Thrombosis of arteries and veins of the intestine is called “mesenteric” after the name of the vessels. Most often it is a complication of acute myocardial infarction, an attack of atrial fibrillation, or slow sepsis. Mesenteric thrombosis usually affects the superior mesenteric artery. Much less often it is found in the inferior artery and mesenteric veins.
Elderly and senile people are prone to the disease. As a result of blocking of the vessel, arterial or venous insufficiency of the intestinal section occurs, which leads to malnutrition and further infarction of the wall.
Thrombosis in veins is less common than in mesenteric arteries. The mixed form, in which blockage of both veins and arteries occurs, is rarely observed in very advanced cases.
The disease is difficult to diagnose. 1/10 of deaths from intestinal infarction occur in people under 40 years of age. Women are more susceptible to this type of pathology than men.
In the International Classification of Diseases (ICD-10), embolisms and thromboses of the iliac artery are coded I 74.5 and are included in the zonal group of pathology of the abdominal aorta. Venous mesenteric thrombosis is a component of acute vascular diseases of the intestine and has code K55.0.
Features of the blood supply to the intestines
The intestinal loops are in a “suspended” state and are secured in place by a dense mesenteric ligament. Arterial and venous vessels pass between the leaves. They are located almost parallel. The arteries (superior and inferior mesenteric) arise from the abdominal aorta and divide the blood supply into sections:
- The superior mesenteric artery carries blood to the small intestine, cecum, ascending colon, and most of the transverse colon. It carries out 90% of the blood supply, so the lesions are more widespread and clinically severe.
- The inferior mesenteric artery supplies a much smaller area (30% of the transverse colon, descending, sigmoid, rectum).
Between the main arteries there are “spare” collateral vessels. Their task is to help blood supply to the damaged area. A feature of intestinal collaterals is that they pump blood in only one direction: from the area of the superior artery to the inferior mesenteric. Therefore, in the case of upper-level thrombosis, no help can be expected from anastomoses.
Venous drainage from the intestine goes to the portal vein. Difficulty occurs when it narrows due to liver disease. Collateral circulation is formed by a group of portocaval anastomoses between the portal and vena cava. The small intestine is in the worst position. It does not have a developed collateral network.
Causes and risk factors
Mesenteric thrombosis is caused by blockage of the mesenteric bloodstream with a thrombus as a result of:
- atherosclerosis, in which the lumen of blood vessels narrows and the risk of thrombosis increases;
- myocardial infarction or endocarditis - a blood clot forms, which reaches the mesenteric arteries with the blood flow and clogs them;
- severe intestinal infection , inflammatory or tumor process in the abdominal cavity - tumors or abscesses can compress the mesenteric vessels, preventing normal blood flow in them;
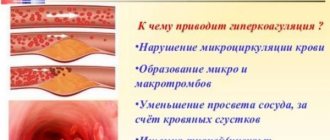
- hypercoagulation – increased blood clotting leads to thrombus formation;
- stagnation of blood in the vessels of the mesentery , which significantly increases the risk of vascular obstruction;
- trauma resulting in bleeding and blood clots may form.
The risk of mesenteric thrombosis increases if a person:
- reached old age (more than 60 years for women, 70 for men);
- suffers from heart and vascular diseases;
- underwent heart surgery;
- suffers from cirrhosis of the liver, which leads to increased pressure in the portal vein;
- suffered prolonged dehydration;
- leads a sedentary lifestyle;
- was subject to long-term chemotherapy.
Where do blood clots and emboli come from?
Through the arterial system, the embolus can reach the mesentery:
- from the heart in case of detachment of a parietal thrombus from the wall of a post-infarction aneurysm, during atrial fibrillation, from the inner layer (epicardium) during sepsis, destruction of valves;
- from the thoracic and abdominal aorta during vessel dissection, softening of atherosclerotic plaques;
- is formed in the mesenteric artery after traumatic damage to the inner layer.
Venous blood, having the opposite direction and a tendency to decrease speed and increase viscosity, is more susceptible to the formation of its own thrombotic masses. The formation of blood clots in the veins is caused by:
- inflammatory bowel diseases, affecting the entire wall, also involve venous vessels, local thrombophlebitis is formed;
- drop in blood pressure caused by various situations;
- portal hypertension in liver diseases;
- congestion in the underlying vessels due to portal vein thrombosis;
- any reasons that increase blood viscosity (diseases of the hematopoietic system, condition after splenectomy, long-term use of hormonal drugs to prevent pregnancy).
If the patient has a heart defect in which the right and left chambers communicate with each other (for example, patent foramen ovale), then a thrombus from the lower extremities can freely pass through the vena cava, the right atrium into the left ventricle and aorta, and then descend to the intestinal arteries .
Causes of the disease
Mesenteric thrombosis (otherwise known as mesothrombosis) occurs in patients who have just suffered from acute or chronic forms of cardiovascular pathologies.
Clots and thrombi form after damage to the heart muscle and vessel walls - in acute conditions, arrhythmias, inflammation, infections and aneurysms.
One of the severe manifestations is embolism of mesenteric vessels (formation of a clot and its rupture), which occurs as a result of the following heart diseases:
- A heart attack, due to which the blood is more susceptible to clotting, and changes in the speed of its flow through the vessels occur.
- Aneurysm.
- Mitral valve stenosis.
- Heart rhythm disturbance.
Such violations lead to the formation of an embolus - a blood clot that breaks off and moves along the vascular branches of the body. As a result, it enters the mesentery area, clogging large vessels (veins, arteries) and stopping the blood supply to the abdominal organs.
Thrombosis of the superior mesenteric artery is more common than its inferior “sister” and occurs due to physical trauma and secondary insufficiency in the mesentery.
Among the injuries, it can be caused by blows to the abdomen, followed by peeling of the internal walls of blood vessels and intima, which block further blood flow.
The causes of secondary vascular (both venous and arterial) insufficiency include the following pathologies:
- Stenosis that occurs as a result of atherosclerosis at the attachment points of the arteries to the aorta (branches at an angle): the speed of blood flow changes (decreases), the plaque that closes the vessel is damaged. The final condition is extensive necrosis.
- Deterioration of heart function with decreased pressure in the arteries. The result is stagnation in the blood vessels.
- Steal syndrome, which occurs during aortic repair operations; the accelerated blood flow, after freeing the vessel from the thrombus, is directed downward, sucking blood from the mesenteric branches into the main artery. The consequence is intestinal necrosis due to intestinal infarction.
- Tumors in the womb, compressing vessels - mainly the upper artery. The inferior artery in this area is much less likely to be damaged.
Read also: Probability of infertility with varicocele
There are also general conditions of the body that can give rise to the formation of blood clots:
- hereditary vascular pathologies - thrombophilia;
- increased blood viscosity due to long-term use of drugs;
- changes in endothelial cells due to chemotherapy, radiation, etc.;
- pregnancy;
- obesity;
- smoking;
- diabetes;
- Coxsackievirus, leading to heart failure.
Types of intestinal vascular damage
The classification of pathology includes different aspects of the mechanism of damage.
The reasons are distinguished:
- arterial thrombosis and embolism;
- venous thrombosis;
- secondary thrombosis of mesenteric vessels in diseases of the aorta;
- impaired vascular patency due to compression by germinating tumors;
- consequence of vascular ligation during surgery.
Depending on the degree of blood flow disturbance, stages are distinguished:
- compensatory,
- subcompensations,
- decompensation.
The pathological consequences of thrombosis can be:
- ischemia of the intestinal wall;
- site of infarction;
- diffuse peritonitis.
Light areas are viable tissues, dark areas are the infarct area.
In surgery, a stage of functional acute obstruction of the mesenteric vessels is distinguished, in which there is no organic lesion, and the pathology is caused by a temporary spasm.
The maximum damaging factor is abdominal trauma. Compensation does not have time to fully develop. Protective mechanisms increase blood clotting are activated, which aggravates the patient’s condition.
During operations on the aorta (narrowing of the isthmus, change in position for congenital defects, replacement of the aneurysm site with a graft), doctors know the possible mechanism of thrombosis of the mesenteric vessels: restored full blood circulation leads to a high flow rate through the thoracic aorta into the abdominal area and the femoral artery to the legs. In this case, partial “robbing” of the mesenteric vessels occurs due to the additional suction action of the jet. Small blood clots may form in the capillaries supplying the intestinal wall.
Thrombosis of mesenteric vessels - symptoms, diagnosis, treatment
Despite great advances in medicine, not all diseases have been thoroughly studied. One of them, thrombosis of mesenteric vessels, is characterized by high patient mortality rates. The disorder is formed due to blockage of the mesenteric veins by clots. An undeniable feature is its rapid development, which increases the risk of complications.
What it is
Definition of this disease: mesenteric thrombosis is a violation of blood circulation in the mesenteric vessels due to their blockage. Occlusion leads to acute ischemia, followed by the development of intestinal infarction and peritonitis.
Often the upper branches of the blood vein are damaged.
Pre-elderly and elderly people are at risk. They may have a predisposition in the form of a blood supply disorder, neoplasm, surgery or injury.
Forms and stages
According to the course format, chronic and acute are distinguished. It can be localized only in arteries, veins, or have a mixed type. First, blood flow is disrupted in the mesenteric arteries, then in the veins. The upper branches suffer more than the lower branches.
According to the degree, venous mesenteric thrombosis is divided into 3 stages:
- Compensatory. It is considered a chronic form, blood circulation is carried out due to healthy vessels.
- Subcompensatory. Partial blood supply to the intestinal tract is maintained.
- Decompensation. A severe stage characterized by irreversible consequences. There is no blood flow in the intestines, which leads to the development of a heart attack. The first phase is 2 hours, during which time there is a chance to reverse the process. After 4 hours, the next one occurs - gangrenous damage to the organ develops. This often ends in disaster.
The clinical picture of mesenteric thrombosis and symptoms can be different and make themselves felt not immediately, but some time after the development of the disease.
Why does it occur
A trombone mass can form due to excessive blood clotting. Hypercoagulability can be acquired, genetic or congenital.
The inner layer of the blood vessel wall takes part in various body processes. These cells synthesize substances that give the command to trigger coagulation.
In a normal state, they are fenced off from the bloodstream by walls; they penetrate into it when the cells are damaged. This can happen due to injury and a gap in the body's all-round defense against aggressive factors.
Against the background of trauma, surgery and other influences, cell walls become permeable. Small blood clots begin to form in it, which subsequently clog it.
Stagnation of blood leads to its stratification into fractions, which, when sticking together, form trombone masses. The reason may lie in insufficient activity or oncological pathologies.
It turns out to be a vicious circle: due to impaired blood circulation, traffic jams form.
Neoplasms in the abdominal area and interlacing of veins are also causes of intestinal infarction or ischemia. Against the background of compression of the arterial vein and blocking of natural blood flow.
Why is it dangerous?
This disease can develop in any part, the scenario is as follows: blockage of a blood vessel - necrosis. The danger depends on what will be affected. So, thrombosis of the heart arteries or in the abdominal cavity is a heart attack. Parts of the brain - stroke.
This organ is located inside a membranous “sac” consisting of connective tissue. In another way, it is called mesentery or mesentery. Due to blockage of the venous arteries, doctors make this diagnosis.
Symptoms
First of all, it is necessary to emphasize the first, striking sign that cannot be ignored - acute, unbearable pain in the abdomen. The location of the pain syndrome depends on which part of the circulatory system is damaged.
The causes of thrombosis of mesenteric vessels have already been discussed, so you need to know in what form the symptoms already tend to manifest themselves:
- In the early stages: nausea, gag reflex, fever, diarrhea. There may be blood streaks in the stool.
- At later stages, the patient may complain of rare stools. This occurs due to the disappearance of the peristaltic reflex of the intestinal tract. That is, a wave-like contraction occurs, which promotes the movement of fecal matter.
To detect this disease, undergo an examination; you should not delay the visit, so as not to complicate your current condition.
When and who to contact
Seeing a doctor is most often postponed if the patient has vomiting, diarrhea, or abdominal pain. They can be confused with food poisoning.
Consult a doctor in the following cases:
- diarrhea gives way to constipation;
- lump below the navel;
- unbearable pain in the abdomen, up to a state of shock;
- The muscles of the anterior abdominal wall are tense.
This is treated surgically. The patient requires emergency care for thrombosis of the mesenteric vessels.
If you feel that your condition is getting worse, call emergency medical help immediately.
Diagnostics
It is important to distinguish this disease in time from appendicitis, performative duodenal ulcer, ruptured ovarian cyst, and ectopic pregnancy.
If thrombosis of mesenteric vessels is detected, diagnosis includes the following procedures:
Laparoscopy is performed if the diagnosis cannot be established. The procedure is performed by a surgeon under anesthesia.
Treatment methods
Therapy depends on the time of the doctor’s report. This could be medication or surgery. But more often, people come in in extreme form, so treatment is impossible without a surgeon.
Medicines
Appropriate if thrombosis occurs in a chronic form. That is, blood circulation in the mesenteric veins is partially preserved.
Prescribe anticoagulants and disaggregation drugs for parenteral administration. The results of treatment are monitored through periodic blood and urine donations.
Surgery
It is performed for interstitial ischemia occurring in an acute form. Help is provided while the patient is being transported to the clinic. Every missed minute can lead to the death of the patient.
To alleviate the condition, the ambulance team resorts to the following actions:
- removing a blood clot from an area of the intestine;
- surgery on a damaged artery;
- resection of necrotic areas of the intestine;
- mixed type operation.
When the disease occurs at a late stage, surgical intervention is extremely difficult. Literally after 6-12 hours, the patient will be re-operated.
Prevention and prognosis
If a person begins to take timely preventive measures, this will help save life.
So, what needs to be done to maintain health.
If surgery was performed, follow the surgeon's recommendations. Even if you feel that it has become much better, do not start treatment, continue to the last course.
Forecasts
If the patient seeks medical help at stage 2-3, the chances of recovery are extremely low. The maximum level of survival is stage 1.
The blood clot is removed until necrosis has formed. A blood clot can clog any vein or artery; this is associated with severe intoxication of the body.
People who suffer from acute disorders of mesenteric circulation at the stage of decompensation die without surgical intervention. Therefore, seeking medical help and undergoing an examination is necessary. Then the chances of recovery increase several times.
: mesenteric thrombosis - intestinal infarction
Source: https://venaprof.ru/tromboz-mezenterialnyh-sosudov/
Stages and forms of blood supply disorders
We recommend reading:Rupture of an abdominal aortic aneurysm
Any circulatory disorders cause intestinal ischemia.
In the compensated stage, the damaged lumen of the vessel is completely replaced by the flow of blood through collaterals. This form is characteristic of chronic ischemia with a gradual course of the disease.
Subcompensation also depends on collaterals, but has clinical manifestations.
During decompensation, the entire period is divided into 2 phases:
- in the first 2 hours, reversible changes are possible with complete restoration of blood supply to the damaged area;
- after 4–6 hours, the irreversible phase of gangrenous changes begins.
Clinical signs of thrombosis
Symptoms of acute thrombosis of mesenteric vessels are determined by the level of circulatory blockage and the form of ischemia.
- Abdominal pain is intense in the subcompensation stage. Localized throughout the abdomen or in the navel and lower back. During the transition to decompensation (after 4–6 hours), the nerve endings on the intestinal wall die off, and the pain decreases. Such an “improvement” does not correspond to the actual extent of the pathology.
- Intoxication of the body is manifested by nausea, vomiting, and decreased blood pressure. Noteworthy is the discrepancy between the general severe condition and moderate abdominal pain.
- Peritoneal phenomena: the abdomen is tense, swollen, dense muscles are felt on palpation. The symptom is more typical of small intestinal thrombosis. During the stage of decompensation, peristalsis disappears, although in the subcompensated form it retains increased activity.
- Stool disorders - frequent diarrhea mixed with blood is possible in the initial stages of ischemia. With decompensation, when there is no intestinal motility, diarrhea stops.
- A state of shock is characterized by pale skin, thread-like pulse, tachycardia, cyanosis of the lips, and a drop in blood pressure.
Any, even short-term, pain in the abdomen requires attention.
Signs of pre-thombosis caused by arterial insufficiency can be identified by questioning and clarifying the patient’s complaints:
- pain in the abdomen along the intestines becomes more intense after eating or long walking;
- tendency to unstable stool, alternating diarrhea and constipation;
- unclear weight loss.
Thrombosis of mesenteric veins is milder and slower. More often it is a chronic process.
Development of the disease
The course of the disease from the initial stage to the occurrence of complications has its own characteristics and characteristics.
The formation of thrombosis occurs due to liquefaction of blood in the vessels. Such low-quality blood clogs the arteries and therefore blood clots occur. In the initial stages and if there is a risk of thrombosis, the patient is prescribed blood thinning medications. But if the moment of liquefaction of the blood clot was missed, then surgical intervention is urgently necessary. Otherwise, intestinal gangrene develops.
Stages of the disease:
- Intestinal ischemia. It is characterized by unbearable pain in the abdomen, in the gastric region, bilious and bloody vomiting, liquid feces with blood in it. At this stage, the damaged organ is subject to restoration.
- Intestinal infarction. It is characterized by the complete onset of intestinal death, followed by infection in the internal organs. The intestinal walls are destroyed. The patient experiences constipation, which also leads to intoxication of the entire body and gradual poisoning by toxins. According to external signs, the patient becomes very pale, and the skin appears blue. Painful sensations in the abdomen do not stop after taking painkillers.
- Stage of peritonitis. The blood circulation in the intestines stops functioning. The patient experiences complete poisoning of the body with toxic substances. Abdominal pain is eliminated and does not bother the patient. Additionally, a symptom of vomiting appears. The patient's abdomen, instead of hard, becomes soft and slightly swollen. But there is no gas formation or urge to defecate. If urgent surgical intervention is not undertaken at this stage, the patient will experience complete intestinal paralysis. Additional symptoms include a change in skin color to earthy and an increase in body temperature.
The stage of peritonitis is the last stage of the disease. In ninety percent of cases it is fatal. Due to the fact that surgical intervention for complete gangrene of the intestine becomes impossible. Also, there is no way to eliminate intoxication of internal organs.
The patient falls into the hands of a doctor at each stage. The subsequent development of events depends on the period in which the patient began to receive treatment:
- blood circulation is completely restored and normalized with intestinal-compensated recovery;
- Blood circulation in the intestine is restored, but not to its full extent in case of subcompensated thrombosis;
- The result of ischemia, infarction and the inability to restore the intestinal walls - in the decompensated course of the disease.
There are unfavorable mortality statistics for mesenteric intestinal thrombosis. Half of the people who get sick die. This is due to seeking medical help too late.
Thus, in order not to be at risk of serious complications, you should be attentive to the sensations in the body and, if you feel unwell, seek examination from a doctor. Such reinsurance can save lives.
https://youtube.com/watch?v=FmJ2wnJRLp8%3Fecver%3D1
Diagnostics
In order to make a correct diagnosis, it is important for the doctor to get answers to questions about the initial manifestations, duration of pain, and characteristics of the stool.
The decisive method is diagnostic laparoscopy, which allows you to examine the intestines and clarify the stage of ischemic changes and the localization of the area.
Leukocytosis with a shift of the formula to the left does not provide certain information, since it is characteristic of many diseases. An elevated level of the enzyme lactate dehydrogenase indicates the presence of necrotic tissue.
Ultrasound of the abdomen and fluoroscopy can provide some assistance in differential diagnosis. Preparing the patient and wasting time on angiography is not rational.
Inspection of the intestine allows you to detect a blood clot or ischemic area
If laparoscopy is not possible, doctors proceed to laparotomy - an operation with a large incision in the midline of the abdomen:
- examine (perform an audit) the abdominal organs and intestines;
- palpate the mesenteric vessels to identify a thrombus;
- assess the sufficiency of arterial pulsation;
- determine the boundaries of viable tissues.
Treatment
Treatment of thrombosis of intestinal vessels is possible only with immediate surgery. The introduction of painkillers and antispasmodics erases the clinic and delays the diagnosis.
For vein thrombosis, fibrinolytic therapy is indicated in the first 6 hours.
During the operation, the doctor must find ways to:
- in the absence of necrotic changes, restore the patency of blood flow through the vessel to relieve ischemia from the affected area of the intestine;
- remove the altered intestine or part of it and sew the upper and lower ends.
Restoring blood supply is carried out in the following way:
- squeezing out a blood clot with your fingers;
- creation of a bypass shunt between the upper and lower levels of the stenosis, bypassing the thrombosed area.
In the postoperative period, the patient is prescribed large doses of Heparin to thin the blood.
An angiogram of the intestinal arteries in an emergency is difficult because it requires patient preparation
Intestinal thrombosis: causes, forms, course, diagnosis and therapy, surgery and doctor’s prognosis
Mesenteric intestinal thrombosis is a rather dangerous disease, the outcome of which depends entirely on the timely provision of medical care. There are cases when a patient did not turn to doctors for qualified help, resulting in death.
In case of thrombosis or embolism of the intestine, the passage of the mesenteric vessel is closed, which provokes vasospasm, as a result of which the nutrition of the affected area of the intestine is disrupted, and as a result, necrosis of the wall occurs. Due to such changes in the body, the patient may develop peritonitis.
The danger of the disease is that many patients may confuse it with other pathologies!
The main symptom of thrombosis is acute abdominal pain. Most often, the patient’s relatives immediately call an ambulance.
However, it is quite difficult to make a diagnosis without the necessary examinations, so the patient may be admitted to the hospital with suspected appendicitis, cholecystitis or intestinal obstruction.
Already in the hospital, after a series of examinations, the doctor will be able to find out the reason for the deterioration in health. The faster this happens, the lower the likelihood of subsequent complications.
Main symptoms of intestinal thrombus
- Severe abdominal pain - at first it can be paroxysmal, but over time it becomes constant and unbearable. There is no clear localization of the pain; it can be described as shingles.
- Nausea, vomiting - possibly mixed with bloody clots.
- Changes in the consistency of stool - it becomes frequent, liquid, and it is also possible to discharge blood along with the feces.
- Fluctuations in blood pressure;
- Increase in general body temperature.
- Pale skin, cold sweat.
- Hard belly (bloating may also be present).
However, it should be repeated once again: you cannot make a diagnosis yourself! This can only be done by a specialist, after a series of examinations.
Diagnosis of intestinal vascular thrombosis
Basic studies that the patient needs to undergo:
- clinical blood test;
- angiography of the walls and intestinal vessels;
- laparoscopy;
- radiograph;
- laparotomy and other examinations that help determine the condition of the patient’s intestines.
Intestinal vascular thrombosis is a disease that requires serious treatment. If a person does not seek qualified help in a timely manner, then it is quite possible that death may occur.
One of the most important symptoms that allows the doctor to immediately make a diagnosis is unbearable pain that does not go away even after painkillers. The patient does not feel relief, even while under the influence of opiates and other drugs used in medicine.
Treatment of intestinal vascular thrombosis in the early stages
If a person seeks help in a timely manner, then doctors prescribe conservative treatment using various medications. This may be an anticoagulant or thrombolytic, which are administered intravenously.
In most cases, conservative treatment of mesenteric arteries is unacceptable, since antispasmodics and other medications lead only to temporary relief of the patient’s condition - in the end, surgical intervention will still be required.
The sooner it is carried out, the better for the patient.
Before performing a surgical intervention, the doctor must take all preoperative preparation measures in order to correct changes in central hemodynamics. Let's consider the mandatory components of preparation for surgical intervention to remove OMAN:
- Examination of the patient's intestines by palpation. The doctor must carefully examine the mesenteric vessels, starting from the very mouth.
- Search for the presence of pulsation in the mesenteric arteries, as well as at the borders of the damaged intestine. If the doctor has doubts, in this case a dissection of the mesentery is performed (scientifically, to establish arterial bleeding).
Surgical intervention can be carried out by performing the following manipulations:
- If intestinal necrosis has not begun, then complete restoration of blood circulation is carried out.
- In case of intestinal pathology, the doctor improves the blood supply to the area.
- Elimination (resection) of pathology.
Carrying out embolectomy for mesothrombosis
However, this operation is quite dangerous, since there is a high probability of death for the patient, so in most cases the doctor takes all necessary measures to completely restore blood flow. Here it should be added once again that the outcome of the surgical intervention depends entirely on the patient - the sooner he seeks medical help, the higher the chance of his salvation.
If you contact a doctor too late, the intestines may become completely dead - in this case, surgery is contraindicated - the patient may die on the operating table.
Stages of development of intestinal thrombosis
The disease develops as a result of the fact that the blood begins to liquefy, as a result of which blood clots appear that clog the arteries. That is why in the initial stages the patient is prescribed blood thinning drugs. However, if the disease was detected already in the last stages, there is no need to hesitate - urgent surgical intervention is required before intestinal gangrene begins.
Let's consider the main stages of the disease:
- Intestinal ischemia - in this case, damaged organs must be restored. The most important symptom of ischemia is severe, unbearable pain in the stomach, vomiting with bile and blood. The feces are liquid, may change color, and spotting is also observed.
- Intestinal infarction - the death of the organ begins to occur, resulting in intoxication of the entire body. The intestinal walls are destroyed, resulting in prolonged constipation - which also leads to poisoning of the body with poisons. You can observe severe paleness of the skin - even cyanosis. Painkillers do not work, the patient's condition is critical.
- Peritonitis - in this case, one can already note the complete poisoning of the body with toxins, the circulatory system practically does not function. At this stage, the pain is practically not bothersome, but frequent vomiting begins. The abdomen upon palpation is soft, slightly swollen. If no measures are taken, complete paralysis of the intestines occurs - there is no stool, as well as gases. Body temperature may rise, and the complexion takes on an earthy tint. This is the last stage, which in 90% of cases ends in the death of the patient - due to the fact that surgical intervention is impossible due to gangrenous changes in the intestine.
Depending on the stage at which the patient decided to seek help, three scenarios can be distinguished:
- compensated recovery – the blood circulation process is completely normalized;
- subcompensated – blood circulation is restored, but partially;
- decompensated course of the disease - implies the impossibility of intestinal restoration, resulting in its infarction.
Unfortunately, this disease has a very high mortality rate. This dynamic is due to the fact that today many people prefer self-medication and self-diagnosis. If in some cases this is acceptable, then intestinal thrombosis is a dangerous disease that requires immediate surgical intervention.
Painkillers can dull the pain for a while, but the process of necrosis still occurs - and the further it goes, the less likely the patient is to save his life.
Types of surgical intervention for intestinal thrombosis
If intestinal obstruction occurs, then the specialist performs partial removal of the damaged tissue. After which the remaining healthy areas of the organ are stitched together. Bypass surgery can also be performed - a passage is artificially created around the blocked vessel, thanks to which blood can circulate freely.
Acute mesenteric ischemia requires immediate surgery. In the diagnostic field, the doctor himself chooses the treatment tactics: bypass surgery, angioplasty, or removal of a blood clot that obstructs blood flow can be performed. Thanks to these procedures, it is possible to restore the intestines and also avoid tissue necrosis.
Mesenteric ischemia requires long-term recovery, as well as taking special medications (to thin the blood) for 6 months after surgery.
Postoperative period: recovery, diet
After surgery for intestinal thrombosis, the patient necessarily needs time to recover. Some complications may occur if you do not strictly follow all the doctor’s instructions:
- scar suppuration;
- the appearance of adhesions;
- painful sensations.
If such symptoms occur, you should immediately contact your doctor.
As a rule, the patient remains in the hospital under the supervision of specialists for about two weeks after surgery. He is not allowed to lift weights. The patient must spend almost all of his time lying down. The use of baths is prohibited, but you can periodically take a warm shower. Experts recommend doing a light abdominal massage.
An important factor in good health is the complete restoration of intestinal function. To do this, the patient is prescribed to follow a special diet, which consists of eating the following foods:
- semolina porridge;
- butter;
- whey, fermented baked milk and other dairy products.
It is recommended to completely exclude smoked meats, alcohol and spicy foods from your diet. If we talk about preventive measures, the main factor also remains proper nutrition and a healthy lifestyle. Smoking and drinking alcoholic beverages with intestinal thrombosis are contraindicated.
Based on all of the above, we can conclude: intestinal thrombosis is a dangerous disease that is quite difficult to treat. The main thing is to detect the disease in time and neutralize it.
Source:
Intestinal thrombosis: why does it occur and how to treat the pathology?
Intestinal thrombosis is a condition characterized by the formation of a vascular clot (thrombus) in the arteries or veins responsible for the blood supply to the intestine. Blockage of blood vessels leads to the fact that the organ does not receive enough oxygen, against which ischemia and necrosis develop.
How does the chronic form of thrombosis manifest?
The chronic form of thrombosis should be considered in patients with heart failure complicated by myocardial infarction. The clinic distinguishes 4 stages:
- I - the patient has no complaints, the thrombus is an accidental finding during angiography;
- II - typical complaints of pain along the intestines after eating, the person refuses food because of this;
- III - constant pain, flatulence, impaired absorption of the small intestine, diarrhea;
- IV - the occurrence of intestinal obstruction, which manifests itself as an “acute abdomen”, with peritonitis and gangrene.
Prevention of mesenteric artery thrombosis
Prevention of mesenteric artery thrombosis comes down to maintaining a healthy lifestyle and quitting smoking. It is also important to monitor your body weight to prevent obesity.
It is imperative to treat all diseases that pose a threat to the formation of a blood clot. We are talking about atherosclerosis, rheumatism, arrhythmia, etc.
Author of the article:
Volkov Dmitry Sergeevich | Ph.D. surgeon, phlebologist Education: Moscow State Medical and Dental University (1996). In 2003, he received a diploma from the educational and scientific medical center for the administration of the President of the Russian Federation. Our authors
Forecast
Mesenteric thrombosis, according to clinical studies, is observed much more often than the number of cases diagnosed. This pathology is masked by various acute conditions: cholecystitis, renal colic, appendicitis. The limited time for diagnosis does not always allow the disease to be detected.
Fatal cases, according to pathologists, are 1–2.5% of hospital mortality. These are thrombosis in the stage of infarction and diffuse peritonitis. Late surgery (after 12 hours) means high mortality (up to 90%).
A good prognosis for recovery with surgical treatment of chronic thrombosis in the first two stages. Timely seeking surgical help for abdominal pain allows the patient to be operated on in a favorable time frame and prevent perforation of the intestinal wall.
How is the operation performed?
Thrombosis of the mesenteric arteries requires invasive treatment methods - surgery is mandatory.
The need for surgery is due to the high mortality rate if the clot is not removed in time. It is impossible to influence it with medication or alternative medical methods in such an acute condition, since complications arise within a couple of hours.
The patient is taken to the hospital urgently, since the condition develops very quickly and death can occur within the first 5-12 hours after symptoms are detected.
Surgical intervention includes:
- Removal of the blood clot itself, which blocks the blood flow.
- Reconstruction of a vessel affected by the consequences of thrombosis.
- Removal of dead parts of organs is only at stage 2 (infarction), when the lesion has already led to necrosis.
- Drainage of the abdominal cavity - if the operation is performed at the stage of peritonitis, and the inflammatory process has spread to the entire abdominal cavity.
Read also: Varicocele differential diagnosis