Heart failure in a child - what kind of disease is it, what are its symptoms and how to treat it? Read about all this in the article.
The disease often leads to disability, deterioration in the quality of life, and the death of the child. However, it is worth noting that with timely comprehensive treatment, the prognosis for recovery is very good, since the existing disease can be completely cured. In order to recognize the presence of the disease in time, it is important to know exactly what symptoms are characteristic of it. When the first signs appear, you should immediately consult a doctor for diagnosis and treatment.
Features of the disease
If heart pathology is detected in a timely manner in newborns and older children, they can be saved and complications can be prevented. However, in most cases, dangerous symptoms go unnoticed for a long period of time, and then the child may develop heart failure. This is a condition in which, as a result of reduced contractility, blood circulation inside and outside the heart is disrupted. In the presence of such a pathology, the entire body suffers.
View gallery
A chronic form of insufficiency often occurs in children, developing as a result of the presence of various pathologies of the heart and blood vessels. The main danger of such a pathological condition is that it can occur latently, therefore, without timely diagnosis, heart failure in a child goes into a particularly severe, life-threatening stage.
In newborns, it is mainly provoked by congenital heart defects, especially if they are severe and combined. In older children, a similar problem often occurs as a result of various injuries that damage the heart muscle.
Acute heart failure in children
Depending on the type of hemodynamics and some features of pathogenesis, the following clinical variants of acute heart failure (AHF) are distinguished:
- with a stagnant type of hemodynamics: right ventricular (venous stagnation in the systemic circulation);
- left ventricular (cardiac asthma, pulmonary edema);
CARDIOGENIC SHOCK (low cardiac output syndrome)
Shock is an acutely developing, life-threatening pathological process characterized by a progressive decrease in tissue perfusion, severe disturbances in the functioning of the central nervous system, blood circulation, respiration and metabolism.
Cardiogenic shock is a clinical syndrome characterized by arterial hypotension and signs of a sharp deterioration in microcirculation and tissue perfusion, including blood supply to the brain and kidneys (lethargy or agitation, drop in diuresis, cold skin covered with sticky sweat, pallor, marbled skin pattern); sinus tachycardia is compensatory in nature.
In addition to cardiogenic shock, possible causes of shock may include:
- A decrease in total blood volume (hypovolemic shock) due to bleeding or dehydration due to losses from the gastrointestinal tract (vomiting, diarrhea), polyuria, burns, etc. The main pathogenetic mechanism is insufficient cardiac preload due to a deficiency of venous inflow.
- Deposition of blood in the venous pools (distributive or vasogenic shock) during anaphylaxis, acute adrenal insufficiency, sepsis, neurogenic or toxic shock. The leading pathogenetic mechanism is insufficiency of cardiac afterload.
Low cardiac output (cardiogenic shock) develops as a result of failure of the pumping function of the heart (acute myocardial ischemia, infectious and toxic carditis, cardiomyopathies), as well as as a result of obstruction of the venous inflow to the heart or cardiac output (obstructive shock) in diseases of the pericardium (pericardial tamponade), tension pneumothorax, acute obstruction of the atrioventricular orifice by atrial myxoma, rupture of chords, heart valves, massive pulmonary embolism, etc. Pericardial tamponade and obstruction of the atrioventricular orifice require immediate surgical intervention; drug therapy in these cases can only worsen the situation.
A special clinical variant of cardiogenic shock is arrhythmic shock, which develops as a result of a drop in cardiac output due to tachycardia/tachyarrhythmia or bradycardia/bradyarrhythmia; After stopping the rhythm disturbance, adequate hemodynamics are quickly restored.
With the development of low cardiac output syndrome, a pain syndrome is observed, manifested by severe anxiety in the child, followed by lethargy. A drop in blood pressure, threadlike pulse, tachycardia, “marble” pallor of the skin, collapsed peripheral veins, sticky cold sweat, acrocyanosis, and oligoanuria are noted.
The course of cardiogenic shock is often accompanied by the development of pulmonary edema, mesenteric ischemia, disseminated intravascular coagulation syndrome, and renal failure.
Cardiogenic shock at the prehospital stage is diagnosed based on:
- progressive drop in systolic blood pressure;
- decrease in pulse pressure - less than 20 mm Hg. Art.;
- signs of impaired microcirculation and tissue perfusion - a drop in urine output of less than 20 ml/h, cold skin covered with sticky sweat, pallor, marbled skin pattern, in some cases - collapsed peripheral veins.
Treatment of cardiogenic shock
- Elimination of the main cause: relief of heart rhythm disturbances and pain. In case of severe pain, administer fentanyl at a dose of 0.01 mg/kg or 1% promedol at a dose of 0.1 ml/year of life intravenously. For children in the first two years of life, prescribe non-narcotic analgesics: baralgin or a 50% analgin solution at a dose of 0.1-0.2 ml/year of life. In the presence of psychomotor agitation, prescribe a 0.5% solution of diazepam (Seduxen, Relanium) at a dose of 0.1-0.3 mg/kg intravenously.
- In the absence of signs of congestive heart failure (shortness of breath, moist rales in the posterior lower parts of the lungs), the patient must be placed in a horizontal position.
- If the clinical picture of shock is extensive and there are no signs of congestive heart failure, therapy should begin with intravenous fluid administration (infusion therapy to increase preload) under the control of blood pressure, heart rate, respiratory rate and auscultation of the lungs. Rheopolyglucin is administered at a dose of 5-8 ml/kg + 10% glucose solution and 0.9% sodium chloride solution at a dose of 50 ml/kg in a ratio of 2 to 1 with the addition of cocarboxylase and 7.5% potassium chloride solution at a dose of 2 mmol/ kg body weight.
- An increase in cardiac output is achieved:
- administration of dopamine (6-9 mg/kg/min), which has a positive inotropic effect. Dopamine, an agonist of dopamine receptors, causes excitation of α- and β-adrenergic receptors, increases the release of norepinephrine into the synaptic cleft, increases the strength of heart contractions and cardiac output, the effect of the drug on heart rate is insignificant. The drug promotes the redistribution of total vascular peripheral resistance, causing dilatation of the renal and mesenteric vessels and a vasoconstrictor effect; improved renal perfusion helps to increase diuresis. Dopamine infusion is carried out in the intensive care unit under continuous monitoring using a dispenser for 24-48 hours. The effect occurs after 5 minutes, its peak after 5-7 minutes. Considering the possible tachycardic and arrhythmogenic effect of dopamine, the drug is used in very short courses, only in extremely severe cases and with complete depletion of the sympathetic-adrenal system, with an increase in AHF to degree III.
- administration of drugs with a positive chronotropic effect: adrenaline, norepinephrine (0.05-0.2 mcg/kg/min).
- The lack of effect from dopamine or the impossibility of its use due to tachycardia, arrhythmia is an indication for the addition or monotherapy with dobutamine, which, unlike dopamine, has a more pronounced vasodilatory effect and a less pronounced ability to cause an increase in heart rate and arrhythmia.
250 mg of the drug is diluted in 500 ml of a 5% glucose solution (1 ml of the mixture contains 0.5 mg, and 1 drop - 25 mcg of dobutamine); in monotherapy, it is prescribed at a dose of 2.5 mcg/kg/min, increasing every 15-30 minutes by 2.5 mcg/kg/min until an effect, side effect is obtained, or a dose of 10 mcg/kg/min is achieved, and with a combination of dobutamine with dopamine - in maximum tolerated doses. Dobutamine is a β1-adrenergic agonist, has a positive inotropic effect on the heart, moderately increases heart rate, as well as stroke and cardiac output, reduces the total peripheral and vascular resistance of the pulmonary circulation, while systemic blood pressure tends to increase, reduces the filling pressure of the ventricles of the heart, increases coronary blood flow, improves oxygen supply to the myocardium. Increased cardiac output improves renal perfusion and increases sodium and water excretion. The drug is used for reduced renal blood flow and cardiac output, moderate hypotension. Dobutamine is not prescribed for systolic blood pressure <70 mm Hg. Art. - If an increase in the volume of administered fluid does not lead to an increase in cardiac output (with high central venous pressure and no effect of drugs with a positive inotropic effect), the reason for its decrease may be either a large afterload, to reduce which sodium nitroprusside is used (0.5-0. 8 mcg/kg/min); or a decrease in myocardial contractility, which is an indication for the administration of cardiac glycosides.
- If there are signs of congestive heart failure and in the case of using inotropic drugs from the group of pressor amines, the administration of peripheral vasodilators - nitrates (nitroglycerin) is indicated.
- Administer a 3% solution of prednisolone at a dose of 3-5 mg/kg intravenously.
- In the absence of contraindications, heparin is prescribed to correct microcirculatory disorders, especially with long-term intractable shock.
- Oxygen therapy.
- Admission to the intensive care unit.
ACUTE CONGESTIVE HEART FAILURE
There are 3 stages of development of acute congestive heart failure.
Stage I:
- decrease in cardiac output, hypervolemia, signs of fluid stagnation in one or both circulations.
- tachycardia and shortness of breath at rest, not consistent with fever,
- change in the ratio between h.s.s. and ch.d. (in children of the first year of life - more than 3.5:1; older than one year - more than 4.5:1),
- increase in liver size,
- periorbital edema (mainly in the first year),
- swelling of the neck veins and puffiness of the face,
- cyanosis,
- bronchospasm,
- silent crepitating or fine rales in the lower parts of the lungs,
- accent of the second tone on the pulmonary artery,
- muffled heart sounds.
Stage II:
- general fluid retention with oliguria or anuria occurs,
- peripheral edema appears in the places most distant from the heart (on the lower extremities, buttocks, in the sacral area),
- pulmonary edema is possible.
Stage III:
- hyposystolic form with the development of arterial hypotension against the background of a clinic overload of the pulmonary circle,
- a decrease in the background of total stagnation, first in systolic and then in minimum pressure,
- against the background of deafness of tones - a significant expansion of the boundaries of the heart.
Directions for treatment of acute heart failure
- Methods that enhance myocardial contractility due to cardiotonic and cardiac stimulating effects:
- cardiac glycosides (strophanthin, korglykon, digoxin),
- pacemakers (dopamine, dobutrex, isadrin).
- Combating hypervolemia and edema:
- diuretics (Lasix 2-5 mg/kg),
- restriction of drinking regime.
- Reducing vascular resistance while improving peripheral and coronary circulation:
- vasodilators (nikoshpan, complamin, papaverine),
- disaggregants.
- Cardiotrophic therapy, oxygen (panangin, KKB, glucose).
At the prehospital stage, emergency care includes:
at stage I AHF:
- position of the patient with legs down;
- vasodilators - papaverine;
- lasix 2-4 mg/kg;
- hospitalization in a specialized department.
at stage II AHF:
- position of the patient with legs down;
- access to fresh air;
- lasix 2-4 mg/kg;
- calling the intensive care team.
at stage III AHF:
- position of the patient with legs down;
- access to fresh air;
- prednisolone 5 mg/kg;
- calling the intensive care team.
ACUTE CONGESTIVE LEFT VENTRICULAR FAILURE
Acute left ventricular failure is associated with a sharp decrease in the pumping function of the left ventricle and a rapid increase in blood stagnation in the lungs.
The main causes of acute left ventricular failure:
- Myocardial diseases in the stage of decompensation (myocarditis, cardiomyopathies of various origins).
- Hemodynamic volume overload of the left chambers of the heart with heart defects: atrial and ventricular septal defects; open aortic duct; insufficiency of the aortic and mitral valves, aortic stenosis, coarctation of the aorta, etc.
- Hemodynamic pressure overload of the left heart with heart defects: coarctation of the aorta; stenosis of the mitral and aortic valves; hypertrophic cardiomyopathy; heart tumors; malignant arterial hypertension.
- Heart rhythm disturbances (paroxysmal tachycardia, atrial fibrillation).
Acute left ventricular failure is characterized by a sequential course of stages : interstitial and alveolar. Clinically, it is manifested by the syndromes of cardiac asthma and pulmonary edema. Cardiac asthma is considered to be the initial stage of pulmonary edema. When it occurs, fluid leaks from the vascular bed into the interstitial (interstitial) tissue, i.e., interstitial pulmonary edema occurs. With pulmonary edema, fluid from the interstitial space moves into the alveoli. In this regard, this phase of acute left ventricular failure is called the alveolar stage.
Cardiac asthma is manifested by attacks of suffocation, which are often preceded by physical and emotional stress. Manifests with paroxysmal shortness of breath, painful suffocation and orthopnea, occurring more often at night (predawn) hours; sometimes - Cheyne-Stokes breathing, cough (initially dry, and then with sputum, which does not bring relief), later - foamy sputum, often pink, pallor, acrocyanosis, hyperhidrosis and is accompanied by excitement, fear of death. The child is restless, complains of tightness in the chest, lack of air. Takes a forced position: sits with legs down. In case of acute congestion, moist rales may not be heard at first, or a meager amount of fine bubbling rales is detected over the lower parts of the lungs; swelling of the mucous membrane of small bronchi can manifest itself as a moderate picture of bronchial obstruction with prolongation of exhalation, dry wheezing and signs of pulmonary emphysema.
A differential diagnostic sign that allows one to differentiate this condition from bronchial asthma can be the dissociation between the severity of the patient’s condition and (in the absence of pronounced expiratory dyspnea, as well as “silent zones”) the paucity of the auscultatory picture. Possible acute expansion of the heart to the left, the appearance of a systolic murmur at the apex of the heart, a proto-diastolic gallop rhythm, as well as an emphasis on the second tone on the pulmonary artery and other signs of load on the right heart, up to the picture of right ventricular failure. Blood pressure can be normal, high or low. A constant symptom is increasing tachycardia with a change in the ratio of heart rate and respiratory rate of more than 3:1. The attack lasts from several minutes to several hours. Cardiac asthma does not always develop into a detailed picture of pulmonary edema, especially if treatment measures are timely.
With the development of cardiogenic pulmonary edema, anxiety is noted at the beginning, children may rush about in bed, and subsequently there may be a disturbance of consciousness. The skin is first pale, and then bluish, covered with cold, sticky sweat. When coughing, foamy sputum of a single color is released, streaks of blood are possible. Breathing is noisy, bubbling. A large number of moist, small- and medium-bubble rales are heard over the lungs, appearing first paravertebrally, and then over all other parts of the chest. The development of oligoanuria is possible.
Differential diagnosis in the interstitial stage is carried out with an attack of bronchial asthma, and in the alveolar stage - with non-cardiogenic pulmonary edema (adult respiratory distress syndrome). The latter is found in pediatric practice much more often than cardiogenic, and develops with toxicosis, disseminated intravascular coagulation syndrome, all types of shock, drowning, poisoning with gasoline, kerosene, turpentine, etc.
Treatment of acute congestive left ventricular failure
- Treatment of acute congestive heart failure begins with giving the patient an elevated position (with an unexpressed picture of congestion - an elevated head end, with extensive pulmonary edema - a sitting position with lowered legs); These measures are not performed in cases of severe arterial hypotension. Ensure patency of the upper respiratory tract by removing mucus from the mouth with a gauze swab.
- A universal pharmacological agent for acute congestive heart failure is furosemide (Lasix), which, due to venous vasodilation within 5-15 minutes after administration, causes hemodynamic unloading of the myocardium, which increases over time due to the diuretic effect that develops later. Furosemide is administered intravenously as a bolus and is not diluted; the dose of the drug is 2-4 mg/kg.
- Severe congestion in the pulmonary circulation in the absence of arterial hypotension is an indication for intravenous drip administration of nitroglycerin. The use of nitrate drugs requires careful monitoring of blood pressure and heart rate. Nitroglycerin is prescribed at a dose of 0.1-0.7 mcg/min. Contraindications to the use of nitrates are arterial hypotension and hypovolemia, pericardial constriction and cardiac tamponade, pulmonary artery obstruction, and inadequate cerebral perfusion.
For mild congestion in the lungs, nitroglycerin can be prescribed ¼ -1 tablet under the tongue.
- Modern methods of drug treatment have minimized the importance of applying venous tourniquets to the extremities; however, if adequate drug therapy is not possible, this method of hemodynamic unloading not only can, but should be used, especially with rapidly progressing pulmonary edema. Tourniquets are applied to 2-3 limbs (upper third of the shoulder or thigh) for 15-20 minutes, with the procedure repeated after 20-30 minutes. An indispensable condition in this case is the preservation of the pulse in the artery distal to the tourniquet.
- Persistent signs of pulmonary edema with stabilization of hemodynamics may indicate an increase in membrane permeability, which requires the administration of glucocorticoids to reduce permeability (prednisolone 2-3 mg/kg).
- A means of combating foaming during pulmonary edema are “defoamers” - substances that ensure the destruction of foam by reducing surface tension. The simplest of these means is alcohol vapor, which is poured into a humidifier (33%), passing oxygen through it, supplied to the patient through a nasal catheter or breathing mask at an initial rate of 2-3 l/min, and after a few minutes - at a rate of 6-8 l/min.
- With low blood pressure and hypokinetic variant (myocardial failure), cardiotonic drugs are indicated: cardiac glycosides (strophanthin, korglykon, digoxin, etc.), sympathomimetic amines (dopamine 2-5 mcg/kg/min.), polarizing mixture (10% solution glucose 5 ml/kg, panangin 0.5-1.0 ml/year of life, insulin - 1 unit per 5 g of dry glucose) intravenous drip.
For the treatment of decompensated heart failure with the development of acute left ventricular failure and pulmonary edema, intravenous drip administration of short-acting cardiac glycosides, namely strophanthin or corglycon, is necessary. The drugs are administered intravenously slowly; the dosage is presented in the table.
| Age | Strophanthin | Korglykon | ||
| release form | Dose | release form | Dose | |
| 1-6 months | 1 ml 0.025% or 0.05% solution | 0.1 ml 0.025% solution | 1 ml 0.06% solution | 0.1 ml |
| 1-3 years | 0.1 ml 0.05% solution; 0.2 ml 0.025% solution | 0.2 ml | ||
| 4-7 years | 0.2 ml 0.05% solution; 0.3 ml 0.025% solution | 0.3 ml | ||
| over 7 years old | 0.3 ml 0.05% solution; 0.6 ml 0.025% solution | 0.6-0.8 ml | ||
- In case of hyperkinetic type of blood circulation with a persistent increase in blood pressure, cardiac glycosides are not indicated; ganglion blockers are prescribed (5% pentamine solution for children 1-3 years old at a dose of 1-3 mg/kg, over 3 years old - 0.5-1 mg/kg or 2% benzohexonium solution for children 1-3 years old at a dose of 0.5-1 .5 mg/kg, over 3 years - 0.25-0.5 mg/kg), droperidol (0.25% solution at a dose of 0.1 ml/kg). The drugs are used once; a reduction in blood pressure by no more than 40% from the initial level is permissible.
- In the absence of contraindications, heparin is indicated for the correction of microcirculatory disorders, especially with long-term intractable pulmonary edema.
- If the condition is severe and there is a risk of cardiac and respiratory arrest, tracheal intubation and transfer to mechanical ventilation are indicated. Urgent hospitalization in the intensive care unit or intensive care unit. Transportation is carried out in a semi-sitting position against the background of ongoing oxygen therapy.
ACUTE RIGHT VENTRICULAR FAILURE
Acute right ventricular failure is the result of a sharp overload of the right parts of the heart. It occurs with thromboembolism of the pulmonary artery trunk and its branches, congenital heart defects (pulmonary stenosis, Ebstein's anomaly, etc.), severe attack of bronchial asthma, etc.
It develops suddenly: a feeling of suffocation, tightness behind the sternum, pain in the heart area, and severe weakness instantly appear. Cyanosis quickly increases, the skin becomes covered with cold sweat, signs of increased central venous pressure and stagnation in the systemic circulation appear or intensify: the neck veins swell, the liver quickly enlarges, which becomes painful. The pulse is weak and increases significantly. Blood pressure is reduced. Edema may appear in the lower parts of the body (with prolonged horizontal position - on the back or side). Clinically, it differs from chronic right ventricular failure by intense pain in the liver area, aggravated by palpation. Signs of dilatation and overload of the right heart are determined (expansion of the borders of the heart to the right, systolic murmur over the xiphoid process and protodiastolic gallop rhythm, emphasis of the second tone on the pulmonary artery and corresponding ECG changes). A decrease in left ventricular filling pressure due to right ventricular failure can lead to a drop in left ventricular minute volume and the development of arterial hypotension, up to a picture of cardiogenic shock.
With pericardial tamponade and constrictive pericarditis, the pattern of large circle congestion is not associated with insufficiency of myocardial contractile function, and treatment is aimed at restoring diastolic filling of the heart.
In acute congestive right ventricular failure, the following have diagnostic value:
- swelling of the neck veins and liver;
- Kussmaul's sign (swelling of the jugular veins on inspiration);
- intense pain in the right hypochondrium;
- ECG signs of acute overload of the right ventricle (type SI-QIII, increasing R wave in leads V1,2 and formation of a deep S wave in leads V4-6, ST depression in I, II, aVL and ST elevation in III, aVF, as well as in leads V1, 2; the formation of right bundle branch block, negative T waves in leads III, aVF, V1-4) and signs of overload of the right atrium (high pointed waves PII, III) are possible.
Treatment of acute congestive right ventricular failure
Treatment is carried out taking into account the cause contributing to the development of acute overload of the right ventricle.
- Give the patient an elevated body position in bed.
- Oxygen therapy.
- Administer a 2% solution of Lasix at a dose of 2-3 mg/kg intravenously.
- Administer a 3% solution of prednisolone at a dose of 3-5 mg/kg intravenously.
- Introduce a 2.4% solution of aminophylline at a dose of 2-4 mg/kg intravenously in a slow stream in 20-40 ml of saline solution.
- In case of pain and severe psychomotor agitation, administer a 1% solution of promedol at a dose of 1 mg/year of life.
- For congenital heart disease, cardiac glycosides are used in small doses and diuretics intravenously.
- Patients with pulmonary embolism are prescribed heparin (20-400 units/kg per day intravenously 4-6 times a day under the control of a coagulogram) and fibrinolytic agents (streptokinase), dipyridamole (5-10 mg/kg intravenously).
- Peripheral vasodilators (nitroglycerin and nitroprusside intravenously or nitroglycerin orally) are effective, which, by promoting blood deposition in the periphery, can improve right ventricular function.
The combination of acute congestive right ventricular and congestive left ventricular failure serves as an indication for therapy in accordance with the principles of treatment of the latter.
When acute congestive right ventricular failure and small output syndrome (cardiogenic shock) are combined, the basis of therapy is inotropic agents from the group of pressor amines.
HYPOXEMIC CRISIS (STROPHENIC-CYANOTIC ATTACK)
A shortness of breath-cyanotic attack is an attack of hypoxia (paroxysmal shortness of breath with severe cyanosis) in a child with blue-type congenital heart disease, most often with tetralogy of Fallot. It occurs as a result of a sudden decrease in pulmonary blood flow associated with spasm of the outflow tract of the right ventricle of the heart, an increase in blood discharge from right to left and hypoxemia in the systemic circulation.
Attacks of hypoxia develop mainly in young children - from 4-6 months. up to 3 years. Provoking factors for a dyspnea-cyanotic attack can be psycho-emotional stress, increased physical activity, intercurrent diseases accompanied by dehydration (fever, diarrhea), iron deficiency anemia, neuro-reflex excitability syndrome with perinatal damage to the central nervous system, etc.
A dyspnea-cyanotic attack is characterized by a sudden onset. The child becomes restless, moans, cries, and cyanosis and shortness of breath increase. Takes a forced position - lies on its side with its legs brought to the stomach or squats. On auscultation of the heart there is tachycardia, a decrease in intensity or disappearance of systolic murmur over the pulmonary artery. The duration of a hypoxic attack ranges from several minutes to several hours. In severe cases, convulsions, loss of consciousness, even coma, and death are possible. Hypoxemia and acidosis.
Emergency care for dyspnea-cyanotic attack
- Calm the child, unbutton tight clothes. Lay on your stomach in a knee-elbow position (with your legs brought to your chest and bent at the knee joints).
- Inhale humidified oxygen through a mask at a rate of 5-8 l/min.
- Administer cordiamin at a dose of 0.02 ml/kg subcutaneously or intramuscularly.
- In case of a severe attack, provide access to the vein and prescribe:
- 4% sodium bicarbonate solution at a dose of 4-5 ml/kg (150-200 mg/kg) IV slowly over 5 minutes; you can repeat the administration in half the dose after 30 minutes and over the next 4 hours under the control of blood pH;
- 1% solution of morphine or promedol at a dose of 0.1 ml/year of life subcutaneously or intravenously (children over 2 years old in the absence of symptoms of respiratory depression);
- if there is no effect, introduce carefully (!) a 0.1% solution of obsidan at a dose of 0.1-0.2 ml/kg (0.1-0.2 mg/kg) in 10 ml of 20% glucose solution IV slowly ( at a rate of 1 ml/min or 0.005 mg/min).
- If cyanosis persists, in order to increase the volume of blood volume, fluids are administered (rheopolyglucin 10-15 ml/kg) or red blood cells are transfused (at a dose of 3-5 ml/kg when hemoglobin decreases below 150 g/l).
- For convulsions, administer a 20% solution of sodium hydroxybutyrate 0.25-0.5 ml/kg (50-100 mg/kg) intravenously in a slow stream.
- In case of an intractable attack and the development of hypoxemic coma, transfer to mechanical ventilation and emergency palliative surgery (aortopulmonary anastomosis) are indicated.
- Cardiac glycosides and diuretics are contraindicated!
- Hospitalization of children with dyspnea-cyanotic attacks is indicated if therapy is ineffective. If first aid measures are successful, the patient can be left at home with a recommendation for the subsequent use of anaprilin at a dose of 0.25-0.5 mg/kg per day.
Classification
According to the classification, heart failure in a child can be acute or chronic. Acute is characterized by the fact that it develops rapidly as a result of impaired myocardial contractility and a simultaneous decrease in minute and systolic blood volume. Clinically, the symptoms are extremely severe: acute renal failure, pulmonary edema, cardiogenic shock.
The chronic form of the disease usually develops as a result of a disease of the cardiovascular system, which leads to a decrease in the pumping function of the human heart. Manifested by fatigue and shortness of breath.
In addition, a distinction is made between diastolic and systolic forms of the disease.
Pathology can also be left ventricular and right ventricular. The left ventricular form is characterized by the fact that it affects the pulmonary circulation and is often called pulmonary. It manifests itself in the form of cyanosis, shortness of breath and cough, and in more dangerous cases, pulmonary edema is observed.
In the right ventricular form, the right side of the heart and the systemic circulation suffer, which is why it is called cardiovascular failure. In children with this pathology, the spleen and liver become enlarged, and swelling also occurs.
Classification and causes
| Classification | Form | |
| By localization | left ventricular | right ventricular |
| According to the form of flow | acute | chronic |
| By degree of compensation | compensated | decompensated |
There are two forms of the disease:
- Chronic (CHF) – progresses over a long period of time with characteristic symptoms.
- Acute (AHF) – has a rapid development with very severe manifestations.
There is no generally accepted systematization of heart failure in global pediatrics.
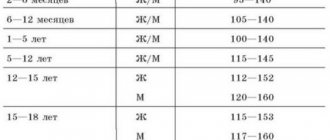
Classification developed by Belokon N.A. back in 1987, to this day it is among the most practical. With its help, chronic heart failure is diagnosed in children, divided into 4 degrees of severity and makes it possible to differentiate approaches to their treatment.
Based on the Belokon classification, failure of the right or left heart is assessed separately; There is no separation only in the initial phase. At the first stage, the patient has no symptoms at rest, but during activity they manifest themselves in the form of shortness of breath and tachycardia.
The following clinical manifestations are characteristic of left ventricular failure at different stages:
- stage 2A – the number of cardiac contractions per minute is 15-30% more, the sum of respiratory cycles increases by 30-50%;
- stage 2B - the number of cardiac contractions increases from 30% to 50% per minute, inhalation and exhalation is carried out 50-70% times more often (bluish coloration of the skin, moist fine bubbling rales, persistent cough are possible);
- stage 3 – the number of heart compressions per minute increases to 50-60%, and breathing to 70-100% (the patient’s condition is the same as before pulmonary edema).
Right ventricular failure is expressed as follows:
- stage 2A – the lower edge of the liver protrudes 2-3 cm beyond the border of the costal arch;
- stage 2B – the liver is extended from 3 to 5 cm beyond the costal arch; there is swelling with looseness of the face and neck, swelling of the veins;
- stage 3 – pathological size of the liver, excess fluid in the tissues of the body, abdominal dropsy, cardiac dropsy.
Acute heart failure causes cardiac asthma, pulmonary edema, and cardiogenic shock in children. It is divided into the following types:
- with stagnant geodynamics (blood movement) - in the right or left ventricle;
- with hypokinetic hemodynamics (weak cardiac output with increased peripheral pressure) - reflex, arrhythmic, cardiogenic shock.
Right-sided failure
In children, cardiovascular insufficiency of the right atrium is associated with stagnation of blood in the systemic circulation. Among the main manifestations of the disease, the following should be highlighted:
- swelling;
- disruption of the liver, intestines and stomach;
- blood stagnation;
- nausea and vomiting.
View gallery
External swelling mainly appears on the legs, and it intensifies significantly in the evening. In this case, the swelling does not affect the shoulders, face and arms, and in bedridden children it is concentrated in the lumbar region. In a newborn baby, the swelling is not very pronounced, but in him the disease can manifest itself as cyanosis on the back of the feet and hands.
Terms and Definitions
New and narrowly focused professional terms are not used in these clinical guidelines.
Chronic heart failure (CHF) is a syndrome that develops as a result of various diseases of the cardiovascular system (CVS), leading to the inability of the heart to provide systemic blood flow adequate to the metabolic needs of the body, which is accompanied by intracardiac and peripheral hemodynamic changes, structural changes in the heart, and disorders of neurohumoral regulation. blood circulation, congestion in the systemic and/or pulmonary circulation.
Depending on how quickly symptoms develop, heart failure (HF) can be acute or chronic.
Acute HF is usually understood as the sudden development of hemodynamic disturbances due to circulatory overload of the heart or acute myocardial damage with the rapid development of stagnation in the pulmonary circulation, up to pulmonary edema or cardiogenic shock.
Chronic heart failure (CHF) is a consequence of long-term disease of the cardiovascular system. The progression of CHF manifests itself either as a sudden or gradual increase/appearance of symptoms.
Acute decompensation of heart failure (ADHF), requiring hospitalization, is usually caused by a combination of myocardial failure, neurohumoral imbalance, and progression of systemic inflammation. ADHF should be regarded as an independent syndrome and differentiated from acute HF.
There are systolic and diastolic heart failure. In the first case, decompensation, including a decrease in cardiac output, is caused by a decrease in myocardial contractile function, which is assessed by the value of the LV ejection fraction (EF) ({amp}lt;45-50%).
In some patients, HF is caused by impaired diastolic function and is mainly caused by a decrease in the filling of the heart cavities during diastole. The reasons for its development in children are: myocardial stiffness (hypertrophic and restrictive cardiomyopathy), increased tension in the arterial bed (arterial hypertension), impaired myocardial relaxation in diastole (constrictive pericarditis), decreased volume of the heart cavities (tumor), significant shortening of diastole (tachysystolic forms of the disorder). heart rate). In most cases, children with HF have signs of both systolic and diastolic dysfunction.
Depending on the predominance of congestion in the pulmonary or systemic circulation, it is accordingly divided into left- or right-ventricular HF.
Left-sided failure
Heart failure in a young child and, especially in newborns, is mainly caused by impaired functioning of the left ventricle of the heart. With this type of pathology, signs such as:
- rapid pulse;
- dyspnea;
- sweating and increased fatigue;
- moist wheezing in the chest.
It is worth noting that many children complain of lack of air. Parents definitely need to pay attention to such quite characteristic signs as intermittent and rapid breathing, as well as shortness of breath even with minor physical exertion.
In addition, among the main signs of the disease in newborns are sleep disturbances, attempts to sit or lie down so that the chest is slightly elevated. In this position, the wheezing subsides, and the attack of suffocation weakens. Stagnation of blood provokes a cough without sputum production. Without timely treatment, a prolonged increase in pressure provokes pulmonary edema. This condition is very dangerous and requires urgent medical intervention.
Symptoms
Heart failure can be acute or chronic, depending on the cause that caused it, the rate of development and duration of the disease. Taking into account the predominant damage to the parts of the heart and their severity, a distinction is made between left-sided and right-sided heart failure, which differ in their manifestations.
But they also have common symptoms:
- increased fatigue;
- pronounced pallor of the skin;
- cyanosis of the nail phalanges of the fingers on the extremities and the nasolabial triangle (acrocyanosis);
- dyspnea;
- dry cough;
- dizziness (possible fainting);
- increased heart rate;
- sleep disturbance;
- swelling.
Initially, most of these manifestations occur after any physical activity (outdoor play or running in older children, feeding or crying in babies). Subsequently, shortness of breath occurs even at rest, and sleep is disturbed due to the feeling of lack of air. Even the minimum load is poorly tolerated, the child lags behind his peers in physical development.
Manifestations of left ventricular failure
In early childhood, including newborns, left ventricular failure develops more often. This is due to the fact that the myocardium in the left ventricle is weaker and therefore more sensitive to overload.
A small child cannot complain of feeling short of air. Parents may notice increased breathing (shortness of breath) with the participation of auxiliary muscles (intercostal spaces, wings of the nose) in breathing with slight load or tension, in a horizontal position. A dry cough occurs periodically.
Overflow of blood into the pulmonary circulation forces an older child to take a forced position - sitting or reclining: in this position, the pulmonary circulation is somewhat unloaded, the feeling of suffocation decreases, and there are fewer moist rales.
Stagnation of blood in the lungs is manifested by a dry cough. Its appearance is associated with swelling of the bronchial mucosa or compression of the recurrent nerve by the blood-filled pulmonary artery. Cardiac asthma develops, in which it is difficult to inhale (in contrast to bronchial asthma with a characteristic difficulty in exhaling).
An attack of cardiac asthma develops most often in the morning. The child is restless, older children feel chest pain and lack of air, and there is a fear of death. In addition to shortness of breath, there is a painful, unproductive cough with a scanty amount of sputum.
As heart failure worsens, the child develops pulmonary edema. At the same time, the cough intensifies, foamy sputum appears (hemoptysis, in which the sputum turns pink, cannot be ruled out). Moist wheezing can be heard from a distance, rapid breathing becomes noisy and bubbling. Cyanosis increases. The number of heartbeats also increases. The condition is life-threatening. In the absence of emergency help, the child loses consciousness.
Manifestations of cardiogenic shock are:
- pronounced marbling of the skin;
- increasing acrocyanosis;
- dyspnea;
- cold sweat;
- swollen neck veins;
- decreased amount of urine excreted;
- progressive drop in blood pressure;
- low pulse pressure (the difference between systolic and diastolic pressure, that is, between the upper and lower pressure readings when measured);
- disturbance of consciousness.
Manifestations of right-sided heart failure
In addition to the shortness of breath and cough characteristic of left ventricular failure, weakness of the muscles of the right heart leads to overload of the right ventricle and atrium, to congestion in the systemic circulation, and an increase in venous pressure.
The main manifestations of this condition will be edema, functional disorders of the gastrointestinal tract, kidneys and liver, nausea, vomiting. Their occurrence is associated with blood stagnation and internal edema.
Swelling is mainly localized in the lower extremities and increases in the evening. They are not on the face and upper shoulder girdle. In newborns, dense swelling may develop on the genitals.
Upon examination, swollen veins in the neck, profuse cold sweat, increasing bluishness of the skin are visible, an enlarged and painful liver, shortness of breath, and increased heart rate are detected. Older children complain of heart pain. In chronic right-sided heart failure, fluid leaks out and accumulates in the abdominal cavity (ascites).
Children often develop total heart failure, when both the left and right sections are affected. Symptoms of such a serious condition will be manifestations of stagnation in both the pulmonary and systemic circulation.
In newborns, detecting heart failure is most difficult, especially in the first months of life.
Additional examination is necessary if the following symptoms are detected:
- fatigue (even when breastfeeding);
- shortness of breath with little activity of the baby and when crying;
- cardiopalmus;
- pale skin;
- cyanosis of the nasolabial triangle;
- regurgitation during feeding;
- the presence of moist rales in the lungs (sometimes audible from a distance);
- coughing;
- increased sweating;
- poor sleep in a horizontal position;
- anxiety when lying down for a long time.
Degrees of the disease
Doctors distinguish 3 degrees of heart failure in children, which are characterized by various signs. The first degree is considered the easiest. Among the main signs of pathology are nervousness, weakness and restless sleep. If the baby’s body is subjected to fairly heavy loads, severe shortness of breath occurs and the pulse accelerates. After comprehensive treatment, the state of health stabilizes, and all symptoms of the disease disappear.
The second degree is further divided into two forms. In the first form, shortness of breath appears even with slight exertion. The child complains of decreased appetite, restless sleep, pain in the right hypochondrium and rapid heartbeat. The symptoms are more pronounced.
View gallery
In the second form of the disease, the child’s well-being worsens. Even in a completely calm state, the pulse quickens, the liver enlarges, shortness of breath occurs, colic, insomnia appear, the skin turns blue and swelling occurs.
The third degree is the most severe, and the patient’s health is very poor. The shortness of breath does not stop, and swelling spreads throughout the body. This degree is characterized by the fact that it is irreversible. It is possible to normalize the patient’s well-being, but the effect will be short-lived. Dangerous and severe pathologies affecting the nervous system occur in the heart and other organs.
The third degree manifests itself in the form of drowsiness, depression, however, at the same time, mental overexcitation and insomnia can be observed, as well as clouding of consciousness.
Treatment
The pathology must be treated immediately after symptoms are identified. The main thing in treatment is to prevent the latter degree of severity, since in this case even modern medicine will not be able to do anything.
Treatment of heart failure in children can be done conservatively or through surgery. If signs of pathology are noticed, emergency assistance will be required, which consists of the following:
- The child must be kept in a semi-sitting position.
- Next, a tourniquet is applied to the legs so that arterial blood flow is not impaired.
- Feet should be placed in warm water.
If the child is already in the hospital, he will be injected with a drug. Typically, morphine is used. After this, an oxygen mask is installed through which breathing occurs. If the patient has acute deficiency, treatment is carried out with the administration of heparin.
Stenosis of the coronary vessels of the heart
Surgeries are performed when other treatments fail. Treatment in this case is radically different:
- In the first case, a complete heart transplant occurs. The damaged organ is removed, after which the donor organ is sutured.
- In the second case, treatment is carried out with cardiomyoplasty. In other words, the surgeon takes a piece of the patient's latissimus dorsi muscle, after which it covers the patient's heart. Due to this, improved contraction of the heart muscles is achieved.
- In the latter case, treatment involves replacing the heart with an artificial one. In this case, prostheses are used that improve contractility.
After the child recovers, certain care will be required.
Important! After surgery and in case of complications, it is necessary to observe bed rest, while maintaining a semi-sitting position. It is better to coordinate the loads with the treating doctor.
Causes of occurrence at an early age
Heart failure is a condition of the cardiac muscle in which it cannot contract and eject the required volume of blood, resulting in congestion in the circulatory system. In infants and children under 3 years of age, the causes of heart failure are usually associated with the presence of congenital heart defects. Among the main risk factors, the following should be highlighted:
- genetic predisposition;
- chronic alcoholism of a woman;
- taking certain medications during pregnancy;
- an early viral infection.
Among the main causes of heart failure in children are cardiac heart defects. In this case, immediately after the birth of the child, characteristic signs are observed, in particular, cyanosis, severe anxiety, shortness of breath, convulsions, and loss of consciousness. Without urgent surgical intervention, the child's death may occur.
Causes
Heart failure is a complication of most congenital heart defects.
In children, heart failure can develop at any age (including newborns) due to various reasons.
The main causes of heart failure are:
- infectious and inflammatory lesions of the myocardium (with carditis of a bacterial, viral, toxic or allergic nature);
- congenital myocardiopathy (weakness of the heart muscle);
- heart defects (congenital and acquired);
- severe lung pathology (cystic fibrosis, congenital anomalies of the bronchopulmonary system, severe bronchial asthma attack, etc.);
- acute hypoxia (oxygen deficiency in tissues);
- imbalance of electrolytes in the body;
- heart rhythm disturbances (arrhythmias);
- severe anemia;
- neoplasms of the valve or cavity of the heart;
- vasculitis (inflammation of blood vessels), etc.
In some cases, several reasons are combined.
There are acute and chronic, left ventricular (or left-sided) and right-sided heart failure.
The cause of acute left ventricular failure can be either a congenital pathology (heart disease in the form of valve insufficiency between the left ventricle and the atrium) or acquired (myocardial inflammation). As a result, the contractile function of the left ventricle is significantly reduced, its overload occurs, and a retrograde increase in pressure in the pulmonary (lesser) circulation occurs.
At the same time, from small arteries and veins, due to the increased permeability of the vascular wall, the liquid part of the blood sweats into the pulmonary alveoli. Gas exchange is disrupted, as a result of which blood oxygen saturation decreases. This leads to hypoxia of various organs. The main manifestations of left ventricular heart failure develop - cardiac asthma, pulmonary edema, cardiogenic shock.
Right ventricular failure of the heart develops when blood flow in the systemic circulation is disrupted, when the right parts are overloaded.
This situation occurs when:
- heart defects;
- severe attack of bronchial asthma;
- cystic fibrosis;
- respiratory distress syndrome with the development of acute hypoxia;
- malformations of the bronchopulmonary system.
According to the mechanism of development, acute heart failure is divided into 2 forms:
- In the energy-dynamic form, it is associated with metabolic (metabolic) disorders in the heart muscle. This form develops with inflammatory, dystrophic and toxic lesions of the heart muscle: myocarditis, viral and bacterial infections, poisoning, myocardiopathy.
- The hemodynamic form occurs when the heart is overloaded, and metabolic changes in the myocardium are secondary, developing against the background of hypertrophy of the heart muscle. This form of heart failure is observed with arrhythmias and heart defects.
If compensatory mechanisms are turned on, then over a period of time the heart copes with the increased load with the help of a higher heart rate, thickening of the heart muscle, and the effects of released biologically active substances. But eventually the compensatory mechanisms are exhausted. Slower (over several months or years) development of the pathology is chronic heart failure.
Causes of occurrence in older age
If signs of heart failure are observed in older children, the cause may be:
- previously suffered rheumatism;
- hypertension;
- cardiomyopathy;
- myocarditis;
- infective endocarditis.
All these disorders and pathologies can provoke a rapid deterioration in health and the development of heart failure. It is very important to promptly identify signs of the disease and visit a doctor for diagnosis and treatment.
Main symptoms
View gallery
Symptoms of heart failure in children can be very different, it all depends on which part of the heart is affected. Among the main signs of pathology in infants are the following:
- frequent crying;
- anxiety;
- constant and heavy sweating;
- breathing disorder.
During breastfeeding, the baby very quickly loses strength and stops sucking milk, and also begins to cry.
Among the main symptoms of the disease in preschool children, the following should be highlighted:
- children try to sit or lie down;
- decreased physical activity of the child;
- children do not particularly want to participate in games;
- Shortness of breath appears during an attack of fear, as well as during active games.
During a period of rapid development of the body, adolescents experience shortness of breath, which many parents do not attach much importance to for a long time. At the very beginning of the development of the disease, no painful manifestations are observed. If pain occurs in the heart area during active movements or when coughing, this is a reason to consult a doctor. Blue lips and excessive paleness of the skin may also occur. In this case, it is imperative to provide timely assistance to the child.
First aid
If you suspect acute heart failure, you should immediately call an ambulance. During an attack, oxygen starvation occurs. It is imperative to provide first aid to the injured child. Emergency assistance is as follows:
- you need to unfasten the collar and ensure the flow of fresh air;
- the child must be placed in a comfortable position;
- calm the victim, distract him from fear and pain;
- to reduce the flow of blood to the heart, make baths for the hands and feet;
- You can also apply a venous tourniquet and relax it after 20 minutes.
If the pressure has risen, then the child should be given half or a whole Nitroglycerin tablet, which he should place under the tongue. To save his life, it is imperative to take all the necessary measures for prompt hospitalization. Transportation must be carried out with the utmost care.
Diagnosis of heart failure
Diagnosis of heart failure begins with a general examination by a doctor. External signs of such a syndrome allow the doctor to quickly make a decision and make a decision either to provide emergency care or to conduct further diagnostics. Auscultation of the heart reveals muffled sounds, as well as the appearance of additional pathological arrhythmic heart sounds. Auscultation also reveals fine-bubble moist rales, characteristic of left ventricular heart failure. Palpation of the abdomen allows you to determine the enlargement and hardening of the child’s liver, which is one of the signs of right ventricular failure.
Assessment of the condition of the heart muscle, as well as determination of the degree of insufficiency of pumping function, is carried out using ultrasound of the heart and large great vessels (EchoCG). This diagnostic method is considered the “gold standard” in establishing most cardiac diagnoses. It allows you to reliably assess the following important parameters:
Carrying out diagnostics
Treatment of heart failure in children requires preliminary competent and comprehensive diagnosis. It is carried out in non-invasive ways:
- radiography;
- electrocardiography;
- exercise test;
- ultrasound diagnostics.
In particularly difficult cases, cardiac catheterization may be indicated to make an accurate diagnosis. Timely diagnosis is important, since if the diagnosis is not made in a timely manner, it can lead to very dangerous consequences. Heart failure leads to a decrease in blood supply to internal organs, as well as the brain. As a result, the child may be severely behind in mental and mental development and, if treatment is not started in a timely manner, growth may stop. This applies not only to height, but also to the lack of growth of internal organs.
What medications should I use?
Medicines do not cure, but only alleviate the symptoms of the disease. To treat heart failure, drugs that act in different ways are used.
Some medications improve cardiac function, the blood is saturated with more oxygen, and with it the entire body. These include cardiac glycosides, including digoxin, digitoxin, lantoside, isolanide. They are found in the foxglove plant. Thanks to them, the strength and speed of contraction of the heart muscle increase, and the metabolism of the myocardium increases. However, in large quantities, these drugs are toxic, cause nausea, headaches, interruptions in heart function and lead to insomnia. Therefore, the doses of these drugs are selected very carefully depending on the degree of the disease, the age of the patient and individual tolerance.
You should not give your child more than what the doctor prescribed on your own, as this can lead to progression of heart failure.
Some medications help the body get rid of excess fluid. They also should not be given to a child without consulting a doctor. Diuretics can enhance the effect of cardiac glycosides, causing dangerous changes in the body. The doctor decides which medications from this group the child needs. He does this based on the parents' observations of how much the patient drinks and how much urine he produces. Its amount should not be less than the volume of liquid that the child drinks per day.