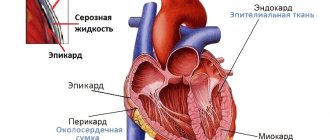
The heart of each of us is located in a special dense closed sac - the pericardium, or pericardial sac. It consists of two leaves, between which there is a slit-like cavity (it is called the pericardial cavity). The cells of one of the leaves produce serous fluid, a small amount of which - up to 25-50 ml - is always present in the pericardial cavity.
The pericardium performs a protective function - it fences off the heart from nearby organs, does not allow it to move or overstretch during increased physical stress on the body or sudden human movements. Pericardial fluid prevents friction of the pericardial layers and facilitates their sliding relative to each other.
You will learn about why it occurs, what symptoms it is accompanied by, as well as the principles of diagnosis and treatment tactics for hydropericardium in our article.
Causes and mechanism of development
In a healthy person, non-inflammatory fluid (transudate) is produced and reabsorbed by the cells of the pericardial sac. The volume of this fluid in the pericardial cavity is relatively constant, that is, the processes of its production and absorption are balanced. In a number of diseases, this balance is disturbed: either a lot of transudate is produced, or it is reabsorbed much more slowly than necessary. There is only one result: an increased amount of non-inflammatory fluid in the pericardial cavity. How elevated it is depends on the severity of the underlying disease - sometimes the volume of transudate is only slightly higher than normal values (50 ml), and sometimes reaches 1000 ml.
Hydropericardium is not an independent disease, but a syndrome that accompanies and complicates the course of a number of other pathologies, often being a sign of their decompensation.
The following diseases can lead to the development of hydropericardium:
- congenital heart defects;
- cardiomyopathies of various nature;
- pericarditis;
- any other heart diseases that are accompanied by chronic heart failure syndrome;
- diseases accompanied by hypoproteinemia (decreased protein levels in the blood);
- chronic renal failure;
- pathologies of the thyroid gland, accompanied by a decrease in its function - hypothyroidism;
- some types of anemia;
- diseases of an allergic nature;
- neoplasms of the mediastinal and cardiac organs (myxedema);
- injuries to the chest and heart organs in particular;
- exhaustion of the body, including anorexia.
Also, this condition can become one of the complications of radiation therapy that a patient receives for the treatment of a particular cancer disease, and can also arise as a result of taking a large number of vasodilators.
Clinical picture
Since most diseases leading to the development of hydropericardium are characterized by a chronic course, its symptoms develop and increase gradually as the main pathological process progresses. Initially, only its symptoms are visible, and a slight increase in the volume of pericardial fluid does not manifest itself in any way. As the amount of transudate in the cavity of the pericardial sac increases, the heart is gradually compressed by it, its movements are limited, contractions become more and more difficult, which is felt by the patient and becomes noticeable to the doctor.
The leading clinical manifestations of this condition are as follows:
- shortness of breath - first with exertion, and then at rest;
- discomfort, heaviness in the heart area, especially when bending forward;
- feeling of heartbeat;
- increased heart rate;
- edema - first peripheral (starting from the lower extremities), then spreading higher and higher until anasarca - edema of the whole body;
- decreased blood pressure;
- general weakness, increasing over time.
If the volume of fluid in the pericardial cavity increases significantly in a short period of time (for example, due to injury), the person suddenly feels worse. This critical condition in cardiology is called cardiac tamponade. It requires emergency medical care to be provided to the patient, otherwise he may die.
Symptoms of cardiac tamponade are as follows:
- severe hypotension (low blood pressure) up to collapse with loss of consciousness;
- severe general weakness; the patient says that his vision is getting dark;
- dizziness;
- palpitations, increased heart rate;
- feeling of heaviness in the chest;
- chest pain;
- patient's agitation, fear of death;
- frequent shallow breathing, feeling that there is not enough air.
Symptoms and diagnosis of pericarditis
In the early stages of the development of this disease, the presence of fluid in the pericardium can be noticed by the corresponding symptoms. It is easiest to treat pericarditis at this stage, but in advanced cases, the process may be irreversible.
The acute form of pericarditis is considered the most amenable to drug treatment. Heart ultrasound and ECG help doctors identify it. It occurs against the background of acute inflammation in the body. Sometimes they occur after surgery or heart injury.
Symptoms of acute pericarditis:
- prolonged pain in the chest (more than two hours), intensifies with deep inspiration, sneezing and even swallowing,
- increase in body temperature,
- nausea, vomiting,
- excessive sweating,
- dyspnea.
The doctor determines this disease by pericardial noise. When two layers of shell rub against each other, a sound appears that is similar to the crunching of snow. If the amount of fluid increases quickly, it can strongly compress the heart, which is why it is unable to expand at the time of diastole, therefore, blood almost stops flowing into the cavity. This condition is called tamponade, and often ends in the death of the patient.
Exudative pericarditis is considered one of the most severe forms of the disease, precisely because of the large volume of fluid between the layers of the pericardium.
Symptoms of exudative pericarditis:
- weakness, loss of strength,
- constant shortness of breath, even during rest periods,
- weight loss,
- liver enlargement,
- swelling,
- hypotension,
- abdominal enlargement,
- tachycardia,
- heavy sweating.
Biochemical tests, MRI, electrocardiography and ultrasound of the heart help diagnose this type of pericarditis.
Cardiac tamponade can be considered the most difficult stage in the development of this disease, since fluid can often only be removed surgically or by puncture. In some cases, the fluid accumulates over a long period of time, while in others it accumulates in a matter of hours. At this stage, a person experiences a constant change in blood pressure, increasing tachycardia and severe shortness of breath. Blood pressure can drop to the point of collapse. Only surgical intervention can save a person in this condition.
Chronic pericarditis develops slowly, so a person may not even notice pain in the heart area. This form develops due to incompletely cured acute inflammation.
Diagnostic principles
- the patient’s appearance (pallor of the skin, cyanosis of the nasolabial triangle (blue tint of the skin between the nose and upper lip);
- sticky cold sweat (with cardiac tamponade);
- when auscultating (listening to) heart sounds, they are significantly muffled, heart rate is increased (tachycardia);
- when percussing (tapping) the borders of the heart, they are expanded.
Additional research methods will help clarify the diagnosis. The most informative are:
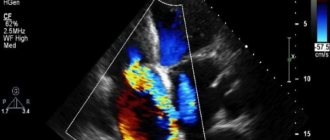
- Echocardiography, or ultrasound of the heart. During the diagnostic process, a divergence of the pericardial layers will be detected, an enlargement of the pericardial cavity - normally it is no wider than 5 mm, and due to the accumulation of fluid in it, it increases from 6 to 20 mm or more.
Ultrasound also allows you to quantify the volume of transudate. Using an ultrasound examination, it is possible to diagnose hydropericardium in the fetus, which will signal the doctor about a possible congenital heart defect and a reason for a complete examination of the pregnant woman.
To find out the nature of the hydropericardium, the patient is prescribed other additional diagnostic methods:
Principles of treatment
The approach to the treatment of hydropericardium is strictly individual and depends on many factors: the underlying disease, the amount of fluid in the pericardial cavity, the general condition of the patient, and so on.
If the volume of transudate in the pericardial cavity is only slightly higher than normal values, the doctor focuses on treating the disease that led to the development of this condition:
- for heart disease, prescribes cardiac glycosides, ACE inhibitors, cardioprotectors and other drugs depending on the disease;
- for heart defects, surgical correction is possible;
- for hypothyroidism - L-thyroxine;
- for anemia - iron supplements and so on.
As the patient's condition improves and stabilizes, the amount of transudate in the pericardial cavity also gradually decreases and returns to normal.
In the case of massive hydropericardium, a more targeted effect on the transudate is necessary, reducing its volume - this will alleviate the patient’s condition and allow his heart to work more efficiently. For this purpose, diuretics can be prescribed (preferably potassium-sparing (spironolactone) or thiazide (hydrochlorothiazide) diuretics in combination with potassium supplements), and in more severe cases, removal of excess fluid from the pericardium by puncturing its cavity - pericardiocentesis.
Types of pericarditis
In most cases, pericarditis develops against the background of another disease. This diagnosis can be called concomitant with the main one.
The reasons for the accumulation of excess fluid in the heart are different, depending on them the following classification has been developed:
- Infectious pericarditis. It is provoked by parasites, bacteria, fungi, and viruses.
- Consequences of systemic autoimmune diseases. Develops with dermatomyositis, systemic lupus erythematosus, scleroderma, rheumatoid arthritis.
- In case of failures in metabolic processes. Accompanies gout, diabetes, myxedema, Addison's disease.
- One of the complications of diseases of neighboring organs. Here the reasons are as follows: lung disease, aortic aneurysm, transmural myocardial infarction.
- Neoplastic appearance. It is provoked by metastases or tumors of the pericardium.
- Traumatic. Occurs as a result of a penetrating wound to the chest.
- Idiopathic pericarditis. The reasons are unknown to science.
Fluid in the pericardial cavity can behave differently. There are three types of pericarditis:
- Dry. A decrease in the amount of fluid in the lining of the heart or its stagnation.
- Fibrinous. A slight addition of liquid with a simultaneous increase in the concentration of protein in it.
- Exudative. Accumulation of a large amount of serous fluid in the cavity between the layers of the pericardium.
According to the stages and duration of the disease, it can be divided into two forms:
- Spicy. The disease develops no longer than two months.
- Chronic. The illness drags on for six months.
Without proper treatment of inflammation, proteins and calcifications will begin to accumulate between the layers of the pericardium. In this case, negative consequences are guaranteed: the cardiac membrane will simply stick together, since the protective and lubricating functions will no longer be performed. This means that the pericardium will become a limiter for the heart muscle during its contractions, thus heart failure will develop at a rapid rate. To eliminate it, you will have to resort to heart surgery.
Pericarditis and pericardial effusion
Pericarditis ( inflammation of the pericardium ) can occur with a variety of diseases, including viral or bacterial infection, metastatic tumors, connective tissue diseases, myocardial infarction, uremia, and heart surgery.
Rice. 11-1. Acute pericarditis with widespread ST segment elevation in leads I, II, aVF, V2-V6 with reciprocal ST segment depression in lead aVR.
Damage to the atrial myocardium is indicated by elevation of the PR segment in lead aVR with reciprocal depression of the PR segment in the left precordial leads and lead II. (From: Goldberger A.
L Myocardial infarction: Electrocardiographic Differential Diagnosis. – 4th ed. – St. Louis: Mosby, 1991.)
Differences between pericarditis and the acute stage of myocardial infarction
The electrocardiogram with pericarditis resembles the acute stage of myocardial infarction. In the early stages of acute pericarditis, ST segment elevation usually occurs (Fig. 11-1) as a consequence of inflammation of the superficial part of the heart, which is not uncommon in pericarditis.
The main difference between ST segment elevation in pericarditis and acute myocardial infarction is their location . ST segment elevation in acute myocardial infarction usually occurs in the anterior or inferior leads due to the limited area of myocardial infarction.
The pericardium covers the entire heart, so changes in the ST-T complex in pericarditis are usually more widespread (in the anterior and inferior leads): for example, ST segment elevation in leads I, II, aVL, aVF, V2-V6 in Fig. 11-1.
| In Fig. Figure 11-1 shows small but diagnostically important changes in repolarization in acute pericarditis. |
In acute pericarditis, not only ventricular repolarization (ST segment) is impaired, but also atrial repolarization. The latter corresponds to the PR segment (from the end of the P wave to the beginning of the QRS complex).
Inflammation of the pericardium often produces electrical flow through the atrium, typical of injury, as evidenced by elevation of the PR segment in lead aVR, as well as depression in the other limb leads and left precordial leads (V5 and V6).
Thus, in acute pericarditis, the PR and ST segments are usually deviated in opposite directions (the elevation of the PR segment is often no more than 1 mm in lead VR and slight depression of the ST segment in the same lead). In other leads, depression of the PR segment and elevation of the ST segment are possible.
After ST segment elevation in acute pericarditis, negative T waves are sometimes formed (Fig. 11-2).
Rice. 11-2. Subacute stage of pericarditis. Widespread T wave inversion in leads I, II, III, aVL, aVF, V2-V6.
The sequence of ST segment elevation and T wave inversion is the same as in myocardial infarction. Sometimes negative T waves caused by pericarditis completely disappear over time and the electrocardiogram returns to normal. Long-term persistence of T-wave inversion is also possible.
The ECG changes in acute pericarditis and acute myocardial infarction are very similar , as ST segment elevation with T wave inversion may occur in both cases. However, ST-T changes in pericarditis are usually more widespread compared with the limited changes in myocardial infarction.
Another important difference is the absence of pathological Q waves in pericarditis.
In myocardial infarction, pathological Q waves are the result of myocardial death and, accordingly, the disappearance of positive depolarization potentials (see section “Ischemia and myocardial infarction”).
Pericarditis usually involves only superficial inflammation and not myocardial necrosis. Thus, pathological Q waves never occur in isolated pericarditis .
Pericardial effusion
Pericardial effusion is the accumulation of fluid in the pericardial cavity. In most cases, this occurs with pericarditis.
However, sometimes pericardial effusion is possible in the absence of pericarditis , such as with myxedema ( hypothyroidism ) or cardiac rupture.
The main clinical significance of pericardial effusion is the risk of cardiac tamponade, when fluid “suffocates” the heart, which can lead to a decrease in blood pressure and even cardiac arrest.
The most common ECG finding of pericardial effusion (with or without tamponade) is low QRS voltage, which is likely due to disruption of the conduction of electrical impulses in the heart due to the fluid surrounding it.
The section “Enlargement of the atria and ventricles” describes the voltage criteria for myocardial hypertrophy. Low voltage is indicated when the amplitude of the QRS complexes in each of the six limb leads does not exceed 5 mm (0.5 mV).
With low voltage in the limb leads, low voltage in the chest leads is possible - the amplitude of the QRS complex is no more than 10 mm in each of the leads V1-V6.
For example, in obesity, low QRS voltage is possible due to fatty tissue lying between the heart and the chest wall. In patients with emphysema, the airiness of the lungs is increased, which contributes to the isolation of the heart.
The most common causes of low electrocardiogram voltage are obesity, anasarca (generalized edema) and pulmonary emphysema.
If low voltage QRS complexes are detected (especially against the background of sinus tachycardia), the presence of pericardial effusion should be suspected, as this can cause cardiac tamponade.
Electrical alternans is another important sign of pericardial effusion and cardiac tamponade (Fig. 11-3).
Rice. 11-3. Electrical alternans in cardiac tamponade. Alternation of the axis of the P-QRS-T complex during successive contractions of the heart, which is associated with its oscillatory movements in the pericardial fluid; relatively low voltage QRS complexes and sinus tachycardia.
In this case, a typical shift in the average electrical axis of the QRS complex from one heart contraction to another is associated with a change in the position of the heart in a large volume of fluid. Electrical alternans in combination with sinus tachycardia is one of the diagnostic signs of cardiac tamponade . However, this sign is not detected in every patient.
| So, in acute pericarditis, the electrocardiogram shows signs of widespread damage with ST segment elevation in the anterior and inferior leads, sometimes with T wave inversion in these leads. However, pathological Q waves do not occur in isolated pericarditis. Pericardial effusion is one of the causes of low wave voltage on the electrocardiogram. |
Source: https://cardiography.ru/izmeneniya_ekg_pri_zabolevaniyah/perikardit_i_perikardialnyiy_vyipot/
Symptoms of the disease
Inflammation of the lining of the heart often has an accompanying nature, so its appearance is easy to miss. How severe the symptoms are depends on the severity of the underlying disease, the filling of the pericardium with fluid, and the rate at which it remains. The manifestations of pericarditis are mostly similar in all cases. The patient usually describes the following picture during his complaints:
- weakness;
- fever;
- pain in the chest area;
- pericardial friction sounds;
- muscle pain;
- shortness of breath;
- headache;
- abnormal heartbeat rhythm;
- dry cough.
If the disease is non-infectious, these signs may be mild or absent altogether. In most cases, a person does not attach importance to these symptoms or incorrectly diagnoses the cause of the problem. Symptomatic measures can also simply be taken: syrup for cough, antipyretic for fever, analgesic for pain, etc. The disease often becomes advanced, and only then does the patient see a doctor.
The abundance of fluid expands the membrane, thereby squeezing the heart. This reason is enough to cause cough, shortness of breath and chest pain. Pain in the left side of the chest often radiates to the shoulder blade, arm or neck. Physical activity only worsens the pain.
When the pericardium rapidly fills with fluid, cardiac tamponade occurs. The heart, compressed by the membrane, cannot contract. Pain in the chest becomes very strong, shortness of breath appears in a calm state, a feeling of lack of air, and anxiety. The person is unable to adopt a suitable position for his body to relieve suffering. This requires emergency medical attention as cardiac arrest is possible.
Diagnosis and treatment of pericarditis
When examining a patient, the cardiologist clearly hears the sound of the membrane rubbing against the heart muscle; this sign may be absent in the early stages of the disease. To clarify the diagnosis, an examination is prescribed, the program of which includes the following procedures:
- electrocardiogram;
- echocardiogram;
- chest x-ray.
Also, such a patient is shown a clinical blood test that determines the degree of inflammation. An external examination mainly evaluates the condition of the neck veins and swelling of the legs. During the examination, the specialist detects changes in the heart muscle and pericardium, as well as disturbances in the functioning of the cardiovascular system that accompany this disease. X-rays can be used to observe changes in the shape and size of the heart.
The cardiac imager will be a very useful and effective tool in the diagnosis and monitoring of pericarditis. This device detects even the smallest changes in the myocardium. Thus, subsequent treatment will proceed without any particular difficulties.
Each technique aimed at ridding a patient of a disease directly depends on the stage of development of the disease. The acute form requires immediate hospitalization, this will prevent the onset of tamponade. Urgent surgery will eliminate the risk to life, saving the patient.
As for treatment, in addition to surgical intervention in the most emergency cases, conservative treatment is advisable. Medicines are selected in accordance with the individual characteristics of the body, the presence of adverse reactions, allergies, and advanced pericarditis. The most popular medications for this type of disease are:
During surgery, the pericardial cavity is opened to remove excess fluid. In the presence of adhesive formations, laser intervention is widely used and is a fairly effective method. And if for some reason it is still impossible to achieve an effect, then it is better to prefer cardinal methods to all the methods described: pericardiectomy, removal of the cardiac membrane. After the operation, the patient is shown complete rest in a quiet environment: the heart must get used to working without a lubricating bag.
Causes and treatment of exudative pericarditis: what to do with fluid in the heart
Exudative, or effusion, pericarditis is a disease in which an excessive amount of fluid is released into the cavity between the two layers of the outer inflamed lining of the heart.
Normally, its volume should not exceed 20–30 ml, but with this pathology it increases tens of times. Rapid filling of the cavity leads to compression of the myocardium (tamponade) and requires emergency care.
Slow accumulation ends in congestion and circulatory failure.
A small amount of lubricant between the visceral and parietal layers of the outer shell of the heart plays a protective role and glides during contraction of the organ.
Pericardial effusion develops with inflammation and increased vascular permeability.
In this state, the serous leaves do not absorb excess fluid; in addition, it sweats from the blood, and the level of secretion increases.
Exudative pericarditis most often occurs as a secondary process, as a complication of the underlying pathology. The reasons for its development may be:
- severe infections;
- autoimmune disorders;
- allergic reactions;
- injuries (impacts, penetrating wounds);
- radioactive exposure;
- blood diseases;
- tumors;
- myocardial infarction;
- metabolic disorders;
- surgical intervention on the heart (at the same time, exudative pleurisy may occur after surgery);
- renal failure.
If fluid in the serous membranes appears for an unknown reason, then the disease is considered idiopathic.
Signs of fluid in the pericardium
When effusion begins to accumulate, it compresses the heart muscle and upper respiratory tract. Common symptoms of pericardial effusion:
- chest pain;
- uncontrollable hiccups;
- fear of death;
- persistent cough;
- hoarseness of voice;
- lack of air;
- attacks of suffocation in a horizontal position;
- periodic fainting.
Nature of pain
Chest discomfort may resemble angina, heart attack, and respiratory inflammation.
The pain has the following characteristics:
- worse when swallowing, moving the body, inhaling, lying down;
- relieved in a sitting position by bending forward;
- most often begin suddenly, but can have an increasing character;
- last from several hours to a day or more;
- vary in intensity (the symptom depends not only on the severity of the pathology, but also on the patient’s pain threshold, as well as the state of his nervous system);
- can be dull, sharp, pressing and burning;
- localized in the projection area of the pericardium or radiate to the left shoulder, arm, neck.
What does a patient with exudative pericarditis look like?
Patients experience the following signs of exudative pericarditis:
- pale skin, acrocyanosis;
- swelling of the upper body and swelling of the neck veins that do not collapse when inhaling;
- the cardiac impulse upon palpation is sharply weakened or not detected;
- increased heart rate and arrhythmia;
- weakening of the pulse on inspiration;
- weakening of heart sounds during auscultation;
- liver enlargement;
- rapid increase in fluid in the peritoneal cavity (ascites);
How to diagnose the disease
To confirm the diagnosis, the following research methods are performed:
- The most informative and accessible method in this case is an ultrasound of the heart. EchoCG reveals the accumulation of excess fluid, atony of the intercostal muscles in the affected area and tissue swelling. Adhesions and thickening of the serosa may also be noticeable.
- The cardiogram shows a significant decrease in voltage, and sometimes you can see a disruption in the functioning of the conduction system.
- Computed tomography helps to clarify the degree of advanced disease, the condition of the lungs and mediastinal organs.
- On MRI of the heart, you can see the earliest signs of pericarditis, pinpoint lesions, adhesions and effusion, even if it is insignificant.
- The fluid in the heart sac is evacuated by puncture. The procedure allows you to clarify the composition of the effusion - it can be serous, hemorrhagic, purulent, or cholesterol.
Features of exudative pericarditis in children
In childhood, the disease is extremely rare, but is very severe. Fluid in a child's heart is formed as a result of infection. This is usually caused by the Epstein-Barr or influenza viruses. In an adult, there are many more reasons, but many of them are revealed only after puncture of the cardiac sac.
Exudative pleurisy in a child is accompanied by high fever, heart pain and increased blood pressure. The protocol for providing assistance does not depend on the age category of the person; treatment is carried out by prescribing medications, puncture with pumping out the contents, or performing surgery.
Treatment algorithms
In the acute stage of the disease, hospital treatment and bed rest are required. Therapy consists of using the following groups of drugs:
- If the cause of exudative pericarditis is a bacterial infection, then the patient is recommended to use broad-spectrum antibiotics. These include semisynthetic penicillins, aminoglycosides, and cephalosporins. In the presence of purulent effusion, drugs are administered directly into the cavity after pumping out the exudate and rinsing with antiseptics.
- For autoimmune lesions and connective tissue diseases, glucocorticoids (Prednisolone, Hydrocortisone) are used. The same medications are used to eliminate severe inflammation in any type of pericarditis.
- Pain relief in the acute period is carried out using NSAIDs and analgesics. For this purpose, take Diclofenac, Meloxicam, Aspirin. Duration of treatment ranges from 2 – 3 days to several weeks.
- Severe congestion in the systemic circulation and a significant volume of effusion require the use of diuretics. To remove excess fluid, Furosemide is prescribed in combination with Spironolactone.
Surgical methods
Surgical treatment of exudative pericarditis includes pericardiocentesis and pericardiectomy:
- During pericardiocentesis, a needle is inserted into the chest from the side of the xiphoid process and, after determining the place of greatest accumulation of fluid, it is replaced with a catheter through which it flows. This allows you to remove most of the effusion, take it for examination and alleviate the person’s condition. Manipulation can be carried out under the control of an X-ray, ECG or ultrasound of the heart. Drainage continues from several hours to days.
- Pericardiectomy involves removing part of the outer lining of the heart. This allows you to restore hemodynamics in most patients with severe compression of the organ. In severe and advanced cases, even this approach is not able to eliminate the problem; mortality after surgery ranges from 6 to 12%.
Rehabilitation
With proper treatment of effusion pericarditis and the absence of complications, recovery occurs after three months. Gradually the person will be able to return to normal life. Longer rehabilitation is necessary in the case of a recurrent form of the disease, when from time to time the effusion in the pericardial cavity accumulates again.
Recovery after surgery requires a longer period: the patient is kept in the hospital for 5 days. If a person’s life is not in danger, he is discharged under the supervision of a cardiologist at his place of residence. Usually, health improves after 3–4 months, and complete restoration of the functioning of blood vessels and the heart occurs after six months.
To speed up the rehabilitation process it is recommended:
- visit your doctor regularly and follow all his instructions;
- monitor your diet: it should be complete and healthy;
- gradually increase physical activity, but do not overload;
- completely eliminate smoking and drinking alcohol;
- monitor your health and immediately seek help if problems arise;
- carry out sanitation of foci of inflammation.
Complications
With exudative pericarditis, a number of complications may develop. The most commonly observed:
- heart failure;
- rhythm disturbances (tachycardia, atrial fibrillation);
- formation of adhesions;
- transition of the disease to a chronic form;
- tamponade (occurs in 40% of cases).
Pediatric pericarditis
Infants are also predisposed to pericardial inflammation. This phenomenon is mainly caused by an infectious nature: staphylococcus, streptococcus, sore throat, etc. The main therapy here is intended not only to eliminate the symptoms, but the very root cause of the imbalance of cardiac fluid. An older child may detect signs of pericarditis due to a viral infection, and if he has been diagnosed with arthrosis, arthritis and other disorders of the connective tissue structure.
Among the causes of inflammation of the heart sac are the following:
- vitamin deficiency;
- blood diseases, hematopoietic disorders;
- malfunction of the thyroid gland;
- hereditary factors;
- hormonal imbalances;
- tumors of the cardiac cavity, pericardium;
- treatment with medications.
There is a possibility of developing rare forms of pathologies caused by nephritis. This process is further aggravated due to the weakening of the body’s protective functions. Diagnosing pericarditis in children is more difficult than in adults. For these purposes, it is advisable to use a cardiovisor for the highest quality diagnosis and recognition of the cause of the development of cardiac pathology.
Drug therapy for children comes down to the prescription of antibiotics and anti-inflammatory drugs, taking into account the specific age category. The duration of treatment depends on the severity of the disease and its form, symptoms and condition of the child’s body.
ECG
ECG changes in acute pericarditis are considered pathognomonic of the disease and are therefore diagnostically innovative. ECG changes develop in four temporally sequential stages, which are influenced by the ST segment and T wave.
- Stage I: In the acute stage, diffuse ST segment elevations with J-point elevation can be seen in several or almost all leads. They develop in the first few days and can last from one to two weeks. In aVR and V1 derivatives, the ST distance is usually reduced. The PQ interval is reduced in nearly two-thirds of cases due to the resulting subepicardial injury—a reciprocal change again found in aVR and V1.
- Stage II: ST line convexities recede and T wave alignment is noticeable.
- Stage III: T wave negatives will occur from the end of the second to the third week.
- Stage IV: During the first three months, T wave changes resolve again.
All four stages can be found in approximately 50 percent of patients. Atrial fibrillation is common, with a trend paralleling the healing of the pericarditis - usually within a few months - decreasing again. On the other hand, calcifications or chronic recurrent events are risk factors for persistence or recurrence of atrial fibrillation in the long term.
ECG 1
ECG 2
Fig.: Acute pericarditis with ECG stage II-III. Regressive ST elevations with negative T in I, aVL, V5 and V6. In V2-V4, positive T waves are followed by clearly visible U waves.