Arrhythmia in the elderly: symptoms, causes, treatment
Heart rhythm disturbances are diagnosed in 85% of people over 65 years of age. Most often, arrhythmia in an elderly person manifests itself as an increase or slowdown of the heartbeat, that is, a violation of the intervals between heartbeats. These interruptions are associated with hypertension, acute or chronic pathologies of the cardiovascular system, and age-related changes in myocardial tissue. Unpleasant symptoms increase the risk of stroke and can even cause death. Therefore, at the first signs of illness, it is important to immediately consult a doctor who will conduct a diagnosis, identify the causes and prescribe therapy that can restore normal heart function.
What will happen without treatment?
Some patients do not attach much importance to the diagnosis of arrhythmia, and in vain. If at a young age this disease is easily corrected and treated, then for older people the consequences of untimely treated arrhythmia can be fatal. If the disease is not treated, the following complications are possible:
- Stroke. An attack of arrhythmia in older people can provoke both a micro-stroke and large-scale damage to the blood vessels of the brain with all the ensuing consequences.
- Death. Without appropriate treatment, the course of this pathology will gradually worsen and can cause death.
Patients with arrhythmia should regularly visit a doctor to monitor the course of the disease and prevent the development of complications.
Types and causes of arrhythmia in the elderly
Depending on the nature of the disease, there are several types of arrhythmia. Differing in similar symptoms, they have different locations and etymologies.
- Bradycardia.
An extremely slow heartbeat, with a heart rate of less than 60 beats per minute. Bradycardia usually occurs against the background of impaired blood supply to the heart muscle, chronic heart failure. - Tachycardia.
Too fast heartbeat (more than 100 beats per minute). With tachycardia, older men and women may experience cardiac arrest followed by sudden “somersaults.” - Sinus type arrhythmia.
Heart contractions occur with different rhythms (fast ones alternate with slow ones). The disease is the result of natural age-related processes, aging of organs and tissues. - Atrial fibrillation.
Fast irregular heartbeats. Slowing blood flow causes blood clots (clots in blood vessels) to form, which can cause a stroke.
Elderly people most often suffer from so-called atrial fibrillation. The disease got its name due to the fact that when the impulses are disrupted, the atria begin to work asynchronously: they twitch, flutter, and flicker. Arrhythmia is otherwise called atrial fibrillation. The development of the disease is associated with increased physical and emotional stress, poor diet, and a sedentary lifestyle, which invariably lead to cardiovascular disorders.
Also, atrial fibrillation in older people manifests itself against the background of various pathologies of internal organs and chronic diseases:
- Hypertension;
- Heart failure;
- Atherosclerotic changes in blood vessels;
- Heart attacks;
- Strokes;
- Heart defects;
- Age-related changes in the myocardium;
- Violation of coronary blood supply;
- Ischemic heart diseases.
In addition, the following factors influence the disruption of the heart muscle and the development of arrhythmia:
- Heredity;
- Abuse of bad habits (alcohol and smoking);
- Hormonal imbalances;
- Diabetes;
- Obesity;
- Vegetovascular dystonia;
- Viral and bacterial infections.
The disease can develop due to long-term use of certain medications (in particular, diuretics or antiarrhythmics). Another provoking factor is poisoning with poisons or gases.
Classification of atrial fibrillation
The modern approach to the classification of atrial fibrillation includes the nature of the clinical course, etiological factors and electrophysiological mechanisms.
There are permanent (chronic), persistent and transient (paroxysmal) forms of atrial fibrillation. In the paroxysmal form, the attack lasts no more than 7 days, usually less than 24 hours. Persistent and chronic atrial fibrillation lasts more than 7 days, the chronic form is determined by the ineffectiveness of electrical cardioversion. Paroxysmal and persistent forms of atrial fibrillation can be recurrent.
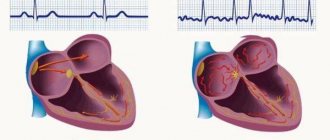
A distinction is made between a newly diagnosed attack of atrial fibrillation and a recurrent one (second and subsequent episodes of atrial fibrillation). Atrial fibrillation can occur through two types of atrial rhythm disturbances: atrial fibrillation and atrial flutter.
With atrial fibrillation (atrial fibrillation), individual groups of muscle fibers contract, resulting in a lack of coordinated contraction of the atrium. A significant number of electrical impulses are concentrated in the atrioventricular junction: some of them are delayed, others spread to the ventricular myocardium, causing them to contract at different rhythms. According to the frequency of ventricular contractions, tachysystolic (ventricular contractions of 90 or more per minute), normosystolic (ventricular contractions from 60 to 90 per minute), and bradysystolic (ventricular contractions of less than 60 per minute) forms of atrial fibrillation are distinguished.
During a paroxysm of atrial fibrillation, blood is not pumped into the ventricles (atrial supplementation). The atria contract ineffectively, so in diastole the ventricles are not completely filled with blood freely flowing into them, as a result of which blood does not periodically be released into the aortic system.
Atrial flutter is rapid (up to 200-400 per minute) atrial contractions while maintaining the correct coordinated atrial rhythm. Myocardial contractions during atrial flutter follow each other almost without interruption, there is almost no diastolic pause, the atria do not relax, being in systole most of the time. Filling the atria with blood is difficult, and, consequently, the flow of blood into the ventricles is reduced.
Every 2nd, 3rd or 4th impulse can arrive through the atrioventricular connections to the ventricles, ensuring the correct ventricular rhythm - this is the correct atrial flutter. If atrioventricular conduction is disrupted, chaotic contraction of the ventricles is observed, i.e., an irregular form of atrial flutter develops.
Symptoms you should definitely pay attention to
Cardiac arrhythmia in old age is insidious in that in the first stages it practically does not manifest itself at all. Each case is individual, and people may experience different feelings with the same diagnosis. Among the most common manifestations are the following signs:
- Weakness and shortness of breath;
- Dizziness and nausea;
- Lack of air, difficulty breathing;
- Increased fatigue;
- Sweating;
- Rapid pulse (above 100 beats per minute);
- Anxiety, causeless worry;
- Chest pain, tingling;
- Pre-fainting state.
Against the background of arrhythmia, symptoms of insufficient blood supply to the brain often occur. Agitation, emotional instability, and memory impairment can progress over time and lead to senile dementia, or dementia.
Diagnosis and treatment features
Making an accurate diagnosis is impossible without a number of studies. Therefore, you should not self-medicate and at the first characteristic symptoms you should consult a doctor. The following modern, informative methods are used for diagnosis:
- Visual inspection;
- Pulse measurement;
- Electrocardiogram;
- Monitoring using Holter;
- Ultrasound;
- MRI or CT.
Based on the data obtained, the doctor prescribes therapy. This may be medication or (in difficult cases) surgery. Medicines for arrhythmia are divided into three groups:
- Anticoagulants, or blood thinners.
Aspirin, Warfarin, Sikusar, Finilin - drugs in this group improve blood circulation and prevent the risk of blood clots in blood vessels. - Means for normalizing heart rhythm, slowing down the conduction of impulses
(Ritmonorm, Allapinin, Cordarone and others). If used incorrectly, these medications can be dangerous, so it is important to follow the dosage and administration instructions exactly. Additionally, it is necessary to constantly monitor pressure. - Beta blockers.
Helps improve oxygen supply to tissues and normalize blood pressure. Anaprilin, Vasocardin, Atenolol - these drugs need to be taken for a long time, as they have a cumulative effect. - Calcium antagonists.
Regulate the functioning of the heart muscle and slow down the heart rate. This group includes Diltiazem, Verapamil, Metoprolol.
If conservative therapy does not bring results for a long time, the doctor may decide to perform surgery (if the patient has no contraindications).
In order for treatment and recovery to be as effective as possible, older people are recommended to spend some time in a boarding house. There are many modern institutions that specialize in diseases of the cardiovascular system and offer patients excellent conditions for rehabilitation.
Arrhythmia prevention and lifestyle
To prevent arrhythmia, elderly patients are often prescribed medications containing potassium and magnesium. These substances have a beneficial effect on the functioning of the heart. To improve the absorption of beneficial components, you can additionally take vitamin B6.
Many sedatives of plant origin (valerian tincture, Persen, Novopassit) have a good effect. They improve sleep, relieve nervous tension, and, accordingly, reduce the likelihood of developing arrhythmia.
To prevent heart disease (including arrhythmias), it is important to pay great attention to lifestyle. Swimming, Nordic walking, even regular walks in the fresh air can improve the condition of the cardiovascular system.
Nutrition plays a huge role. The menu must include foods rich in magnesium and potassium (fresh vegetables, seafood, nuts, dried fruits). Eating foods made from whole grains is encouraged. It is important to avoid overeating. Doctors advise giving up tea and coffee, replacing them with freshly brewed compotes or fruit drinks. Bad habits are unacceptable. Smoking and alcohol increase blood pressure and increase cholesterol in the blood, which leads to arrhythmia and other heart diseases.
It is difficult to get rid of heart rhythm disturbances on your own. However, following simple rules and following the doctor’s recommendations can work a real miracle and return the heart to normal functioning.
Risk of long-term poor prognosis
The main prognostic criteria for atrial fibrillation are the causes and complications of arrhythmia. Atrial fibrillation caused by heart defects, severe myocardial lesions (large focal myocardial infarction, extensive or diffuse cardiosclerosis, dilated cardiomyopathy) quickly leads to the development of heart failure.
Thromboembolic complications caused by atrial fibrillation are prognostically unfavorable. Atrial fibrillation increases mortality associated with heart disease by 1.7 times.
In the absence of severe cardiac pathology and satisfactory condition of the ventricular myocardium, the prognosis is more favorable, although the frequent occurrence of paroxysms of atrial fibrillation significantly reduces the quality of life of patients. With idiopathic atrial fibrillation, health is usually not affected; people feel practically healthy and can perform any work.
In some cases, specific complications of atrial fibrillation are noted. Basically, diseases or health-threatening symptoms are observed against the background of other disorders and diseases.
- A specific disorder is the development of ventricular tachycardia, which is a consequence of cardiac arrhythmia.
- In the case of concomitant mitral stenosis, pathological fibrillation can provoke pulmonary edema due to the anatomical features of the body. An increase in pressure in the left atrium complicates the filling of the left ventricle, and as a result, reduces the intensity of blood flow in the pulmonary circulation.
- Intense pulmonary edema also develops with severe heart failure. The same dangerous condition develops against the background of systolic dysfunction of the left chamber against the background of irrational use of drugs with a pronounced negative inotropic effect.
- Experts call the risk of thromboembolism the most dangerous and difficult to predict. Impassive statistics say that a cerebral stroke develops precisely against the background of atrial fibrillation in every sixth case.
- Paroxysm of arrhythmia does not directly lead to death in patients. However, such a categorical prognosis is possible against the background of confirmed Wolff-Parkinson-White syndrome, as well as hypertrophic cardiomyopathy.
- Wolff-Parkinson-White disease, in turn, can lead to ventricular tachycardia, which will affect ventricular fibrillation. This dangerous condition offers a chance to save a life only if emergency medical care is provided.
- Among the dangerous factors that lead to dangerous complications is coronary heart disease. Some negative aspects can bring such “ordinary” diseases as bronchitis, food poisoning and alcohol intoxication, bronchial asthma and allergic reactions. Chronic atrial fibrillation can be caused by periodic and intense stress, disruption of the thyroid gland, as well as menopausal syndrome.
These complications and related factors explain the categorical need to undergo diagnostics or at least obtain consultations from specialized specialists: endocrinologist, neurologist, pulmonologist, allergist, infectious disease specialist and others.
If a rapid heart rate is suspected, the patient will be prescribed a number of necessary diagnostic procedures: transesophageal electrophysiological study, bicycle ergometry, daily ECG monitoring, echocardiography and more.
At the same time, preventive therapy is prescribed, the purpose of which is to maintain the stability of the pathological condition and minimize the pathological impact of adverse factors. Patients who have completed the course of treatment are prescribed sedative drugs and undergo mandatory periodic diagnostic examinations.
As a rule, the dosage of a maintenance drug is prescribed by a specialist based on the characteristics of the patient’s body and the course of the disease. The duration of taking the drug, which maintains the stability of the heart rhythm, is about a year.
The permanent form of atrial fibrillation requires lifelong use of maintenance medications that minimize heart failure, the likelihood of developing thrombosis, and other complications.
Patients are advised to abstain from alcohol and smoking. In order to prevent relapse, it is important to maintain a reasonable intensity of physical, emotional and mental stress.