Related transplantation of the right lobe of the liver
The first successful liver transplantation in our country was performed at the Russian Scientific Center for Surgery named after.
Academician Petrovsky on February 14, 1990. The next important achievement in global and domestic transplantology was the transplantation of the right lobe of the liver from a living related donor - in November 1997. The operation was performed by Sergei Gauthier. At the age of eight, Alexey from the town of Alexandrov near Moscow was diagnosed with an “abdominal tumor”, and even later - “liver cirrhosis”. The medical report stated that if the transplant was not performed, the boy would not live a year. Alyosha was sent to Moscow to the Russian Scientific Center of Surgery named after. Academician Petrovsky, where Sergei Gauthier then worked.
“20 years ago there were no state quotas or charitable foundations. But we didn't pay anything for treatment. When Sergei Vladimirovich Gauthier said that he was ready to operate on us, I asked: “How much will it cost?” To which he joked: “What, do you have a lot of money?” I was embarrassed and said that that’s the point, there was no money. Gauthier answered seriously: “Don’t think about it, there are more important things,” recalls the boy’s mother, Valentina.
The Surgery Center conducted a thorough examination of the compatibility of the mother as a donor and the son as a recipient, and six months later they performed the world's first related transplantation of the right lobe of the liver. Previously, a smaller part of the liver fragment was taken from a living donor - the left lateral sector.
A few years later, Alexey began to have kidney problems due to the medications he was taking, and in 2014 he had to undergo another operation. Valentina also became a kidney donor for her son.
Now Alexey and his mother are doing well, he works as a programmer, she works as a painter.
Heart transplant
Based on the National Medical Research Center named after. acad. E.N. Meshalkin performs the most complex and unique heart transplant operations. Heart transplantation is an expensive treatment that requires medical personnel to be highly qualified and have many years of experience. To perform a surgical intervention, complete compatibility of the tissues of the patient and the donor organ is necessary. The lack of donor organs causes a limited number of this type of surgical treatment. But despite this, hope and the desire to live never fades in people, and we are ready to help such patients. Our clinic has a whole team of doctors who treat patients with heart transplants.
When is a heart transplant necessary?
The need for a heart transplant is most often caused by dilated cardiomyopathy, when the size of the heart begins to increase, the heart muscle “stretches”, and its contractions become weaker. The second place among diseases leading to the need for a heart transplant is coronary heart disease, which often leads to the formation of myocardial infarctions with subsequent scar areas, which leads to the loss of the heart’s ability to perform effective contractions. A small percentage of patients who are candidates for heart transplantation are patients with valve defects.
In order to prolong the patient’s life until a donor heart is found, it is necessary to use what transplantologists call a “bridge”, i.e. one or another technique that improves blood circulation. The first of them is the “pharmacological bridge” - the intensive use of powerful cardiotonic drugs. Often, after some time, these drugs are no longer able to provide the required level of blood circulation in the body, then it is necessary to move on to a “mechanical bridge” - the use of various mechanical pumping devices - an artificial heart, which partially and sometimes completely provides blood circulation.
What do you need to know before transplantation?
In order to prevent donor organ rejection, a number of rules must be followed. First of all, it is necessary that the donor and recipient are similar in their histocompatibility antigens, which in humans are combined into the HLA (Human leucocyte antigens) system. Based on the results of the compatibility test, the most suitable donor and recipient are selected.
Using the second test (cross-match), potentially dangerous antibodies in the recipient that can damage the transplant are determined. If there are a lot of them in the recipient's blood, there is a high probability of donor organ rejection.
What should a patient remember after transplantation?
Due to the reaction of the body's immune system to a foreign organ, after a heart transplant it is necessary to take medications that do not allow the body to reject the donor heart. A person with a transplanted heart needs to regularly maintain contact with their attending physicians, especially cardiologists. NMRC specialists in the clinic and after discharge will monitor your health and do tests to make sure that your new heart is working correctly. In the first year after surgery, you need to take special care of your health to avoid infectious complications.
In most cases, people do well after surgery. They can go to work and lead an active lifestyle. At the Clinic named after. acad. E.N. Meshalkin several transplantations are performed annually. Experienced specialists carry out this complex procedure at the highest level. Caring medical staff helps make the waiting period for a donor organ and the postoperative period as comfortable as possible for the patient.
Split liver transplantation
A healthy liver from a deceased donor can be divided and transplanted into two patients. Split transplantation is of great importance in saving the lives of children who cannot benefit from an organ from a related donor.
11-year-old Nastya from the Dagestan city of Kizlyar has been under observation since the age of two due to polycystic kidney disease, which arose as a result of an intrauterine mutation. At first a kidney transplant was planned, and then a liver transplant was needed. The mother was not suitable as a donor. At the end of July 2020, at the Shumakov Center, the girl underwent a kidney and part of the liver transplantation from a deceased adult donor. The second part of the liver was transplanted into a boy from Chechen Gudermes, Ibragim, who was diagnosed with tyrosinemia, a congenital genetic disease. This was one of the first operations in Russia for two children - a complete split was performed, when the organ was divided into two equal halves. Typically, the liver transplant is divided into a larger part for an adult patient and a smaller part for small children.
Transplantologist Sergei Gauthier explains that several years ago, mostly related transplants were performed on children, and when there were no related donors suitable in terms of health and anatomy, the child found himself in a critical situation. Now, if a child’s disease progresses sharply, transplantologists can count on the possibility of receiving an organ from a deceased donor.
Chief transplantologist of Russia Valery Shumakov
– Valery Ivanovich, in February of this year, an amendment was made to the Federal Law “On Transplantation of Human Organs and (or) Tissues” to allow the collection of donor organs in state and municipal medical institutions. Will this somehow help solve the problem of shortage of donor organs?
– Of course, the state of transplantation will improve.
When the law was adopted, and this was in 1992, there was no division of state property into federal and municipal, including medical institutions. Therefore, until recently, the wording was as follows: “The collection and procurement of human organs and (or) tissues is permitted only in government health care institutions.” Not a word about municipal ones, which are the same as state ones. And in regions where there are mainly municipal hospitals, law enforcement agencies often refused doctors permission to collect organs from the deceased, citing the law. Now there are no formal barriers. – Are there enough clinics and specialists in Russia capable of collecting and transplanting organs?
– There are enough hospitals and doctors.
Officially, today a little more than thirty centers are engaged in organ transplantation. Our potential capabilities are tens of times greater than the actual number of operations. Only on the basis of our research institute it is possible to perform at least 10 times more transplants than we do today. Today's need is thousands, and we perform dozens of operations. – How long did it take for the amendment to the law to be made?
- A few months.
- Just everything?
“Probably because the problem has already become so ripe that everyone understands that there is no longer room for delay.”
We simply have nothing to replant. We support patients who have only a few days to live as best we can, but there are no organs for transplantation. And people who can be saved die. – In order for a deceased person to become a donor, the consent of relatives is required in Russia.
But in Spain or Belgium, for example, such consent is not required. Which model is more effective? – Both models are approved by the World Health Organization and are successfully used.
In our country, this area is regulated by the eighth article of the Law on Transplantation (“Presumption of consent to the removal of organs and (or) tissues.” - “NI.”), and the relationship between doctors and relatives of the donor is the so-called presumption of consent. What does this mean? When the question of whether to take organs from a deceased person for transplantation is decided or not, the final word remains with the relatives. If they are against it or declare that the deceased was against it during his lifetime, the question is dropped. But this principle only works when relatives are informed about what happened, when they are in the hospital or have informed about their intention to arrive. If a person brought in in a state of shock or unconsciousness, for example after an accident, has no documents and dies without regaining consciousness, doctors are not obliged to actively search for relatives and ask their permission. Doctors must assess the situation and quickly decide whether the deceased can become a donor. In such a situation, you cannot hesitate: the collection is carried out in the first hours after death. This is what was inflated until recently in the press: they say that doctors are just waiting for the patient, delivered in critical condition, to die, and he can be disassembled for spare parts. But, I repeat, doctors are obliged first of all to save people, and not to look for their relatives. If it is not possible to save a person, doctors think about the possibility of transplanting some organ or organs of the deceased to other people who can still be saved. In Russia, these are hundreds of thousands of patients, they have no alternative: either they receive a donor heart or kidney and continue to live, or they die. – How many people are waiting in line for a transplant?
– I won’t even name the numbers, because there are tens, even hundreds of times more people who can be saved with a donor organ transplant.
Our patients are mainly 20-40 year old men and women, the most socially active part of the population. – Are there age restrictions for this type of operation?
– Age limits are constantly expanding.
The most interesting thing is that the older the person, the lower the risk of organ rejection and the better the prognosis. Of course, at 60–65 years of age, the immediate postoperative period is more difficult than for young people, but if everything goes well, then the long-term results are no worse, and even better, than those of 20–30 year olds. This may be surprising, but logically it should be so: with age, a person’s immune system seems to harden, becoming more resistant to any influences. And a transplanted organ, as you know, is a very serious test for the immune system. – The immunity of our society also reacts painfully to the problems of transplantology...
– Yes, but gradually everything is changing, although not as quickly as we would like.
And the attitude of the media has changed for the better (there is no longer bias and any unfounded accusations against doctors), and the attitude of society as a whole. I have already cited Spain more than once, where 15 years ago the situation with transplantation was the same as ours, and today it is one of the first places in the world. There are posters pasted on the entrance doors of cathedrals: “Don’t take your organs to heaven. You won't need them there." Clergy, politicians, public figures - everyone takes part in shaping the right attitude towards donation. After all, donation is not an end in itself, it is a humane action that saves people doomed to death. In one country, I saw a documentary on television: the mother of a dead boy was asked if she agreed to have her son’s organs removed. She agrees and explains it this way: “A part of my child will live. His death will help save the lives of other children." – Do most of your patients return to normal life after a kidney or heart transplant?
– They even play football with a donor heart.
70 of our patients who underwent a kidney transplant at different times successfully gave birth to children. But for some reason little is said about the fact that donation turns disabled people sentenced to death into normal people. This is not explained to ordinary citizens, legislators, or lawyers. And as long as our society takes the position of such an outside observer, Russian transplantology will fall catastrophically behind the rest of the world. - And where are we?
– Somewhere in the late twenties. The leaders in the number of organ transplants are the USA, Germany, France, and Spain. In Europe there is an organization called Eurotransplant, which unites more than ten countries with a common list of recipients. And it happens that an organ is purchased, say, in Belgium, and taken to Luxembourg. The organization has existed for 40 years, and it makes the task very easy for doctors. By the way, in Soviet times we had the same organization, it was called “Sotstransplant”, and it managed to work for ten years until the Union collapsed. We quite actively exchanged donor organs with all countries of the former socialist camp.
Prevention after heart transplant
Following some rules will help to increase the overall life expectancy after a heart transplant and improve its quality:
- Take special medications. The dosage and time of administration should be observed. Most of the drugs are cytostatics and hormonal drugs aimed at suppressing the immune system.
- Avoid physical activity.
- Follow your diet. Drinking alcohol, smoking and eating fatty foods is strictly prohibited. It is worth following a gentle diet.
- Avoid temperature changes and taking hot baths.
- Avoid infections as much as possible. Do not visit places with large crowds of people, carefully monitor personal hygiene, drink boiled water, and eat thermally processed food.
Despite a number of limitations, the life of a recipient after a heart transplant changes for the better. By following a number of simple rules, you can forget about shortness of breath, rapid heartbeat and tissue swelling.
How much is a person's heart worth?
A heart transplant is one of the most expensive operations in the world. The price varies depending on the location of the clinic and its prestige in the world rankings, and the number of diagnostic procedures performed.
The cost of transplantation for each case is determined individually. On average, an operation of this kind costs 250-370 thousand dollars.
The sale of human organs is prohibited and punishable by law in the world. Therefore, a heart can only be transplanted from deceased relatives, or donors, with written permission.
The patient receives the organ itself free of charge, but the surgical intervention itself, the course of medication, and the rehabilitation period require material costs.
Donor heart ready for transplantation
The cost of a heart transplant in the Russian Federation ranges from $70 thousand to $500 thousand dollars . The country has a quota program for patients who need high-tech operations.
The more accurate cost of transplantation and the chances of it being performed free of charge are clarified individually - during a consultation with a transplantologist.
There is only one coordination center on the territory of the Russian Federation that is engaged in the selection of donors. It covers the territory of Moscow and the region.
Operations are directly carried out in Novosibirsk (NIIPK named after E. N. Meshalkin), St. Petersburg (FSBI "North-West Federal Medical Research Center named after V. A. Almazov") and in the capital (FSBI "FSTIIO named after V. I. Shumakov").
The principles of organ donation in Russia are not yet sufficiently developed at the official level, which becomes an obstacle to heart transplantation.
Thus, on average, about 200 transplants are performed per year throughout the country, while in the United States there are more than 28 thousand. Therefore, most people with incurable heart disease require expensive surgery abroad.
Postoperative difficulties
Many people believe that after a donor organ transplant, a person begins to live a new life, in which there is no place for diseases and medications. And yet this is a huge misconception. After transplantation of a foreign organ, the recipient’s immune system begins to reject it, and in order to reduce this activity, patients are advised to take several drugs from the group of immunosuppressants continuously and for life. These drugs have a large number of side effects, mainly associated with increased sensitivity to infectious diseases. Therefore, bacterial, viral and fungal diseases are the most common complication after any transplant, not just the heart.
The period of postoperative rehabilitation after a heart transplant is also extremely difficult and long. And even after a very successfully performed operation, regularly taking all medications and following the recommendations, the life of such a patient is extended by only a few years, on average - 10.
Who may need a transplant and what kind of donation happens?
A transplant may be needed for any patient for whom other treatment methods do not help. Doctors use liver, kidneys, heart, lungs and some other organs and tissues of the body for transplantation. Donation can be lifetime or posthumous. In Russia, as throughout the world, organs cannot be the subject of commercial transactions, and the professional community perceives all horror stories about people stolen for organs and advertisements in the style of “selling a kidney” with skepticism. Only a relative can become a living donor. You can share a kidney or part of a liver with a loved one.
After death, a person can save several lives - if his organs are suitable for transplantation. Doctors do not work with organs and tissues of cancer patients, patients with hepatitis and tuberculosis. Mostly posthumous donors are those who died from accidents or strokes. For posthumous donation in Russia there is a presumption of consent. That is, doctors are not required to ask permission to remove organs from the patient or his relatives. At the same time, the law provides for refusal of transplantation. Relatives have the right to prohibit doctors from carrying out the removal procedure and, according to the doctors themselves, this right is often used. Transplantologists attribute this to mentality and poor education. People simply do not realize that refusing to use the organs of a deceased person actually kills several more people, people on the waiting list who are really waiting for help.
When is a patient eligible for a heart transplant?
Transplantation of any donor organ is indicated in cases where doctors have tried all possible types of conservative (medicinal) therapy and they do not bring relief to the patient. This is the most backup option, because it involves a huge risk to the patient’s life.
What diseases are grounds for putting a patient on the waiting list for a heart transplant? The main criterion for compliance is ineffective heart function with a decrease in ejection fraction below 20%. This indicator shows what proportion of blood the heart pumps into the vessels from the left ventricle. Doctors determine it using ultrasound. The lower the ejection fraction, the weaker the heart. Reduced ejection fraction is the result of various heart diseases, which can be either congenital or acquired. Over time, severe chronic heart failure develops (grade 3 or 4), and the prognosis for such patients is limited to several months. What diseases can lead to this?
- Dilated or hypertrophic cardiomyopathy. It can be congenital and appear in early childhood, or it can become a complication of other heart ailments.
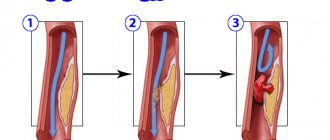
- Widespread atherosclerosis of the coronary vessels, in which effective operations such as coronary artery bypass grafting or stenting of the coronary arteries are either contraindicated or have already been performed, but turned out to be ineffective.
- Heart defects (valve or blood vessels), in which prosthetic surgery is impossible or ineffective.
- Severe cardiac arrhythmia that cannot be corrected with medications.
Thus, transplantation of a donor heart is a therapy of despair. It is carried out when the patient’s life is impossible without it, and all available means and methods of treatment have already been exhausted.