What is the difference from tachycardia?
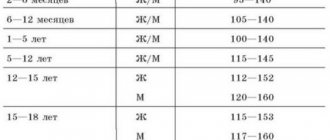
According to the generally accepted classification of heart rhythm and conduction disorders, they are all divided into disorders based on the type of rapid heartbeat (tachycardia, more than 80 heart beats per minute) and the type of rare heartbeat (bradycardia, less than 60 beats per minute).
Rapid heartbeat, in turn, can be accompanied by sinus (correct) and non-sinus (incorrect) rhythm. In the first case, the disorder is called tachycardia, when the heart contracts frequently, but at regular intervals, and in the second, tachyarrhythmia, when the heart contracts frequently and irregularly.
Clinically, tachyarrhythmias and tachycardias appear almost identically, so it can be quite difficult to distinguish them without an electrocardiogram.
Tachyarrhythmia can be:
- Localization of sources of tachycardia
Sinus. It is caused by premature frequent receipt of impulses to the sinus node, which normally sets the heart rhythm (is the pacemaker). Heart rate reaches 90-120 beats per minute.
- Supraventricular, or supraventricular , which is divided into atrial and tachyarrhythmia from the AV connection. These types are caused by the circulation of pathological impulses in the tissues of the atrium (atrial fibrillation) or in the atrioventricular node. Heart rate reaches 130-150 beats per minute and above.
- Zheludochkova . In this case, pathologically frequent impulses of conductive fibers in the ventricles of the heart occur. Heart rate reaches 200-400 beats per minute. Ventricular tachyarrhythmia can progress to ventricular fibrillation and lead to cardiac arrest.
Sinus arrhythmia
The main node of the conduction system that generates nerve impulses is the sinus, and in a healthy person, heart contractions are repeated at regular intervals. Sinus arrhythmia is characterized by deviations associated with both rhythm disturbances and changes in heart rate that arise due to pathologies of the sinus node.
Moderate sinus arrhythmia is the most favorable option of all possible heart rhythm disorders. In most cases, this pathology does not require treatment; you just need to constantly monitor the child’s condition from the first years of life with the attending physician in order to notice the occurrence of complications in time, if they occur.
Sinus arrhythmia in children can be constant or occur in the form of attacks of heart palpitations.
Sinus arrhythmia includes several types of heartbeat disorders. Most often, tachycardia (rapid contraction rhythm), bradycardia (slow rhythm) or extrasystole (single irregular impulses) occurs. All of them are treatable and in most cases are temporary.
Causes of tachyarrhythmia
Tachyarrhythmia most often develops in people over 40-50 years of age, but also quite often occurs in young people and children. This happens due to various reasons.
Thus, sinus tachyarrhythmia, in principle, is not a sign of any organic damage to the heart muscle. This type of tachyarrhythmia can occur under stress, strong emotions or after physical activity.
The causes of other tachyarrhythmias can be divided into the following groups:
1) Functional causes are a set of factors that, in principle, are not a manifestation of any disease:
- Violation of vascular tone in vegetative-vascular dystonia,
- Mild electrolyte imbalances, such as due to dehydration, alcohol poisoning or a hangover,
However, despite the apparent “harmlessness” of this group of causes of tachyarrhythmia, the consequences of the arrhythmia itself can be disastrous if you do not seek medical help in a timely manner.
2) Extracardiac causes . These include diseases of other organs and systems:
- Thyrotoxicosis, which develops as a result of increased secretion of thyroid hormones,
- Acute infectious diseases (influenza, botulism, malaria, etc.),
- Fever,
- Diseases of the gastrointestinal tract,
- Severe anemia
- Alcoholism,
- Drug use.
3) Cardiac causes are caused by pathology of the heart and blood vessels. These include:
- Arterial hypertension,
- Cardiac ischemia,
- Myocarditis - inflammatory lesions of the heart muscle,
- Past or acute myocardial infarction,
- Heart defects
- Cardiomyopathy - hypertrophic (thickening of the heart muscle of the ventricles), restrictive (impaired relaxation of the heart muscle) or dilated (enlargement of the heart chambers) type.
Tachyarrhythmia in childhood
In children, tachyarrhythmias can be caused by organic damage to the myocardium (for example, after myocarditis or heart defects), as well as by functional causes or a combination of the above factors. However, most often in children without heart defects, without surgical interventions on the heart and without myocarditis, sinus arrhythmia is the most common, which is caused by a violation of the autonomic influences on the heart and is easily corrected.
Symptoms
Tachyarrhythmia can begin gradually or acutely in a patient.
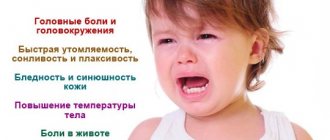
During an acute attack (paroxysm), the patient is bothered by a sudden sensation of interruptions in the heart's function and a feeling of rapid heartbeat, accompanied by severe weakness, discomfort in the chest, and a feeling of lack of air. Some patients immediately lose consciousness due to decreased cerebral blood flow, report cold sweat, and severe pallor of the skin. The condition and well-being worsen without emergency assistance.
With a permanent form of atrial fibrillation, the only type of tachyarrhythmia that lasts for a long time, for years, without the possibility of spontaneous restoration of the rhythm, patients report minor symptoms. They are mainly concerned about shortness of breath on exertion and periodic pressing pain in the chest.
The heart rate varies between patients and may even remain slightly higher than normal, for example in patients with atrial fibrillation.
Diagnostics
A patient may suspect a paroxysm of tachyarrhythmia immediately after the onset of clinical symptoms, especially if paroxysms have occurred before. However, the main diagnostic criteria for tachyarrhythmia can only be determined by ECG. For example, such as changes in the interval between complexes, reflecting ventricular contractions; flicker waves - atrial flutter; absence of waves indicating atrial contraction before the ventricular complexes.
After the diagnosis of paroxysmal tachyarrhythmia has been made by an emergency doctor or a clinic physician, the patient is taken to the hospital, as he requires hospitalization for further diagnosis and treatment. Additional examinations are prescribed in the cardiology or therapy department:
- Ultrasound of the heart,
- 24-hour blood pressure and ECG monitoring,
- TEE (transesophageal electrophysiological study) in case it is not possible to register tachyarrhythmia during a standard ECG.
Treatment of tachyarrhythmia
Treatment of tachyarrhythmia begins at the stage of emergency medical care. The patient is administered intravenously drugs such as novocainamide, strophantine, cordarone, panangin, and for ventricular tachyarrhythmia - lidocaine.
After the patient has been taken to the therapy or cardiology department, the treatment started continues. Basically, doctors use a solution of a polarizing mixture (potassium chloride + glucose 5% + insulin) in the form of intravenous infusions (droppers), or the above drugs. This treatment is a rim-restorative therapy. In addition, rhythm-lowering drugs are prescribed - egilok, concor, coronal, digoxin, etc.
If sinus rhythm is restored at the prehospital stage during paroxysm of atrial fibrillation or supraventricular tachycardia, the patient can be left at home under the supervision of a local physician in a clinic at the place of residence.
In the case of a permanent form of atrial fibrillation, rhythm-restoring therapy is not carried out; the patient is prescribed only rhythm-slowing drugs under the supervision of a local physician, unless the emergency doctor suspects complications of tachyarrhythmia.
If the patient has a paroxysm of ventricular tachyarrhythmia recorded by ECG, he should be taken to the hospital even if the rhythm is restored.
Treatment of tachyarrhythmia in children
The child should be treated only by a pediatric cardiologist. Sinus arrhythmia does not require special treatment, and the child can engage in physical activity if he does not have an organic pathology of the heart or central nervous system that led to the occurrence of arrhythmia. However, serious diseases (tumors, defects, myocarditis) should only be treated by a cardiologist. In addition to antiarrhythmic drugs, patients are prescribed Elcar, Mildronate, Mexidol and vitamin complexes.
Lifestyle
Lifestyle for any form of tachyarrhythmia includes basic recommendations used for any other pathology of the heart and blood vessels. For example, giving up bad habits and poor nutrition, eliminating significant physical activity and professional sports.
However, the most important thing in correcting lifestyle after diagnosis of tachyarrhythmia is timely, regular visits to a cardiologist and taking medications prescribed by the doctor. Sometimes medications need to be taken throughout life, for example, with a permanent form of atrial fibrillation.
What happens if the disease is not treated?
Only a doctor can determine whether treatment is needed.
If a mild and sometimes moderate form of the disease, not accompanied by other abnormalities, can be managed without medications, excluding vitamins and microelements, then the disease combined with other diseases requires mandatory treatment. Disorder of the blood supply leads to disruption of the delivery of oxygen and nutrients to other organs, for example, to the brain. The article contains the answer to the question: what is sinus arrhythmia, clearly describing the symptoms, causes, diagnosis, treatment and prevention of the disease, but this information does not replace a doctor’s consultation.
We wish you good health.
Complications and prognosis
In the absence of timely treatment of tachyarrhythmias, complications may develop. The most common causes are pulmonary embolism, arrhythmogenic shock, ischemic stroke, and acute myocardial infarction.
PE (thromboembolism) is manifested by sudden shortness of breath, suffocation, and bluish discoloration of the skin of the face and neck. With arrhythmogenic shock, the patient’s extremely serious condition immediately occurs, accompanied by loss of consciousness (collapse), a drop in pressure and pale skin. Stroke and heart attack have their own symptoms with paralysis of the limbs, chest pain and other symptoms.
Ventricular tachyarrhythmia can lead to sudden cardiac death.
To ensure that the patient does not develop complications, he should be immediately examined by a doctor at the first appearance of signs of tachyarrhythmia.
The prognosis for sinus tachyarrhythmia, as well as for paroxysmal and permanent forms of atrial fibrillation, is favorable in the absence of complications.
In patients with ventricular tachyarrhythmia, especially in those who have experienced clinical death, the prognosis is unfavorable, since fatal rhythm disturbances develop in the first year after this in more than 50% of cases.
Preventive measures
As already mentioned, arrhythmia can occur both at a young age and in adolescence. Based on this, methods of prevention are determined. First of all, it is necessary to promptly treat the disease that causes irregular heart function. It is important for teenagers to stop smoking and drinking alcoholic beverages. You should avoid stressful situations, and also run and jump less.
Traditional preventive methods include following a diet (the predominance of plant foods and low-fat foods), moderate physical activity, and frequent walks in the fresh air. The child will feel better if he is in a calm emotional state; rest during the daytime will not hurt; night sleep should be at least 8 hours.