Fluid in the lungs due to cancer is a serious and dangerous symptom that requires urgent medical attention. In case of cancer, fluid can accumulate in the human chest, both in the pleural cavity (pleurisy) and in the lung tissues (pulmonary edema).
The accumulation of water in the respiratory organs occurs gradually and reaches a very large amount. This interferes with the normal functioning of the lungs and contributes to an increase in respiratory failure. The presence of fluid in the respiratory system, if left untreated, can lead to dangerous consequences and even cause the patient’s premature death.
Pleurisy and pulmonary edema
Pulmonary edema - what is it? This is an extremely dangerous and difficult to treat condition, which is accompanied by cardiovascular failure and organ failure. The characteristic signs of this disease appear in advanced late stages of the disease, so treatment is most often ineffective. With the help of intensive therapy, the patient's condition is temporarily alleviated, but it is impossible to live with such a pathology for a long time.
Water in the pleural cavity is less dangerous than with pulmonary edema. Currently, there are effective methods to remove excess fluid in the edematous pleural cavity and stabilize the patient’s condition. A disease in which the pleural cavity is filled with fluid is called pleurisy.
The pleural cavity is the area between the two pleural layers. The outer layer covers the lungs from the outside and provides protection and tightness. The inner leaf lines the wall inside the chest cavity. In the normal state, between the layers of the pleura there is always a fluid of the required volume (about 10 ml of fluid), which ensures the movement of the lungs during breathing. Normally, the layer of fluid in the pleural cavity should be 2 mm thick. In cases where more fluid accumulates, congestion in the lungs and edema are observed.
Water in the lungs or in the pleural cavity can appear with cancer of the lungs, breast and pancreas, genitals, stomach, and intestines. This can happen at any stage of the disease. Water accumulates in the lungs when the body is severely weakened and cannot resist the disease. The accumulation of water in the pleural cavity is called pleural effusion.
Hydrothorax is the accumulation of fluid in the pleural cavity, which is not of inflammatory origin. The popular name for this disease is dropsy. Dropsy of the right or left lung is quite rare. The most common type is bilateral hydrothorax.
Signs of pulmonary edema
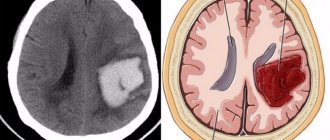
Pulmonary infarction is a disease caused by a thromboembolic process in the vascular system of the lungs and, in especially severe cases, leads to the instant death of the patient. Hemorrhagic consolidation of the pulmonary parenchyma is a consequence of pulmonary embolism. The main cause of the pathology is blood clots that form in the vessels of the lungs or are brought in from peripheral veins. Inflammatory and sclerotic changes in the pulmonary artery and its branches often result in the development of thrombosis.
The thrombus blocks the lumen of the vessel, ischemia of the lung tissue occurs, the pressure in the affected artery reaches a maximum, which leads to hemorrhage into the lung. Infection of the affected area ends with the development of pneumonia, suppuration, and abscess formation.
Pulmonary infarction often occurs in people with heart diseases: congenital and acquired defects, arrhythmia, coronary heart disease, cardiomyopathy. Cardiac blood clots usually form in the right atrium, break off and travel to the pulmonary arteries. Slow blood flow or stagnation in the pulmonary vessels also leads to thrombosis. The pathology develops quickly, and the affected area falls out of the functioning pattern.
When the first signs of illness appear, the patient must be urgently taken to the hospital. After an X-ray contrast examination of the chest and electrocardiography, he will be prescribed fibrinolytic agents and drugs that improve the rheological properties of blood, which will improve the trophism of the damaged area. When the patient's condition has stabilized, they move on to antibacterial and anti-inflammatory therapy.
Causes
Various diseases can provoke the development of a pulmonary infarction:
- Rheumatism,
- Tumors,
- Sepsis,
- Bone fractures,
- Hypercoagulation,
- Phlebothrombosis and thrombophlebitis,
- Polycythemia,
- Anemia,
- Burns,
- Cardiomyopathy,
- Infectious kidney pathology,
- Endocarditis.
Obstruction of the pulmonary arteries leads to pulmonary ischemia. In this case, the permeability of blood vessels is disrupted, and the ischemic area becomes overfilled with blood. Occlusion of the pulmonary vessels and reflex vasoconstriction lead to overload of the right chambers of the heart. Due to blood stagnation, hypertension occurs in the pulmonary circle.
The affected area acquires a rich red color, becomes dense and rises above the healthy lung tissue. The pleural layers become dull, and hemorrhagic exudate accumulates in the pleural cavity. The risk of developing pathology increases if patients have floating blood clots. Insufficient oxygenation and trophism of the lung tissue lead to its dystrophy, and subsequently to necrosis.
Factors contributing to the development of pathology:
- Long-term hormone therapy
- Early postpartum period,
- Splenectomy,
- Taking medications that increase blood clotting
- Chemotherapy,
- Damage to the vascular wall during venous puncture,
- Overweight,
- Prolonged immobilization.
Symptoms
The symptoms of pulmonary infarction depend on the area of damage to the lung tissue and the general condition of the body. If the size of the lesion is small, clinical signs may be absent, and the disease is detected only with the help of X-ray diagnostics. With an asymptomatic course, radiological changes disappear on their own after 7-10 days. A microinfarction of the lung is detected accidentally during the treatment of its infectious consequences.
- Signs of acute blockage of the pulmonary vessels are the main symptoms of the pathology. The disease is characterized by a sudden onset with the appearance of acute chest pain and inspiratory shortness of breath against a background of general well-being. Pain syndrome is a clinical manifestation of ischemia.
- The cough in patients is dry at first, then becomes wet, and bloody, foamy sputum of a dark brown color is released. Sputum with bloody streaks is a characteristic sign of the hemorrhagic form of the disease. The reason for its appearance is the rupture of a vessel clogged with thrombotic masses and saturation of the lung tissue with blood.
- Shortness of breath is accompanied by a vascular reaction: pale skin, sticky and cold sweat.
- Myocardial ischemia often accompanies pulmonary infarction. This is due to impaired coronary blood flow. Among other symptoms of the pathology are: frequent shallow breathing, thready pulse, chills, fever, pale or gray skin, acrocyanosis.
Patients develop hypotension, cerebral disorders, hepatomegaly, abdominal syndrome, asthma attacks, atrial fibrillation, panic attacks, leukocytosis in the blood, and an increase in ESR. The doctor, examining patients, discovers characteristic percussion, percussion and auscultation signs.
Complications
Pulmonary infarction is a serious disease that leads to dangerous consequences and threatens the patient’s life.
Complications:
- Post-infarction pneumonia develops 10-14 days after a lung infarction. Patients suffer from sore throat and discomfort. They develop a dry or wet cough with a small amount of sputum, and hemoptysis. Chest pain worsens with every breath. During microbiological examination of sputum, atypical pathogens of pneumonia are detected - mycoplasmas, chlamydia, fungi.
- Purulent pleurisy is the result of infection of the pleural cavity. Usually the disease is a complication of pneumonia, pulmonary infarction, or abscess. Patients develop fever, chills, tachycardia, shortness of breath, cyanosis, sweating, chest pain, and cough. The prognosis of purulent pleurisy is always serious. Mortality reaches 20%.
- Post-infarction abscess formation of lung tissue occurs in a relatively short time after pulmonary infarction. As a result of necrosis and infection of the lesion, a cavity is formed in the lung tissue. A lung abscess breaks into the pleural cavity with the development of pleural empyema. With a favorable course of the pathology, the lung tissue becomes scarred.
- Spontaneous pneumothorax develops when air from the alveoli enters the pleural cavity. Patients experience acute chest pain, shortness of breath, tachycardia, and fear of death. Patients take a forced position that brings them relief. The prognosis of the disease is favorable. Relapses are possible.
- Scars on the lung after a heart attack can have different sizes, on which the clinical picture of the pathology depends. With diffuse pneumosclerosis, when there are many scars on the lung, patients experience shortness of breath, weakness, difficulty breathing, and tingling in the chest. If the pathology is not treated, it will develop into cardiopulmonary failure.
- Pulmonary hemorrhage is characterized by the release of dark blood mixed with sputum, clots and food masses. Profuse bleeding can lead to death. When the first signs of bleeding appear, the patient must be immediately hospitalized in a hospital. Blood that constantly enters the respiratory tract should be coughed out. The most dangerous complication of pulmonary hemorrhage is asphyxia. In the hospital, the source of bleeding is determined and appropriate treatment is carried out.
- Rupture of an aortic aneurysm is manifested by severe burning and tearing pain in the chest, a sharp drop in blood pressure and other signs of cardiogenic shock. If patients do not seek medical help in time, they are unlikely to be helped.
- Lung gangrene is a destructive process in the lung tissue caused by exposure to putrefactive bacteria. An early sign of the disease is bad breath. Then patients experience hemoptysis, production of large amounts of sputum, fever, chills, and they suddenly lose weight. The disease is very difficult. If lung gangrene is not treated, sepsis develops and death is possible.
Diagnostics
Before starting treatment for a pulmonary infarction, a specialist must identify the disease that became its direct cause. Diagnosis of pulmonary infarction consists of conducting a thorough examination of the patient, instrumental and laboratory examination.
The radiograph shows a thin wedge-shaped shadow in the middle field, usually on the right. The ischemic area has the shape of a pyramid, the base of which faces the periphery, and the apex faces the root of the lung. The characteristic triangular opacification is located in the middle and basal segments of the lung. Additional diagnostic methods are ECG, CT, MRI.
Treatment
Pulmonary infarction is an emergency condition that requires emergency medical care in the intensive care unit of a hospital.
Treatment of pulmonary infarction is complex and long-term. The patient is prescribed several groups of drugs that dissolve blood clots and eliminate the symptoms of the pathology.
- Treatment begins by administering fibrinolytics to the patient. In the absence of severe arterial hypertension, the following fibrinolytic agents are used - “Streptokinase”, “Urokinase”, “Tissue plasminogen activator”. These medications are contraindicated for persons who suffered a stroke a month ago, as well as those suffering from hemorrhagic diathesis, and pregnant women. In severe cases, they switch from thrombolytic therapy to surgery - thrombectomy.
- Patients with pulmonary infarction are prescribed direct and indirect anticoagulants. Heparin is a drug that does not dissolve a blood clot, but prevents its growth and stops the process of thrombus formation. This medicine reduces spasm of the pulmonary capillaries, alveoli and bronchioles. Heparin therapy lasts ten days. Then they move on to treatment with Dicoumarin, Neodicoumarin, and Phenilin. Anticoagulants prevent further thrombus formation and prevent re-embolization.
- Antiplatelet therapy is carried out to prevent recurrent thrombosis. Patients are prescribed Aspirin, Thrombo ACC, Cardiomagnyl.
- Narcotic analgesics are used for acute pain. They relieve pain, improve blood circulation, and relieve shortness of breath. A 1% Morphine solution is administered intravenously. Non-narcotic analgesics are prescribed when pleural pain appears during breathing and coughing, or when body position changes. A 50% Analgin solution is administered intravenously.
- To relieve reflex vascular spasm, large doses of antispasmodics - Papaverine, Drotaverine - are administered intramuscularly.
- When pulmonary hemorrhage develops, calcium supplements are used.
- To treat shock, vasopressors are used - Dopamine, Dobutomin.
- "Eufillin" is administered intravenously slowly in the presence of bronchospasm.
- After stabilization of the patient's condition, they proceed to antibacterial therapy and standard symptomatic treatment. Antibiotics are prescribed to prevent pneumonia and suppuration. Typically, broad-spectrum drugs are used from the group of fluoroquinolones - Ciprofloxacin, macrolides - Azithromycin, cephalosporins - Ceftriaxone, penicillins - Amoxicillin.
- Intravenous injections of cardiac glycosides - “Strofanthin”, “Korglikon” - will help to ease the work of the heart.
- To improve the rheological properties of blood and accelerate regeneration processes in tissues, Trental, Cavinton, Actovegin are used.
- In case of severe hypertension, intravenous administration of Furosemide is prescribed. The drug ensures blood redistribution and a decrease in its volume in the lungs. Lasix is also used intravenously.
- For hypotension, Prednisolone, Strophanthin and Reopoliglucin are administered intravenously. In this case, all of the above therapeutic measures are prohibited. To combat collapse, Dopamine, Glucose or sodium chloride are administered intravenously.
- In case of pulmonary infarction, a vena cava filter is installed in the inferior vena cava, which will retain blood clots and prevent them from entering the systemic circulation.
Symptoms
Malignant pleurisy is characterized by systematic and slow development. In cases of cancer, the accumulation of water in the lungs occurs over many years. Therefore, in some cases, diagnosing pleurisy helps to detect a tumor and prevent the formation of metastases in the pleura. Read also : lung cancer symptoms and signs.
In the early stages, the accumulation of water does not appear in any way and is not felt by the patient. Most often, the disease is discovered accidentally during a clinical examination.
Over time, a lot of fluid collects in the edematous pleural cavity, and characteristic symptoms appear:
- heaviness in the chest, feeling of constriction;
- sensation as if a foreign object had entered the lung;
- aching and stabbing pain in the area of the diseased lung;
- shortness of breath even with little physical exertion, a “lump in the throat” is felt;
- hacking cough that does not go away for a long time;
- low-grade body temperature;
- secretion of thick sputum.
Pulmonary edema is an extremely dangerous condition, the symptoms of which develop very quickly, within a few hours. Why is liquid dangerous in this pathology? Manifestations of pulmonary edema can cause an attack of suffocation, which without timely help can even result in the death of the patient.
Typical signs of water accumulation depend on the amount of fluid in the respiratory organs and location.
There are several typical manifestations of the disease:
- increasing shortness of breath, first from physical activity, and then at rest;
- general weakness, decreased performance;
- cough with mucus and foam from the nose and mouth;
- a feeling of pain in the lower or lateral region of the sternum (pain increases with physical activity or coughing);
- breathing problems (gurgling sounds and wheezing are heard);
- dizziness, lightheadedness;
- bluish or pale skin;
- numbness of hands and feet;
- chills, constantly feeling “chill”;
- increased sweating, cold sticky sweat;
- tachycardia (rapid heartbeat);
- increased nervous excitability.
If such symptoms appear, it is necessary to begin treatment immediately, remove water from the respiratory tract if possible, and carry out procedures to restore breathing in order to avoid serious consequences.
Important! The appearance of copious pink, frothy sputum means that the patient needs urgent medical attention. If the patient is not helped in time, this can lead to death.
Causes
Pulmonary edema is not a separate disease; it is always a symptom of intoxication, disease, surgery or chest injury. Reasons for the development of this condition:
- Intoxication due to sepsis, inflammation of the lung tissue, uncontrolled use of medications or drugs.
- Diseases of the heart and its blood vessels: with overload of the pulmonary circulation (emphysema), with left ventricular failure (valvular defects, acute coronary insufficiency), embolism with a pulmonary thrombus.
- Reduced level of protein fractions in the blood (with cirrhotic liver damage, kidney disease with massive protein excretion in the urine - nephrotic syndrome).
- Excessive intravenous fluid therapy without subsequent forced diuresis.
- Chest injuries with damage to the integrity of the lungs and blood vessels.
- After heart surgery, including coronary artery bypass grafting (CABG).
- After surgical interventions on the lungs.
Coronary artery bypass grafting (CABG) is an operation performed by cardiologists to restore blood flow in the blood vessels of the heart. It is performed by installing special shunts (vascular grafts) and removing a blood clot or other agent that caused obstruction and hypoxia of the myocardial area.
A complication such as fluid in the lungs after surgery is expected, so prophylactic decongestant is prescribed along with the main therapy.
Most often, a pathognomonic condition such as pulmonary edema occurs 1–2 weeks after CABG surgery.
Diagnostics
If a patient develops similar symptoms, he should urgently go to a medical facility and be examined by an oncologist, who, if necessary, will refer him to other specialists: a pulmonologist, an ENT doctor, and others. All specialists collect a detailed medical history and conduct a thorough examination of the patient.
In order to determine an accurate diagnosis, a comprehensive examination is carried out. During an examination by a doctor, the lag of the diseased lung in the breathing process is determined. When palpating the chest, a shortened sound is taken into account when the lower part of the chest is tapped.
If there are signs of pleurisy, the doctor prescribes the following tests:
- chest x-ray;
- Ultrasound of the chest;
- CT scan – determines the cause of the disease;
- puncture from the pleural cavity - fluid is collected and sent for histological and cytological examination.
Causes and treatment of fluid in the heart
Postoperative pneumonia is the most common complication in surgery. Inflammation of the lungs in the postoperative period occurs in more than 60% of cases, and deaths are up to 15%.
The immediate cause of the development of pneumonia after surgery is infectious pathogens that enter directly into the respiratory tract. Typically, infections that occur after surgery are classified as atypical.
The most common causes of pneumonia after surgery:
- staphylococci;
- Escherichia;
- pseudomonas;
- Klebsiella;
- Proteus;
- enterobacter;
- candida.
Nosocomial or nosocomial pneumonia is difficult to treat due to the resistance of microorganisms to antibiotics. Therefore, it is much more economically profitable to prevent pneumonia than to start complex therapy later.
Provoking factors for the development of postoperative pneumonia are:
- congestion in the pulmonary circulation due to a long stay in a horizontal position;
- hypoventilation of the lungs;
- prolonged stay on artificial ventilation;
- therapeutic and diagnostic manipulations on the bronchi.
Newborns, premature babies due to underdevelopment of the respiratory system, and elderly people due to reduced immunity are more susceptible to developing complications after surgery.
Ventilation is sometimes the only way to save a life. Mechanical ventilation in the postoperative period can last from several hours to a month or more.
The composition of the air entering the lungs is carefully selected in terms of humidity and gas concentration, but the bronchial mucosa and epithelium still gradually begin to undergo pathological changes. Small villi cease to perform their protective function. Pathogenic and opportunistic microorganisms linger on the surface of the bronchi and trachea for a long time, begin to multiply and cause inflammation of the mucous membrane.
Carrying out bronchoscopy, as a prophylaxis or treatment, is mandatory for the rehabilitation of the lungs under certain conditions. But sometimes accidental damage to the inner surface of the bronchial tree occurs during manipulation. Defects in the mucosa contribute to the rapid development of bacteria and the penetration of infection further into the interstitium.
Small blood clots from the inferior vena cava system in the branch of the pulmonary artery are an additional provoking factor in the development of pneumonia. In severe sepsis, bacterial emboli enter the bloodstream directly into the pulmonary parenchyma. Postoperative lung injury complicates the pathological process. Damages to the central nervous system in the form of strokes and injuries contribute to a decrease in normal ventilation of the lungs and the development of infection.
With prolonged horizontal position after surgery, reflux of stomach contents into the trachea often occurs and aspiration postoperative pneumonia develops.
Especially after surgery on the chest and heart, the most favorable conditions are created for the development of inflammation. The reasons are as follows:
- lung injury;
- contamination from preoperative purulent foci;
- microembolism during artificial circulation;
- rigid fixation of the chest - hypoventilation.
A life-threatening condition occurs after removal of one lung, if a pathogenic postoperative process develops in the only healthy lung. Failure of the bronchial suture and reflux of blood into the stump can contribute to pneumonia.
Concomitant diseases of the bronchopulmonary system, such as tuberculosis, chronic bronchitis, atelectasis, and bronchiectasis, contribute to the severe course of the postoperative period.
After heart surgery, complications in the form of pneumonia most often occur after interventions for infective endocarditis. Postoperative mortality approaches 30%.
Factors contributing to the development of inflammation of the lung tissue after heart surgery are:
- The duration of the operation is more than 5 hours.
- Massive trauma to surrounding tissues.
- Artificial circulation.
- Hypoxia.
- Hypothermia.
Each reoperation, which is the only correct aggressive method of treating many diseases, increases the risk of developing infectious complications several times.
Pneumonia often occurs after abdominal surgery on the abdominal organs, retroperitoneal space, and pelvis. Prolonged anesthesia and massive blood loss, especially in cancer patients, provoke the occurrence of inflammation.
Anemia, dehydration, intestinal paresis - all of these can also serve as risk factors. Moreover, after abdominal surgery, early complications most often occur in the first week.
Considering the symptoms of the primary disease and the serious condition in the postoperative period, great difficulties arise in diagnosing pneumonia. An increase in body temperature, as the most common symptom of acute pneumonia, can be associated with many other processes - a postoperative wound, fluid accumulation in the resection area.
A sharp decrease in respiratory function and shortness of breath should always be alarming. But only radiological methods can unambiguously resolve the issue of diagnosis.
Changes that indicate the development of a pathological process in the lungs:
- local strengthening of the pulmonary-bronchial pattern;
- cloud-like infiltrates;
- diffuse enhancement of the bronchopulmonary pattern.
Isolation of the pathogen from sputum, throat swabs, and aspirate from the bronchi allows one to accurately establish the etiology and select the correct antibacterial treatment.
Therapy for the postoperative period almost always includes the prescription of antibiotics as a preventive measure for infectious complications. The addition of atypical flora, resistant to many drugs, complicates the treatment of nosocomial pneumonia.
In intensive care and intensive care settings, active sanitation of the bronchial tree, intravenous administration of anti-inflammatory drugs and massive infusions are carried out, helping to reduce general intoxication. If a massive pleural effusion is detected, puncture drainage is performed to aspirate the contents and straighten the lung tissue.
Depending on the underlying disease, prevention methods differ. After operations on the heart and chest, the use of antisecretory drugs to prevent aspiration and compression stockings to prevent thromboembolism can be recommended.
Common features are early activation of patients in the postoperative period and physical procedures, if there are no contraindications. The most accessible are two methods of self-prevention that help straighten the lung tissue:
- inflating balloons or balls;
- blowing air through a tube into a jar filled with water.
Simple manipulations can increase pressure in the bronchi and increase lung volume, which has a beneficial effect on restoring the functional state of the pulmonary parenchyma in the postoperative period.
In surgery and resuscitation, for emergency removal of fluid from the lungs, the following is used:
- Oxygen masks.
- Antifoam drugs, glucocorticoids, urea drugs (if there is no azotemia).
- Bronchodilators.
- Nitrates (to eliminate transient myocardial ischemia).
- It is possible to install controlled artificial ventilation.
- In the future, forced diuresis, sedatives and antihistamines are used.
For prevention, a restorative postoperative complex of physical therapy and physiotherapy is prescribed. It is aimed at increasing the vital volume of the lungs, improving blood circulation in the pulmonary and systemic circulation, and strengthening the muscular frame of the chest.
If pulmonary edema occurs at home after discharge, you should immediately contact your local physician and pulmonologist. A chest x-ray will be required.
If the diagnosis is confirmed, then you additionally need to undergo an ultrasound examination to determine the amount of effusion. Further management tactics are determined by the attending doctor depending on the severity of the complication, concomitant diseases, and the age of the patient.
In order to minimize the likelihood of complications, today a sufficient number of preventive measures are carried out, which consist of identifying risk groups and drug correction of existing pathology, as well as the use of modern technologies when performing coronary artery bypass surgery, as well as high-quality monitoring of the patient’s health status.
To consolidate the results of treatment, it is recommended to adhere to a diet with a minimum content of animal fats. At the same time, it is very important to exercise and give up bad habits. Regularly taking medications prescribed by your doctor will help improve your overall condition.
Taking antibiotics and antiviral drugs.
Antibiotic therapy, glucocorticoids.
Cirrhotic changes in the liver (hepatic hydrothorax).
Taking diuretics, liver transplantation.
Mechanical removal of exudate (pleurodesis, thoracentesis).
Taking diuretics and heart rate optimizers.
Removing fluid from the lungs artificially.
The infectious nature of exudate formation requires treatment with antibacterial agents. The choice of drug depends on the sensitivity of the pathogen to a specific group of antibiotics. For treatment, the penicillin group of drugs is traditionally used, which is represented by Amoxiclav and Sultasin:
- name: Amoxiclav;
- description: a combined systemic agent, the mechanism is based on the suppression of the enzymatic activity of microorganisms;
- pros: highly effective against most known bacteria;
- cons: cannot be taken if you have kidney dysfunction.
The semi-synthetic antibiotic Sultasin has few contraindications for use and rarely causes side effects:
- name: Sultasin;
- description: broad-spectrum antibiotic, has a high degree of penetration into body tissues and fluids;
- advantages: fast action;
- cons: interacts poorly with drugs from other groups.
Causes
Treatment
When the causes and symptoms of the disease are clarified, treatment begins directly. Surgical operations for pulmonary edema are ineffective; only drug therapy is used.
Various medications are used to treat this disease:
- cardiac glycosides – substances that stimulate myocardial contraction (strophanthin, corglycone);
- diuretics - diuretics that stimulate the removal of fluid from the body (furosemide, etc.);
- drugs that expand and tone the smooth muscles of the bronchi (aminophylline).
Using modern methods of therapy, it is possible to completely cure malignant pleurisy, thereby significantly increasing the patient’s life expectancy. For malignant pleurisy, treatment will be very different, since in this case drug treatment is ineffective.
A radical method of treatment is a surgical operation that pumps out fluid from the respiratory tract in case of oncology. For pleurisy, two types of surgery are used to remove water from the lungs: thoracentesis and pleurodesis.
Pleurocentesis is an operation in which exudate is removed mechanically (by puncturing). During the operation, a thin needle is used to puncture the lung to pump out water. Then another needle is used with an electric suction tube attached. Thus, excess fluid is pumped out, and the patient immediately feels relief. If the fluid after pumping out of the pleural cavity is yellow-brown and transparent, then there is no infection.
After such an operation, fluid in the lungs sometimes builds up again, since the main cause of the disease has not been eliminated. There are times when the liquid has to be pumped out several times. Repeated pumping of fluid is very difficult for the patient to tolerate.
In addition, after this procedure, the formation of adhesions is observed, which further complicate the course of the main disease. During or after surgery, mucus plugs may develop in the airways because the patient is unable to cough. Such plugs are removed using special suction.
Pleurodesis is a surgical intervention during which the pleural cavity is filled with special means that prevent the re-accumulation of fluid. Currently, this operation is widely used in medicine and allows to achieve maximum effectiveness of treatment and eliminate recurrence of the disease.
The following drugs are used during therapy:
- cytostatics (cisplatin, embiquin);
- immunomodulators (interleukin);
- antibiotics and antimicrobials (tetracycline);
- radioisotopes.
For oncological diseases sensitive to chemotherapy, cytostatic agents are used. In 65% of cases, this approach to therapy helps to get rid of exudative symptoms of pleurisy.
In some cases, the cause of the accumulation of water in the respiratory system is pneumonia. Then, to combat a dangerous infection, the patient is prescribed antibiotics. In addition, it is recommended to take antitussive and antiviral drugs.
Some folk remedies allow you to remove fluid from the respiratory tract right at home. But they should not be used without prior discussion with your doctor. Here are some of the plants used in folk medicine to remove water from the lungs: oats, parsley, onions, viburnum, anise, flax seeds, aloe.
Empyema drainage and decortication
Procedure – Surgical removal of pus (empyema) and organized thick fibrinous pleural deposits (decortication)
Time – Drainage 20-40 min. Decortication 2-3 hours
Pain – +++/++++++
Position – On the side, as for thoracotomy
Blood loss – Simple drainage – minimal. Decortication - 500-2000 ml, 3 units of erythromass must be combined
Practical recommendations - OA with careful IV induction, relaxants, intubation and mechanical ventilation. DPT is recommended for decortication (risk of air leakage); for drainage procedures, a single-lumen tube is sufficient; arterial and central venous catheter.
Before surgery
- Intrapleural infection is usually secondary to pneumonia, intercostal drainage, or thoracic surgery.
- Patients are usually weakened by chronic infection, and obvious sepsis may occur. The adequacy of antibiotic therapy received by the patient should be ensured.
- Respiratory function is often already impaired by pneumonia or previous lung resection.
- You should verify the presence or absence of a bronchopleural fistula, which sometimes forms as a result of lung erosion.
During surgery
- Empyema is usually drained with rib resection and placement of a large-diameter intercostal drainage.
- Thoracoscopy can be used to disrupt multilocular effusion collections or empyema and free pleural adhesions.
- Decortication requires standard thoracic anesthesia and epidural analgesia, as pleural changes often preclude the use of a paravertebral catheter.
- Decortication is often accompanied by significant blood loss, and air leakage is typical.
- Invasive monitoring of blood pressure and central venous pressure is recommended for all, even healthy patients.
After operation
- Balanced analgesia with regular administration of paracetamol, NSAIDs (attention to renal function), regional block (intercostal block is useful for drainage procedures) and additional opioids.
- After decortication, it is recommended to transfer the patient to the ICU.
Peculiarities
- From a surgical point of view, it is important to remove infected tissue, including pleural adhesions, completely expand the lung and obliterate the infected part of the pleural cavity.
- Decortication is a major intervention that requires careful consideration of the risk/benefit balance in elderly and frail patients.
- In selected cases, a lobectomy may be required if a massive air leak or severe damage to the lung parenchyma occurs during the decortication process.
Forecast
How long do patients with pleurisy or pulmonary edema live? According to statistics, timely treatment of pleurisy in half of all cases prolongs the patient’s life and improves its quality. If manifestations of the disease are detected at stage II or III of oncology, there is a possibility of successful treatment.
In cases where edema or pleurisy has developed at an advanced stage, treatment is usually difficult and brings only temporary relief to the patient. First, the fluid is pumped out, then procedures are carried out to make breathing easier during metastases.
With metastatic changes in the respiratory organs and regional lymph nodes, the prognosis is unfavorable - survival ranges from several months to a year. If a cancer patient has pulmonary edema and lacks medical care (timely pumping out of fluid), the patient may die within a few hours.
Approximate price for some services for detecting pulmonary edema in large medical centers:
- consultation with a pulmonologist – 10,000 rubles;
- X-ray – 5,000 rubles;
- examination of external respiration function – 3,000 rubles;
- MSCT of the chest – 10,000 rubles.
Physiotherapeutic procedures for pleurisy
Types of physiotherapeutic treatment depend on the type and stage of pleurisy.
Preference is given to:
- UV irradiation on the chest area,
- paraffin and mud applications on the back of the chest,
- electrophoresis with anti-inflammatory and absorbable drugs (iodine for dry pleurisy, and calcium for exudative),
- in the late rehabilitation period, climatotherapy is prescribed in the sanatoriums of the Crimea, coniferous forest. Their analogues are salt “caves” in local sanatoriums and dispensaries - a halochamber.
Preparing for surgery
The patient arrives at the hospital at noon or the evening before the operation, less often - in the morning on the day of the operation.
You need to take a blood test, x-ray, and ECG in advance.
Each hospital has its own method of familiarizing the patient with preparations for surgery. Typically, the surgical team (cardiac surgeon, anesthesiologist, cardiologist) meets with the patient and his family the evening before surgery or the morning of surgery to conduct a short examination and obtain information from the medical history. The patient may be shown a video about the operation and post-operative care for cardiac patients.
Relatives should find out where they can be during the operation and when they can expect to hear first about the progress of the operation. The patient and his relatives will be told about the means of special observation (monitoring) in the intensive care ward, where he will remain for the first few days after the operation.
The doctor will explain what medications you can take before surgery. Anti-angina medications are allowed as usual. After 24 hours on the eve of surgery, the patient should not eat or drink anything, because anesthesia is safer to do on an empty stomach.
Final preparations include shaving the body hair from neck to ankles (hair can absorb bacteria) and washing with a special cleaning soap.
Before surgery, sedatives are administered to relieve anxiety. In the preoperative room, a catheter is installed: small and flexible, it is inserted along the needle and left in the vein, and the needle is removed. Anesthetics and other medications are administered through this catheter. The patient is now completely ready for surgery.
Pumping fluid from the lungs: indications, consequences, how it goes
According to statistics, the trend towards an increase in respiratory diseases is growing every year. In Russia alone, today about 5 million people suffer from pathologies of the bronchopulmonary system.
Among the diseases, chronic bronchitis, pneumonia, asthma, pleurisy, COPD (chronic obstructive pulmonary disease) predominate. Next comes tuberculosis. The incidence of lung cancer, which leads among all other oncologies, is growing.
The main contingent of patients are experienced smokers and residents of large industrial centers.
What is fluid in the lungs
Gas exchange in human blood occurs in the alveoli. These are the many vesicular components of the lungs. Oxygen is captured from the incoming air and carbon dioxide is released. This is a basic physiological process that provides the body with oxygen.
When air exchange in tissues is disrupted, capillary permeability increases or the integrity of blood vessels is compromised in general. Liquid begins to seep through their walls, which can fill the alveoli. It often accumulates not in the lung itself, but in the pleural cavity, between the pleural layers.
To ensure normal lung excursion, a healthy person always has about 2 ml of serous fluid in the pleural area. If its volume exceeds 10 ml, removal is required.
One of the reasons is a malfunction in the lymph system, which causes swelling. Fluid accumulation most often occurs when:
- heart diseases - arrhythmias, heart defects, heart attacks, heart failure;
- liver diseases - liver failure or cirrhosis;
- diabetes mellitus;
- renal failure;
- inflammation in the lungs - pneumonia, tuberculosis, pleurisy;
- lung cancer;
- COPD;
- pulmonary edema;
- head and chest injuries (pneumothorax).
Fluid in the elderly
In addition to the above pathologies, in old age, fluid in the lungs is possible after long-term use of aspirin, which is used as an analgesic. Physical inactivity may also be a cause, since old people move little for various reasons. In this case, pulmonary circulation is disrupted.
Liquid composition
The composition will be different for different pathologies. Accumulation of serous fluid, sometimes mixed with blood, occurs in lung oncology, when malignant pleurisy develops. Purulent exudate is observed during an acute inflammatory process in the lungs.
Any composition of the liquid is not the norm, and measures must be urgent. Water in the pleura is not as dangerous as swelling.
During sleep, attacks of shortness of breath appear, which indicates respiratory failure, and the skin becomes cyanotic. A wet cough with pink foam is observed, later attacks of suffocation appear during the day. This indicates pulmonary edema. Such symptoms require fluid to be pumped out of the lungs.
Thoracentesis
When and how is fluid pumped out of the lungs? Usually transudate, which is caused by a non-infectious nature, is removed. If the pathology is associated with inflammation and there is an admixture of pus in it, then this is exudate.
In such cases, the inflammation should be treated before the procedure. If liquid remains after this, it is removed. It should be borne in mind that pumping occurs from the pleural cavity; it is impossible to do this by suction. In these cases (pulmonary edema, for example), treatment is medicinal.
What is pumping fluid from the lungs called? Thoracentesis or thoracentesis. During these procedures, fluid is mechanically removed. Pain relief is performed with local anesthesia. No special preparation of the patient is required.
Usually, the doctor tries to stabilize the state of the cardiovascular and respiratory systems with the help of symptomatic therapy before centesis.
The patient is in a sitting position, slightly leaning forward, placing his hands on a special table or placing them behind his head.
How is the procedure for pumping fluid out of the lungs? First, using ultrasound or x-ray, the location of the accumulation of exudate is determined, then a local anesthetic is administered and an injection of novocaine is given.
The skin is wiped with alcohol, and the doctor carefully pierces the pleural cavity in the area under the scapula (in the middle between the mid- and posterior axillary lines) strictly along the upper edge of the rib between the 6th and 7th intercostal spaces with a thin injection needle. In this way, tissue infiltration is carried out with novocaine or lidocaine. Actions must be extremely careful, because there is a possibility of damaging the neurovascular bundle.
The depth must also be precise, so periodically the syringe plunger is pulled back to check. If the needle is inserted too deeply, the lung parenchyma may be damaged. The needle is inserted until a sensation of failure is felt - at this point the depth of penetration is measured. The upper lining of the lung (pleura) is denser than its contents.
Next, the anesthesia needle is removed, and a thick thoracentesis needle is inserted (to the measured depth). Through an adapter, the needle is connected to the electric suction pipe.
Part of the effusion goes to the laboratory for analysis, the adapter is switched to suction and the effusion is evacuated. A device for pumping fluid from the lungs is an electric suction device or a drainage-suction device.
In the absence of an electric suction, a Janet syringe is used.
https://www.youtube.com/watch?v=GgR44IINHv0
The fluid is pumped out (aspiration of fluid from the pleura), catheters are inserted, through which exudate is released for some time. Pumping out fluid from the lungs does not take much time - about 15 minutes. After this, the catheters are removed and the puncture site is again lubricated with alcohol. A sterile dressing is applied. Sometimes catheters are left in place if necessary. A control x-ray is performed.
The procedure for pumping out fluid must be performed exclusively under sterile conditions. Therefore, pumping fluid from the lungs at home is not carried out. Depending on the purpose, aspiration can be therapeutic or diagnostic.
You can pump out no more than 1 liter of liquid at a time. If the volume is exceeded, complications arise and even death is possible. With a gradual decrease in the fluid level during the process of pumping it out, the patient becomes clearly relieved.
After pumping out fluid from the lungs, it can collect again, since the main cause of the disease itself is not eliminated during the procedure, and there are no guarantees for complete primary removal. For etiotropic treatment, other methods are used. Repeated thoracentesis is very difficult for patients to tolerate, because there are already adhesions that complicate the operation.
Weakening of the immune system always contributes to the re-accumulation of fluid. Patients over 60 years of age are at risk. Normalizing fluid levels in the lungs often requires treatment of other organs, judging by the list of diseases.
Artificial removal of exudate from the lungs by puncturing them is another name for pumping out fluid from the lungs. The most radical method is bypass surgery.
When a shunt is installed, it transfers the accumulated fluid from the pleural cavity to the abdominal cavity.
In case of non-surgical pathology, proper treatment of the underlying disease allows the amount of fluid to normalize on its own - this option is not excluded. But this does not apply to severe pathologies. Thus, the consequences of pumping fluid from the lungs are a short-term improvement in the patient’s well-being. To influence the cause of the pathology, pleurodesis is used.
How many times can fluid be pumped out of the lungs?
The number of repetitions of the procedure is determined by the doctor. Sometimes the procedure is carried out every other day. It is important to identify the cause of fluid accumulation and eliminate it.
Pleurodesis
Quite a popular procedure in pulmonology. Pleurodesis is also a surgical operation, but with a reverse algorithm: the pleural cavity is filled with special therapeutic agents to prevent the re-formation of fluid.
A variety of drugs are used for this: sclerosing drugs (Embiquin or Cisplatin), immunomodulators (Interleukin), antimicrobial drugs (Tetracycline) and anti-tuberculosis drugs. This treatment is quite effective because it acts directly at the site of the pathology. In other words, pleurodesis is the treatment after pumping out fluid from the lungs.
Recovery forecasts
The chances of recovery depend on the etiology of the disease. A negative prognosis exists only for cancer. In this case, it does not matter at what stage the accumulated fluid in the lungs is detected. For other pathologies, if treatment is started on time, the prognosis is favorable, the functioning of the pulmonary system is completely restored.
Self-therapy with traditional methods is excluded - not a single patient has yet been cured using this method. Precious time is lost, and the consequences are dire. A person may die due to respiratory failure.
Consequences of fluid accumulation
If the volume of fluid accumulation is insignificant, no significant harm is caused to the body, especially if you consult a doctor in a timely manner.
But in chronic pulmonary pathologies, the elastic tissue of the lungs is replaced with fibrous tissue, which worsens the already impaired gas exchange and leads to severe oxygen starvation.
With a lack of oxygen, the brain and central nervous system suffer. The outcome is often fatal.
Fluid in the lungs with cancer
Oncology is becoming the most dangerous cause of exudate accumulation in the lungs. Pumping out fluid from the lungs in case of cancer is practiced in the initial stages.
In cancer patients with lung cancer, accumulation, unfortunately, indicates critical depletion of the body and is observed already in the last stages of the disease.
Edema often occurs against the background of a decrease in protein levels - a necessary consequence of cancer progression. In this case, you should not expect a good result from treatment.
Source: https://FB.ru/article/458748/otkachivanie-jidkosti-iz-legkih-pokazaniya-posledstviya-kak-prohodit