The structure of the human heart - anatomy
The heart muscle consists of 4 chambers - 2 atria and 2 ventricles. The left ventricle and left atrium form the so-called arterial part of the organ, based on the nature of the blood found here. In contrast, the right ventricle and right atrium make up the venous part of the heart.
The circulatory organ is presented in the shape of a flattened cone. It has a base, apex, lower and anterosuperior surfaces, as well as two edges - left and right. The apex of the heart has a rounded shape and is formed entirely by the left ventricle. The atria are located in the base area, and the aorta lies in its anterior part.
Major myocardial diseases: their danger and algorithm for dealing with the consequences
The heart is one of the cavity organs of our body. It has four cavities that are filled with blood (circulating from one chamber to another): the right and left ventricles, the right and left atria. All of them are separated from each other by partitions, in the walls of which there are small holes with valves responsible for the targeted movement of blood.
The myocardium is one of the layers of the heart wall. It is muscular in nature. The inside is covered with an inner membrane - the endocardium. It is surrounded on the outside by the epicardium.
Heart muscle cells are histologically slightly different from our skeletal muscles. This difference in structure is associated with electrophysiological characteristics and the need to propagate the action potential between myocardial cells (cardiomyocytes).
The wall of the left ventricle is better developed than the right part and the atria, which allows it to carry out a greater load.
There are many clinical classifications of heart diseases, which include the myocardium as one of the layers of the organ. Its pathologies are divided into coronarogenic and non-coronarogenic.
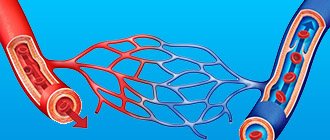
Coronarogenic diseases are diseases accompanied by disruption of blood flow in the vessels of the heart. Similar conditions can occur due to cardiosclerosis and thrombus formation, which lead to myocardial infarction. High blood pressure, bad habits, prolonged stress, excessive caffeine consumption and many other factors can also cause ischemia, strokes, hibernating myocardium, etc.
Non-coronarogenic are pathologies that arise against the background of inflammatory processes, dystrophic changes that involve the heart muscle in the process of degeneration.
Among myocardial diseases it is also common to distinguish:
- myocarditis;
- myocardial dystrophy;
- cardiomyopathy.
They all have different causes (etiology), and have different effects on well-being, changing a person’s quality of life for the worse.
Diagnosis of the above diseases requires special attention, since their clinical manifestations are often similar to each other, and untimely provision of qualified assistance leads to the progression of hypoxia and hypertrophy of the myocardial walls. As a result, we observe an increase in preload, changes in ejection fraction, rhythm disturbances, conduction, excitability, etc.
Major myocardial diseases
| Disease | Etiology | Possible consequences | Fighting algorithm |
| Myocarditis |
| Rhythm disturbances, development of heart failure, sepsis, cardiac arrest | First of all, the disease must be prevented. Preventing the occurrence of myocarditis consists of maintaining bed rest during infectious processes and timely treatment. If the patient has pathology, hospitalization in a cardiology hospital is required according to the standards |
| Myocardial dystrophy | Non-inflammatory muscle damage as a consequence of metabolic disorders in various diseases:
| Rhythm disturbances, myocardial contractility, development of heart failure, increased fatigue, cardiac arrest | You can prevent the occurrence of the disease by balancing your diet and regulating your lifestyle. Avoiding stress also has a positive effect on the likelihood of illness. Preventive examinations once a year help to identify endocrine and other pathologies in the early stages, that is, before myocardial dystrophy is detected as a consequence |
| Cardiomyopathies |
| Rhythm disturbances, development of heart failure, increased fatigue, cardiac arrest | You can prevent the development of cardiomyopathy by changing your lifestyle, giving up bad habits and staying in the environment of cardiotoxic drugs. When diagnosing a pathology, treatment by a cardiologist and specialists is necessary, whose consultation is required in the presence of concomitant pathology |
| Vegetative-disovarial (menopausal) cardiopathy |
| Rhythm disturbances, development of heart failure, increased fatigue | A balanced diet, consumption of vitamins, minerals and trace elements contribute to an easier course of menopause. Regular examinations by a gynecologist help to identify disorders in the early stages, when treatment is quite effective. |
The structure of the myocardium of the atria and ventricles has a number of features and certain functions, due to which the uninterrupted functioning of the heart occurs. From the veins, blood flows into the atria, they, in turn, push them into the ventricles, and they already direct the blood flow through the arteries. The right ventricle supplies blood to the pulmonary arteries, and the left one throws blood into the aorta, which extends its arteries to all the walls and organs of the human body.
Speaking about the atrial myocardium, it is definitely worth mentioning their muscle layers, which are divided into superficial and deep. The structure of the upper layer contains transversely or circularly arranged fibers, and the deep layer contains longitudinal fibers. There are only 2 atria - the right and left, they are separated from each other by the interatrial septum.
The right atrium has a cubic shape and contains a fairly large cavity, which is called the right appendage. The left one is represented by a non-standard cubic shape, consists of 5 holes, 4 of which are localized from top to bottom and represent the openings of the pulmonary veins. But the fifth hole of the largest shape is called the left atrioventricular foramen; it provides communication between the atrium and the ventricle of the same name.
Atria and ventricles - location features
The structure of the myocardium of the atria and ventricles of the heart is quite unique and has significant differences. If in the atria there are two layers of muscles, then in the ventricles there are three. Two of them are single, but the third layer, which is located between those two, has horizontally located fibers; it is this middle horizontal layer that exists separately for the left and right representatives.
In addition, speaking about the structure of the ventricles, it is imperative to highlight such a feature of their structure as various bulges and irregularities that extend from their deep muscular layer. Some of them are fleshy crossbars, others have the form of columns that become sharper towards the apex and in medicine are called papillary muscles. All of these, even the smallest components, are of great importance and help ensure normal cardiac activity in general.
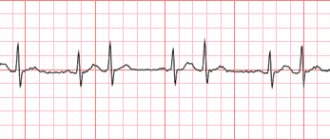
Phases of the heart
There are several separate phases of contraction of the heart muscle:
- At the beginning, contraction of the atria occurs. Then, with some slowdown, ventricular contraction begins. During this process, blood naturally tends to fill the chambers with reduced pressure. Why doesn’t it flow back into the atria after this? The fact is that the blood is blocked by the gastric valves. Therefore, it can only move in the direction of the aorta, as well as the vessels of the pulmonary trunk.
- The second phase is relaxation of the ventricles and atria. The process is characterized by a short-term decrease in the tone of the muscle structures from which these chambers are formed. The process causes a decrease in pressure in the ventricles. Thus, the blood begins to move in the opposite direction. However, this is prevented by the closing pulmonary and arterial valves. During relaxation, the ventricles fill with blood that comes from the atria. On the contrary, the atria are filled with bodily fluid from the large and
Cardiac cycle
This is one complete contraction and relaxation of all chambers of the heart.
- Phase I - atrial systole - 0.1 s.
- Phase II - ventricular systole - 0.33 s.
- Phase III - general pause - 0.37 s.
The cardiac cycle lasts 0.8 s. at 75 beats/min.
Phase I
- pressure in the left atrium - max=8-15 mm Hg. (average value 5-7 mmHg);
- pressure in the right atrium - max=3-8 mm Hg. (average value 2-4 mmHg).
During atrial systole, the ventricles are in the diastole phase, they are filled with blood. The pressure in them = 2-3 mm Hg. The pressure in the atria is greater, which means blood enters the ventricles.
Flap valves are open . The lumen of the veins closes due to contraction of smooth muscles.
II phase
Phase II - ventricular systole - 0.33 s.
Voltage period (0.08 s)
Asynchronous contraction phase (0.05 s):
- the excitation process spreads throughout the ventricular myocardium;
- pressure in the ventricles is close to 0;
- gradually contraction covers all myocardial fibers;
- pressure in the ventricles increases;
- blood rushes back into the atria;
- but blood does not enter the atria, because flap valves close;
- I or systolic sound occurs .
Isometric contraction phase (0.03 s):
- there is no shortening of myocardial fibers (both leaflet and semilunar valves are closed);
- the volume of blood in the ventricles remains constant;
- the length of the fibers does not change, but the voltage increases;
- the left ventricle is rounded and hits the inner surface of the chest with force (cardiac impulse);
- the pressure in the ventricles becomes higher than the pressure in the aorta and pulmonary artery;
- in the left ventricle reaches 70-80 mm Hg, in the right - 15-20 mm Hg;
- blood from the ventricles rushes into the vessels.
Ejection period (0.25 s)
- protosphygmic interval - 0.005 s;
- rapid ejection phase - 0.1-0.12 s.: pressure in the left ventricle - 120-130 mm Hg,
- pressure in the right ventricle - 25-39 mm Hg;
III phase
Phase III - ventricular diastole - 0.47 s.
Relaxation period - 0.12 s.:
- protodiastolic interval - 0.04 s ( closing of semilunar valves - II heart sound );
- isometric relaxation phase - 0.08 s (the length of the fibers does not change, the pressure in the ventricles gradually decreases with the valves closed and becomes slightly less than in the atria).
The flap valves open and the filling period begins.
Filling period - 0.25 s
- rapid filling phase - 0.08-0.09 s (oscillations of the walls of the ventricles due to the rapid flow of blood to them, hence the appearance of the third heart sound );
- slow filling phase - 0.16-0.17 s (this phase is hemodynamically ineffective; at heart rate = 120-140 beats/min it is absent).
At this point the heart rhythm ends, but ventricular diastole continues for another 0.1 s.
Atrial systole (presystole for the ventricles) occurs.
Presystole - 0.1 s
Active filling of the ventricles with blood. The atria pump additional blood into the ventricles - a fourth heart sound .
Intersystolic interval - 0.007 s.
Diastole is necessary for:
- ensuring the initial polarization of cardiomyocytes (operation of the Na-K pump),
- removal of Ca from the sarcoplasm,
- resynthesis of glycogen and ATP,
- filling the heart with blood.
A new cycle of ventricular activity begins again.
What is responsible for the work of the heart?
As is known, the functioning of the heart muscle is not a voluntary act. The organ remains active continuously, even when a person is in a state of deep sleep. There are hardly people who pay attention to their heart rate during activity. But this is achieved due to a special structure built into the heart muscle itself - a system for generating biological impulses. It is noteworthy that the formation of this mechanism occurs in the first weeks of intrauterine conception of the fetus. Subsequently, the impulse generation system does not allow the heart to stop throughout life.
In a calm state, the number of contractions of the heart muscle per minute is about 70 beats. Within one hour the number reaches 4200 beats. Considering that during one contraction the heart releases 70 ml of fluid into the circulatory system, it is easy to guess that up to 300 liters of blood passes through it in an hour. How much blood does this organ pump over its entire life? This figure averages 175 million liters. Therefore, it is not surprising that the heart is called an ideal engine that practically does not fail.
Myocardium
The myocardium is a multi-tissue muscular layer of the heart that is formed by striated fibers, loose connective structures, nerve processes, and a branched network of capillaries. Here are P-cells that form and conduct nerve impulses. In addition, the myocardium contains myocytes and cardiomyocytes, which are responsible for the contraction of the blood organ.
The myocardium consists of several layers: inner, middle and outer. The internal structure consists of muscle bundles that are located longitudinally in relation to each other. In the outer layer, bundles of muscle tissue are located obliquely. The latter go to the very top of the heart, where they form the so-called curl. The middle layer consists of circular muscle bundles, separate for each of the ventricles of the heart.
General information about the muscular system of the heart
The immediate responsibility of the muscle is to uniformly load all parts, namely the atria and ventricles. It is worth saying that our “motor” consists of two parts, each of which has its own sections, like the atria and ventricles. So, one of the missions is to ensure that these departments have completely independent work.
| Endocardium | Is the thinnest and is placed inside |
| Myocardium | The middle layer of the heart wall, which has a fairly thick cross-sectional appearance |
| Epicard | Outer layer, distinguished by its thinness |
Attention! A distinctive factor in the composition of muscle tissue is the peculiarity of the location of its cells, which have some processes, and thanks to them are closely intertwined with each other.
It is worth saying that the cells have an elongated nucleus inside them, which has adapted to the work of the cells themselves in such a way that when they contract, they also decrease. This phenomenon is a rather interesting design from an anatomical point of view. In addition, the presence of chromosomes in these cells significantly exceeds standard indicators, due to which cardiomyocytes withstand significant cardiac loads.
Speaking about the structure of the myocardium of the atria and ventricles, they are distinguished by an interesting feature, with the help of which the performance of the cardiac organ increases significantly. More precisely, the muscle tissue of the ventricles has a special structure, which has three layers of muscles. The peculiarity of their placement is that two of these layers have the same structure and are located at the edges of the muscles, and the middle one is distinguished by a horizontal arrangement of fibers.
Epicard
The presented membrane of the heart muscle has the smoothest, thinnest and somewhat transparent structure. The epicardium forms the outer tissue of the organ. In fact, the membrane acts as the inner layer of the pericardium - the so-called cardiac sac.
The surface of the epicardium is formed from mesothelial cells, under which there is a connective, loose structure represented by connective fibers. In the region of the apex of the heart and in its grooves, the lining in question includes adipose tissue. The epicardium fuses with the myocardium in the areas of least accumulation of fat cells.
Endocardium
text_fields
text_fields
arrow_upward
Endocardium (endocardium) –
thin membrane lining the cavities of the heart. The endocardium in the atria is thicker than in the ventricles. In its structure and development, the endocardium is similar to the inner lining of the vascular wall - the intima. The deep layer of the endocardium consists of connective tissue with numerous elastic fibers, blood vessels, smooth muscle and fat cells. The endothelium covers the endocardium, lining the cavities of the heart from the inside, and passes directly into the wall of the vessels connected to the heart.
Heart valves, both leaflet and semilunar, are folds (doublings, duplications) of the endocardium, having a connective tissue base with numerous collagen and elastic fibers. At the base of the valves, these fibers pass into the dense connective tissue of the rings surrounding the openings. From the middle layer of each leaflet of the atrioventricular valve, tendon threads begin, which are also covered with endocardium. These threads are stretched between the papillary muscles and the surface of the valve leaflets facing the ventricles. The leaflets of the semilunar valves are thinner than those of the atrioventricular valves and do not have tendon strands. Near the edges of such valves, the layer of dense connective tissue is somewhat thickened and forms a nodule in their middle part. These thickened strips of fabric touch each other when the valve closes. The narrow free edge of each flap ensures complete tightness when the valve is closed.
In various diseases, the structure of the valve leaflets may be disrupted. In this case, the valves are deformed, become denser, and do not close completely; they can shorten or grow together at the edges. As a result of such defects, the valve loses its ability to prevent the reverse flow of blood.
Outer lining of the heart Fig. 701. Heart, cor. Sternocostal (anterior) surface.] (The pericardium is removed at the point of its transition into the epicardium.) (diagram). Rice. 700. X-ray image of the heart and large vessels in various projections (diagram).
The right and left fibrous rings are interconnected into a common plate, which completely, with the exception of a small area, isolates the atrium muscles from the ventricular muscles. In the middle of the fibrous plate connecting the ring there is a hole through which the muscles of the atria are connected to the muscles of the ventricles through the atrioventricular bundle.
In the circumference of the openings of the aorta and pulmonary trunk (see Fig.) there are also interconnected fibrous rings; The aortic ring is connected to the fibrous rings of the atrioventricular orifices.
Pericardium
The pericardium is the outer layer of the heart, also called the pericardial sac. This structure is presented in the form of an obliquely cut cone. The inferior base of the pericardium is placed on the diaphragm. Toward the top, the shell goes more to the left than to the right. This peculiar bag surrounds not only the heart muscle, but also the aorta, the mouth of the pulmonary trunk and adjacent veins.
The pericardium forms in human individuals during the early stages of fetal development. This happens approximately 3-4 weeks after the formation of the embryo. Violations of the structure of this membrane, its partial or complete absence, often lead to congenital heart defects.
The structure of the walls of the heart
STRUCTURE OF THE WALLS OF THE HEART
The walls of the heart consist of 3 layers: the inner - endocardium, the middle - myocardium4 and the outer - epicardium, which is the visceral layer of the pericardium, the pericardium.
The thickness of the walls of the heart is formed mainly by the middle layer, the myocardium, myocardium, consisting of muscle tissue. The outer layer, epicardium, represents the visceral layer of the serous pericardium. The inner layer, endocardium, lines the cavities of the heart.
Myocardium myocardium , or muscle tissue of the heart, although it has transverse striations, differs from skeletal muscles in that it does not consist of individual bundles, but is a network of interconnected fibers with a central location of the nuclei. The musculature of the heart is divided into two sections: the muscular layers of the atrium and the muscular layers of the ventricles. The fibers of both begin from two fibrous rings - anuli fibrosi, of which one surrounds the ostium atrioventriculare dextrum, the other - the ostium atrioventriculare sinistrurn. Since the fibers of one section, as a rule, do not pass into the fibers of another, the result is the possibility of contraction of the atria separately from the ventricles. In the atria, there are superficial and deep muscle layers: the superficial one consists of circularly or transversely located fibers, the deep one - of longitudinal ones, which with their ends start from the fibrous rings and cover the atrium in a loop. Along the circumference of the large venous trunks flowing into the atria, there are circular fibers covering them, like sphincters. The fibers of the superficial layer cover both atria, the deep fibers belong separately to each atrium.
The musculature of the ventricles is even more complex. Three layers can be distinguished in it: a thin superficial layer is composed of longitudinal fibers that start from the right fibrous ring and go obliquely downwards, moving to the left ventricle; at the apex of the heart they form a curl, vortex cordis, bending here in a loop-like manner in depth and forming an internal longitudinal layer, the fibers of which are attached to the fibrous rings with their upper ends. The fibers of the middle layer, located between the longitudinal outer and inner ones, run more or less circularly, and, unlike the superficial layer, they do not pass from one ventricle to another, but are independent for each ventricle separately (Fig. 206, 207).
The so-called conduction system of the heart plays an important role in the rhythmic functioning of the heart and in coordinating the activity of the muscles of the individual chambers of the heart. Although the muscles of the atria are separated from the muscles of the ventricles by fibrous rings, there is a connection between them through the conduction system, which is a complex neuromuscular formation. The muscle fibers that make up it (Purkinje fibers) have a special structure: they are poor in myofibrils and rich in sarcoplasm, therefore lighter. They are sometimes visible to the naked eye in the form of light-colored threads and represent a less differentiated part of the original syncytium, although they are larger in size than ordinary muscle fibers of the heart. In the conductive system, nodes and bundles are distinguished (Fig. 208).
1. Atrioventricular bundle, fasciculus atrioventricularis , begins with a thickening of the nodus atrioventricularis (Aschof-Tavara node), located in the wall of the right atrium, near the cuspis septalis of the tricuspid valve. The fibers of the node, directly connected to the muscles of the atrium, continue into the septum between the ventricles in the form of the bundle of His (noted a little earlier by Kent). In the ventricular septum, the bundle of His is divided into two legs - crus dextrum and sinistrum, which go into the walls of the ventricles and branch under the endocardium in their muscles. The atrioventricular bundle is very important for the functioning of the heart, since it transmits a wave of contraction from the atria to the ventricles, thereby establishing the regulation of the rhythm of systole - the atria and ventricles.
2. The sinus node, nodus sinuatriali s, or sinusoatrial bundle of Keys-Flyak, is located in the section of the wall of the right atrium corresponding to the sinus venosus of cold-blooded animals (in the sulcus terminalis, between the superior vena cava and the right ear). It is associated with the muscles of the atrium and is important for their rhythmic contraction.
Consequently, the atria are connected to each other by the sinusoatrial bundle, and the atria and ventricles are connected by the atrioventricular bundle. Typically, irritation from the right atrium is transmitted from the sinus node to the atrioventricular node, and from it along the His bundle to both ventricles.
The epicardium, epicardium, covers the outside of the myocardium and is a regular serous membrane lined on the free surface with mesothelium.
Endocardium, endocardium , lines the inner surface of the cavities of the heart. It, in turn, consists of a layer of connective tissue with a large number of elastic fibers and smooth muscle cells, another layer of connective tissue located externally with an admixture of elastic fibers, and an internal endothelial layer, which is how the endocardium differs from the epicardium. The endocardium in its origin corresponds to the vascular wall, and its listed layers correspond to the 3 membranes of the vessels. All heart valves represent folds (duplicates) of the endocardium.
The described features of the structure of the heart determine the features of its vessels, which form, as it were, a separate circle of blood circulation - the heart.
Arteries of the heart (Fig. 209, 210) - aa. coronariae dextra et sinistra, coronary arteries, right and left, begin from the bulbus aortae below the upper edges of the semilunar valves.
Therefore, during systole, the entrance to the coronary arteries is covered with valves, and the arteries themselves are compressed by the contracted heart muscle. As a result, during systole the blood supply to the heart decreases; blood enters the coronary arteries during diastole, when the entrance openings of these arteries, located at the mouth of the aorta, are not closed by the semilunar valves. Right coronary artery, a. coronaria dextra, leaves the aorta according to the right semilunar valve and lies between the aorta and the appendage of the right atrium, outward from which it bends around the right edge of the heart along the coronary groove and passes to its posterior surface. Here it continues into the interventricular branch, r. interventricularis posterior. The latter descends along the posterior interventricular groove to the apex of the heart, where it anastomoses with a branch of the left coronary artery.
The branches of the right coronary artery vascularize: the right atrium, part of the anterior and entire posterior wall of the right ventricle, a small portion of the posterior wall of the left ventricle, the interatrial septum, the posterior third of the interventricular septum, the papillary muscles of the right ventricle and the posterior papillary muscle of the left ventricle.
Left coronary artery, a. coronaria sinistra , emerging from the aorta at its left semilunar valve, also lies in the coronary groove anterior to the left atrium. Between the pulmonary trunk and the left ear, it gives off two branches: a thinner one - the anterior, interventricular, ramus interventricularis anterior, and a larger one - the left, circumflex, ramus circumflexus.
Stomach diseases
The first descends along the anterior interventricular groove to the apex of the heart, where it anastomoses with the branch of the right coronary artery, as discussed above. The second, continuing the main trunk of the left coronary artery, bends around the heart on the left side along the coronary groove and also connects with the right coronary artery. As a result, an arterial ring is formed along the entire coronary sulcus, located in a horizontal plane, from which branches extend perpendicularly to the heart. The ring is a functional device for collateral circulation of the heart. The branches of the left coronary artery vascularize the left atrium, the entire anterior and most of the posterior wall of the left ventricle, part of the anterior wall of the right ventricle, the anterior 2/3 of the interventricular septum and the anterior papillary muscle of the left ventricle.
There are various options for the development of the coronary arteries, as a result of which there are different ratios of blood supply basins.
From this point of view, three forms of blood supply to the heart are distinguished: uniform with the same development of both coronary arteries, left coronary and right coronary. In addition to the coronary arteries, “additional” arteries from the bronchial arteries, from the lower surface of the aortic arch near the arterial ligament, approach the heart, which is important to consider so as not to damage them during operations on the lungs and esophagus and thereby not worsen the blood supply to the heart.
Intraorgan arteries of the heart (Fig. 211, 212): from the trunks of the coronary arteries and their large branches, respectively, to the 4 chambers of the heart, the arteries of the atria (aa. atriales) and their ears (aa. auriculares), the arteries of the ventricles (aa. ventriculares), and the arteries of the septa depart between them (aa. septi anterior et posterior).
Having penetrated into the thickness of the myocardium, they branch according to the number, location and structure of its layers: first in the outer layer, then in the middle (in the ventricles) and, finally, in the inner layer, after which they penetrate into the papillary muscles (aa. papillares) and even into the atrioventricular muscles valves The intramuscular arteries in each layer follow the course of the muscle bundles and anastomose in all layers and parts of the heart.
Some of these arteries have a highly developed layer of smooth muscle in their wall, the contraction of which completely closes the lumen of the vessel, which is why these arteries are called “closing”. A temporary spasm of the “closing” arteries can lead to a cessation of blood flow to this area of the heart muscle and cause myocardial infarction. A case of an accessory coronary artery of the heart arising from the truncus pulmonalis is described.
The veins of the heart do not open into the vena cava, but directly into the cavity of the heart.
Intramuscular veins are found in all layers of the myocardium and, accompanying the arteries, correspond to the course of muscle bundles. Small arteries (up to 3rd order) are accompanied by double veins, large ones - by single ones. Venous outflow goes along three paths: 1) into the coronary sinus, 2) into the anterior veins of the heart and 3) into the small veins (Tebesia - Viessen), flowing directly into the right side of the heart. There are more of these veins in the right half of the heart than in the left, and therefore the coronary veins are more developed on the left.
The predominance of Tebesia veins in the walls of the right ventricle with a small outflow through the coronary sinus vein system indicates that they play an important role in the redistribution of venous blood in the cardiac region.
1. Veins of the coronary sinus system, sinus coronarius cordis. It is a remnant of the left duct of Cuvier and lies in the posterior part of the coronary sulcus of the heart between the left atrium and the left ventricle. With its right, thicker end, it flows into the right atrium near the septum between the ventricles, between the valve of the inferior vena cava and the atrium septum. The following veins drain into the sinus coronarius:
a) v. cordis magna, starting at the apex of the heart, rises along the anterior interventricular groove of the heart, turns to the left and, going around the left side of the heart, continues into the sinus coronarius; b) v. posterior ventriculi sinistri - one or more venous trunks on the posterior surface of the left ventricle, flowing into the sinus coronarius or v. cordis magna; c) v. obliqua atrii sinistri - a small branch located on the posterior surface of the left atrium (remnant of the embryonic v. cava superior sinistra); it begins in the pericardial fold, which encloses a connective tissue cord, plica venae cavae sinistrae, also representing the remnant of the left vena cava; d) v. cordis media lies in the posterior interventricular groove of the heart and, having reached the transverse groove, flows into the sinus coronarius; e) v. cordis parva is a thin branch located in the right half of the transverse sulcus of the heart and usually flows into the v. cordis media, in the place where this vein reaches the transverse groove.
2. Anterior veins of the heart, vv. cordis anteriores, - small veins, are located on the anterior surface of the right ventricle and flow directly into the cavity of the right atrium.
3. Small veins of the heart, vv. cordis minimae, - very small venous trunks, do not appear on the surface of the heart, but, collected from capillaries, flow directly into the cavities of the atria and ventricles.
There are 3 networks of lymphatic capillaries in the heart: under the endocardium, inside the myocardium and under the epicardium. Among the efferent vessels, two main lymphatic collectors of the heart are formed. The right collector arises at the beginning of the posterior interventricular groove; it receives lymph from the right ventricle and atrium and reaches the left upper anterior nodes of the mediastinum, lying on the aortic arch near the beginning of the left common carotid artery.
The left collector is formed in the coronary groove at the left edge of the pulmonary trunk, where it receives vessels carrying lymph from the left atrium, left ventricle and partially from the anterior surface of the right ventricle; then it goes to the tracheobronchial, or tracheal nodes, or the nodes of the root of the left lung.
Both collectors flow into the nodes of the anterior mediastinum, into the left tracheal or tracheobronchial nodes.
The nerves that provide innervation to the cardiac muscles, which have a special structure and function, are complex and form numerous plexuses. The entire nervous system is composed of: 1) suitable trunks, 2) plexuses in the heart itself, and 3) nodal fields associated with the plexus.
Functionally, the nerves of the heart are divided into 4 types: slowing and accelerating, weakening and strengthening. Morphologically, these nerves are part of n. vagus and tr. sympathicus. Sympathetic nerves (mainly postganglionic fibers) arise from the three upper cervical and five upper thoracic sympathetic nodes: n. cardiacus cervicitis superior - from ganglion cervicale superius, n. cardiacus cervicalis medius - from ganglion cervicale medium, n. cardiacus cervicalis inferior - from ganglion cervicale inferius or ganglion cervicothoracicum s. ganglion stellatum and nn. cardiaci thoracici from the thoracic nodes of the sympathetic trunk.
The cardiac branches of the vagus nerve begin from its cervical region (rami cardiaci superiores), thoracic region (rami cardiaci medii) and from n. laryngeus recurrens vagi (rami cardiaci inferiores). The nerves approaching the heart are divided into two groups - superficial and deep. The superficial group is adjacent to the carotid and subclavian arteries in the upper section, and to the aorta and pulmonary trunk in the lower section. The deep group, composed mainly of the branches of the vagus nerve, lies on the anterior surface of the lower third of the trachea. These branches come into contact with the lymph nodes located in the trachea, and when the nodes become enlarged, for example in pulmonary tuberculosis, they can be compressed by them, which leads to a change in heart rhythm. From these sources, two nerve plexuses are formed.
1) superficial, plexus cardiacus superficialis, between the aortic arch (under it) and the bifurcation of the pulmonary trunk;
2) deep, plexus cardiacus profundus, between the aortic arch (behind it) and the tracheal bifurcation.
These plexuses continue into the plexus coronarius dexter et sinister, surrounding the homonymous vessels, as well as into the plexus located between the epicardium and myocardium. Intraorgan branches of nerves depart from the last plexus. The plexuses contain numerous groups of ganglion cells and nerve nodes.
Afferent fibers start from the receptors and go along with the efferent fibers as part of the vagus and sympathetic nerves.
Functions of the heart - why do we need a heart?
Our blood provides the entire body with oxygen and nutrients. In addition, it also has a cleansing function, helping in the removal of metabolic waste.
The function of the heart is to pump blood through blood vessels.
How much blood does the human heart pump?
The human heart pumps from 7,000 to 10,000 liters of blood in one day. This amounts to approximately 3 million liters per year. That works out to 200 million liters over a lifetime!
The amount of blood pumped per minute depends on the current physical and emotional load - the greater the load, the more blood the body requires. So the heart can conduct from 5 to 30 liters through itself in one minute.
The circulatory system consists of about 65 thousand vessels, their total length is about 100 thousand kilometers! Yes, we didn't make a mistake.
Circulatory system
The human cardiovascular system is formed by two circles of blood circulation. With each heartbeat, blood moves in both circles at once.
Pulmonary circulation
- Deoxygenated blood from the superior and inferior vena cava enters the right atrium and then into the right ventricle.
- From the right ventricle, blood is pushed into the pulmonary trunk. The pulmonary arteries carry blood directly to the lungs (to the pulmonary capillaries), where it receives oxygen and releases carbon dioxide.
- Having received enough oxygen, the blood returns to the left atrium of the heart through the pulmonary veins.
Systemic circulation
- From the left atrium, blood moves into the left ventricle, from where it is subsequently pumped through the aorta into the systemic circulation.
- After going through a difficult path, the blood again arrives through the vena cava to the right atrium of the heart.
Normally, the amount of blood pushed out of the ventricles of the heart is the same with each contraction. Thus, an equal volume of blood simultaneously enters the greater and lesser circulation.
What is the difference between veins and arteries?
- Veins are designed to transport blood to the heart, and the job of arteries is to supply blood in the opposite direction.
- In veins, blood pressure is lower than in arteries. Accordingly, the walls of arteries are more elastic and dense.
- Arteries saturate “fresh” tissue, and veins take away “waste” blood.
- In the case of vascular damage, arterial or venous bleeding can be distinguished by its intensity and the color of the blood. Arterial - strong, pulsating, beating like a “fountain”, the color of the blood is bright. Venous - bleeding of constant intensity (continuous flow), the color of the blood is dark.
The weight of a human heart is only about 300 grams (on average 250 grams for women and 330 grams for men). Despite its relatively low weight, it is undoubtedly the main muscle in the human body and the basis of its life activity. The size of the heart is indeed approximately equal to a human fist. Athletes' hearts can be one and a half times larger than those of the average person.
Anatomical structure
The heart is located in the middle of the chest at the level of 5-8 vertebrae.
Normally, the lower part of the heart is located mostly in the left side of the chest. There is a variant of congenital pathology in which all organs are mirrored. It is called transposition of internal organs. The lung, next to which the heart is located (normally the left one), is smaller in size relative to the other half.
The back surface of the heart is located near the spinal column, and the front surface is reliably protected by the sternum and ribs.
The human heart consists of four independent cavities (chambers) divided by partitions:
- two upper ones - the left and right atria;
- and two lower ones - the left and right ventricles.
The right side of the heart includes the right atrium and ventricle. The left half of the heart is represented, respectively, by the left ventricle and atrium.
The inferior and superior vena cava enter the right atrium, and the pulmonary veins enter the left atrium. From the right ventricle
the pulmonary arteries (also called the pulmonary trunk) emerge.
from the left ventricle
.
The heart has protection from overstretching and other organs, which is called the pericardium or pericardial sac (a kind of membrane in which the organ is enclosed). It has two layers: an outer dense, strong connective tissue called the fibrous membrane of the pericardium
and internal (
serous pericardium
).
Thus, the heart itself consists of three layers: epicardium, myocardium, endocardium. It is the contraction of the myocardium that pumps blood through the vessels of the body.
The walls of the left ventricle are approximately three times larger than the walls of the right! This fact is explained by the fact that the function of the left ventricle is to push blood into the systemic circulation, where the resistance and pressure are much higher than in the pulmonary circulation.
The device of heart valves
Special heart valves allow you to constantly maintain blood flow in the correct (unidirectional) direction. The valves alternately open and close, either letting blood through or blocking its path. Interestingly, all four valves are located along the same plane.
Between the right atrium and the right ventricle is the tricuspid
valve. It contains three special leaflet plates that, during contraction of the right ventricle, can provide protection from the reverse flow (regurgitation) of blood into the atrium.
The mitral valve works in a similar way
, only it is located on the left side of the heart and is bicuspid in its structure.
Aortic valve
prevents the reverse flow of blood from the aorta into the left ventricle. Interestingly, when the left ventricle contracts, the aortic valve opens as a result of blood pressure on it, so it moves into the aorta. After which, during diastole (the period of relaxation of the heart), the reverse flow of blood from the artery promotes the closure of the valves.
Normally, the aortic valve has three leaflets. The most common congenital heart abnormality is bicuspid aortic valve. This pathology occurs in 2% of the human population.
Pulmonary valve
at the moment of contraction of the right ventricle, it allows blood to flow into the pulmonary trunk, and during diastole it does not allow it to flow in the opposite direction. It also consists of three doors.
Cardiac vessels and coronary circulation
The human heart requires nutrition and oxygen, just like any other organ. The vessels that supply (feed) the heart with blood are called coronary or coronary
. These vessels branch from the base of the aorta.
The coronary arteries supply the heart with blood, and the coronary veins remove deoxygenated blood. Those arteries that are located on the surface of the heart are called epicardial. Subendocardial arteries are called coronary arteries hidden deep in the myocardium.
Most of the blood outflow from the myocardium occurs through three cardiac veins: large, middle and small. Forming the coronary sinus, they flow into the right atrium. The anterior and small veins of the heart deliver blood directly to the right atrium.
Coronary arteries are divided into two types - right and left. The latter consists of the anterior interventricular and circumflex arteries. The great cardiac vein branches into the posterior, middle and small veins of the heart.
Even absolutely healthy people have their own unique characteristics of coronary circulation. In reality, the vessels may look and be located differently than shown in the picture.
Frequently asked questions to the doctor
What is the anatomical axis of the heart?
This is a collective term for 3 conventional lines perpendicular to each other passing through the center of the organ:
- longitudinal - from top to base;
- transverse - from the outer wall of the right to the outer wall of the left ventricle
- anteroposterior.
The heart can turn relative to these lines. Such changes are detected when performing an electrocardiogram.
Is the structure of the right half of the heart different from the left, where is the heart muscle and where is the apex of the heart?
Oblique longitudinal incision through the left half of the heart and the right atrium
The lower, “pointed-rounded” part is called the Apex of the Heart. You can see where it is located in the photo above. With strong heartbeats and a small subcutaneous fat layer, its tremors can be visible on the left side of the solar plexus.
Despite the similarity in the names of the heart chambers, there is a difference in structure between the right and left halves of the heart. The different functional roles of the atria and ventricles determine their differences in volume and wall thickness.
In addition, there is a 3-leaf valve on the right side, and a 2-leaf (mitral) valve on the left. Completely different arteries enter and exit the atria. The location of the nodes and bundles of the conducting system of electrical impulses also differs.
What is the distinctive feature of the structure of the arteries of the heart, in particular the aorta?
The larger the lumen of the blood vessel, the thicker its wall. But unlike veins, in arteries this occurs due to an increase in the middle layer of the vascular walls - muscle fibers consisting of smooth myocytes.
Structure of the aortic wall
The pulmonary trunk and aorta are the largest arteries in diameter and belong to the elastic type vessels. To withstand large pressure drops resulting from blood impulses, their walls, in all 3 layers that form them, contain a large number of thick elastic elements and an amorphous intercellular substance - glycosaminoglycan.
Smooth myocytes in the middle layer of the aortic wall have a circular-spiral direction, and there are fewer of them than in the walls of other arteries. In addition, the outer and middle layers of the aorta contain vessels (vasa vasorum) and nerves.
How does the heart develop (form)?
Pulse path
This system ensures automatism of the heart - excitation of impulses generated in cardiomyocytes without an external stimulus. In a healthy heart, the main source of impulses is the sinoatrial (sinus) node. He is the leader and blocks the impulses from all other pacemakers. But if any disease occurs that leads to sick sinus syndrome, then other parts of the heart take over its function. Thus, the atrioventricular node (automatic center of the second order) and the His bundle (AC of the third order) are able to activate when the sinus node is weak. There are cases when secondary nodes enhance their own automaticity even during normal operation of the sinus node.
Sinus node
located in the upper posterior wall of the right atrium in close proximity to the mouth of the superior vena cava. This node initiates pulses with a frequency of approximately 80-100 times per minute.
Atrioventricular node (AV)
located in the lower part of the right atrium in the atrioventricular septum. This septum prevents the impulse from propagating directly into the ventricles, bypassing the AV node. If the sinus node is weakened, then the atrioventricular node will take over its function and begin to transmit impulses to the heart muscle at a frequency of 40-60 contractions per minute.
The atrioventricular node then passes into the bundle of His.
(atrioventricular bundle divided into two legs). The right leg rushes towards the right ventricle. The left leg is divided into two more halves.
The situation with the left bundle branch has not been fully studied. It is believed that the left leg with fibers from the anterior branch rushes to the anterior and lateral wall of the left ventricle, and the posterior branch supplies fibers to the posterior wall of the left ventricle and the lower parts of the lateral wall.
In case of weakness of the sinus node and atrioventricular block, the His bundle is capable of creating impulses at a speed of 30-40 per minute.
The conducting system deepens and further branches into smaller branches, eventually passing into Purkinje fibers
, which penetrate the entire myocardium and serve as a transmission mechanism for contraction of the ventricular muscles. Purkinje fibers are capable of initiating impulses at a frequency of 15-20 per minute.
Exceptionally trained athletes can have a normal resting heart rate down to the lowest recorded figure of just 28 beats per minute! However, for the average person, even one leading a very active lifestyle, a heart rate below 50 beats per minute may be a sign of bradycardia. If your heart rate is this low, you should be examined by a cardiologist.
Heartbeat
A newborn's heart rate may be around 120 beats per minute. As a person gets older, the pulse stabilizes between 60 and 100 beats per minute. Well-trained athletes (we are talking about people with well-trained cardiovascular and respiratory systems) have a heart rate of 40 to 100 beats per minute.
The rhythm of the heart is controlled by the nervous system - the sympathetic strengthens contractions, and the parasympathetic weakens.
Cardiac activity, to a certain extent, depends on the content of calcium and potassium ions in the blood. Other biologically active substances also contribute to the regulation of heart rhythm. Our heart may begin to beat faster under the influence of endorphins and hormones released when listening to our favorite music or kissing.
In addition, the endocrine system can have a significant impact on the heart rhythm - both the frequency of contractions and their strength. For example, the release of the well-known adrenaline by the adrenal glands causes an increase in heart rate. The hormone with the opposite effect is acetylcholine.
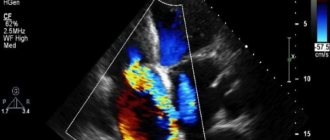
Heart sounds
One of the simplest methods for diagnosing heart disease is to listen to the chest using a stethoscope (auscultation).
In a healthy heart, during standard auscultation, only two heart sounds are heard - they are called S1 and S2:
- S1 is the sound heard when the atrioventricular (mitral and tricuspid) valves close during ventricular systole (contraction).
- S2 - the sound heard when the semilunar (aortic and pulmonary) valves close during diastole (relaxation) of the ventricles.
Each sound consists of two components, but to the human ear they merge into one due to the very short period of time between them. If, under normal conditions of auscultation, additional tones become audible, this may indicate some kind of disease of the cardiovascular system.
Sometimes additional abnormal sounds may be heard in the heart, called a heart murmur. As a rule, the presence of murmurs indicates some kind of heart pathology. For example, noise can cause blood to flow back in the opposite direction (regurgitation) due to malfunction or damage to a valve. However, noise is not always a symptom of a disease. To clarify the reasons for the appearance of additional sounds in the heart, it is worth doing echocardiography (ultrasound of the heart).
Variant and age-related features of the heart structure
The “motor organ,” which begins pumping blood as early as the 4th week of fetal development and works throughout life, has distinctive features in children, and in some people it may occupy a different position in the chest.
Dextrocardia
To the question - Which side is the heart located, they usually answer - On the left. Is there a heart on the right side?
Yes, this arrangement occurs, but not more often than 1 in 10,000 people. It's called dextrocardia. In 75% of cases, this situation is considered as a variant of the norm. However, in 25% this is a consequence of a gene defect in the cilia of the ciliated epithelium.
Dextrocardia (drawing and x-ray)
People with an isolated right-sided heart have been plagued since childhood by a constant cough with purulent sputum and otitis media, causing hearing loss. The fingers gradually become like drumsticks.
Such men are often infertile, and in women the fertilized egg is implanted not in the uterus, but in the fallopian tube.
Features of the structure of the heart of a newborn and child
After birth, the blood “pump” is not cone-shaped, but spherical, the size of a penny coin and weighs from 18 to 20 grams.
On the interatrial septum after birth there is still an oval hole, which usually closes with a petal with the first breath, closes quite quickly, and is then called the fossa ovale. If this does not happen before the age of 5, then a diagnosis is made - Patent foramen ovale.
Oval window, chamber sizes, place and location of the heart in a newborn
At first, the heart of a newborn baby is located transversely and cranially (very high in relation to the diaphragm). This is due to the unusual position and different sizes compared to the adult state - a huge thymus gland, a large liver and atria, small ventricles. The “motor” gradually descends and assumes its normal and oblique position only by the age of 10.
For your information. The heart rate of a fetus is 2 times faster than that of a mature person, and is about 160 beats per minute. At 12 weeks of intrauterine development, the “pump”, which is just beginning to develop, already pumps more than 60 liters of blood per day.
The anatomy of the heart and blood vessels in newborns also includes the following differences:
- the diameter of the aorta is less than the diameter of the pulmonary trunk;
- the aortic arch is located almost horizontally;
- the carotid artery has a convexity posteriorly and outwardly, and its division site is located near the high 2nd cervical vertebra, and descends as it grows.
In the first months of life, the atria grow rapidly, and the ventricles begin to rapidly increase in volume, especially the left one, only starting from the age of 10. Such anatomical and physiological features of a child’s heart, such as low blood pressure and tachycardia in the first years of life, are caused by: the high need of the growing body for oxygen, the small volume of chambers and blood squeezed out with each beat, and sympathicotonia.
Cardiac activity until the age of 3-4 years, until the branches of the vagus nerve are myelinated, is regulated mainly by the sympathetic nervous system.
In the first years of life, girls have smaller hearts than boys. During puberty, at the age of 12-16, girls experience an intensive increase in cardiac mass, after which it begins to lag again. The increase in the mass of the heart walls stops at the age of 21-25 years.
And in conclusion, for those who want to learn even more details about the structure of one of the main human organs, we suggest watching the video - Anatomy of the human heart and its secrets.
Heart diseases
It is not surprising that the number of cardiovascular diseases is increasing in the world. The heart is a complex organ that actually rests (if it can be called rest) only in the intervals between heartbeats. Any complex and constantly working mechanism itself requires the most careful treatment and constant prevention.
Just imagine what a monstrous burden falls on the heart given our lifestyle and low-quality, abundant nutrition. Interestingly, mortality from cardiovascular diseases is also quite high in high-income countries.
The huge amounts of food consumed by the population of wealthy countries and the endless pursuit of money, as well as the associated stress, destroy our hearts. Another reason for the spread of cardiovascular diseases is physical inactivity - catastrophically low physical activity that destroys the entire body. Or, on the contrary, an illiterate passion for heavy physical exercise, often occurring against the background of which people do not even suspect and manage to die right during “health” activities.
Lifestyle and heart health
The main factors that increase the risk of developing cardiovascular diseases are:
- Obesity.
- High blood pressure.
- Increased blood cholesterol levels.
- Physical inactivity or excessive physical activity.
- Abundant, low-quality food.
- Depressed emotional state and stress.
Make reading this great article a turning point in your life - give up bad habits and change your lifestyle.
On this topic...
The walls of the heart consist of three layers:
- endocardium
- thin inner layer; - myocardium
- a thick muscle layer; - epicardium
is a thin outer layer that is the visceral layer of the pericardium - the serous membrane of the heart (heart sac).
Endocardium
lines the cavity of the heart from the inside, exactly repeating its complex relief. The endocardium is formed by a single layer of flat polygonal endothelial cells located on a thin basement membrane.
Myocardium
formed by cardiac striated muscle tissue and consists of cardiac myocytes interconnected by a large number of jumpers, with the help of which they are connected into muscle complexes that form a narrow-loop network. This muscle network ensures the rhythmic contraction of the atria and ventricles. The atria have the smallest myocardial thickness; in the left ventricle it is the greatest.
Atrial myocardium
separated by fibrous rings from the ventricular myocardium. The synchrony of myocardial contractions is ensured by the conduction system of the heart, which is common to the atria and ventricles. In the atria, the myocardium consists of two layers: superficial (common to both atria) and deep (separate). In the superficial layer, the muscle bundles are located transversely, in the deep layer - longitudinally.
Ventricular myocardium
consists of three different layers: outer, middle and inner. In the outer layer, the muscle bundles are oriented obliquely, starting from the fibrous rings, continuing down to the apex of the heart, where they form the helix of the heart. The inner layer of the myocardium consists of longitudinally located muscle bundles. Due to this layer, papillary muscles and trabeculae are formed. The outer and inner layers are common to both ventricles. The middle layer is formed by circular muscle bundles, separate for each ventricle.
Epicard
built like serous membranes and consists of a thin plate of connective tissue covered with mesothelium. The epicardium covers the heart, the initial sections of the ascending aorta and pulmonary trunk, and the terminal sections of the vena cava and pulmonary veins.
General information about the muscular system of the heart
Myocardium is the muscle tissue of the heart, which consists of mononuclear, transversely arranged cells.
It is this arrangement of cardiomyocytes that makes it very durable, capable of evenly distributing the load on all parts of the heart. The structure of the myocardium has one very important feature - the complete independence of the atria and ventricles. Another equally important feature of the heart muscle is its unique ability to contain skeletal and smooth muscle tissue. Speaking about skeletal muscle tissue, it was from it that the myocardium took its striated transverse striations, and from smooth tissue its cellular structure, which allows it to avoid control by human consciousness
The myocardium of the heart has another very interesting feature. Namely, the cells of a hollow organ are very closely interconnected. This is due to the fact that they have processes that cling closely and tightly to each other. Consequently, cardiomyocytes form a common network where structural fibers are very closely intertwined and pass into each other.
The places where cell processes connect to each other are called intercalary discs; they have many slits through which, in fact, excitation is transmitted to all cells. It is this unique moment that is the main feature of muscle tissue; intercalated discs transmit excitation along the fibers with incredible speed, this leads to the fact that the entire muscular structure of the heart is very quickly covered by excitation and contracts in response to it. The response to excitation - contractility - can be achieved in about 0.4 seconds.
The main properties of the heart muscle include:
- excitability, which is manifested by the ability to react to the received irritation;
- conductivity, which distributes excitation throughout all parts of the myocardium and conduction system;
- contractility, when in response to excitability the heart muscle has the ability to contract;
- relaxation.
If we talk about the strength of contraction of the heart muscle, it depends on several factors, namely:
- from the total number of available actomyosin bridges formed simultaneously;
- on the amount of calcium ions entering the sarcoplasm. The greater their number, the stronger the contraction ability will be.
Features of the internal structure of the myocardium
Our heart has the incredible ability to work like a powerful motor, as it is sometimes called. There is no need to talk about its importance, because everyone knows that without it, a person’s life comes to an end. It is for this reason that you should take care of your health in advance, and have at least some understanding of the structure of the heart.
Knowing the structure and functions of the heart, many ailments can be detected in time.
For its full functioning, the human “engine” must perform the following tasks:
- supply the body with the necessary amount of blood;
- promptly convert biochemical energy into mechanical energy.
Important! You should know that this “motor” is located in the pericardial sac. This absolutely does not prevent it from supplying all vital human organs with oxygen, which comes with blood.
But the most important information is the importance of the middle layer in the entire physiological process. It is important to know that the structure of the myocardium of the heart is distinguished by the transverse arrangement of mononuclear cells; they, in turn, are called cardiomyocytes. This feature makes the walls of the organ strong enough to perform all the necessary functions in the life of the body. Thanks to this structure, the load is distributed evenly and does not create unnecessary problems and overloads.
Thus, regular contraction of the middle layer in the human cardiac organ depends on correctly distributed such processes:
- autogenic;
- heterogeneous;
- neurohumoral.
In addition, its proper operation requires an even distribution of preloads and afterloads, which provide control in the distribution of blood flow.