Medical Center » Diagnostics » Functional diagnostics » Bicycle ergometry (VEM)
Prices Doctors Info
Sign up
Bicycle ergometry
is one of the stress tests that is used to identify diseases of the cardiovascular system. The basis of the technique is a comparison of data obtained after an ECG, as well as measurements of the patient’s blood pressure at rest, during a gradual increase in physical activity and after its completion.
At SM-Clinic in Moscow, bicycle ergometry is performed using expert-level equipment, which guarantees the most accurate and reliable results.
Why is bicycle ergometry performed?
This diagnostic method makes it possible to assess the severity of existing cardiovascular pathologies, as well as identify their hidden symptoms.
At SM-Clinic, different categories of patients can undergo VEM. Thus, using the test, our specialists will determine the severity of coronary heart disease and the functional class of angina in people experiencing pain during physical activity. In addition, we recommend that people who are at risk undergo bicycle ergometry for early diagnosis of pathologies, namely:
- suffer from arterial hypertension;
- have high cholesterol levels;
- are subject to the harmful habit of smoking.
The advantages of examination at SM-Clinic are undeniable. Among them:
- Using a modern Tunturi simulator, as well as the latest generation cardio equipment. Thanks to this, high efficiency and informativeness of the examination and reliable results are guaranteed.
- Conducting a stress test on the heart by functional diagnostic doctors who have undergone special training and have significant practical experience in conducting examinations of this type.
- Favorable cost of diagnostics. Prices for bicycle ergometry at SM-Clinic are affordable for most of our patients.
Tips for passing (for patients)
The need to come in clothes special for this purpose, which do not restrict movement, to ensure the necessary load, since an incorrectly chosen wardrobe can hinder movement, reduce the degree of load, or, conversely, increase it.
Since during the procedure you need to pay attention to the most vulnerable areas in the electrode - amplifiers - recording system, one of which is the place of contact of the electrodes with the human skin. From this it is clear that preparing the skin for bicycle ergometry is no less important.
Before starting the procedure, wipe the shaved areas with a concentrated alcohol solution and wait until they dry. After drying the treated areas, these areas are highlighted with a special pencil and gently wiped with fine sandpaper or other rough material, for example, special disposable exfoliating graters, microabrasive strips, tampons with a special gel with microparticles.
When these recommendations are followed, the resistance of the skin is reduced to optimal, namely 5000 Ohms or less. It should be remembered that the most modern ones, such as disposable electrodes, if this technology is followed, such preparation of the skin as treatment with alcohol not only does not require, but is not recommended.
In this case, this can cause an increase in skin impedance due to dehydration of its upper layer (stratum corneum). When using disposable electrodes, the skin is wiped with a damp cloth instead of an alcohol consistency, which helps degrease it and at the same time promotes hydration (attachment of water molecules to molecules or ions).
Indications for bicycle ergometry
It is recommended to undergo bicycle ergometry if there are certain indications, which include:
- The patient complains of pain in the chest area, which is not accompanied by changes during an ECG.
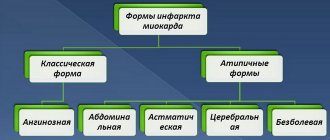
- Post-acute myocardial infarction. In this case, a prognosis of the patient’s health condition is made.
- Preparation for coronary angiography.
- Disturbed lipid composition of the blood, in which clinical symptoms of coronary artery disease do not appear.
- The patient's age is over 40 years and there is a high risk of developing coronary disease due to the specifics of the profession. This category includes pilots, divers, drivers, etc.
Evaluation of results
Decoding the obtained indicators is a comprehensive analysis of all indicators of heart function, blood pressure, heart rate, etc. It shows how developed the pathology or complication is.
Test score
After bicycle ergometry, the cardiologist issues a conclusion to the patient, which indicates:
- reasons for stopping the load,
- the amount of work done, measured in J,
- blood pressure and heart rate readings,
- patient's performance,
- type of blood pressure response to the received load,
- recovery time,
- heart rate characteristics,
- presence or absence of coronary changes,
- degree of neglect of ischemia.
After receiving the conclusion, the doctor can additionally refer the patient for a heart examination, but with the help of coronary angiography, ultrasound examination of the heart, and blood vessels. If necessary, he will offer surgery on the organ, but this occurs in severe cases of the disease.
Bicycle ergometry is a proven method for diagnosing the cardiovascular system, which is gaining momentum. It has gained popularity due to the accuracy of the indicators, physiology, accessibility and the chance to repeat the procedure again. The cost of bicycle ergometry in Moscow blades varies between 3,000 rubles. If we talk about clinics in St. Petersburg, then the cost drops to 1500-1700 rubles. The method can be used not only for diagnosing diseases, but also for preventive examinations of athletes, people over 40 years old, conscripts, etc.
Contraindications to bicycle ergometry
Bicycle ergometry is the most optimal way to assess the severity of existing heart and vascular diseases, as well as early detection of their hidden signs. At SM-Clinic, different categories of patients can undergo examination. For example, using the test, you can determine the degree of coronary heart disease, the functional class of angina in people with pain resulting from physical activity. In addition, we recommend performing bicycle ergometry for early diagnosis of diseases in people at risk: those suffering from arterial hypertension, high cholesterol, and smokers. A stress test is also carried out on healthy patients over 30 years of age who decide to take up fitness for the first time to determine optimal physical activity.
Indications for examination
Despite the relative safety of VEM, there are a number of contraindications to its implementation. Among them:
- high arterial hypertension;
- unstable angina;
- pericarditis and myocarditis in the acute stage;
- congestive uncompensated heart failure;
- acute infectious process, which is accompanied by fever;
- serious disturbances of heart rhythm and conduction;
- active thrombophlebitis;
- stroke;
- pulmonary embolism;
- aneurysm of the aorta and other large vessels;
- severe respiratory failure;
- multivalve heart defects;
- severe hypotension leading to fainting;
- the presence of malignant neoplasms;
- blood diseases.
Also, bicycle ergometry should not be performed on patients with diseases that require restrictions on physical activity.
Cardiac auscultation technique and points
Auscultation of the heart is considered the most accurate of the most informative methods for diagnosing diseases of this organ. Note that the doctor performing the listening must have excellent hearing, but more importantly, be able to listen, that is, recognize noise by amplitude and time. Auscultation is the most complex method for diagnosing diseases of the cardiovascular system.
- The invention of the device and the emergence of the method
- Goals and objectives of the study
- Standard procedure
- Auscultatory zones of the heart
- Changing the sonority of tones
- Noise detection
There are certain rules for conducting research. Data is sampled at five points. During diagnostics, a stethoscope (phonendoscope) is used.
The invention of the device and the emergence of the method
The stethoscope at first was a rigid tube for one ear. The history of medicine owes its invention to the invention of the device and the advent of a method for listening to the heart to the French doctor Rene Laennec. In 1816, he invented the stethoscope, and just a year later he described his experience in the work “Indirect Auscultation”. The main symptoms were discovered and systematized by this Frenchman.
Monaural wooden tubes have been in common use for over a century. In the first half of the twentieth century, rural doctors and paramedics continued to use this model.
After the release of binaural instruments, doctors made several more observations. For example, the murmurs of mitral stenosis (low-frequency sounds) are better heard through a bell-shaped stethoscope. Whereas aortic insufficiency (sound at high frequencies) is more clearly distinguished when using a membrane tip. In 1926, a binaural phonendoscope with a combination head was released.
The next step in improving the design of the device was the invention of electronic auscultatory instruments: stethoscopes with the ability to amplify sound, filter noise, as well as sound “visualization” (phonocardiograph).
Data obtained through a physical examination of the patient are not only signs of disease, but also provide a more complete picture of the functionality of the human circulatory system:
- cardiac output assessment;
- determination of pressure when filling chambers;
- volemia;
- the nature and extent of valve pathologies;
- localization of lesions in the system, and so on.
This not only improved the possibility of making a diagnosis, but also contributed to the prescription of more adequate therapy.
Goals and objectives of the study
The main purpose of diagnosis is to recognize a patient’s heart disease through analysis of its rhythm. While working, the organ is in constant tension, its individual parts move at a certain frequency, promoting the “dispersal” of the blood mass. Due to this movement, vibration occurs, reaching the surface of the breast through the adjacent soft tissue. You can listen to them. Using the heart auscultation technique, doctors:
- assess the nature of the sounds “produced” by the heart muscle during operation;
- characterize them;
- identify the causes of their occurrence.
First of all, the doctor checks the heart rhythm at standard points in a certain order. If changes have been identified and a number of accompanying symptoms indicating pathology are observed, additional listening is carried out:
- the whole area of absolute cardiac dullness;
- area above the sternum;
- left axillary fossa;
- interscapular space;
- carotid and subclavian arteries (in the neck).
Standard procedure
The rules for conducting the study are quite simple. Preparation is required in rare cases: if the patient has a lot of hair on his chest, then before auscultation the hair is moistened with water or greased. Sometimes the listening areas need to be shaved.
The first stage of the procedure is carried out in a sitting or standing position. The algorithm is then repeated with the patient lying down. He is required to take a deep breath, exhale and hold his breath for a moment. Sometimes special techniques are used:
- several gymnastic exercises;
- listening while lying on your side;
- listening when inhaling, straining.
Certain segments are listened to one by one: the standard algorithm is five points, with additional assignments - other areas.
Auscultatory zones of the heart
Auscultation points are examined in the following order:
- Apex impulse point: area of the mitral valve and left atrioventricular orifice;
- The point of the second intercostal space is the right edge of the sternum: the region of the valve and the mouth of the aorta;
- The point of the second intercostal space is the left edge of the sternum: the region of the pulmonary valve;
- A point in the lower third of the sternum at the base of the xiphoid process and the place of attachment of the V-shaped rib to the right edge: the area of the tricuspid valve and atrioventricular foramen;
- The point of the third intercostal space is the left edge of the sternum: the area of the aortic valves.
Heart auscultation points
1st zone. Palpation of the area where the apex beat is located. If it cannot be palpated, the left border of the relative dullness of the heart is determined by percussion. Installation of a phonendoscope. The tool is applied to the identified point. The patient takes a deep breath, exhales and does not breathe for 3-5 seconds. Next, you need to listen to sounds, identify and evaluate them.
The first tone appears after a long pause, the second tone - due to a short one. The first tone, moreover, is consonant with the pulsation of the carotid artery (palpation is performed). The norm corresponds to twice the volume of the first tone. If it is higher than twice, strengthening is stated; weaker or equally – weakening. Sometimes the rhythm is determined in three keys.
The triple tone of a healthy (normal) heart is more often observed in pediatric patients. In adults, only in the period of 20-30 years of age can one hear three tones. But they have other noises: the rhythm of a quail, the rhythm of a gallop, the bifurcation of the first tone.
2nd zone. Palpation of the second intercostal space on the right, installation of the device. The patient inhales and exhales while holding his breath. And again the researcher hears two-tone consonance.
What is heard is assessed by the volume of the second tone:
- stronger – the condition is normal;
- lower or equal – weakening at this point;
- fuzzy echo – splitting;
- clear two sounds in one - bifurcation.
3rd zone. Palpation of the second intercostal space on the left, installation of the device. The patient takes a deep breath, exhales and holds his breath for a few seconds. Here, as in the study of the 2nd point, one listens to the second tone. Normally, tone II is louder. Deviations are considered by analogy with the previous zone. Next, repeated auscultation is performed to compare the amplitude of the sound of the second tone. If there is a strong increase in the volume of this tone, the emphasis shifts to the aorta or pulmonary artery.
4th zone. Palpation is performed at the indicated point, and a phonendoscope is installed. Inhale and exhale again, holding your breath. The tonality indicators are similar to the assessment of heart sounds at the first point, that is, in a healthy person, here the first tone is louder than the second.
5th zone. The researcher repeats all the steps:
- palpation in a specific area to determine the point of installation of the phonendoscope;
- command the patient to inhale and exhale and hold his breath;
- listening to sounds, identifying tones and evaluating them.
In the area of the aortic valves, the sound strength of both tones in a healthy person is approximately the same. Deviations in the ratio at this point have no specific meaning when making a diagnosis. Noises between tones are defined as:
- systolic (in the interval between the I and II sounds);
- diastolic (in the interval between the II and I sounds).
Changing the sonority of tones
A weakening or strengthening of the tone indicates many things. For example, a change in the sound of tone I occurs due to:
- decreased airiness of lung tissue;
- paralytic or barrel-shaped, thick chest;
- chest emphysema;
- effusion in the pericardial area;
- damage to the heart muscle;
- myocarditis, cardiosclerosis;
- destruction of valves, reduction in the amplitude of movement of the valves;
- mitral and tricuspid insufficiency;
- reducing the rate of pressure rise in the cavities of the ventricles.
Strengthening of the first tone is observed with mitral stenosis, and so on.
Change in the sound of the second tone: a short-term emphasis on increasing is observed with emotional outbursts, excessive excitement, and also as a symptom of hypertension. A decrease in the sound intensity of the second tone is a sign of aortic valve insufficiency.
At the 3rd point, an increase in the volume of the second tone is always with mitral stenosis and other heart defects of any nature.
In addition to tonality, auscultation makes it possible to listen to pathological sounds, for example, clicking. They are characterized by high-pitched sound, inconsistency, and short duration.
Noise detection
If auscultation of the heart reveals murmurs in the main zones, then they are analyzed as follows:
- phase of the cardiac cycle of listening to the sound, in which part it is heard;
- duration;
- sound strength in general and sound gradation throughout the phase;
- variability (strength, timbre, duration in different body positions, respiratory periods and physical stress).
The described diagnostic measure allows you to identify health problems. In case of insufficiency, high-frequency and low-frequency auscultatory symptoms are also considered.
The latter is more often associated with the movement of blood mass, while the former is more often associated with the speed of flow. These sound vibrations are defined as noise, but this terminology also applies to tones.
As an example, consider mitral regurgitation. With this dysfunction, the left ventricle (LV) directs blood flow into the aorta and back into the left atrium (LA), therefore, the pressure in it is greater. But in the LP it’s low. The gradient of this indicator can be up to 65 mmHg. This means that with mitral insufficiency, the blood flow rate is high, and the noise is defined as high-frequency.
High-frequency sound vibrations are observed with minor mitral regurgitation (valve incompetence leading to flow from the left ventricle into the left atrium due to contraction).
The presence of low-frequency noise indicates that regurgitation is severe, that is, insufficiency can be severe with rupture of the chordae tendineae of the valve.
Auscultation (or the method of physically listening to the “music” of the heart), detection of changes in the sound of tones and analysis of the information obtained indicate the following:
- weakening of the first tone – insufficiency of the mitral and aortic valves;
- strengthening of the first tone – stenosis of the left atrioventricular orifice;
- weakening of the second tone – aortic valve insufficiency, hypotension;
- increased tone II – hypertension, pulmonary hypertension;
- bifurcation of the first tone – bundle branch block;
- bifurcation of the second tone – stenosis of the aortic mouth, hypertension.
Auscultation gives an idea of the noise:
- systolic – stenosis of the aorta or pulmonary trunk, mitral and tricuspid valve insufficiency;
- diastolic - narrowing of the left or right atrioventricular orifice;
- pericardial friction with pericarditis;
- pleuropericardial friction - inflammation of the pleura adjacent to the heart.
The heart is the most important organ. It is very important for our health that it functions without failure! Auscultation helps to identify these failures.
– by leaving a comment, you accept the User Agreement
- Arrhythmia
- Atherosclerosis
- Varicose veins
- Varicocele
- Vienna
- Haemorrhoids
- Hypertension
- Hypotension
- Diagnostics
- Dystonia
- Stroke
- Heart attack
- Ischemia
- Blood
- Operations
- Heart
- Vessels
- Angina pectoris
- Tachycardia
- Thrombosis and thrombophlebitis
- Heart tea
- Hypertension
- Pressure bracelet
- Normalife
- Allapinin
- Asparkam
- Detralex
Features of preparation
No serious preparation is required before performing VEM. On the eve of the examination, you must avoid smoking and do not drink coffee, energy drinks, or alcoholic drinks. It is undesirable to allow great physical or psycho-emotional stress. If the patient is taking nitroglycerin and its derivatives, drugs from the group of beta-blockers, ACE inhibitors, in agreement with the attending physician two to three days before the examination, they must be discontinued. The last meal is allowed no later than 2-3 hours before the test.
How is the examination carried out at SM-Clinic?
How is bicycle ergometry performed in the clinic?
First, the doctor measures the patient's blood pressure and takes ECG readings at rest. To do this, the patient lies down on the couch, sensors are attached to him, and he is transferred to a bicycle ergometer. At first the patient pedals at a normal pace, but the load increases every 2-3 minutes.
Your doctor may stop an exercise test for several reasons, including:
- Achieving the required heart rate: usually 75-80% of the maximum load. It is calculated individually for each patient, taking into account his age, gender and weight.
- The appearance of pain in the chest, shortness of breath, and a strong increase in blood pressure in the patient.
ECG and blood pressure measurements are performed every 2 minutes.
The examination takes about 20 minutes. After the test, the specialist immediately deciphers the readings. If no patient complaints are recorded, there are no changes on the ECG, and a high level of performance has been achieved, the test is considered negative. If abnormalities are detected, the doctor will advise you to consult a cardiologist.
Registration for examination, price of bicycle ergometry
The examination at SM-Clinic is carried out under the supervision of experienced doctors who will competently interpret the test results and give an expert opinion.
You can get detailed information about bicycle ergometry, find out prices or sign up for a study from contact operators.
General information
Bicycle ergometer research is one of the newest methods that appeared in the 21st century. The patient may not be aware of pathologies of the cardiovascular system that initially develop asymptomatically in his body. It is possible to identify diseases such as, for example, cardiac ischemia or pathology of the coronary vessels only during physical activity. The tests are carried out on a special simulator - a cardio bicycle, while using sensors attached to the patient's upper body, an electrocardiogram (ECG) is taken and changes in blood pressure are recorded. VEM is used in the following areas:
- Cardiology - for diagnosing specific diseases of the cardiovascular system (CVS).
- Pulmonology - simultaneous VEM and gas analysis helps to more accurately establish a diagnosis for pulmonary pathologies.
- Sports medicine - used to select training or rehabilitation programs.
VEM is accompanied by complex physiological reactions in the human body. As under any other load, during a bicycle ergometer test, all human organs experience an increased need to supply them with oxygen. Externally, the aerobic nature of the effect is manifested by rapid breathing. The musculoskeletal system receives more oxygen due to the redistribution of blood flow - most of it is directed not to the internal organs, but to the muscles.
During dynamic exercise, blood pressure and heart rate increase. The heart, in fact, is a muscle and also needs an additional supply of oxygen, which should be provided by the coronary vessels. If the blood circulation in them is impaired, this will manifest itself in a lack of oxygen for the heart and will be displayed on the ECG. As a result, deciphering VEM indicators makes it possible to diagnose hidden pathologies of the cardiovascular system.
Now you can undergo such a test in many clinics and diagnostic centers, its average cost is about 2-3 thousand rubles, but prices can vary significantly depending on the equipment used.
Types of diagnostics
- A bicycle ergometer is not an ordinary exercise machine, but one equipped in such a way that it precisely doses the load. These devices have different types of braking systems, which affect the way this load is generated and adjusted. With a mechanical device, regulation occurs using a belt pressed against the surface of the wheel from the outside. On such a bicycle ergometer, you need to maintain the number of pedal revolutions at the same level (60 revolutions per minute). The electric braking system provides braking by moving a conductor (i.e., a metal strip on the outside of the wheel) in an electromagnetic field. The power of the load in this case will not depend on the speed of pedaling, so the patient can make only 30 revolutions per minute.
- The treadmill test is a normal walk on a treadmill. At first, walking is slow, but the task gradually becomes more difficult, since the angle of inclination and speed of the treadmill change every 3 minutes.
- EchoCG test . Echocardiography is performed before or after a treadmill test (veloergometry). This allows not only to accurately identify coronary artery disease, but also to identify viable areas of scars after a heart attack and evaluate the pumping function of the heart muscle.
- Routine test with ECG.
- Stress cardiopulmonary testing treadmill test and VEM with a gas analyzer . With this type of study, pulmonary activity is also recorded. It is used for different categories of patients, since the method is very accurate.
- Testing in combination with Doppler ultrasound of the vessels of the lower extremities. A set of these studies is aimed at assessing arterial insufficiency and ischemia.
Next, indications and contraindications for performing a treadmill test and bicycle ergometry will be discussed.
Complete the “bike” and get the result
You shouldn’t think that passing the VEM is so simple: get a direction and go. Before doing a stress test, the patient must understand that there are many conditions for this procedure to be performed. And even taking into account relative and absolute contraindications, the patient will not be able to undergo bicycle ergometry without preparation, therefore:
- A week before the study, he stops using cardiac glycosides, cordarone, and tricyclic antidepressants;
- Eliminates lithium salts in 3-4 days;
- 48 hours before – cancels beta blockers;
- 24 hours (or no less) the patient stops taking siuretics and antianginal drugs (medicines used for angina attacks), and although all nitrates are discontinued the day before the study, the patient can afford to take nitroglycerin, since he is allowed to stop an angina attack with this way.
It should be noted: if the study is carried out to determine the effect of antianginal drugs on exercise tolerance in patients suffering from angina pectoris, then the drugs of this pharmacological group are not canceled.
After the procedure is completed, the functional diagnostics doctor gives a conclusion on the results of the stress test:
- The result is negative (with submaximal load, all indicators remain within normal limits);
- The test is questionable (the occurrence of chest pain, ST depression on the cardiogram);
- The test is positive (description of ischemic transformations of the ST segment).
In other cases, the purpose of an increasing load test is to select certain chemotherapy drugs, then a bicycle ergometry or treadmill test should be done 1-2 hours after a person has taken the medicine, that is, at the supposed “peak” of its pharmacological action. How effective this drug will be can be judged by the increase in tolerance to physical stress after taking the drug in relation to the initial values of exercise tolerance.