Nursing care for acute cardiovascular failure
Cardiovascular failure in acute form is a severe condition of the human body, in which cardiac functions are disrupted, circulatory deficiency quickly develops with a decrease in the pumping function of one of the ventricles and pumping them with blood fluid. Often the consequence is the death of a person, so when the first symptoms of the disease occur, you need to urgently contact a specialist.
Causes and signs of the disease
Acute heart failure is a severe circulatory disorder that develops with a lack of oxygen. Among the causes are blood loss, failure of the respiratory system, heart disease, heart attack, hypertension, shock from injury, and intoxication with toxic substances.
When the lack of left ventricular blood flow predominates, blood stagnation in the lungs and saturation of the small circle with blood occurs, cardiac asthma and pulmonary edema occur.
With right ventricular failure, blood stagnates in the systemic circle, swelling occurs, blood flow decreases, and organ nutrition is disrupted.
Vascular insufficiency can be provoked by:
- stressful situations;
- physical stress;
- increased blood flow into the pulmonary circle with a sudden adoption of a vertical state.
Clinical manifestations have an initial or erased form: increased shortness of breath, inability to lie down, weakened breathing, coughing, suffocation, wheezing, whistling breathing. Then cardiac asthma and pulmonary edema occur, which, if assistance is not provided in a timely manner, cause death.
Cardiac asthma. During an attack, suffocation, difficulty breathing, a dry cough, and fear of death, which turns into panic, occur. An attack can last from 2-3 minutes to a day. Cardiac asthma is not a disease, but a condition of the body that develops as a result of a heart attack, pneumonia, kidney disease, or a sharp increase in blood pressure.
Pulmonary edema. Symptoms occur more often during night sleep, an attack of lack of air suddenly occurs, shortness of breath is not associated with the load on the heart, the patient is forced to take a sitting position due to lack of oxygen.
What is happening in the body, or signs of pulmonary edema:
- pain behind the sternum, pressing, stabbing;
- rapid breathing with audible bubbling;
- strong heartbeat, it seems to jump out of the chest;
- at first a slight cough, then a cough with strong wheezing, pinkish sputum with foam is released;
- the face is gray or bluish, then this color flows to other parts of the body due to the fact that the blood has accumulated carbon dioxide.
- sticky sweat, swollen veins in the neck, pale skin due to stagnation in the pulmonary circulation;
- there may be a surge in pressure;
- cardiac symptom: pulse is hard to palpate, weak, thread-like;
- confusion of consciousness when assistance is not provided, its absence.
In this case, the patient needs emergency assistance from medical workers, and the further prognosis of the disease, and sometimes the patient’s life, depends on their competent, clear, professional actions. For this purpose, there are special actions of the nurse, approved by the protocol, called the nursing process.
Features of the nursing process
The nursing process is a set of scientific activities and actions of a nurse that are carried out in practice to provide assistance to a sick person, and can be used in different medical institutions. The goals of this assistance are to ensure the necessary quality of life for the ill patient, to make it accessible or as close as possible to the usual way of life.
The nursing process has its own characteristics, which are determined by the problems of the patient, as well as his physical condition. The correct actions of the nurse influence the outcome of the disease.
Activities of the nursing process include several stages, related to the signs of the disease and the problems of the patient with acute failure:
- dyspnea;
- disturbed sleep;
- difficulty in defecation (constipation);
- decrease in physical activity;
- inability to go to the toilet in the usual position;
- frequent urination (taking diuretics).
Examination of the patient
The purpose of the examination is to collect information, which includes asking the patient about past illnesses, to find out when shortness of breath and palpitations appeared, when it intensified, and whether the person can solve these problems himself. You also need to know:
- what kind of pain, intensity, character, location, how long it lasts;
- what kind of cough, when did it appear, dry or with sputum, was there sputum with blood;
- where the swelling is located, at what time it appeared or intensified;
- what medications he uses, their dosage, how they are tolerated;
- features in the diet;
- the problem of inability to take care of oneself;
- how often does he go to the toilet, is there any constipation.
For medical personnel, the causes of organ dysfunction are not as important as the external signs of these disorders. Examination of a patient by a nurse is independent and does not replace medical examination.
Diagnostics
The nurse must convince the patient of the need to reduce physical activity and adhere to the regimen prescribed by the doctor. Together with the patient, choose a position in bed when he will feel the least shortness of breath and the heartbeat will not be felt as much. Carry out an inspection and pay attention to:
- what color is the skin and visible mucous membranes, is there cyanosis;
- what position does he take in bed?
- are there any swellings, their location, color, density;
- measure pulse, respiration, blood pressure.
Nursing diagnosis is the determination of the patient’s problem based on the data collected during the examination period and the requirement for the intervention of a nurse.
When diagnosing, evaluate:
- what is currently bothering the patient;
- those manifestations that can occur due to insufficient care.
In the first place are the problems of a patient with acute insufficiency - pain behind the sternum, swelling, fever. If, for example, the patient considers shortness of breath to be his main ailment, then it is the first priority for resolution.
The nurse needs to work with the patient’s family, talk with the patient, as well as with his relatives and friends. Action planning for acute heart and vascular failure occurs in connection with identified problems and consists of helping the patient and alleviating his ailment. For each problem, a goal and care plan are formulated.
After determining a clear plan, the nurse coordinates her actions with the doctor and patient and begins to implement them.
Possible help from the nurse:
- performing medical procedures;
- prevention of consequences and prevention of complications;
- providing psycho-assistance;
- self-care assistance;
- providing emergency care during exacerbations.
The nurse monitors the effectiveness of the actions taken on a daily basis and, if necessary, adjustments are made in consultation with the doctor.
Life Saving Measures
Emergency care for pathology consists of maintaining vital human functions - breathing and blood circulation. First aid is provided before the arrival of senior medical personnel to prevent the death of the patient.
- Call CPR.
- Give the patient a comfortable sitting position using pillows.
- Increase air access to the room.
- Measure blood pressure, if it increases, give an additional dose of the prescribed drug under the tongue.
- The main symptom is chest pain. When it appears, give nitroglycerin.
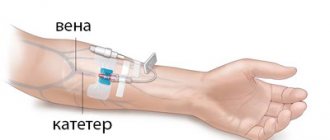
- Apply venous tourniquets. They are applied to both legs and one arm, the other is left for intravenous administration of drugs. Every 15 minutes, transfer one tourniquet from your leg to your free hand.
- To ensure blood flow, if possible, you can take a hot bath for your feet.
The patient must be hospitalized in the cardiac intensive care unit or intensive care unit. Transportation is carried out sitting or in a semi-sitting position, legs down.
Emergency medical measures include the administration of drugs.
- Cardiac glycosides and potassium preparations to help the heart muscle and enhance its contractility.
- Diuretics intravenously to relieve pulmonary circulation.
- For high blood pressure - corticosteroids, for low blood pressure - antihypertensive medications.
- In case of rhythm disturbances, drugs are administered to correct it.
- Use defoamers - inhaling oxygen through an alcohol solution.
Help for symptoms must be provided quickly to avoid death.
Prevention of cardiovascular diseases
Cardiologists, having studied pathological conditions of the heart and blood vessels for many years, have concluded that the main signs causing the disease are predisposing factors:
- hereditary diseases;
- birth defects.
And etiological factors:
- Obesity;
- emotional type of nervous system;
- physical inactivity;
- smoking;
- alcohol consumption;
- hormonal diseases (diabetes mellitus);
- acute and chronic infections;
- elderly age.
Prevention of the disease consists of eliminating all causes leading to the disease. Timely treatment of heart diseases is of great importance. Don’t be lazy and go to the doctor if you experience even minor heart pain. If, despite the prescribed medications, it gets worse over time, you should repeat the visit to specialists; perhaps the treatment requires correction.
Considering that today's patients are mostly knowledgeable people and have a sufficient level of experience in relation to their health, I would like everyone to independently eliminate the causes leading to the disease (fighting smoking and alcohol, excess weight, avoiding stress). You need to think and decide for yourself what kind of lifestyle to lead, so that it is bright, colorful, filled with meaning, and most importantly healthy.
Source: https://MirKardio.ru/dekompensaciya-serdca/sestrinskij-protsess-pri-ostroj-serdechno-sosudistoj-nedostatochnosti.html
Registration procedure
If your loved one has heart failure or is diagnosed with a vascular disease, we can admit them to one of our assisted living facilities, offering ongoing geriatric monitoring and professional care.
To place a disabled or elderly person in a boarding house you will need:
- passport of the guardian and the patient;
- outpatient card, policy and certificate of a disabled person;
- medical certificate confirming the absence of infectious diseases in elderly residents;
- results of fluorography, blood and urine tests.
We accept guests from any region of Russia. The only reason for refusal can only be the diagnosis of a sexually transmitted disease or tuberculosis (in open form). In addition, we do not accept guests with diseases such as alcoholism and drug addiction.
Nursing process in chronic heart failure
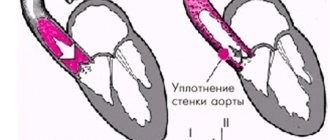
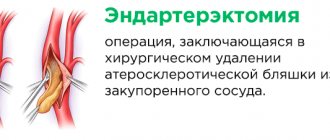
CHF is circulatory failure associated with a decrease in myocardial contractility, as a result of which the supply of organs and tissues with substances necessary for their normal functioning is disrupted. The causes of chronic circulatory failure are diverse: hypertension, heart defects, atherosclerosis of the coronary arteries, anemia, intoxication, infections, endocrine diseases.
Patient problems in the nursing process for chronic heart failure:
A. Existing (present) : Shortness of breath (during physical activity and at rest). Heartbeat. Edema. Cough. Hemoptysis. Sleep disturbance. Constipation. Decreased physical activity.
Difficulties in carrying out physiological functions in the usual position. The need to frequently visit the toilet due to frequent urination (when taking diuretics). Lack of knowledge about your health. Risk of falling.
B. Potential :
Risk of developing bedsores. Risk of developing congestive pneumonia. Risk of overdose of drugs (cardiac glycosides). Loss of social status and role in society and family.
Possibility of changing profession, disability.
Collection of information during the initial examination:
A.
Questioning the patient about : – previous diseases; – conditions of shortness of breath and palpitations or their intensification, whether he can independently solve these problems; – the patient’s current physical activity; - the nature of the cough (dry or with sputum - its nature, whether there was hemoptysis), the time of cough onset; – the presence of edema, places of its localization, at what time of day they appear or intensify; – taking medications: cardiac glycosides, diuretics (regularity of taking them, dose, tolerance); – nutritional characteristics, water regime; – problems associated with the impossibility or insufficiency of self-care: – problems associated with disruption of physiological functions (frequent urination when taking diuretics, constipation).
B. Examination of the patient :
The color of the skin and visible mucous membranes, the presence of cyanosis. Position in bed. Presence of edema (localization, density, color). Counting the frequency of respiratory movements. Heart rate study.
Blood pressure measurement.
Nursing interventions, including work with the patient's family:
1. Together with the patient, choose a position in bed in which shortness of breath and palpitations will significantly decrease or disappear. 2. Convince the patient to reduce physical activity and follow the regimen prescribed by the doctor. 3. Ensure frequent ventilation of the room where the patient is located. 4.
Conduct a conversation with the patient/family and loved ones about the need to strictly follow a diet with limited salt and liquid. 5. Support the patient's efforts to change his diet and physical activity. 6. Monitor respiratory rate, pulse and blood pressure.
If the pulse slows below normal (overdose of cardiac glycosides), immediately notify the enemy. 7. Perform oxygen therapy as prescribed by the doctor. 8. Monitor the dynamics of edema and the condition of the skin in the area of edema. 9. Recommend wearing socks and sports pants with loose elastic bands. 10.
As prescribed by the doctor, determine daily diuresis and water balance. 11. If necessary, ensure comfortable delivery of physiological goods. 12. Help the patient with self-care (hygienic care, feeding, etc.). 13. Monitor the patient’s body weight. 14. Inform the patient about the action of cardiac glycosides.
diuretics prescribed by a doctor, rules for taking them, tolerability, side effects, signs of an overdose of cardiac glycosides (nausea, anorexia); control their intake. 15. Prevent bedsores, congestive pneumonia, constipation (as prescribed by a doctor, administer a cleansing enema). 16.
Provide the patient with sufficient sleep (ventilate the room before bedtime; the last meal should be 3-4 hours before bedtime).
Educate the patient/family:
– determine the frequency of respiratory movements; – examine pulse and heart rate; – measure blood pressure; – determine daily diuresis and water balance; – prevention of bedsores; – prevention of congestive pneumonia; – prevention of constipation;
– administering a cleansing enema for persistent constipation.
Source: https://sestrinskoe-delo.ru/sestrinskoe-delo-v-terapii/sestrinskiy-protsess-pri-chronicheskoy-serdechnoy-nedostatochnosti