cells can only be done if the level of leukocytes in the animal is within the reference interval.
When interpreting a leukogram, the veterinarian should ask himself the following questions:
– Is there inflammation here? – Is there any effect of glucocorticoids (stress)? – Is there any influence of adrenaline (excitement, excitement)? – Are there necrotic tissue lesions? – If there is inflammation, can it be classified? – Is there systemic toxemia?
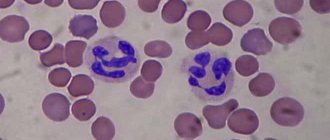
Leukocytosis and neutrophilia
In most cases, the concepts of leukocytosis and neutrophilia are synonymous. They are characteristic of the inflammatory process. The duration and severity of the inflammatory process, as well as the response of the bone marrow to infection will determine the degree of neutrophilia and the possibility of immature forms (band neutrophils, metamyelocytes and myelocytes) appearing in the blood - a shift to the left. A shift to the left is indicated when the number of band neutrophils exceeds more than 1.0x10⁹/ l, which is typical for acute inflammatory processes. A less pronounced shift to the left (0.3–1.0x10⁹/l) is characteristic of chronic and granulomatous processes. There are regenerative and degenerative shifts of the nucleus to the left. With a regenerative shift, mature neutrophils predominate in the blood; it is assessed as an adequate response of the bone marrow to a damaging effect. With a degenerative shift of the nucleus to the left, the number of immature neutrophils is greater than mature ones, and the total number of leukocytes is within normal limits or reduced. A degenerative shift indicates an acute inflammatory process that exceeds the ability of the bone marrow to supply the need for mature neutrophils. At the beginning of the inflammatory process, neutrophilic leukocytosis and a pronounced nuclear shift to the left occur. As the segmented neutrophils that existed in the bone marrow maturation and storage depot are depleted, band neutrophils and metamyelocytes are released. Over time, myeloid hyperplasia in the bone marrow will increase the production of neutrophils. The release of mature cells into the blood will increase and the severity of the left shift will decrease. Once tissue inflammation has stabilized at a sustained low level, the bone marrow should achieve a sufficient rate of neutrophil production so that most of them can mature before being released into the circulation. Thus, during a chronic inflammatory process, leukocytosis is not observed, and a shift to the left is insignificant or absent. Chronic inflammation is difficult to detect with a general blood test. If the need for neutrophils is very strong, hyperplasia of the granulocytic lineage may be observed in the bone marrow, without being reflected in the form of neutrophilia in the peripheral blood. For example, with pyometra in dogs, there may be a normal or slightly elevated white blood cell count and a moderate (to strong) shift in the white blood cell count to the left. After surgery, such animals may experience rebound neutrophilia, reflecting the degree of neutrophilia of the granulocytic lineage. It typically takes about a week for these dogs' blood profiles to return to normal. Persistent neutrophilia should be investigated for the presence of a focus of chronic inflammation, abscess, necrosis, and tumor. In such cases, it is recommended to carefully examine the joints (polyarthritis), the central nervous system (meningitis), the cardiovascular system (endocarditis) and the gastrointestinal tract (ulcerative lesions).
Differential diagnosis of neutrophilic leukocytosis includes:
- Inflammation; – Exposure to corticosteroids (stress, glucocorticoid therapy, Cushing’s syndrome); – Impact of adrenaline (excitement, fear, physical activity); – Leukemia.
The main causes of neutrophilic leukocytosis with a nuclear shift to the left:
– Bacterial infections (sepsis); – Protozoal, fungal and viral infections (for example, feline infectious peritonitis); – Nonseptic (necrotic) processes (for example, pancreatitis, thromboembolism); – Chemical influences; – Hemoblastoses (AML, CML, myeloproliferative diseases of the bone marrow); – Tumors of various origins (as a result of the production of cytokines); – Pelger-Hewitt anomaly; – immune-mediated diseases (for example, systemic lupus erythematosus and immune hemolytic anemia); – Toxins: endotoxins (eg, chronic renal failure) and exotoxins (eg, snake bites).
The absence of changes in the leukogram does not exclude inflammatory processes. Mild and chronic inflammation (for example, with cystitis) does not cause changes in the level of leukocytes and leukogram. In this connection, in some cases it is necessary to study proteins of the acute phase of inflammation (for example, determination of C-reactive protein in dogs and antithrombin III in cats, or determination of a protein profile). Rice. 5
Forecast
A poor or cautious prognosis includes:
– Leukocytosis more than 60x10⁹/l in dogs and more than 30x10⁹/l in cats; – Degenerative shift to the left; – Leukemoid reaction; – Toxic changes in neutrophils.
Such changes in the leukogram often accompany gram-negative sepsis and indicate severe inflammation. In such animals, it is recommended to conduct a blood test daily. Hypersegmentation of nuclei (shift to the right) The presence of nuclei in neutrophils with five or more lobes is a natural process of cell aging. Hypersegmentation is characteristic of long-term residence of neutrophils in the bloodstream. May occur in older animals.
The main reasons for the appearance:
– Chronic inflammatory processes; – Hyperadrenocorticism or glucocorticoid therapy; – Myeloproliferative diseases; – Cobalamin absorption defect in dogs; – Folic acid deficiency in cats.
Hypersegmentation of neutrophil nuclei can appear in vitro, with late preparation of blood smears (Fig. 6).
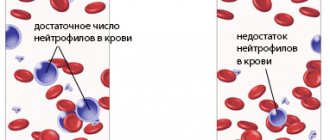
Neutropenia
– a rather rare phenomenon.
Causes of neutropenia:
– Reduced yield of neutrophils from the bone marrow (dysgranulopoiesis); – Increased migration of neutrophils into tissues (consumptive neutropenia); – Transition of neutrophils from the circulating to the marginal pool.
Neutropenia accompanies:
– Hemoblastoses; – Feline leukemia virus (FeLV); – Feline immunodeficiency virus (FIV); – Idiosyncrasies to drugs (cephalosporins, trimethoprim, phenylbutazone); – The influence of endogenous and exogenous estrogen; – Chemotherapy; – Viral infections (parvovirus); – Blood parasitic infections – ehrlichiosis (Ehrlichia canis); – Hereditary disorders (cyclic hematopoiesis in gray collies and Chediak-Higashi syndrome in cats); – Myelophthisis (multiple myeloma, lymphocytic leukemia, myelodysplastic syndrome); – Primary immune-mediated neutropenia (systemic lupus erythematosus).
During shock, neutrophils move from the circulating pool to the marginal pool - pseudoneutropenia. Belgian Shepherd Tervurens are characterized by physiological leukopenia/neutropenia/lymphopenia. In the presence of persistent irreversible neutropenia, a bone marrow punctate study is recommended.
Dysgranulopoiesis
Dysgranulopoiesis
characterized by a decrease in the number of progenitor cells in the bone marrow or a disruption in the process of cell maturation.
Causes:
– Hemoblastoses; – Feline leukemia virus (FeLV); – Feline immunodeficiency virus (FIV).
What is neutrophilic leukocytosis? Causes of development, types, blood counts
23.05.2019
If a person is healthy, then the leukocytes in his blood will be constantly replaced by new cells.
Their lifespan can reach 12 days; during the presence of infection, the number of white cells decreases.
Typically, neutrophilic leukocytosis develops in acute infectious pathologies, in the presence of chronic infectious diseases, and in some myeloproliferative pathologies.
What is it and why is it dangerous?
Neutrophilic leukocytosis is a condition when the level of neurophils in the blood increases, which can be young and rod-shaped. If tests show this deviation, the doctor may assume the presence of an infectious-inflammatory process in a person.
The condition is diagnosed when an increased number of neutrophils are produced in the bloodstream, if the person has myeloproliferative diseases or inflammatory processes.
The danger of this condition is that it poses a threat to health, since neutrophilic leukocytosis indicates the presence of the following pathological processes in a person:
- Purulent-septic infections. Mainly of bacterial, fungal or rickettsial origin, sometimes of viral etiology.
- For poisoning, for example, carbon monoxide, ethylene glycol, arsenic, mercury, etc.
- Endogenous intoxication – eclampsia, ketoacidosis, uremia.
- Bleeding and tissue necrosis.
- Impact on the central nervous system. For example, surgery, trauma, anesthesia, cerebral hemorrhage.
- Gout.
- Early stage radiation sickness.
- Influenza condition complicated by purulent processes.
- Diseases associated with dysfunction of the bone marrow - metastasis of cancer tumors to the bone marrow, osteomyelitis.
Indicators
If a person is not sick, then the normal indicator for him will be the following number of leukocytes - from 4 to 8.8X10⁹/liter for adults. In children, this indicator may vary, everything will depend on how old the child is:
- Newly born babies - from 9.4 to 32.2.
- At one month of age - from 9.2 to 13.8.
- From 12 months to three years of age - from 6 to 17.5.
- From 4 to 10 years – 6-11.4.
- By the age of 20 – 4.5-10.
Reference! Thus, we can talk about leukocytosis when the white cell count begins to exceed 10X10⁹/liter.
If leukocyte counts are high, it is imperative to start treatment:
- Doctors usually prescribe antibiotic therapy and sometimes steroid drugs.
- If there is increased acidity in the urine, then antacids are prescribed.
- In severe situations, leukapheresis is indicated, a procedure that involves removing white blood cells from the blood. After this, the person’s purified blood is poured back into him.
Leukocytosis can be of various types, in addition to neutrophilic it can be:
- Short term.
- Pathological.
- Physiological.
- Eosinophilic.
- Lymphocytic.
- Monocytic.
- Basophilic.
Important! The condition is usually manifested by the symptoms that are inherent in a particular disease.
Kinds
When characterizing neutrophilic leukocytosis, the nuclear shifts of neutrophils are taken into account.
Nuclear shift is characterized by a violation of the ratio of young (myelocytes, metamyelocytes, band) and mature (segmented) forms of neutrophilic leukocytes.
Neutrophilic leukocytosis, depending on the movement of the nuclear base in the leukocyte formula, can be divided into the following types:
- Without nuclear shift - the number of mature segmented neutrophils increases against the background of general leukocytosis. This can be noticeable after eating, when working muscles, during bleeding, or with a mild infectious disease.
- With a nuclear shift to the left, when young forms increase in the blood. This type, in turn, can be divided into the following varieties:
- Simple or hyporegenerative nuclear shift to the left, when band neutrophils increase. Occurs with mild infection or inflammation. For example, with tonsillitis, catarrhal appendicitis, malarial conditions.
- With a regenerative shift of the nucleus to the left, when metamyelocytes appear and band cells increase. This occurs during purulent-septic processes with pneumonia, scarlet fever, typhus, and diphtheria.
- Hypergenerative nuclear shift to the left. With it, in addition to the appearance of metamyelocytes and the growth of band neutrophils, myelocytes also appear. The diseases are accompanied by a purulent-septic course, for example, purulent appendicitis, peritonitis, purulent cholecystitis, etc. A nuclear shift to the left in neutrophilic leukocytosis can be observed not only with bacterial infections, it also develops with various injuries, such as burns, bleeding, acute hemolysis, and also during surgical interventions.
- With deregenerative nuclear shift – indicates bone marrow suppression. Manifests itself in severe infectious processes and endogenous intoxication.
- With a shift of the nucleus to the right, when mature neutrophils increase with hypersegmentation of the nucleus (more than five segments), young cells disappear against this background - this condition can be present in healthy patients and in patients with Addison-Birmer anemia.
Features and reasons for development
In general, the causes of the development of neutrophilic leukocytosis in adults and children are quite similar. It can develop due to tissue trauma, poor nutrition and obesity, and an excessive immune response.
This is observed in allergy sufferers or those suffering from autoimmune pathologies.
In children
In childhood, leukocytosis occurs for the following main reasons:
- Infections.
- Power failures.
- Excessive physical activity.
- Stressful conditions.
In rare cases, acute leukemia may develop, which is considered an extremely dangerous condition. However, in leukemia, the phagocytic activity of neutrophils is reduced.
Attention! Sometimes leukocytosis in children is accompanied by cardiovascular disorders.
In adults
Leukocytosis in adults can also develop for the following reasons:
- The development of acute infection is the most common cause of leukocytosis.
- Chronic inflammation - when the fight between leukocytes and pathogenic microorganisms begins, an inflammatory process occurs. If the condition becomes chronic, the level of leukocytes in the blood will be constantly elevated.
- Damage to the bone marrow, since this is where the production of white blood cells begins.
- Stressful conditions, psychological tension that lasts more than one day.
- Taking certain medications. These may include epinephrine, corticosteroids, and recombinant growth agents such as G-CSF and GM-CSF.
- Sickle cell anemia.
In some cases, leukocytosis can be avoided if certain preventive rules are followed. This is, first of all, timely treatment of all infectious pathologies, monitoring the general condition of a person through blood tests.
also necessary to monitor the immune system and prevent it from weakening. Undergo annual preventive medical examination by all specialists.
Neutrophilic leukocytosis can sometimes be asymptomatic, especially in childhood; only regular examination of the body will save you from developing serious complications.
What is neutrophilic leukocytosis? Causes of development, types, blood parameters Link to main publication
Source: https://doctor-krov.com/zabolevaniya/neytrofilnyy-leykocitoz.html
Leukemoid reactions
Leukemoid reactions are changes in the blood that are sometimes observed in a number of diseases and are characterized by the appearance in the peripheral blood of a large number of young cells, usually found only in the bone marrow. The picture of peripheral blood in leukemoid reactions is similar to the blood picture in leukemia: in myeloid-type reactions, the blood picture resembles CML , with reactions of the lymphatic type - CLL. The leukemoid reaction is characterized by pronounced leukocytosis (50–100x10⁹/l).
Differences between leukemoid reactions and leukemia:
– In leukemoid reactions, in most cases it is possible to find an etiological factor; – Blood changes during leukemoid reactions are usually unstable; after eliminating the factor that caused the pathological process, the blood profile quickly returns to normal; – Significant differences are found when examining bone marrow punctures.
There are three types of leukemoid reactions:
– Myeloid (granulocytic); – Monocytic; – Lymphocytic.
In humans, leukemoid reactions of the eosinophilic type are also described. Most often, leukemoid reactions of the myeloid type occur in animals. They are characterized by the presence of a large number of immature neutrophils (pronounced shift of the nucleus to the left), and the appearance of single blast cells is possible. Neutrophils are often degeneratively changed (severe neutrophil toxicity is observed).
May occur when:
– Pyometra; – Peritonitis; – Pneumonia; – Pyothorax; – Pyelonephritis; – Abscesses; – Immune hemolytic anemia; – Functional disorders of neutrophils (for example, deficiency of protein adhesion in leukocytes in Irish setters); – Blood parasitic diseases (for example, canine piroplasmosis).
Leukemoid reactions of the lymphocytic type are characterized by the presence of a large number of lymphocytes, and the appearance of prolymphocytes and lymphoblasts is also possible. Can accompany piroplasmosis of dogs and hemobartonellosis. Leukemoid reactions of the monocytic type are characterized by a predominance of monocytes in the leukogram, the monocytes themselves can be morphologically changed, and single monoblasts are found. In dogs, a similar type of reaction has been described with hemobartonellosis.
A shift in the leukocyte formula is a specific situation of redistribution of components in the leukogram. Because white blood cells are a family of specialized cells that perform different but complementary functions, counting them individually may not always provide comprehensive information.
When conducting a blood test, it is customary to count the total number of leukocytes and isolate the components as a percentage of it. The calculation data is first summarized in a table (Egorov’s grid), and then provided in the form of a document called a leukogram.
Any change in the body (for example, a particular disease) leads to a change in the percentage of some leukocytes in the leukogram due to a corresponding change in others. This change is usually called a shift in the leukocyte formula.
Leukogram
Therefore, when assessing CBC ( complete blood count ) indicators, not only the total number of leukocytes is studied, but also the proportion of each cell type. The percentage of all leukocyte cells is called the leukocyte formula or leukogram.
Counting leukocytes in a blood smear is carried out using two methods (according to Schilling or Filipchenko). The essence of the methods is approximately identical. Using a microscope, from 100 to 200 leukocyte cells are counted and their number is arranged in a special table according to their type.
The percentage is then calculated for each type. This is the leukocyte formula (leukogram). Based on its changes (shift to the right or left), one can draw conclusions about the course of the disease, possible complications, and also make a prognosis for recovery.
Types of leukocyte cells and their functions
Based on the presence of specific granularity, all types of leukocytes are divided into:
- granulocytic (neutrophilic (N), eosinophilic (E), basophilic (B));
- agranulocytic (lymphocytic (L), monocyte (M)).
The main function of all leukocyte cells is to provide immune responses.
The most numerous group of leukocytes are neutrophils. Depending on the degree of maturity, young (rod) forms and mature (segmented) forms are distinguished among them. Together with monocytes, neutrophils are responsible for the processes of active phagocytosis (capture and destruction of pathogenic agents).
Thanks to monocytes, phagocytosis of destroyed and dead cells, denatured proteins, bacteria, antigen-antibody complexes, etc. occurs.
Lymphocytes are the most important component of immunity. Among them there are three types of cells:
- T (provide cellular immune responses);
- B (responsible for humoral immune response reactions);
- NK (destruction of viruses, tumor and mutated cells).
The main role of eosinophils is to phagocytose the antigen-antibody complex formed by immunoglobulin E. Together with basophils, they participate in the development of type 1 hypersensitivity reactions.
Basophils belong to the smallest group. However, they play a significant role in ensuring the inflammatory response and the development of allergic reactions.
Leukocyte indices [edit | edit code ]
Leukocyte (or hematological) indices are the ratio of the content of various forms of leukocytes, and in some cases, ESR:
- Harkavi index (IG = lymphocytes/segmented neutrophils) [1],
- leukocyte index of intoxication Ya. Ya. Kalf-Kalif (LII = (4×myelocytes + 3×metamyelocytes + 2×band neutrophils + 1×segmented neutrophils) × (plasma cells + 1) / ((monocytes + lymphocytes) × (eosinophils + 1))),
- LII modified by B. A. Reis (LII Reis = (myelocytes + metamycelocytes + band neutrophils + segmented neutrophils) / (monocytes + lymphocytes + eosinophils)),
- hematological index of intoxication (GPI) according to V. S. Vasiliev with additions by P. I. Poteyko (GPI = LII × Glue × KSOE × Ker × Ktrom, where Glue, KSOE, Ker and Ktrom are coefficients corresponding to the number of leukocytes, ESR, erythrocytes and platelets, determined from the tables given in [2] ),
- nuclear index of the degree of endotoxemia (NAISE = (monocytes + metamyelocytes + band neutrophils) / segmented neutrophils),
- nuclear shift index (NSI = (myelocytes + metamyelocytes + band neutrophils) / segmented neutrophils),
- allergy index (IA = (lymphocytes + 10 × (eosinophils + 1)) / (band neutrophils + segmented neutrophils + monocytes + basophils)),
- immunoreactivity index (IIR = (lymphocytes + eosinophils) / monocytes) according to D. O. Ivanov et al [3].
- neutrophil to monocyte ratio index (ISNM = myelocytes + metamycelocytes + band neutrophils + segmented neutrophils / monocytes),
- lymphocytes and monocytes (ISLM = lymphocytes/monocytes),
- lymphocytes and eosinophils (ISLE = lymphocytes/eosinophils in the presence of eosinophils and ISLE = lymphocytes in the absence of eosinophils),
- eosinophil-lymphocyte ratio index (ESL = eosinophil/lymphocyte), which does not depend on the presence or absence of eosinophils,
- ratio index of leukocytes and ESR (ILSE = (leukocytes × ESR) / 100),
- agranulocytes and ESR (ISLMSOE = (lymphocytes + monocytes) / ESR),
- neutrophil-lymphocyte ratio (NLK = (myelocytes + metamyelocytes + band neutrophils + segmented neutrophils) / lymphocytes),
- leukocyte shift index (WSI = (eosinophils + basophils + myelocytes + metamyelocytes + band + segmented) / (monocytes + lymphocytes)),
- lymphocytic granulocyte index (LGI = lymphocytes × 10 / (eosinophils + basophils + myelocytes + metamyelocytes + band + segmented)) [4],
- intoxication indicator (PI = (LII × leukocytes, G/l × ESR, mm/h) / 1000).
Shift of the leukocyte formula to the left
This change in the CBC is due to the appearance of many young cells. A shift in the leukocyte formula to the left indicates that
the body is forced to “throw immature immune cells into battle” with pathogenic agents.
A hyporegenerative shift to the left is accompanied by rodocytosis up to 6%. Such changes in blood tests are typical for:
- infectious diseases of mild severity;
- mild inflammation (catarrhal form of appendicitis);
- active tuberculosis;
- fresh syphilis;
- malarial attack;
- the first day after myocardial infarction;
- malignant neoplasms (in the initial stages).
Neutrophilia, accompanied by a regenerative shift to the left, with an increase in the number of band neutrophils above six percent and leukocytosis of more than 12 * 109 L, is characteristic of infections with a moderate course (scarlet fever, erysipelas, typhus, diphtheria, pneumonia, septic endocarditis).
A hyperregenerative shift to the left, not accompanied by a significant increase in band neutrophils, however, characterized by the appearance of neutrophilic myelocytes, is observed with:
- infectious diseases with severe course (severe pneumonia, erysipelas, cholera);
- meningococcal meningitis;
- purulent diseases of the ENT organs (sinusitis, frontal sinusitis, ethmoiditis, sphenoiditis, streptococcal tonsillitis, otitis), biliary tract (phlegmonous or gangrenous cholecystitis, etc.), urinary system (severe pyelonephritis);
- hemolytic anemia;
- perforated and gangrenous appendicitis;
- diffuse peritonitis, sepsis;
- oncological neoplasms, with severe intoxication.
An increase in the number of neutrophils, accompanied by a degenerative shift (that is, with an increase in the number of band forms, but without the appearance of immature cells), is characterized by a large number of destructively altered hypersegmented cells with toxic granularity. A similar phenomenon is observed in severe tuberculosis, intoxication, and bone marrow suppression.
Neutrophilia, not accompanied by a shift to the left, can be detected during physical and emotional stress, menstruation, after taking steroids, administering vaccines, or eating food. Among the pathological causes of such neutrophilia are gout, eclampsia, uremia, drug poisoning, acidosis, acute blood loss, the first day after tissue necrosis (after myocardial infarction, with necrotic decay of tumors, with gangrene).
High leukocytosis with neutrophilia, as well as the appearance of myeloblasts, band cells and young forms in the blood, is observed in leukemoid reactions of the myeloid type.
How to take a blood test with a leukocyte count
Venous or capillary blood is used for diagnosis. As a standard, the analysis arrives the next day. In emergency situations, the laboratory provides an answer within an hour.
To obtain the most reliable indicators, a blood test is taken on an empty stomach. During the day, it is necessary to eliminate physical and emotional stress, smoking and drinking alcohol. The attending physician and laboratory personnel should be notified of any medications taken as they may interfere with test results.
✓ Article checked by doctor
A general blood test with determination of its leukocyte formula is one of the most informative types of studies that are carried out to identify a number of ailments and assess the general state of health. Any deviations from the generally accepted ones in this case may indicate an infection, the presence of inflammation or other changes in the body. Changes in the composition of the blood can be different, depending on the characteristics of the pathological process and the patient’s body. One of the conditions that requires close attention from a doctor and additional research is called a shift in the leukocyte formula.
Shift of the leukocyte formula to the left
What is the leukocyte formula?
Blood cells known as white cells or leukocytes play an important role in the body's immune system - they identify and neutralize foreign agents, viruses and bacteria. There are five types of leukocytes in total, each of which performs its own function.
- Lymphocytes destroy foreign agents, malignant cells, and are also responsible for the production of protective antibodies.
Causes of decreased lymphocytes
Reasons for the decrease in eosinophils
Reasons for the decrease in monocytes
Reasons for decreased neutrophil levels
What are basophils
The leukocyte formula reflects the relative number and ratio of the above types of cells in the patient’s blood. The presence of infections in the body, the presence of foci of inflammation or pathological processes may be indicated by deviations from the norm, which are determined through laboratory tests.
The number of white cells can vary depending on age and some physiological factors, so when determining the number of white blood cells, the characteristics of the patient’s body are taken into account.
Norms for the number and percentage of leukocytes for adults
| Type of leukocytes | Number of cells in the sample x 109/l | Percentage |
Since human blood mainly consists of lymphocytes and neutrophils, abnormalities are most often associated with these types of leukocytes.
The norms of band and segmented neutrophils in representatives of both sexes are approximately the same, and changes in the leukoformula depend on age.
So, immediately after birth, the child’s body is freed from maternal blood cells and begins to form its own, therefore the number of young leukocytes in the sample is significantly increased. The second shift is observed at the age of about a year due to physiological changes in the body, and is also considered normal.
| Lymphocytes | 1,2-3 | 19-37 |
| Segmented neutrophils | 2-5,5 | 47-72 |
| Band neutrophils | 0,04-0,3 | 1-6 |
| Monocytes | 0,09-0,6 | 3-11 |
| Eosinophils | 0,02-0,3 | 0,5-5 |
| Basophils | 0-0,065 | 0-1 |
| Age | Norms of band neutrophils | Norms of segmented neutrophils |
What is leukocyte formula
Clinical significance [edit | edit code ]
In clinical practice, the leukogram is of great importance, since with any changes in the body, the percentage of some types of white blood cells increases or decreases due to an increase or decrease to one degree or another in others. Based on leukogram data, one can judge the course of the pathological process, the occurrence of complications and predict the outcome of the disease. Leukogram data must be compared with the clinical manifestation of the disease
Description of specific indicators [ edit | edit code ]
Neutrophils [edit | edit code ]
Neutrophils
normally presented in three or two groups: may be present in small quantities or absent: young (u) 0-0.5%; rod-nuclear (s/i) 1-5% and segmented (s/i) 40-68%. They have mainly bactericidal and detoxification functions, bearing the conventional name of microphages (which reflects the leading mechanism of their immune function - phagocytosis).
Depending on the degree of maturity and the shape of the nucleus, band (younger) and segmented (mature) neutrophils are distinguished in the peripheral blood. Younger cells of the neutrophil series - young (metamyelocytes), myelocytes, promyelocytes - appear in the peripheral blood in case of pathology and are evidence of stimulation of the formation of cells of this type. The duration of neutrophil circulation in the blood is on average approximately 6.5 hours, then they migrate into tissues.
Normal blood content: 48-78%
Limits of the normal content of neutrophils in the leukocyte formula:
Adults 47 – 72%
In children, 2 crossovers of the leukocyte formula normally occur at the age of five days and 4-5 years, while up to 5 days neutrophils predominate over lymphocytes, almost like in an adult, then the first crossover occurs: the ratio of lymphocytes/neutrophils is approximately 20%/60%. turns into 60%/20%, this remains until the second crossover of the leukocyte formula, usually it occurs at 4 years, but is acceptable up to 5 years, after which the content and proportions of neutrophils/lymphocytes correspond to the norms of an adult.
- inflammatory processes;
- myocardial infarction, lung;
- malignant neoplasms;
- many infectious processes.
Analysis transcript
As mentioned above, deviations from the norm in the leukoformula may indicate the presence of infections and pathological processes, so the patient needs to consult a doctor, and in some cases additional examinations. When deciphering the analysis result, not only their number is taken into account, but also the ratio between different types of leukocytes, in particular, between young and mature cells. A decrease or increase in the number of mature blood cells in relation to young ones is called a shift in the leukocyte formula.
It should be noted that deciphering the analysis and determining the reasons for the shift in the leukoformula should be done exclusively by a specialist after assessing the general condition of the patient and collecting an anamnesis, taking into account the age and characteristics of the human body.
What to do in case of deviations
If there are deviations in the leukocyte formula, an urgent consultation with a doctor and a secondary examination are necessary, because These indicators indicate the presence of various diseases in the body and require, first of all, to identify the cause of this condition, and then eliminate it.
To make any accurate diagnosis, each of us undergoes a procedure such as donating blood for analysis. In most cases, a sample from a finger is enough, but sometimes you have to take biomaterial from a vein. Often, during research, doctors use such a definition as a shift in the leukocyte formula. Having heard such an expression somewhere, not everyone will be able to understand what they are actually talking about.
It is worth noting that each person’s blood composition is individual, and it can change due to various biological processes. The leukocyte formula tells about these changes. And it is precisely this that will be discussed further in the topic of this article.
Shift of the leukocyte formula to the left
What is a leukocyte formula shift?
If a pathological process or certain physiological changes occur in the body, mature blood cells die first, after which their place is taken by “young” cells. For this reason, the number of immature leukocytes (band neutrophils) in relation to old ones (segmented neutrophils) increases - this condition is called a shift of the leukocyte formula to the left.
Sometimes, in addition to the high content of band neutrophils, their precursor forms appear in the blood - myelocytes, metamyelocytes, promyelocytes, etc., which clearly indicates the presence of certain pathologies (they are not present in the analysis of a healthy person).
Pathological shift to the left
Sometimes, however, the leuko-erythroblastic reaction is pathological. If the bone marrow is crowded with something other than blood-forming tissue—say, for example, a cancerous tumor in leukemia—then the hematopoietic cells will not have enough space or time to mature properly. They will end up maturing by leaving the bone marrow before they are ready to function fully, and you will see both immature red blood cells and neutrophil precursors in the blood. This is an extremely worrying sign.
One way to determine whether leukoerythroblastic reaction should be a concern is to look at the hemoglobin. As mentioned above, if the hemoglobin is very low (say, below 60g/l), then the leukoerythroblastotic reaction is likely physiological. However, if the hemoglobin is normal or has only decreased slightly, then the patient does not have a compelling reason for a leukoerythroblastic reaction and it is worth investigating what is causing it. This requires a repeat blood test and a more in-depth examination.
Alena Paretskaya, pediatrician, medical columnist
just today
( 45 votes, average: 4.73 out of 5)
Increased basophils in a child and in an adult’s blood: possible causes
Reduced monocytes in the blood of adults: causes of deviations and norms
Related Posts
Causes of deviations in the leukoformula
The reasons for the shift of the leukoformula to the left include:
- a number of acute infectious diseases, including pneumonia, mumps, meningococcal infection, salmonellosis;
- processes with the formation of pus;
- inflammation (rheumatism, thyroiditis, peritonitis, pancreatitis);
- injuries or surgical interventions that were accompanied by heavy bleeding;
- pathological processes accompanied by tissue necrosis: myocardial infarction, burns, stroke;
- intoxication with alcohol, heavy metals, bacterial toxins;
- oncological diseases.
Percentage of different types of leukocytes
Rejuvenation of the blood composition (if the analysis contains myocytes, erythroblasts, promyelocytes) indicates serious disorders in the body - metastases that have entered the bone marrow, leukemia, coma.
A variant of the norm is considered to be a shift in the leukocyte formula during the recovery of the body after operations or serious illnesses, as well as heavy physical exertion - in this case, the shift is called reactive, and does not require medical intervention. In addition, minor changes in the formula are observed in pregnant women.
According to statistics, approximately 2-5% of the world's population has a shift in the leukocyte formula to the left with an increase in the number of young types of leukocytes without any infections or pathologies.
To determine the degree of neutrophilia (increased number of neutrophils) and the intensity of the ongoing pathological process, it is necessary to summarize all the indicators of a given group of leukocytes in the analysis and determine the total number. With a moderate shift it will not exceed 10 x 109/l, with a pronounced shift it will vary within 10-20 x 109/l, with a severe shift - 20-60 x 109/l. The most unfavorable is severe neutrophilia, which indicates serious pathologies in the body, and sometimes a direct threat to human life.
Video - Leukocyte blood formula
Signs of changes in the leukocyte formula
An increase in the number of neutrophils in the blood does not leave its mark on the general condition and well-being of a person - most of the diseases that accompany it have pronounced symptoms. In addition, when the leukocyte formula shifts, severe weakness, decreased performance, decreased blood pressure, and dizziness may occur. If such signs appear, you should consult a doctor as soon as possible in order to promptly identify the causes of changes in the composition of the blood.
Features of the leukocyte formula in children
All leukocytes are divided into two large groups:
- Granulocytes have a clearly defined nucleus and peripheral muscles, thanks to which they are able to actively move and move in the blood stream not only under pressure, but also spontaneously.
- Agranulocytes lack a nucleus and remain relatively motionless, but actively fight foreign microorganisms by producing antigen.
Based on their qualitative content, leukocytes are usually divided into 5 types:
- lymphocytes;
- monocytes;
- eosinophils;
- basophils;
- neutrophils.
Each cell in the body has its own role, so their active production may indicate the presence of a specific disease in children.
The leukocyte formula shows what percentage of cells of one type or another are contained in every 100 leukocytes. This relative ratio allows you to identify all the cells present in the smear, as well as estimate their number in the total leukocyte mass.
Analysis for leukocytes in children is carried out as planned, adhering to the following scheme:
- up to a year - every trimester;
- 1-3 years – once (once a year);
- 3-6 years – according to doctors’ indications;
- 6-12 years - as planned when undergoing an annual medical examination;
- 12-18 years old - planned and unplanned, in the presence of chronic diseases.
Indications for studying the leukocyte formula may include such manifestations as:
- poor sleep;
- excessive sweating;
- poor appetite;
- frequent rhinitis;
- constant acute respiratory infections and acute respiratory viral infections;
- enlarged lymph nodes.
Typically, the leukocyte count is assessed during hospitalization of a sick child to confirm or refute the diagnosis made by the doctor.