home › Cardiovascular › Aneurysm
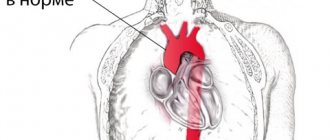
Aneurysm of the splenic artery is a pathology of blood vessels, manifested in the form of deformation and thinning of its walls, the formation of cavities on them filled with blood.
The main danger is rupture of the damaged area, followed by internal bleeding, which can lead to death if qualified medical help is not sought in a timely manner. Interesting! Splenic artery aneurysm (SAA) is the second most common disease after aortic aneurysm. A quarter of the cases described in the medical literature had complications such as rupture and severe bleeding into the abdominal cavity.
Anatomy and causes of aneurysm
The splenic artery originates from the celiac trunk and runs along the pancreas. From the artery in question there are branches that go almost to the bottom of the stomach. Typically, there are three roots of the splenic branch that connect to form one large venous column. It is very dangerous when a disease called aneurysm begins to develop.
Splenic artery aneurysm occurs more often in women and older people. The reason lies in the development of atherosclerosis and poor nutrition over a long period of time. Men are less likely to be affected by the disease, and if cases occur in medicine, it is associated with age. Despite this, young people may also be at risk, and the reasons for this lie in the following:
- If a patient suffers from high pressure in the hepatic vein or spleen, then, most likely, he will begin to develop an aneurysm over time.
- People with damaged inner arterial walls are at risk.
- In women, an aneurysm may develop after a multiple pregnancy.
Only a professional can determine the exact cause and prescribe treatment.
How to recognize pathology?
Most often, patients do not have pronounced symptoms, and the disease can be detected during examination of the abdominal organs. In this regard, it is difficult to quickly understand that a person is sick with a splenic aneurysm. If the disease can be detected in the early stages, then treatment will give the most positive result, but before that it will be important to conduct a full diagnosis of the whole organism. To identify an aneurysm, you should pay attention to the following signs:
- Dull and prolonged pain may occur in the left hypochondrium.
- If the doctor palpates the affected area, the person will feel discomfort.

The branches of the splenic artery can be checked using x-rays, ultrasound and MRI. X-rays are still considered the priority research method, since with the help of this type of research it will be possible to determine the size of the aneurysm and its location.
Main signs and distinctive symptoms
A feature of the disease is the variety of nonspecific manifestations. Some patients are asymptomatic. Signs differ in uncomplicated and complicated cases.

Symptoms in the uncomplicated form:
- Dull periodic or constant pain localized in the left hypochondrium;
- Pain may radiate to the left costovertebral angle;
- The pain increases in proportion to the size of the aneurysm.
The complicated course is acute and can mimic many surgical diseases . The following symptoms are observed:
- Cutting, cramping pain in the abdomen and lower back;
- Fever up to 38 degrees or higher;
- Increased breathing and heart rate;
- “Board-shaped” tense abdomen;
- Bloody stool;
- Local swelling in the lumbar region (appearance of retroperitoneal hematoma);
- Fall in blood pressure.
The complicated course of ASA in pregnant women imitates obstetric pathology:
- Placental abruption;
- Amniotic fluid embolism;
- Uterine rupture.
ASA is characterized by the phenomenon of “incomplete rupture”, observed in 25% of patients. At the time of rupture, only part of the aneurysm is damaged, which leads to a temporary stop of bleeding due to a compressive hematoma. During this period, most patients feel an improvement in their condition, but after 1-2 days the rupture becomes complete, which causes a repeated attack of “acute abdomen” and worsens the prognosis for life.
Types of aneurysm
Doctors distinguish two main types of aneurysm:
- Saccular aneurysms of the splenic arteries, which develop precisely in those places where branches of the artery originate.
- Diffuse aneurysms are located in the area of the main trunk.
It should be noted that aneurysms can be true or false. Most often, one aneurysm develops; multiple lesions are much less common in medicine.
Surgical tactics in a patient with a splenic artery aneurysm
Batrashov V.A., Yudaev S.S., Mirzemagomedov G.A., Sergeev O.G., Khamroev S.Sh.
SURGICAL TREATMENT OF PATIENT WITH SPLENIC ARTERY ANEURYSM
Batrashov V.A., Yudaev S.S., Mirzemagomedov G.A., Sergeev O.G., Khamroev S.Sh.
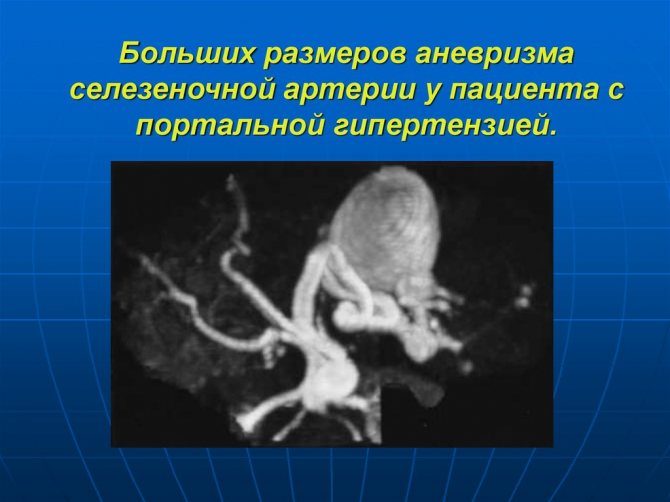
Aneurysms of the visceral branches of the abdominal aorta include aneurysms of the branches of the celiac trunk and renal arteries. The prevalence of this pathology is higher than it seems. Autopsy results showed that aneurysms of the visceral branches are more common than aneurysms of the abdominal aorta. Timely detection of aneurysms of this location is important, since in 25% of cases they are complicated by rupture, and the mortality rate after rupture ranges from 25% to 70%. Aneurysms of the branches of the celiac trunk are twice as common as aneurysms of the renal arteries, and the most common are aneurysms of the splenic artery (up to 60%). Splenic artery aneurysms (SAA) in clinical practice are the third most common intra-abdominal aneurysm, after aortic and iliac aneurysms. The exact prevalence of splenic artery aneurysms is difficult to determine, since most of them are asymptomatic and are diagnosed incidentally. Information on the prevalence of ASA was first reported in 1770 in Brussels based on autopsy results, which reported an incidence of 0.02% to 0.1%. At the same time, in patients with portal hypertension, ASA was detected at autopsy in 7.1% of cases. There is a predominance of the disease in females (male to female ratio 1:4). Aneurysms most often occur in the distal third of the splenic artery (80%), usually they have a saccular structure and are located in the bifurcation area. The pathogenesis of ASA is currently poorly understood and the causes of the disease remain unknown. Typical atherosclerotic changes are often found in aneurysmally dilated areas of arteries, but they are usually secondary. The main predisposing factors for the development of ASA are the presence of pregnancy or portal hypertension with splenomegaly. Less common causes are: pancreatitis and penetrating trauma (they mainly lead to the formation of false ASA), septic embolism, hypertension, fibromuscular dysplasia, congenital or acquired connective tissue diseases. According to the largest studies published to date, Abbas (217 patients over 18 years) and Trastek (100 patients over 20 years), the average diameter of the ACA is 2.2 cm and 2.1 cm, respectively. Giant ACAs (more than 10 cm) are extremely rare. Differential diagnosis is carried out with aneurysms of the renal arteries, calcifications of the lymph nodes, spleen and adrenal gland. ASA is asymptomatic in most cases, but pain may be present in the left hypochondrium or in the epigastric region. Spontaneous rupture of an aneurysm is the most common complication and its risk is much higher in pregnant women and when the aneurysm is larger than 2 cm in diameter. In rare cases, ASA may be complicated by the formation of arteriovenous fistulas, which subsequently lead to portal hypertension, or thrombosis of the splenic artery with the development of splenic infarction. Indications for elective surgical treatment are: aneurysms more than 2 cm in diameter, aneurysms more than 1 cm in pregnant women and women of childbearing age, symptomatic ASA of any size. Patients with aneurysms between 1 and 2 cm in diameter should be monitored and evaluated every 6 months. If a tendency towards growth or the appearance of symptoms is detected, surgical treatment is indicated. It is advisable to use ultrasound diagnostics as a primary diagnosis and follow-up. If there are indications for surgical treatment, it is necessary to perform computed tomography, magnetic resonance imaging or standard angiography. Surgical tactics for ASA are varied and include both standard open operations and minimally invasive laparoscopic and endovascular techniques. Until recently, aneurysm resection, with or without splenectomy, was the mainstay of treatment for ASA. However, in the last decade, endovascular technologies such as aneurysm embolization and stent graft implantation have been introduced as an alternative. Endovascular treatment is characterized by fewer postoperative complications and is currently the treatment of choice in many vascular centers.
Here is a description of a clinical case.
Patient M., 51 years old, sought a consultation at the Department of Vascular Surgery of the National Medical Clinical Center named after. N.I. Pirogov with the results of an ultrasound examination of the abdominal cavity, according to which the presence of an aneurysm of the splenic artery was suspected. At the same time, the patient did not present any complaints, there was no other somatic pathology. An outpatient MSCT of the abdominal aorta was performed: the splenic artery with a diameter of 6.2 mm with smooth contours, tortuous, filled with a contrast agent throughout its entire length, without signs of stenosis. In the distal part of the splenic artery at the level of the upper pole of the left kidney, two aneurysms with parietal calcifications are identified, the first measuring 3.2x2.3x2 cm, the second - 1.6x1.5x1.5 cm. The surrounding fatty tissue is not changed (Fig. 1).
Rice. 1.
Fig 2.
Rice. 3.
The postoperative period was uneventful and the patient had no complaints. She was discharged in satisfactory condition on the 7th day. Currently, the observation period for the patient is 1.5 years. During control ultrasound, the splenic artery is patent, there is no evidence of relapse of the disease. Thus, we present a case of successful surgical treatment of a patient with two splenic artery aneurysms. Considering the high prevalence of ASA and the increased risk of fatal complications associated with aneurysm rupture, surgical tactics must be active. Preference should be given to endovascular methods, but in some cases open surgical treatment is the method of choice.
How does a false aneurysm manifest?
False aneurysm is rare, but is considered the most dangerous. The reason for the appearance of such an aneurysm may not be a deformed splenic artery, but a rupture of the vessel and the formation of a hematoma. The disease can be detected when the patient has bleeding from the upper intestine, and there will be no reason for the manifestation of this symptom.

A doctor can also diagnose a false aneurysm by the appearance of noise; it will intensify during pulsation and listening to noise in the internal organs.
What complications can there be?
The main danger is that the splenic artery may rupture. If the patient is not provided with first aid, this will lead to death. Basically, there are two types of rupture: complete and incomplete. In the first case, the wall of the vessel, which was deformed, is completely damaged, a hematoma is formed, and the person himself experiences severe pain and anemia at this time. If the aneurysm does not rupture completely, a hematoma forms behind the peritoneum and the bleeding stops for a while, and the patient’s blood pressure decreases. In any case, you should not hesitate to go to the hospital, where specialists will be able to diagnose and prescribe the correct treatment.
Diagnostics
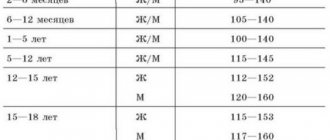
List of basic and additional diagnostic measures: Basic (mandatory) diagnostic examinations performed at the outpatient level: · Ultrasound ultrasound of the abdominal aorta.
Additional diagnostic examinations performed on an outpatient basis: • coagulogram (APTT, INR, Fibrinogen, PT, PTI); • biochemical blood test for lipid spectrum (HDL, LDL, cholesterol, triglycerides); • CTA/MRA of the abdominal aorta and arteries of the lower extremities; • measurement of the ankle-brachial pressure index.
The minimum list of examinations that must be carried out when referred for planned hospitalization: in accordance with the internal regulations of the hospital, taking into account the current order of the authorized body in the field of healthcare.
Basic (mandatory) diagnostic examinations carried out at the inpatient level (in case of emergency hospitalization, diagnostic examinations not carried out at the outpatient level are carried out): · CBC; · OAM; · biochemical blood test (total bilirubin, direct and indirect bilirubin, ALT, AST, total protein, urea, creatinine, electrolytes, blood glucose); · coagulogram (APTT, INR, Fibrinogen, PT, PTI); · UAS of the abdominal aorta and/or arteries of the lower extremities; · blood type and Rh factor; · ECG; · blood testing for HIV using ELISA; · ELISA for hepatitis B, C; · Wasserman reaction; · X-ray of the chest organs in 2 projections; · computed tomography with contrast and or aortography.
Additional diagnostic examinations performed at the hospital level: · CTA/MRA; angiography; chest x-ray; · Ultrasound of the abdominal cavity; · FGDS.
Diagnostic measures carried out at the stage of emergency care: · ECG.
Diagnostic criteria***: Complaints of: · the presence of a pulsating formation in the abdomen, · dull pain in the abdomen; · backache. History: risk factors for the development of aneurysm (smoking, presence of arterial hypertension (blood pressure above 139/89 mm Hg), etc.). Family history: close relatives have heart disease, cases of sudden death.
Physical examination: Palpation: pulsating formation in the epigastrium or mesogastrium. On palpation, an abdominal aortic aneurysm: · dense; · pulsates synchronously with heart contractions; · round or oblong shape; · inactive; · low pain. Auscultation: vascular murmurs (systolic murmur) in the projection of the aneurysm. Pulse measurement: tachycardia at rupture. Examination: presence of a pulsating tumor-like formation in the abdominal cavity.
Laboratory tests: CBC: Anemia (in case of rupture) Blood supply: Dyslipidemia, increased levels of urea, creatinine (in case of renal malperfusion due to disconnection of the aortic lumen)
Instrumental studies: Ultrasound ultrasound: dilation and/or dissection of the aortic lumen, the presence of an aneurysm CT with contrast: dilation and/or dissection of the lumen, the presence of aneurysmal dilatation Vascular angiography: aneurysmal dilatation of the vessel.
Indications for consultation with specialists · consultation with specialists in the presence of other concomitant pathologies.
Treatment
If the patient has been diagnosed with a splenic artery aneurysm, treatment can be carried out depending on the complexity of the disease and its stage. If treatment is started on time, complications can be easily avoided.
Most often, doctors use drug therapy, but surgery remains the most effective method. The operation may be prescribed in the following cases:
- Aneurysm rupture.
- Pathology that was identified at birth.
- When is a large aneurysm diagnosed?
Splenic artery embolization is often used. With the help of such an operation, there is every chance of successfully decompressing the artery, which will dramatically reduce blood flow to the spleen area and lower the pressure in the hepatic artery.

Such treatment can be carried out even in later stages. If surgery is not necessary, the patient should be constantly examined and monitored by the attending physician to prevent its further development.
Conditions for the occurrence of arterial pathology
Most often, a splenic artery aneurysm is diagnosed in patients who suffer from fibromuscular dysplasia, a disease characterized by the replacement of bone tissue with fibrous formations.
Atherosclerosis is also the cause of ASA in older patients. It weakens the walls of blood vessels, reducing their elasticity and tone.
A slightly younger age category of patients is susceptible to aneurysm due to sudden changes in pressure that weaken vascular tissue. Their illness can also be triggered by inflammatory processes in nearby organs, such as chronic pancreatitis or stomach ulcers. A tenth of cases of the disease are the result of exposure to infections.
Another category of patients in which the diagnosis of saccular aneurysm of the splenic artery is quite common is women with many children, whose vascular system was subjected to hormonal and hemodynamic effects (impaired blood flow) during multiple pregnancies.
Important! Whatever the cause of the aneurysm, specialized experts advise solving this problem using a radical method and in the shortest possible time.
Forecast
The splenic artery plays an important role in the human body and an aneurysm prevents it from functioning. The main danger is that the disease may not be detected for a long time, since it is asymptomatic. If acute pain appears in the right hypochondrium, you should immediately consult a doctor. Modern medicine allows you to choose the most appropriate treatment and serves as a preventive measure for the development of more complex other diseases.
If the surgical intervention was successful, then the prognosis for recovery is favorable. But if the patient refuses the operation when the doctor insists on it, then the consequences can be sad, since at any moment the splenic artery can rupture, and this will lead to death. Any negative change in the body should be monitored and constantly monitored by doctors. It is worth paying special attention to the principles of proper nutrition:
- Monitor cholesterol levels in the body.
- Give up all bad habits.
- Measure blood pressure.
It is not recommended to treat such a serious pathology with folk remedies, since it can only worsen the general condition. According to statistics, the threat to life with an arterial aneurysm is only 2%, but among them, almost 25% are fatal. The disease is especially dangerous for pregnant women, as there is a high risk of complications, it is almost 70%.

After operations, patients recover quickly, and the risk of complications is reduced to only 30%. It follows from this that it is necessary to identify the disease in time and begin proper treatment. In this case, the quality of life and its duration of the sick person will not change.