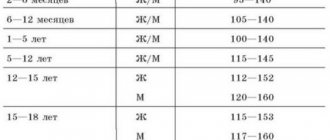
general information
Vaquez disease (also called polycythemia vera or primary polycythemia) is a chronic tumor pathology that develops in the human circulatory system. As a rule, this disease can be identified through diagnostic tests, during which it turns out that the level of red blood cells in the patient’s blood is too high. However, the patients do not experience any damage to internal organs, in which such indicators are considered normal.
Also, with the development of Vaquez disease, the blood structure becomes more viscous and thick. Against this background, there is a strong slowdown in blood flow, which can lead to the formation of blood clots. This condition can provoke hypoxia.
If we talk about the history of Vaquez’s disease, it was first described back in 1892. Then one scientist discovered a relationship between certain patient indicators and the development of erythremia. Subsequently, the disease was named after the specialist himself. Therefore, in medical reference books this pathology is more often found under the name Vaquez Osler disease.
If we talk about who is most predisposed to this disease, then older people should be most careful about their health. Most often, men suffer from polycythemia
Children and middle-aged people are much less likely to experience this disease. However, if the younger generation shows the first signs of the disease, then in this case Vaquez’s disease is much more severe.
Reasons for the development of polycythemia
It is difficult to say about the specific factors that lead to the development of pathology. This disease is still being studied by medical specialists. However, the etiology and pathogenesis of Vaquez disease contain information that the disease develops against the background of mutational changes. They originate in stem cells located in the bone marrow. Accordingly, we are talking about genetic pathology.
Very often, several relatives have the same form of erythremia. Vaquez's disease also develops against the background of increased erythropoiesis. As a rule, absolute erythrocytosis leads to it.
Disorders associated with blood clotting can also provoke this condition. However, experts admit other causes of pathology.
History of leprosy and general information about the disease
Leprosy (leprosy) is an infectious disease that affects the skin and peripheral nervous system of humans.
The disease leprosy is considered one of the oldest diseases, mentions of which are found in the Old Testament. In those days, people with leprosy were considered “unclean.” Healthy people shunned them, they were persecuted and deprived of the right to a normal life. The peak incidence of leprosy occurred in the 12th-14th centuries, when the infection affected the population of almost all European countries. To combat leprosy, medieval aesculapians used numerous leper colonies - institutions that identified and treated lepers. Initially, leprosy patients were located on the territory of monasteries, where they were allocated houses and plots for agricultural activities. In fact, the unfortunate people lived in a kind of reservations and did not have the opportunity to communicate with the rest of the world. However, then the isolation of leprosy patients was completely justified and bore fruit. By the 16th century, leprosy had disappeared from Europe. Isolated cases of the disease were recorded for some time on the Mediterranean coast and Scandinavia, but large-scale epidemics never developed.
Today we know almost everything about leprosy. Contrary to popular belief, the infection is not transmitted by simply touching a patient and does not always lead to death. It is known that the disease leprosy threatens only 5-7% of people, and the remaining inhabitants of the Earth have stable immunological protection against the pathogen. As for the method of transmission of infection. In most cases, infection requires prolonged direct skin contact. There is also a theory that leprosy, the symptoms of which can appear 10 years after the infection, enters the body by inhaling bacteria secreted from the mouth or nasal cavity of a sick person. Perhaps it is this assumption that partly explains the fact that today there are about 11 million leprosy patients registered in the world and many of them have not had any skin contact with infected people.
Causes and factors for the development of the disease
Polycythemia vera occurs due to the development of tumors in the red bone marrow (especially of a malignant nature), any congenital mutations, a genetic predisposition to impaired production of blood cells (in particular, red blood cells) and insufficient oxygen supply to the body (hypoxia).
A false type of pathology is formed under the influence of many factors on the human body, for example, such as:
- the presence of malignant neoplasms of internal organs;
- chronic heart failure (CHF);
- chronic renal failure (CRF);
- various infectious diseases, both viral and bacterial;
- various intoxications, including alcohol and drugs;
- increased blood pressure in the pulmonary artery (pulmonary hypertension syndrome);
- chronic obstructive pulmonary disease (COPD);
- smoking abuse for a long time;
- unfavorable climatic conditions (for example, it has been noted that people living in the equatorial and high mountain zones are more susceptible to the disease);
- unfavorable working conditions (pathology is most common among people working deep underground, for example, in mines, and at high altitudes);
- unfavorable environmental conditions (the risk of disease increases for people living in cities with high levels of pollution, as well as near them and near factories);
- hypoxia (insufficient oxygen supply to the body as a result of constant exposure to stuffy, poorly ventilated rooms, exposure to heat, and so on);
- dehydration of the body (excessive loss of fluid due to various poisonings, diarrhea, vomiting, burns affecting a large area of skin, and so on);
- nervous overstrain for a long time;
- unhealthy lifestyle, including poor nutrition.
Bad habits and poor lifestyle can contribute to the development of polycythemia
In general, the exact reasons for the occurrence of multiblood are still unknown to science. Scientists suggest that the disease occurs as a result of a mutational change in a special enzyme produced in the red bone marrow, which causes excess production and increased division of all stem cells, from which blood cells subsequently develop, especially red blood cells.
Polycythemia is often found in newborns. As a rule, it is secondary in nature and is associated with the presence of other pathologies or is transmitted from the mother through the placenta (in this case, the pathology is temporary and after some time disappears on its own without any interventions or external influences). In addition, it can also occur as a consequence of hypoxia. The baby’s body begins to compensate for the lack of oxygen by the excessive production of red blood cells.
Polycythemia is most often detected in newborn twins.
Methods for diagnosing Vaquez disease
Modern diagnosis of pathology is quite accurate. Testing should include methods that will rule out or confirm other diseases with similar symptoms. The doctor first performs a detailed analysis of the entire body to identify complications of Vaquez disease.
Important! Some symptoms of erythremia are similar to other diseases. For example, hypoxia is often associated with disorders of the respiratory system, and anemia can be caused by improper use of vitamin B12 or blood loss. And minor changes in blood composition occur after taking certain medications.
Establishing a diagnosis is a complex of examinations that create an overall clinical picture. The interpretation of the tests and the prescription of studies should be carried out by the attending doctor. It is impossible to diagnose Vaquez disease at home.
General inspection
The initial check carried out by the doctor includes an analysis of all the patient’s complaints, examination of the skin and mucous membranes of the oral cavity. The doctor palpates the spleen and taps the flat bones. He is interested in whether there has been a sharp weight loss, what chronic diseases there are, including allergic reactions. The therapist should find out about recent infections and surgeries, taking medications and dietary supplements, and bad habits.
Hereditary traits are also an important indicator. The patient talks about diseases that his immediate family has, including cardiovascular disease and oncology. Next, the therapist decides what examinations to send the patient for. First of all, a blood test is prescribed.
Laboratory research
A blood test is the most informative initial test. It is after this that the doctor decides to send the patient for other studies. The patient undergoes general and biochemical tests, which reveal the number of red blood cells, leukocytes, lymphocytes, platelets, neutrophils, and hemoglobin. They also check coagulability, the amount of serum vitamin B12 and phosphatase, and arterial blood oxygen saturation.
| Index | Norm for women | Norm for men |
| Red blood cells | 3,7 – 4,7 | 4,0 – 5,1 |
| Hemoglobin | 117 – 160 | 130 – 172 |
| Leukocytes | 4,0 – 9,0 | 4,0 – 9,0 |
| Platelets | 180 – 320 | 180 – 320 |
| Band neutrophils | 1 – 5 | 1 – 5 |
| Segmented neutrophils | 47 – 72 | 47 – 72 |
A blood test will help your doctor distinguish polycythemia vera from secondary or false erythrocytosis. Next, the patient is referred for a bone marrow puncture.
Bone marrow check
A bone marrow biopsy is the test that most accurately diagnoses Vaquez disease. But since this procedure is a mini-operation with its own contraindications and possible complications, it is resorted to in case of serious suspicion of polycythemia.
A bone marrow puncture is performed from the ilium or sternum. The selected material is sent for histological and cytogenetic examination. The histology result shows the presence of benign or malignant neoplasms. Cytogenetic research analyzes the state of chromosomes and genetic abnormalities in them.
Ultrasound of internal organs
An enlarged spleen and liver is a very important indicator when making a diagnosis. Palpation can only determine a strong enlargement of the spleen, so an ultrasound of the abdominal organs is prescribed for a detailed and accurate check. In addition to the hematopoietic organs, they look at the duodenum, pancreas, gall bladder, stomach, and intestines.
Important! Splenomegaly and hepatomegaly occur in the clinical picture of many other diseases. The size of these organs is affected by infections, hepatitis, autoimmune disorders, alcohol and smoking abuse, anemia, and cysts.
At the initial stage of the disease, the size and tissue of organs may not change. But their condition is not a reason to cancel the diagnosis of polycythemia vera if it was established after a bone marrow puncture. Ultrasound of internal organs shows treatment methods and the severity of the patient’s condition.
Vessel check
The attending physician must understand the state of the blood vessels at the time of the patient's visit. The dilation of the veins, their tortuosity, dystrophic processes, and the presence of blood clots are assessed. Blood clots can form not only due to pathological viscosity. With atherosclerosis, plaques also form in the vessels, which interfere with normal blood circulation. To rule out atherosclerotic plaques, your doctor may prescribe an additional blood test for cholesterol.
The examinations are carried out by a phlebologist using special equipment. Particular attention is paid to the condition of the large vessels of the legs and internal veins (esophagus). The main methods are ultrasound of veins and venography (X-ray examination with the introduction of a contrast agent).
Traditional medicine and proper nutrition
First of all, it is worth noting that in order to get rid of polycythemia, it is very important to eat right and make sure that the person does not overload himself physically. If we are talking about the very beginning of the development of pathology, the patient is assigned table No. 15
However, there are some caveats. First of all, the patient should not eat foods that can increase blood flow and hematopoiesis, so he should stop eating liver. It is worth consuming dairy and plant products.
If the patient’s condition is characterized by the second stage of the pathology, then he is prescribed table No. 6. A similar diet is recommended for gout. In this case, you must completely exclude meat and fish dishes from your diet. It is also necessary to avoid legumes and sorrel.
After the patient is discharged from the hospital, he must carefully monitor his health and adhere to all doctor’s recommendations.
If we talk about traditional treatment, then almost all patients are interested in this issue. You need to understand that this pathology develops over many years, so choosing the appropriate treatment with herbs will be problematic. Even if the symptoms of the pathology have subsided, this does not mean that the patient has been completely cured. He may still experience exacerbations of the disease. Unfortunately, with the help of herbs you can only relieve pain or dull it. However, in this case there is no talk of a complete cure.
First of all, you need to talk to your doctor, and only then think about traditional methods of treatment. If the doctor agrees to additional methods of therapy, then you need to remember that we are talking about a blood disease.
You can find a huge number of recipes online that will help increase your hemoglobin levels. However, this does not mean that these recommendations are suitable for the treatment of polycythemia. Erythremia (Vaquez disease) is not easily treated with natural remedies. Although doctors are not against traditional medicine, when it comes to polycythemia, almost everyone agrees that in this case it is impossible to select a complex of medicinal herbs. The course of the pathology affects the functioning of the bone marrow and affects the circulatory system. It is necessary to objectively evaluate all the possibilities of natural drugs.
However, to improve their condition, some resort to blood thinner prescriptions. For example, you can brew a spoonful of sweet clover herb in a glass of boiling water. After the mixture has cooled, it must be strained through cheesecloth. The finished medicine is taken three times a day, approximately 80-100 ml. The course of such treatment should not be more than one month. After this, you must definitely take a break.
Many people also use dry or fresh cranberries. Two spoons of a natural product are poured into a glass of boiling water. After this, the container must be covered and wait 20-30 minutes for the broth to infuse. After this, the sour juice can be diluted with honey or regular granulated sugar. The main advantage of this method is that cranberries can be drunk in any quantity if the patient is not allergic to it.
Content:
The structure of hematopoietic cells in this pathology is completely normal. However, their number continues to increase, so the viscosity becomes greater. As a result, blood begins to flow more slowly, and this leads to the formation of blood clots. As a result, blood circulation is obstructed and hypoxia occurs.
Polycythemia vera is another name for erythremia. In other words, we have leukemia in a chronic form.
You can determine the pathology by looking at the face of a person suffering from erythremia: it will be red. Usually a blood test confirms the assumption.
Important! Redness can also be caused by other reasons, such as increased blood pressure. Emotional people tend to blush very often. But such redness goes away quickly, but with erythremia it will last a long time.
This disease was first described in the 19th century by Dr. Vaquez, hence another name - Vaquez's disease. In the 20th century, the initiative was taken up by Osler, who studied the pathogenesis and compiled its description. The disease is rare - approximately 1 person out of 25,000. It has been noted that in older men (over 60 years old), erythremia is common, but age is not a hindrance for the pathology. It was found that erythremia does not affect young children, and if detected, it indicates another disease, for example, toxic dyspepsia.
The pathogenesis of erythremia proposed by Osler, still used in scientific works
It was already said above that erythremia refers to leukemia. This raises a burning question for many people: is erythremia cancer or not? To begin with, it should be clarified that cancer is a tumor that occurs in isepithelial tissues, and erythremia occurs in blood tissues. Yes, the tumor is malignant, but the cell changes are high, and the course of the pathology is benign until a certain time.
Important! The course will be benign only if the prescribed treatment is started in a timely manner and the patient follows all the doctor’s recommendations.
Video about polycythemia vera (erythremia)
As soon as erythropoiesis begins to change, the manifestation of the disease worsens and the course becomes malignant. No one can say the exact forecast - it all depends on progress.
Varicose veins in the legs can occur in both older and younger people. There are many reasons for it: poor lifestyle, choice of uncomfortable shoes and clothes, spending most of the time in a sitting position, and even heredity. Depending on the severity of the disease, appropriate treatment is required: from exercises, massage and drug therapy to surgery.
Treatment of polycythemia
Phlebotomy (bloodletting)
Phlebotomy tubes for bloodletting
Normalizes the level of hemoglobin and red blood cells by reducing the patient's blood volume. The volume of bloodletting is up to 500 milliliters per procedure. Such procedures are carried out under the supervision of a hematologist once every two days until hemoglobin (140–150) and hematocrit (45%) decrease within normal limits. This method stimulates the bone marrow well and relieves skin itching. In most cases, bloodletting is used in combination with chemotherapy.
Cytoreductive therapy (chemotherapy)
Used to inhibit the recovery of red blood cells and platelets. For this purpose, pharmacological drugs of different groups are used: imifos, myelobromol, myelosan, chlorambucil, and also hydroxyurea and pipobroman are used.
In each specific case, the hematologist selects an individual treatment regimen.
Diagnosis of erythremia
Vaquez disease can be diagnosed by donating blood for analysis and undergoing an examination using instrumental devices.
Methods for diagnosing erythremia:
- A general clinical analysis of blood mass shows the level of red blood cells, hemoglobin, platelets, leukocytes, hematocrit and ESR.
- A biochemical study of the blood substance establishes the indicators of uric acid, bilirubin, iron, alkaline phosphatase, AST (aspartate aminotransferase) and ALT (alanine aminotransferase).
- A laboratory study of the blood flow of the blood supply reveals the level of total serum that binds iron.
- Study of blood samples to determine the level of erythropoietin. By determining the indicators of this hormone, it is possible to detect the degree of abnormalities in the hematopoietic system.
- Ultrasound (ultrasound) is used to examine the liver and spleen.
Examination of bone marrow in Vaquez disease by histological or cytological method. For this purpose, trepanobiopsy or sternal puncture is performed. In addition to everything, it would be useful to conduct Doppler sonography. This diagnostic method shows the speed of blood flow in the organs and tissues being examined. Thanks to Doppler ultrasound in Vaquez disease, it is possible to identify areas of the circulatory system affected by blood clots.
Treatment
Treatment of erythremia begins immediately after diagnosis. It is impossible to postpone therapy until later, as this can lead to progression of the disease and the development of complications.
The emphasis is on the following:
- use of medications;
- symptomatic therapy;
- and hemoglobin;
- correction of urate diathesis;
- improved blood flow;
- elimination of iron deficiency.
Drug therapy
If there are severe symptoms of erythremia, treatment is based on the use of cytostatics - drugs that suppress cell growth. These drugs are prescribed in the following cases:
- the concentration of blood cells increases rapidly;
- internal organs (liver, spleen) enlarge;
- complications associated with the formation of blood clots (heart attacks, strokes) occur.
The most commonly prescribed medications are Myelosan, Busulfan, Imiphos, hydroxyurea, and radioactive phosphorus. The most effective is the latter drug, which accumulates in the bones and suppresses the functioning of the bone marrow. In most cases, treatment gives a positive result: it helps to eliminate the symptoms of the disease and the onset of remission for a period of 2-3 years. If therapy is ineffective, another 1 course is given.
Cytostatics are potent drugs that can cause adverse reactions. Therefore, treatment is carried out in a hospital setting under the supervision of a doctor who monitors compliance with dosages and dosage regimen. Treatment with cytostatics requires constant monitoring of peripheral blood parameters.
Improving blood flow
When blood becomes viscous, blood pressure increases and the risk of blood clots increases. You can improve blood flow and prevent the development of thrombotic complications with the help of medications: Heparin, Dipyridamole, Aspirin, etc.
Also for this purpose, bloodletting can be performed - a procedure associated with the artificial removal of part of the blood from the body. First, the doctor disinfects the patient’s skin, then pierces one of the superficial veins with a special needle. Sessions are held every other day. In one procedure, you can remove from 150 to 400 ml of blood.
Bloodletting leads to the following results:
- normalization of the number of blood cells;
- decreased blood pressure;
- elimination of erythromelalgia - bright hyperemia and burning pain in the extremities;
- normalization of hematocrit and hemoglobin.
Decreased hemoglobin and hematocrit levels
If the examination results show an increase in the number of red blood cells while maintaining a normal number of white blood cells and platelets, treatment is reduced to removal. This therapy has a positive effect on the course of the disease.
To reduce the level of hematocrit and hemoglobin, bloodletting is used (method described earlier). Vaquez disease can also be treated using erythrocytepheresis, a method associated with the removal of red blood cells from the blood.
Elimination of iron deficiency
Patients with erythremia often present with anemia. Iron deficiency may be a consequence of treatment (bloodletting, erythrocytepheresis) or active formation of red blood cells. Regardless of what causes this condition, it must be treated, because it negatively affects the course of the disease.
You can replenish the amount of iron in your body using the following medications:
- Maltofer.
- Ferrum Lek.
- Hemopher.
- Sorbifer.
- Totema et al.
Correction of urate diathesis
An increased level of uric acid in the blood indicates the presence of urate diathesis, a condition that requires immediate treatment. If therapy is delayed until later, severe complications (including disability) may develop.
To correct urate diathesis, drugs such as Anturan (Sulfinpyrazone) and Allopurinol are prescribed.
Symptomatic therapy
Symptomatic treatment of Vaquez disease is carried out at all stages of the development of the pathological process. The task comes down to eliminating the symptoms of increased blood volume, thrombotic and anemic complications.
The following medications are used as part of symptomatic therapy:
- hypotensive - reduce high blood pressure;
- antihistamines - relieve skin itching;
- cardiac glycosides - improve heart function;
- gastroprotectors - protect the gastrointestinal tract.
For anemia, transfusions of blood, red blood cells and platelets are performed. With increased destruction of blood cells in the spleen, resection (removal) of the organ is performed.
Vaquez disease requires complex treatment. Proper implementation of therapy increases the length and quality of life of the patient.
Treatment methods
To choose a treatment strategy for erythremia, it is necessary to accurately determine which disease acted as the root cause. In addition, it is important to find out whether polycythemia is primary or secondary. For this purpose, the necessary laboratory tests are carried out.
True erythremia requires treatment of tumors in the bone marrow, and the secondary type requires getting rid of the root cause, that is, the disease that provoked a violation of the blood composition.
With true erythremia, treatment requires a lot of effort from doctors, which includes eliminating tumors in the bone marrow and preventing their reappearance. Here, an important role is played by the patient’s age, his individual characteristics, and concomitant pathologies. Not all medications are approved for older people, which significantly complicates the therapy process.
Bloodletting is considered an effective method of treatment. During the session, the blood volume decreases by approximately 500 ml. This allows you to reduce the concentration of platelets and thin the blood.
Cytopheresis is often used for treatment. This method allows you to filter the blood. The patient is given 2 catheters in one and the other arm, through one the blood enters a special device, and through the second it returns in a purified state. Sessions are held every other day.
The method of treatment is selected taking into account the type of disease and the severity of its course.
Secondary Vaquez disease is treated by getting rid of the pathology that caused polycythemia. This is, as a rule, a violation of the functioning of the lungs, heart, dehydration, etc.
Does folk treatment help?
Many patients with polycythemia are interested in the question of whether it is possible to improve blood composition using folk recipes? The fact is that Vaquez’s disease is a serious pathology, and without timely drug treatment, traditional methods will be absolutely ineffective. The main goal of drug therapy is to maximize the period of remission and delay the transition of erythremia to the third stage.
Even if there is a lull, the patient must remember that the pathology can recur at any time and make every effort to prevent this process. Throughout his life, he must be under medical supervision, discuss his condition with his attending physician, and undergo all necessary tests.
In folk medicine, indeed, there are a lot of recipes designed to improve blood composition, but they should not be used to increase hemoglobin and thin the blood. To date, no medicinal herbs that could slow down the progression of the pathology have been found. Therefore, you should not risk your health and self-medicate.
Causes
The provoking factors for the development of the disease depend on the form of the disease. Primary polycythemia occurs as a result of a neoplastic neoplasm of the red bone marrow. The predetermining causes of true erythrocytosis are:
- genetic malfunctions in the body - mutation of the tyrosine kinase enzyme, when the amino acid valine is replaced by phenylalanine;
- hereditary predisposition;
- bone marrow cancers;
- oxygen deficiency - hypoxia.
The secondary form of erythrocytosis is caused by external causes. Concomitant diseases play an equally important role in development. Provoking factors are:
- climatic conditions;
- living in high mountains;
- congestive heart failure;
- cancerous tumors of internal organs;
- pulmonary hypertension;
- action of toxic substances;
- overstrain of the body;
- x-ray radiation;
- insufficient oxygen supply to the kidneys;
- infections that cause intoxication of the body;
- smoking;
- bad ecology;
- genetic features - Europeans are more likely to get sick.
The secondary form of Vaquez disease is caused by congenital causes - autonomous production of erythropoietin, high affinity of hemoglobin for oxygen. There are also acquired factors in the development of the disease:
- arterial hypoxemia;
- kidney pathologies - cystic lesions, tumors, hydronephrosis, renal artery stenosis;
- bronchial carcinoma;
- adrenal tumors;
- cerebellar hemangioblastoma;
- hepatitis;
- cirrhosis of the liver;
- tuberculosis.
Prevention
There are no ways to prevent this disease.
Polycythemia vera (from the ancient Greek πολυ - many, κúτος - cell and αïμα - blood), or erythremia, Vaquez disease, is a chronic leukemia belonging to the group of benign tumor processes of the blood system, affecting all hematopoiesis, but especially erythroid. Clinically, this is manifested by an increase in the number of red blood cells in the peripheral blood, an increase in hemoglobin levels, an increase in the viscosity and coagulation ability of circulating blood. In some cases, leuko- and thrombocytosis occurs.
The disease mainly occurs in old age. For many years, erythremia may not manifest itself in any way. If it occurs in young people, which is very rare, the picture is much more serious.
During polycythemia vera there are three stages of progression. In the initial phase, patients are usually bothered by a feeling of heaviness in the head, tinnitus, increased fatigue, dizziness, decreased mental performance, sleep disturbance and chilliness of the extremities. External more or less characteristic signs may well be absent.
The advanced (erythremic) stage is characterized by the development of vivid symptoms. The most common complaint here is headaches, which sometimes take the form of painful migraines, accompanied by vision problems. Many experience pain or discomfort in the heart area, sometimes reminiscent of angina pectoris, pain in the epigastric region, in the bones, tips of the fingers, toes, as well as weight loss, hearing impairment, emotional lability and, very often, itchy skin.
During a physical examination, attention is drawn to the specific reddish-cyanotic color of the skin with a predominance of a dark cherry hue. The redness of visible mucous membranes is also determined
Against the background of frequent thrombosis of the vessels of the extremities, darkening of the skin on the legs and sometimes trophic ulcers are observed. Many patients complain of bleeding gums and causeless bruises.
In 80% of patients, a moderate enlargement of the spleen is detected (severe splenomegaly is characteristic already of the third, terminal phase). The size of the liver is usually increased, and blood pressure is often increased. As a result of malnutrition of the mucous membrane, ulcers of the stomach and duodenum can occur. Thrombosis of the coronary, cerebral and lower extremity vessels is observed.
The picture of the terminal stage is determined by the outcome of the disease: coronary thrombosis, cirrhosis of the liver, focal softening of the brain due to thrombosis of the feeding arteries and hemorrhages, or myelofibrosis accompanied by anemia, acute leukemia, chronic myeloid leukemia.
As for treatment, in the advanced stage of Vaquez's disease, cytostatic therapy is carried out. If hypoplasia of hematopoiesis occurs against its background, prednisolone, anabolic steroids, vitamins B6 and B12 are prescribed, and blood transfusions are performed. On average, the duration of remission is about two years, during which time, as a rule, maintenance therapy is not required. Depending on the situation, anticoagulants, antiplatelet agents, antihypertensive drugs, etc. are used as symptomatic drugs.
The prognosis is relatively favorable, life expectancy is generally about 10-15 years, and sometimes reaches 20 years. The condition is significantly worsened by the transformation of the disease into myelofibrosis or acute leukemia and the development of vascular complications that threaten death.
Erythremia (polycythemia vera, Vaquez disease) is a hereditary disease of the blood system, occurring mainly in older women.
Increased red blood cell count in polycythemia vera
This pathology is characterized by malignant bone marrow hypertrophy. Most often, this pathology is known to patients as blood cancer (although such a judgment is erroneous) and leads to a progressive increase in the number of blood cells, primarily red blood cells (the number of other elements also increases). As a result of an increase in their number, an increase in hematocrit is observed, which leads to a decrease in the rheological properties of blood, a decrease in the speed of blood flow through the vessels, and, as a consequence, an increase in thrombus formation and a deterioration in tissue supply.
On average, Vaquez disease occurs around the age of 40, and symptoms peak between 60 and 70 years of age. There is a hereditary predisposition to the disease. In the population, erythremia is quite rare - about 30 cases per million population.
Stages and their symptoms
In the early stages of development, the disease does not reveal itself in any way, so the person is not aware of its presence. As it progresses, the first symptoms of erythremia appear.
Initial
Signs of the disease at stage 1:
- Redness of the skin and mucous membranes. The cause of hyperemia lies in the increase in the concentration of red blood cells in the blood. The skin becomes pale pink or red, and in all parts of the body.
- Unpleasant sensations in fingers and limbs. The presence of pain in erythremia is due to impaired circulation in small vessels.
Some patients may experience headaches.
Erythremic
As the disease develops, the next stage of erythremia occurs, the symptoms of which are more pronounced. These include:
- Deterioration in general health. Pathological processes occurring in the body cause weakness, dizziness, increased fatigue, tinnitus and other unpleasant symptoms.
- Erythromelalgia. Accompanied by the appearance of purple spots and burning pain localized in the tips of the fingers and toes.
- Splenomegaly and hepatomegaly (enlarged spleen and liver).
- Increased hyperemia of the skin and mucous membranes, the appearance of swollen veins.
- Gastrointestinal diseases. Trophic processes prevent the normal flow of blood to the tissues, which leads to the development of peptic ulcer of the duodenum and stomach.
- Bleeding (including increased bleeding of gums).
- Skin itching (especially after contact with water).
- Severe joint pain.
- High blood pressure.
Important information: How to treat chronic idiopathic myelofibrosis and its symptoms
Anemic
As Vaquez's disease progresses, symptoms worsen. The patient faces the following pathological conditions:
- Heavy bleeding. They occur spontaneously or as a result of injuries. In some cases, bleeding cannot be stopped within several hours.
- Anemia. Iron deficiency is accompanied by pale skin, deterioration of general health, weakness and dizziness.
- Thrombosis. The formation of thrombotic plaques leads to impaired blood circulation in the vessels of the brain, lower extremities, etc. In such cases, the likelihood of death increases sharply.
Forecast
In order to normalize the volume of the bcc and reduce the risk of thrombotic complications, the first measure is bloodletting. Blood exfusions are carried out in a volume of 200-500 ml 2-3 times a week, followed by replenishment of the removed blood volume with saline solution or rheopolyglucin. Frequent bloodletting may result in the development of iron deficiency anemia. Bloodletting for polycythemia can be successfully replaced by erythrocytepheresis, which allows only the red blood cell mass to be removed from the bloodstream, returning the plasma.
In case of pronounced clinical and hematological changes, the development of vascular and visceral complications, they resort to myelosuppressive therapy with cytostatics (busulfan, mitobronitol, cyclophosphamide, etc.). Radioactive phosphorus therapy is sometimes given. To normalize the state of aggregation of the blood, heparin, acetylsalicylic acid, dipyridamole are prescribed under the control of a coagulogram; for hemorrhages, platelet transfusions are indicated; for urate diathesis - allopurinol.
The course of erythremia is progressive; the disease is not prone to spontaneous remissions and spontaneous cure. Patients are forced to be under the supervision of a hematologist for life and undergo courses of hemoexfusion therapy. With polycythemia there is a high risk of thromboembolic and hemorrhagic complications. The incidence of transformation of polycythemia into leukemia is 1% in patients who have not undergone chemotherapy treatment, and 11-15% in those receiving cytotoxic therapy.
”alt=””>
Since the introduction of radioactive phosphorus into practice, the course of the disease has been benign.
- ↑ Vaquez LH. Sur une forme spéciale de cyanose s'accompagnant d'hyperglobulie excessive et persistante. CR Soc Biol (Paris). 1892;44:384-388.
- ↑ Osler W. Chronic cyanosis, with polycythaemia and enlarged spleen: a new clinical entity. Am J Med Sci. 1903;126:187-201.
- ↑Passamonti F, Malabarba L, Orlandi E, Baratè C, Canevari A, Brusamolino E, Bonfichi M, Arcaini L, Caberlon S, Pascutto C, Lazzarino M (2003). "Polycythemia vera in young patients: a study on the long-term risk of thrombosis, myelofibrosis and leukemia." Haematologica88(1): 13-8. PMID 12551821.
- ↑ Berlin, NI. (1975). "Diagnosis and classification of polycythemias". Semin Hematol12: 339.
- ↑Anía B, Suman V, Sobell J, Codd M, Silverstein M, Melton L (1994). "Trends in the incidence of polycythemia vera among Olmsted County, Minnesota residents, 1935-1989." Am J Hematol47(2):89–93. PMID 8092146.
- ↑ Adamson JW, Fialkow PJ, Murphy S, Prchal JF, Steinmann L. Polycythemia vera: stem-cell and probable clonal origin of the disease. N Engl J Med. 1976;295:913-916
- ↑ Levine RL, Wadleigh M, Cools J, Ebert BL, Wernig G, Huntly BJ, Boggon TJ, Wlodarska I, Clark JJ, Moore S, Adelsperger J, Koo S, Lee JC, Gabriel S, Mercher T, D'Andrea A , Frohling S, Dohner K, Marynen P, Vandenberghe P, Mesa RA, Tefferi A, Griffin JD, Eck MJ, Sellers WR, Meyerson M, Golub TR, Lee SJ, Gilliland DG (2005). "Activating mutation in the tyrosine kinase JAK2 in polycythemia vera, essential thrombocythemia, and myeloid metaplasia with myelofibrosis." Cancer Cell 7(4):387–97. .
- ↑ James C, Ugo V, Le Couedic JP, et al. A unique clonal JAK2 mutation leading to constitutive signaling causes polycythaemia vera. Nature 2005;434:1144-1148 Artikel
- ↑ Torgano G, Mandelli C, Massaro P, Abbiati C, Ponzetto A, Bertinieri G, Bogetto S, Terruzzi E, de Franchis R (2002). "Gastroduodenal lesions in polycythaemia vera: frequency and role of Helicobacter pylori." Br J Haematol 117(1):198–202.
- ↑ Brian J Stuart and Anthony J. Viera "Polycythemia Vera" American Family Physician Vol. 69/No.9: 2139-2144
- ↑ Ayalew Tefferi, Polycythemia Vera: A Comprehensive Review and Clinical Recommendations Mayo Clin Proc. 2003; 78:174-194
- ↑ Ayalew Tefferi, Polycythemia Vera: A Comprehensive Review and Clinical Recommendations Mayo Clin Proc. 2003; 78:174-194
Diagnosis of polycythemia
Communication between a patient and a hematologist begins with a conversation, an external examination, and an anamnesis. The doctor finds out heredity, features of the course of the disease, the presence of pain, frequent bleeding, and signs of thrombosis. During admission, the patient is diagnosed with polycythaemic syndrome:
- purplish-red blush;
- intense coloring of the mucous membranes of the mouth and nose;
- cyanotic (blue) color of the palate;
- change in the shape of the fingers;
- red eyes;
- Palpation reveals an increase in the size of the spleen and liver.
The next stage of diagnosis is laboratory tests. Indicators that indicate the development of the disease:
- an increase in the total mass of red blood cells in the blood;
- increased number of platelets, leukocytes;
- significant levels of alkaline phosphatase;
- a large amount of vitamin B 12 in the blood serum;
- increased erythropoietin in secondary polycythemia;
- decrease in situration (blood oxygen saturation) – less than 92%;
- decrease in ESR;
- increase in hemoglobin to 240 g/l.
For differential diagnosis of pathology, special types of studies and analyzes are used. Consultations with a urologist, cardiologist, and gastroenterologist are provided. The doctor prescribes:
- biochemical blood test - determines the level of uric acid, alkaline phosphatase;
- radiological examination - reveals an increase in circulating red blood cells;
- sternal puncture - collection of bone marrow from the sternum for cytological analysis;
- trephine biopsy - histology of tissue from the ilium, revealing three-line hyperplasia;
- molecular genetic analysis.
Laboratory research
Polycythemia disease is confirmed by hematological changes in blood parameters. There are parameters that characterize the development of pathology. Laboratory data indicating the presence of polycythemia:
| Index | Units | Meaning |
| Hemoglobin | g/l | 180-240 |
| Circulating red blood cell mass | ml/kg | 32-36 |
| Erythrocytosis | cells/liter | up to 6.5-7.5 |
| Leukocytosis | more than 12x109 | |
| Thrombocytosis | over 400x109 | |
| Hematocrit | % | 47-52 |
| ESR | mm/hour | 1-2 |
| Serum vitamin B 12 level | ng | 2200 |
| Alkaline phosphatase | units/l | more than 100 |
| Color indicator | 0,6-0,7 |
Hardware diagnostics
After laboratory tests, hematologists prescribe additional tests. To assess the risk of developing metabolic and thrombohemorrhagic disorders, hardware diagnostics are used. The patient undergoes studies depending on the characteristics of the disease. A patient with polycythemia is given:
- Ultrasound of the spleen, kidneys;
- heart examination - echocardiography.
Hardware diagnostic methods help assess the condition of blood vessels, identify the presence of bleeding and ulcers. Appointed:
- fibrogastroduodenoscopy (FGDS) – instrumental study of the mucous membranes of the stomach and duodenum;
- Doppler ultrasound (USDG) of the vessels of the neck, head, veins of the extremities;
- computed tomography of internal organs.
Treatment of polycythemia
Treatment for secondary polycythemia depends on its cause. Supplemental oxygen may be needed for people with chronic hypoxia. Other treatments may be aimed at treating the cause of polycythemia (for example, appropriate treatment for heart failure or chronic lung disease).
Individuals with primary polycythemia can take several home treatment measures to control symptoms and avoid possible complications.
It is important to drink enough fluids to avoid further blood concentration and dehydration. There are no restrictions on physical activity
If a person has an enlarged spleen, contact sports should be avoided to prevent spleen injury and rupture. It is best to avoid iron supplements as they may contribute to the overproduction of red blood cells.
The mainstay of therapy for polycythemia remains bloodletting (blood donation). The goal of phlebotomy is to maintain hematocrit around 45% in men and 42% in women. Initially, phlebotomy may be necessary every 2 to 3 days, removing 250 to 500 ml of blood each time. Once the goal is achieved, bloodletting may not be performed as often.
A widely recommended drug for the treatment of polycythemia is hydroxyurea. This medication is especially recommended for people at risk of developing blood clots. This drug is especially recommended for people over 70 years of age with an increased level of platelets (thrombocytosis; more than 1.5 million), with a high risk of cardiovascular diseases. Hydroxyurea is also recommended for patients who are unable to tolerate phlebotomy. Hydroxyurea can lower all elevated blood counts (white blood cells, red blood cells, and platelets), while phlebotomy only lowers the hematocrit.
Aspirin is also used in the treatment of polycythemia to reduce the risk of blood clots. However, this drug should not be used by people with any history of bleeding. Aspirin is usually used in combination with bloodletting.
Complications of polycythemia
Frequent monitoring is recommended at the beginning of treatment with phlebotomy until an acceptable hematocrit. Some of the complications of primary polycythemia, as listed below, often require constant medical supervision. These complications include: 1) a blood clot (thrombosis) causing a heart attack, blood clots in the legs or lungs, or blood clots in the arteries. These events are considered the leading causes of death in polycythemia; 2) severe blood loss or hemorrhage; 3) transformation into blood cancer (for example, leukemia, myelofibrosis).
Causes of the disease
True Vaquez disease is a rare type that can be transmitted through an autosomal recessive mode of inheritance. That is, a violation of the production of red blood cells occurs when one recessive gene is transmitted to the child from the mother and father. In this case, tumor growth is associated with the production of cells that do not correspond in size and shape to normal red blood cells. These are the so-called progenitor cells.
Secondary polycythemia occurs under the influence of such provoking factors:
- dehydration of the body, which is caused by severe vomiting, diarrhea and other conditions;
- lack of oxygen. This occurs at high body temperature, hot climate, being in the mountains;
- lung diseases (bronchitis, pneumonia, emphysema);
- increased pulmonary resistance;
- heart failure;
- apnea syndrome;
- impaired blood supply to the kidneys;
- neoplasms in the uterus, kidneys, adrenal glands, liver.
The lack of oxygen and water forces the body to make up for this deficiency through increased synthesis of red blood cells. At the same time, red blood cells continue to fully perform their functions, their size and shape correspond to the norm. Reasons for increased production of the hormone erythropoietin also include kidney cysts, long-term smoking and some other factors.
Lung and heart diseases are becoming common causes of secondary erythremia
Important! Vaquez disease is a tumor disease of hematopoietic tissue that develops at the level of erythropoiesis stem cells.
Symptoms of erythremia
Symptoms of the initial stage
Manifestations of the initial stage of erythremia may be:
- Redness of the skin and mucous membranes. Occurs as a result of an increase in the number of red blood cells in the vessels. Redness is observed in all parts of the body, in the head and limbs, oral mucosa, and eye membranes. At the initial stage of the disease, this symptom may be mild, as a result of which a pinkish tint to the skin is often taken as normal.
- Pain in fingers and toes. This symptom is caused by a violation of blood flow through small vessels. At the initial stage, this is largely due to increased blood viscosity due to an increase in the number of cellular elements. Impaired oxygen delivery to organs leads to the development of tissue ischemia (oxygen starvation), which is manifested by attacks of burning pain.
- Headache. A nonspecific symptom, which, however, can be very pronounced in the initial stage of the disease. Frequent headaches can occur as a result of impaired blood circulation in the small vessels of the brain.
Symptoms of the erythremic stage
as a result, it becomes more viscous. Symptoms of the erythremic stage are:
- redness of the skin;
- erythromelalgia;
- necrosis of fingers and toes;
- increased blood pressure;
- liver enlargement;
- enlarged spleen;
- skin itching;
- increased bleeding;
- joint pain;
- ulcers of the gastrointestinal system;
- symptoms of iron deficiency;
- thrombotic strokes;
- myocardial infarction;
- dilated cardiomyopathy.
Redness of the skin as a result of rupture of small vessels Erythromelalgia Necrosis of the fingers and toes characteristic of this stage of the disease Increased blood pressure OCCU Enlargement of the liver (hepatomegaly) it can retain more than 1 liter of blood, ten or more kilograms arising due to excessive stretching of the liver capsule Enlargement of the spleen (splenomegaly) red blood cells, platelets, leukocytes Skin itching when washing hands, taking a bath, exposure to rain Increased bleeding Pain in the joints of the genetic apparatus of cells uric acid salts urate diathesis develops first in small and then in larger ones Ulcers of the organs of the gastrointestinal system, especially acute or rough, poorly treated abdominal pain with a stomach ulcer with a duodenal ulcer ado 90 – 95% Manifestations of iron deficiency are:
- dry skin and mucous membranes;
- thinning and increased fragility of hair;
- cracks in the corners of the mouth;
- peeling of nails;
- lack of appetite;
- indigestion;
- disturbance of taste and smell;
- decreased resistance to infections.
Thrombotic stroke acute circulatory disorder in a certain area of the brain blood clots depending on the area of the brain in which blood flow is impaired Myocardial infarction heart Dilated cardiomyopathy weakness edema
Symptoms of the anemic stage
The main manifestations of the terminal stage of erythremia are:
- bleeding;
- anemia.
BleedingThe occurrence of bleeding in the terminal stage is due to:
- decreased platelet formation;
- the formation of functionally incompetent platelets.
AnemiaThe causes of anemia in the terminal stage of the disease can be:
- Inhibition of hematopoiesis in the bone marrow. The reason for this is the proliferation of connective tissue (myelofibrosis), which completely displaces hematopoietic cells from the bone marrow. As a result, so-called aplastic anemia develops, manifested by a decrease in the level of red blood cells, platelets and leukocytes.
- Iron deficiency. The lack of this microelement leads to a disruption in the formation of hemoglobin, as a result of which large, functionally incompetent red blood cells enter the blood.
- Frequent bleeding. In this case, the rate of formation of new blood cells is not sufficient to compensate for the losses that occur during bleeding. This situation is further aggravated by iron deficiency.
- Increased destruction of red blood cells. The enlarged spleen retains a large number of red blood cells and platelets, which are destroyed over time, causing the development of anemia.
Clinical manifestations of anemia are:
- pallor of the skin and mucous membranes;
- general weakness;
- increased fatigue;
- feeling of lack of air (especially during physical activity);
- frequent fainting.
Stages of true erythremia
The first stage (initial) of erythremia is characterized by the absence of symptoms. The person feels as usual, the hematopoietic system still functions normally, but the process of increased production of red blood cells is already beginning to gain momentum. At this stage of Vaquez’s disease, even if tests are taken, they will show an insignificant excess of all blood elements, except leukocytes, due to which increased blood supply to all internal organs may be observed.
In this phase of erythremia, both the physician and the patient himself should not underestimate what appear to be completely normal tests at first glance. Knowing about such a pathology of the hematopoietic apparatus as erythremia, it is better to play it safe and, in case of the slightest suspicion, continue research. This will help either dispel suspicions about the presence of Vaquez’s disease, or begin treatment in time to avoid serious consequences and significantly prolong the patient’s life. The initial stage of erythremia with inactivity can last about six years.
Starting from the second stage (A), the person already exhibits symptoms of erythremia. Vaquez's disease can remain in this phase for 10 to 12 years. During this period of erythremia, a person's hematopoietic organs, such as the spleen and liver, gradually grow and increase in size. In blood tests for Vaquez's diseases, iron deficiency is clearly visible.
Thrombosis may occur in the vascular system with erythremia.
Erythremia of the second stage (B) is characterized by a pronounced enlargement of the liver and spleen due to tumor processes. In the bone marrow of Vaquez disease, a lot of scarred tissue can be seen. A patient in this period of progression of Vaquez's disease may notice a tendency to bleeding. And when examining the body, a large number of blood clots are easily detected.
The third stage of erythremia - anemic, occurs if the patient neglects to undergo examination and treatment. The period of its development from the onset of erythremia ranges from 9 to 23 years. In addition to all the above deviations, blood cells gradually cease to cope with the mission assigned to them, which entails many irreversible processes in the human body. One of these processes includes large-scale scarring of brain tissue. At this stage of erythremia, the chances of staying alive are minimal. With constant medical supervision and continuous treatment of Vaquez's disease, it is possible to maintain vital functions in the body for some time. But this condition is unlikely to last long.
Laboratory indicators for polycythemia vera
The number of red blood cells is increased and is usually 6-8 × 1012 /l or more. Hemoglobin increases to 180-220 g/l. The color index is usually less than one (0.7-0.6). The total volume of circulating blood is significantly increased by 1.5-2.5 times, mainly due to an increase in the number of red blood cells. The hematocrit indicator (the ratio of the formed elements of blood and plasma) changes sharply due to an increase in red blood cells and reaches 65% or more. The number of reticulocytes in the blood is increased to 15-20 ‰, which indicates enhanced regeneration of erythrocytes. Polychromasia of erythrocytes is noted; individual erythroblasts can be detected in the smear. The number of leukocytes increased by 1.5-2 times (up to 10-12 × 109 /l). In some patients, leukocytosis can reach even higher numbers. The increase occurs due to neutrophils, the content of which increases to 70-85%. A band or, less commonly, myelocytic shift (shift of the leukocyte formula to the left) is observed. The number of eosinophils increases, and less often basophils. The platelet count is increased to 400-600 × 109 /l, sometimes more. Blood viscosity is significantly increased. ESR is slow (1-2 mm/hour). Uric acid levels increase.
Diagnostics
This pathology is quite easily detected if the doctor conducts a general and biochemical blood test. Vaquez disease is detected due to an increased volume of red blood cells and hemoglobin. In this case, hematocrit values can reach up to 65% or more. Among the additional indicators, it is worth noting the increased concentration of uric acid. Also, in Vaquez disease, a blood test will show an increased volume of young red blood cells.
However, in some situations, experts doubt the accuracy of the diagnosis. To make sure that a person really suffers from polycythemia, it is necessary to perform a brain tap. If there is a suspicion that the disease has been transmitted genetically, appropriate blood testing will be required.
Additionally, the doctor needs to clarify how severe the degree of damage to human organs is. For this purpose, patients are referred to ultrasound, ECG and other diagnostic procedures.