What does normosystole mean?
Normosystole refers to sinus heart rhythm, accompanied by a normal heart rate - from 55-60 to 80-90 per minute. It is this heart rate that allows the heart muscle to work without increased load on the myocardium, while at the same time providing the necessary cardiac output to supply blood to the internal organs.
In other words, the commonly used term “sinus rhythm, normosystole” in the ECG protocol indicates that the heart is working correctly and the examination result is good.
Bradysystole and tachysystole, in turn, indicate a slowdown and acceleration of the heart rhythm, respectively. Read about these abnormalities on the ECG in separate materials - bradysystole, tachysystole.
Normal heart rate
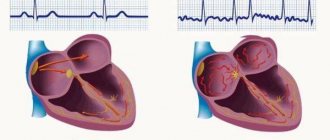
The concept of normosystole usually also refers to the fact that electrical signals that contribute to the sequential electrical excitation of all parts of the heart are generated in the sinus node, which is normally the first-order pacemaker. In all other cases, they speak of pacemaker migration or non-sinus rhythm. These processes are united by the concept of heart rhythm disturbances, or arrhythmias.
Therefore, usually in the ECG conclusion, in addition to the characteristics of the heart rate (HR), in the first place there is a mention of whether the patient has sinus rhythm or not. If the patient sees the term “normosystole” in the protocol, then most likely this means that he has not only a correct, normal heart rhythm, but also a sinus rhythm - that is, it comes from the sinus node, as it should be normally. (Nevertheless, there are formulations of “normosystole” with an even heart rate, but non-sinus rhythm - more on this at the end of the article).
Prevention of attacks of tachysystole
The problem of preventing attacks of tachysystole is of great importance in ischemic cardiomyopathy. It is difficult to predict in advance which drugs may be effective. If you need to take drugs for a long time, you have to take into account their side effects. Therefore, preference is given to drugs whose negative impact on myocardial contractile function and conductivity, as well as other side effects, is minimal.
Sensitivity to the drug may be different for the same type of arrhythmias. Our employee T.G. Gomzyakova (1972), who treated a large group of patients with persistent attacks of tachysystole on an outpatient basis, before finding an effective remedy for each patient, in most cases tested 3 to 5 drugs in succession. At the same time, in 75% of patients it was possible to achieve a reduction in the frequency of attacks by 2-3 times or their disappearance. In half of the patients the effect lasted from a year to 3-4 years, in 1/5 - up to a year, in the rest - at least 2 months.
Potassium preparations, in particular potassium chloride (2.0 - 4.0 g per day) and panangin (2 tablets 3 times a day), often in combination with glycosides, maintain sinus rhythm in cases where paroxysms of flutter and flicker appeared for the first time or occurred rarely before treatment and the patients were not actually treated.
Most patients received quinidine before admission to the clinic, and it turned out to be ineffective or stopped working. Of the 11 patients in whom treatment with quinidine began in our clinic (0.45 - 0.6 g per day), the effect was noted in only one case, which does not agree with the data of other authors on the effectiveness of quinidine in these cases (I.M. Arrigoni, 1968). Perhaps this is due to the particular persistence of attacks in our patients. Recently, data have appeared on the great promise of using durul quinidine for this purpose.
One of the most promising drugs for the prevention of paroxysmal tachysystoles, especially atrial fibrillation and supraventricular, in patients with coronary artery disease is ethmozin (carbazine). Its long-term use (0.05 - 0.075 g per day) gives virtually no side effects, and success is achieved in 50% of all cases. Novocainamide (1.5 - 2.0 g per day) is effective only for ventricular tachysystoles in approximately 1/4 of patients. In some cases of this type of arrhythmia, antithyroid drugs were effective.
β-blockers, always in combination with glycosides (usually obzidan 0.04 - 0.06 g per day) gave a preventive effect only in some cases of atrial fibrillation and supraventricular tachycardia. In a number of cases, with supraventricular tachycardias, a very convincing effect was obtained from isoptin and rhythmodan, and in ventricular tachysystole - from ajmaline.
"Ischemic heart disease", ed. I.E. Ganelina
Common deviations from the norm (brady- and tachysystole)
Sometimes the ECG conclusion may show a combination of normosystole and irregular sinus rhythm. The latter can occur, for example, with respiratory or sinus arrhythmia. In this case, the rhythm comes from the sinus node (as it should be normally), but there are minor functional fluctuations in the heart rate due to the phases of inhalation and exhalation (normally, when inhaling, the heartbeat speeds up slightly, and when exhaling, it slows down slightly). Therefore, if a patient sees a conclusion about normosystole with an irregular but sinus rhythm, there is no point in panicking.
When a patient experiences an increase or decrease in heart rate, the doctor describes this as tachycardia or bradycardia. But sometimes he may write about tachysystole or bradysystole, which literally means frequent or rare heartbeats, respectively. In this context (assuming sinus ri and “systole” are synonymous.
Again, tachysystole and bradysystole can occur both in a completely healthy person and in various diseases of the heart or other organs. Here everything depends on other nuances obtained from the ECG. But if a person has a sinus rhythm with a slightly slow heart rate (at least 50 per minute) or increased heart rate (90-100) - especially from excitement, then we can talk about normal indicators.
Prevention of tachysystole
Prevention of attacks of tachysystole has problems in the context of ischemic cardiomyopathy, since it is very difficult to predict in advance the effectiveness of a particular drug. During long-term use of the drug, one must take into account its side effects. It is because of this that those drugs with minimal side effects are preferred.
The most promising drug for the prevention of attacks of tachysystole is Ethmozin. Since with its long-term use it has practically no side effects and at the same time success with its use is achieved in 50% of all identified cases. Also, in a number of cases, a convincing effect was obtained from “Ri and Isotin”.
If you have been diagnosed with this by a qualified specialist, then you first need to follow all his recommendations to improve your health. In addition, you should not self-medicate, because traditional medicine can only worsen your health condition. After diagnosing tachysystole, constant supervision by the attending physician is necessary. If new symptoms appear, you should seek advice from a medical institution to avoid a sharp deterioration in health.
Normosystole with atrial fibrillation
Of all rhythm disturbances, only this type of arrhythmia, such as fibrillation or atrial flutter, is divided into normo-, tachy- and bradysystolic variants. In this case, the diagnosis “atrial fibrillation, normosystole” indicates a pathology in the form of arrhythmia, but with a normal final heart rate.
In this case, we are talking about both a permanent form of atrial fibrillation, when a person lives for a long time (months and years) with an abnormal or non-sinus rhythm, and a paroxysmal form (paroxysm - attack), when a non-sinus rhythm occurs suddenly and may well recover spontaneously or with the help of medications. Diagnostic criteria are similar to those for normo-, brady- and tachysystole in sinus rhythm - from 60 to 80, less than 60 and more than 80 beats per minute, respectively.
With a permanent form of atrial fibrillation, normosystole is usually more easily tolerated by patients in terms of the sensation of interruptions in the work of the heart, since bradysystole is fraught with a decrease in cardiac output and resulting fainting, and the heart rate during tachysystole sometimes reaches 200 beats per minute, which can lead to severe circulatory disorders.
Is it necessary to treat the normosystolic variant of atrial fibrillation?
Treatment of paroxysmal atrial fibrillation with normosystole is strictly necessary, because paroxysm, even with a normal heart rate, requires emergency drug restoration of rhythm. Typically, drugs such as cordarone, procainamide, and a polarizing mixture are administered intravenously.
A patient with normosystole with a permanent form of atrial fibrillation must take drugs such as digoxin, aspirin to prevent blood clots, and sometimes warfarin for the same purpose. Rhythm-slowing therapy for normosystole should be treated with extreme caution, since metoprolol, bisoprolol, verapamil and similar drugs can provoke a significant slowdown in heart rate and cause bradycardia with loss of consciousness.
In conclusion, it should be said once again that normosystole with the correct sinus rhythm is a sign of normal functioning of a healthy heart, therefore this term only indicates that according to a specific ECG everything is in order.
Source: sosudinfo.ru
Heart rhythm during arrhythmia
- 1 Why does the heart rhythm change? 1.1 Types of arrhythmia
Have you been struggling with HYPERTENSION for many years without success?
Head of the Institute: “You will be amazed at how easy it is to cure hypertension by taking it every day...
Read more "
When a person is healthy and calm, his heart rate is sinus with a heart rate of 60 to 90 beats per minute. At the same time, the body is able to quickly restore sinus rhythm and pulse if they are disturbed. If the heart rhythm disturbance is constant, and there are also other unpleasant symptoms, such as shortness of breath, dizziness, weakness, then this is a cause for concern.

Why does the heart rhythm change?
The pattern of heartbeat can be pathologically changed by:
- Cardiac diseases: coronary disease;
- heart failure;
- arterial hypertension;
- myocarditis;
- heart defects.
- disruption of the nervous, endocrine, and digestive systems;
Return to contents
Types of arrhythmia
Heart rhythm disturbances occur when electrical impulses do not work correctly.
- Sinus tachycardia - pulse up to 160 beats/min, sinus pattern is preserved. In the short term it can be caused by stress, strong coffee, and physical activity. In this case, the heartbeat returns to normal after the cessation of these factors, and tachycardia does not cause discomfort. Otherwise, pathology is suspected.
- Sinus bradycardia - heart rate up to 60 beats/min, sinus pattern is preserved. A low pulse is a normal condition for athletes. If a person is untrained, then bradycardia can be caused by diseases of the thyroid gland, liver, and viruses.
- Paroxysmal ventricular tachycardia is a paroxysmal increase in heart rate up to 170 beats/min, tachycardia with disturbance of sinus rhythm. This type of arrhythmia also includes extrasystole, ventricular flutter, and atrial fibrillation.
- Atrioventricular block - heart rate drops to 20-40 beats per minute, a person feels severe weakness, dizziness, and is close to losing consciousness.
Return to contents
Heart rate measurement for arrhythmia
Arrhythmia can be diagnosed by performing an ECG (electrocardiogram). In this case, a number of special parameters are analyzed, as well as heart rate. You can also measure your heart rate yourself. You need to find a pulsating artery on the inside of the wrist or on the neck under the jaw, and count the pulsation for 15 seconds, and then multiply this value by 4. If the pulsation is uneven, it is better to measure within a minute. A more complex and accurate measurement method is this: turn on the stopwatch, count 15 pulse beats, turn off the stopwatch and divide 900 by the number of seconds obtained on the stopwatch.
on
Return to contents
How to restore heart rhythm?
Since sinus arrhythmia is not an independent disease, but a symptom, it is necessary to act on the disease leading to the arrhythmia. To restore the heart rhythm during arrhythmias, antiarrhythmic drugs are used (Amiadoron, Ritmonorm, glycosides, beta blockers). For atrial fibrillation, statins and angiotensin-converting enzyme inhibitors are used. All of them have unwanted side effects, so they should be used as directed and under the supervision of a doctor. A special medical device, a pacemaker, is used to stabilize the heartbeat. Rehabilitation for such cardiac disorders also includes breathing exercises, dieting, giving up bad habits, and normalizing the psycho-emotional state.
on
A comment
Nickname
Characteristics of the concept
What is tachysystole? This concept comes from two words - “tachy” (quickly) and “systole” (contraction). Thus, tachysystole is an acceleration of heart contractions. The normal heart rate is between 60-80 beats per minute. Anything over 80 is called tachyarrhythmia.
These disorders are quite common in cardiology.
The following forms of tachysystole are distinguished:
- sinus tachycardia;
- atrial tachycardia, fibrillation and fibrillation;
- ventricular tachycardia and fibrillation.
Each condition has its own manifestations.
Sinus tachycardia
This condition is not considered a disease and is not life-threatening. With sinus tachycardia, the heart rate exceeds 100 beats per minute.
There are two types of ST:
- Physiological . Appears with pronounced emotional excitement, physical stress, consumption of large doses of nicotine and caffeine. Physiological tachycardia is observed in young children and athletes.
- Pathological . Caused by certain diseases - anemia, fever, thyrotoxicosis, heart failure.
Symptoms of sinus tachycardia are rarely severe. A person may be bothered by a feeling of rapid heartbeat, interruptions in heart function, dizziness, and shortness of breath.
Sinus tachycardia is diagnosed by auscultation or by electrocardiogram. In the physiological form, it is necessary to avoid provoking factors and take sedatives. In the pathological form, the underlying disease is treated.
Supraventricular tachycardia
These conditions are associated with rapid contraction of the atria. There are several forms of pathology.
Table. Characteristics of atrial tachycardias:
| Form | Symptoms | Treatment instructions |
| Paroxysmal tachycardia - regular contractions are observed with a frequency of 150-230 per minute | Starts and stops suddenly. A person complains of an attack of rapid heartbeat and severe weakness. A decrease in pressure may be observed, and with significant hypotension, acute heart failure develops | You can stop the attack by inducing vomiting or coughing, inhaling with straining, and massaging the interclavicular fossa. The drugs used are adenosine or verapamil intravenously |
| Multifocal atrial tachycardia - the appearance of three or more consecutive extrasystoles | Usually not felt sick, numerous extrasystoles can cause weakness and dizziness | Verapamil is used intravenously |
| AV nodal tachycardia - increased frequency of atrial contractions up to 130 per minute | Manifested by dizziness. Usually occurs due to intoxication with glycosides, heart attack, heart surgery | Does not require specific treatment |
These diseases are also not life-threatening. For diagnosis, an electrocardiogram or Holter monitoring is used, where attacks of increased contractions are recorded.
Atrial fibrillation
This is an uncoordinated contraction of the muscle fibers of the atria, in which the heart rate reaches 700 beats per minute.
There are two forms of fibrillation:
- paroxysmal - lasts no more than two days;
- chronic - lasts more than two days.
Atrial fibrillation is registered in 0.5% of the population, but among people over 65 years of age it occurs in 5%.
Causes
30% of the population has an idiopathic form of the disease, that is, it has no apparent cause.
In the rest, the pathology develops against the background of cardiac and extracardiac diseases:
- heart attack;
- pericarditis or myocarditis;
- heart surgery;
- heart defects;
- hypertension;
- cardiomyopathy;
- alcoholism;
- thyrotoxicosis;
- TELA;
- electrical injury;
- pneumonia.
More often, the pathology develops against the background of heart disease. Many foci appear in the cardiac tissue that generate electrical impulses (photo). As a result, excitation and contraction of individual areas of the myocardium occur.
Manifestations
Patients with atrial fibrillation complain of increased fatigue, dizziness, a feeling of rapid heartbeat, shortness of breath, and attacks of loss of consciousness. In some patients with underlying heart disease, signs of heart failure increase. Less commonly, there are no complaints - the asymptomatic form.
The examination reveals characteristic signs of the underlying disease. On auscultation, a rapid heartbeat is recorded.
Diagnostics
The diagnosis is confirmed after instrumental studies:
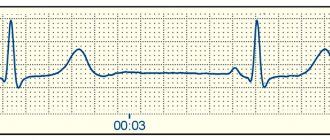
- ECG . There is an absence of P waves (normal atrial contractions); instead, specific f waves appear. There is an irregular heart rhythm.
- Holter monitoring . It is carried out to determine the number of attacks of fibrillation per day.
- Ultrasound of the heart . Detects heart disease, assesses ventricular function, and detects intracardiac blood clots.
To exclude thyrotoxicosis as a cause of fibrillation, the content of thyroid hormones in the blood is examined.
Therapeutic measures
Treatment goals for atrial fibrillation:
- restoration of normal rhythm;
- prevention of paroxysms of fibrillation;
- prevention of complications, primarily thromboembolic.
If the rhythm is severely disrupted, emergency defibrillation is performed.
Restoring a normal rhythm helps improve the patient’s overall well-being and reduces the risk of thromboembolic complications. For this purpose, first class antiarrhythmic drugs are used - Propafenone or Amiodarone. The drugs are administered orally or intravenously. In case of chronic fibrillation, anticoagulants are prescribed on a regular basis.
Surgical treatment is indicated when conservative methods are ineffective. It consists of destroying the AV connection with a radio knife and installing an artificial pacemaker.
What is Tachysystole: Causes, Symptoms, Treatment Methods
Tachysystole is a collective concept used to designate disturbances in heart rhythm in the direction of its acceleration.
Tachysystole includes several pathologies accompanied by accelerated contraction of the atria or ventricles. Some of them are relatively mild, while others are life-threatening. Tachysystole is a type of arrhythmia
Characteristics of the concept
What is tachysystole? This concept comes from two words - “tachy” (quickly) and “systole” (contraction). Thus, tachysystole is an acceleration of heart contractions. The normal heart rate is between 60-80 beats per minute. Anything over 80 is called tachyarrhythmia.
These disorders are quite common in cardiology.
The following forms of tachysystole are distinguished:
- sinus tachycardia;
- atrial tachycardia, fibrillation and fibrillation;
- ventricular tachycardia and fibrillation.
Each condition has its own manifestations.
Sinus tachycardia
This condition is not considered a disease and is not life-threatening. With sinus tachycardia, the heart rate exceeds 100 beats per minute.
There are two types of ST:
- Physiological . Appears with pronounced emotional excitement, physical stress, consumption of large doses of nicotine and caffeine. Physiological tachycardia is observed in young children and athletes.
- Pathological . Caused by certain diseases - anemia, fever, thyrotoxicosis, heart failure.
Symptoms of sinus tachycardia are rarely severe. A person may be bothered by a feeling of rapid heartbeat, interruptions in heart function, dizziness, and shortness of breath.
Sinus tachycardia is diagnosed by auscultation or by electrocardiogram. In the physiological form, it is necessary to avoid provoking factors and take sedatives. In the pathological form, the underlying disease is treated.
Sinus tachycardia is normal for newborns
Supraventricular tachycardia
These conditions are associated with rapid contraction of the atria. There are several forms of pathology.
Table. Characteristics of atrial tachycardias:
| Form | Symptoms | Treatment instructions |
| Paroxysmal tachycardia - regular contractions are observed with a frequency of 150-230 per minute | Starts and stops suddenly. A person complains of an attack of rapid heartbeat and severe weakness. A decrease in pressure may be observed, and with significant hypotension, acute heart failure develops | You can stop the attack by inducing vomiting or coughing, inhaling with straining, and massaging the interclavicular fossa. The drugs used are adenosine or verapamil intravenously |
| Multifocal atrial tachycardia - the appearance of three or more consecutive extrasystoles | Usually not felt sick, numerous extrasystoles can cause weakness and dizziness | Verapamil is used intravenously |
| AV nodal tachycardia - increased frequency of atrial contractions up to 130 per minute | Manifested by dizziness. Usually occurs due to intoxication with glycosides, heart attack, heart surgery | Does not require specific treatment |
These diseases are also not life-threatening. For diagnosis, an electrocardiogram or Holter monitoring is used, where attacks of increased contractions are recorded.
Atrial fibrillation
This is an uncoordinated contraction of the muscle fibers of the atria, in which the heart rate reaches 700 beats per minute.
There are two forms of fibrillation:
- paroxysmal - lasts no more than two days;
- chronic - lasts more than two days.
Atrial fibrillation is registered in 0.5% of the population, but among people over 65 years of age it occurs in 5%.
Causes
30% of the population has an idiopathic form of the disease, that is, it has no apparent cause.
In the rest, the pathology develops against the background of cardiac and extracardiac diseases:
- heart attack;
- pericarditis or myocarditis;
- heart surgery;
- heart defects;
- hypertension;
- cardiomyopathy;
- alcoholism;
- thyrotoxicosis;
- TELA;
- electrical injury;
- pneumonia.
More often, the pathology develops against the background of heart disease. Many foci appear in the cardiac tissue that generate electrical impulses. As a result, excitation and contraction of individual areas of the myocardium occur.
Mechanism of development of atrial fibrillation
Manifestations
Patients with atrial fibrillation complain of increased fatigue, dizziness, a feeling of rapid heartbeat, shortness of breath, and attacks of loss of consciousness. In some patients with underlying heart disease, signs of heart failure increase. Less commonly, there are no complaints - the asymptomatic form.
The examination reveals characteristic signs of the underlying disease. On auscultation, a rapid heartbeat is recorded.
Diagnostics
The diagnosis is confirmed after instrumental studies:
- ECG . There is an absence of P waves (normal atrial contractions); instead, specific f waves appear. There is an irregular heart rhythm.
- Holter monitoring . It is carried out to determine the number of attacks of fibrillation per day.
- Ultrasound of the heart . Detects heart disease, assesses ventricular function, and detects intracardiac blood clots.
To exclude thyrotoxicosis as a cause of fibrillation, the content of thyroid hormones in the blood is examined.
Therapeutic measures
Treatment goals for atrial fibrillation:
- restoration of normal rhythm;
- prevention of paroxysms of fibrillation;
- prevention of complications, primarily thromboembolic.
If the rhythm is severely disrupted, emergency defibrillation is performed.
Restoring a normal rhythm helps improve the patient’s overall well-being and reduces the risk of thromboembolic complications. For this purpose, first class antiarrhythmic drugs are used - Propafenone or Amiodarone. The drugs are administered orally or intravenously. In case of chronic fibrillation, anticoagulants are prescribed on a regular basis.
Surgical treatment is indicated when conservative methods are ineffective. It consists of destroying the AV connection with a radio knife and installing an artificial pacemaker.
Atrial flutter
This is a regular contraction of the atrium muscle with a frequency of 250-300 per minute. It is rarely observed, as it is an unstable condition that quickly turns into a normal rhythm or fibrillation. It can be paroxysmal or chronic.
The causes and symptoms of flutter are no different from those of fibrillation. The ECG shows sawtooth F waves at the site of the P waves.
Treatment is similar to fibrillation.
F waves in atrial flutter
Paroxysmal ventricular tachycardia
This is a condition that occurs as a result of the appearance of three or more ventricular extrasystoles following each other.
Symptoms
The clinical picture of paroxysmal tachycardia is poor. The patient complains of dizziness, clouding of consciousness. A decrease in pressure is objectively determined.
Treatment
In most cases, the condition does not require specific treatment. A persistent attack of VT is treated with intravenous lidocaine. Signs of hemodynamic compromise require defibrillation.
Ventricular fibrillation and flutter
These rhythm disturbances are characterized by uncoordinated contraction of the ventricles at a rate of 250-300 per minute. On the ECG it is recorded as a sinusoidal curve. Leads to cardiac arrest and clinical death.
Emergency defibrillation is required and resuscitation measures are taken. To prevent this condition, patients have a cardioverter-defibrillator installed in the heart area.
Tachysystolic heart rhythm disturbances are a large group of conditions characterized by various types of increased heart rate. Some of them are safe for life and do not cause any clinical manifestations. Some arrhythmias are life-threatening and require urgent treatment.
Questions for the doctor
Good afternoon. I was diagnosed with sinus tachycardia. The doctor said that no treatment is required at the moment, it is enough to lead a healthy lifestyle. What restrictions do I need to put into my lifestyle?
Mikhail, 25 years old, Saratov
Good afternoon, Mikhail. Sinus tachycardia is the most harmless of all tachysystoles. In fact, it almost never requires special treatment. You need to give up bad habits, do not abuse strong tea and coffee. If possible, emotional overload and physical stress should be limited.
Source: https://Cardio-help.ru/serdechnyj-cikl/tahisistoliya-chto-eto-takoe-603
Paroxysmal ventricular tachycardia
This is a condition that occurs as a result of the appearance of three or more ventricular extrasystoles following each other.
Causes
There is an idiopathic form that occurs for no apparent reason. In other cases, ventricular tachycardia develops against the background of any heart disease. An ectopic focus forming in the ventricle causes its extraordinary contractions.
Symptoms
The clinical picture of paroxysmal tachycardia is poor. The patient complains of dizziness, clouding of consciousness. A decrease in pressure is objectively determined.
Diagnostics
Ventricular tachycardia is determined using an electrocardiogram. There is a deformation of the QRS complex (contraction of the ventricle), overlapping of the atrial and ventricular complexes.
Treatment
In most cases, the condition does not require specific treatment. A persistent attack of VT is treated with intravenous lidocaine. Signs of hemodynamic compromise require defibrillation.
Causes and mechanism of development of the disease
Physiological factors can slow down heart rate. In this case, symptoms do not appear and treatment is not required. Often a low pulse is a sign of a dangerous pathology.
Bradycardia can appear as a result of the influence of certain external influences. For example, with frostbite, body temperature drops to 35°C, which leads to a decrease in heart rate. Such a decrease is considered a normal physiological manifestation; the body seems to be protecting itself from negative influences. Heart rate is restored gradually along with normalization of body temperature.
Bradycardia develops against the background of cardiac and endocrine disorders, diseases of the nervous system and internal organs, as well as as a result of pathological processes and the use of certain medications.
Cardiac (associated with heart disease) and organic forms have the following causes of development:
- myocardial infarction;
- endocarditis or myocarditis;
- cardiosclerosis;
- age-related changes in the heart;
- cardiac ischemia;
- neuroses with autonomic dysfunction;
- increased intracranial pressure.
All this leads to conduction disturbances in the myocardium or fibrotic and degenerative changes in the sinus node, which subsequently contributes to a decrease in heart rate.
The following reasons provoke bradycardia:
- infectious diseases (meningitis, typhoid fever, hepatitis);
- long-term use of certain medications;
- depression and neuroses;
- anemia, hypovitaminosis;
- renal and liver failure;
- gastrointestinal ulcers, gastritis;
- endocrine diseases;
- swelling and tumors of the brain;
- changes in the functioning of the adrenal glands;
- disorders in the cardiovascular system;
- alcohol dependence (alcoholism);
- imbalance of calcium, potassium and sodium in the blood;
- unexpected and severe shock.
Ventricular fibrillation and flutter
These rhythm disturbances are characterized by uncoordinated contraction of the ventricles at a rate of 250-300 per minute. On the ECG it is recorded as a sinusoidal curve. Leads to cardiac arrest and clinical death.
Emergency defibrillation is required and resuscitation measures are taken. To prevent this condition, patients have a cardioverter-defibrillator installed in the heart area.
Tachysystolic heart rhythm disturbances are a large group of conditions characterized by various types of increased heart rate. Some of them are safe for life and do not cause any clinical manifestations. Some arrhythmias are life-threatening and require urgent treatment.
Questions for the doctor
Good afternoon. I was diagnosed with sinus tachycardia. The doctor said that no treatment is required at the moment, it is enough to lead a healthy lifestyle. What restrictions do I need to put into my lifestyle?
Mikhail, 25 years old, Saratov
Good afternoon, Mikhail. Sinus tachycardia is the most harmless of all tachysystoles. In fact, it almost never requires special treatment. You need to give up bad habits, do not abuse strong tea and coffee. If possible, emotional overload and physical stress should be limited.
Source: Cardio-help.ru
Sinus rhythm: essence, reflection on the ECG, norm and deviations, features
Sinus rhythm is one of the most important indicators of normal heart function, which indicates that the source of contractions comes from the main, sinus node of the organ. This parameter is one of the first in the ECG conclusion, and patients who have undergone the study are eager to find out what it means and whether they should worry.
The heart is the main organ that supplies blood to all organs and tissues; the degree of oxygenation and the function of the entire organism depend on its rhythmic and consistent work. To contract a muscle, a push is needed - an impulse emanating from special cells of the conduction system. The characteristics of the rhythm depend on where this signal comes from and what its frequency is.
The sinus node (SU) is located under the inner lining of the right atrium, it is well supplied with blood, receiving blood directly from the coronary arteries, and is richly supplied with fibers of the autonomic nervous system, both parts of which influence it, contributing to both an increase and a decrease in the frequency of impulse generation.
The cells of the sinus node are grouped into bundles; they are smaller than ordinary cardiomyocytes and have a spindle-shaped shape. Their contractile function is extremely weak, but their ability to form an electrical impulse is akin to nerve fibers. The main node is connected to the atrioventricular junction, to which it transmits signals for further excitation of the myocardium.
The sinus node is called the main pacemaker, because it is the one that provides the frequency of heart contractions that gives the organs adequate blood supply, therefore maintaining a regular sinus rhythm is extremely important for assessing the work of the heart when it is damaged.
The control system generates pulses of the highest frequency compared to other parts of the conduction system, and then transmits them further at high speed. The frequency of impulse formation by the sinus node ranges from 60 to 90 per minute, which corresponds to the normal heart rate when they occur due to the main pacemaker.
Electrocardiography is the main method that allows you to quickly and painlessly determine where the heart receives impulses, what their frequency and rhythm are. ECG has become firmly established in the practice of therapists and cardiologists due to its accessibility, ease of implementation and high information content.
Having received the result of electrocardiography, everyone will look at the conclusion left there by the doctor. The first of the indicators will be the assessment of the rhythm - sinus, if it comes from the main node, or non-sinus, indicating its specific source (AV node, atrial tissue, etc.). So, for example, the result “sinus rhythm with heart rate 75” should not worry you, this is the norm, and if a specialist writes about non-sinus ectopic rhythm, increased heart rate (tachycardia) or slowdown (bradycardia), then it’s time to go for further examination.
Also in conclusion, the patient can find information about the position of the EOS (electrical axis of the heart). Normally, it can be either vertical or semi-vertical, or horizontal or semi-horizontal, depending on the individual characteristics of the person. Deviations of the EOS to the left or right, in turn, usually indicate organic pathology of the heart. The EOS and its position options are described in more detail in a separate publication.
Sinus rhythm is normal
Often, patients who detect sinus rhythm in the ECG report begin to worry whether everything is in order, because the term is not known to everyone, and therefore may indicate pathology. However, they can be reassured: sinus rhythm is the norm, which indicates the active functioning of the sinus node.
On the other hand, even with preserved activity of the main pacemaker, some deviations are possible, but they do not always serve as an indicator of pathology. Rhythm fluctuations occur in various physiological conditions that are not caused by a pathological process in the myocardium.
The impact of the vagus nerve and fibers of the sympathetic nervous system on the sinus node often causes a change in its function towards a higher or lower frequency of formation of nerve signals. This is reflected in the heart rate, which is calculated on the same cardiogram.
Normally, the frequency of sinus rhythm lies in the range from 60 to 90 beats per minute, but experts note that there is no clear boundary for determining normality and pathology, that is, with a heart rate of 58 beats per minute, it is too early to talk about bradycardia, as well as tachycardia if it exceeds indicator of 90. All these parameters must be assessed comprehensively, taking into account the general condition of the patient, the characteristics of his metabolism, type of activity, and even what he was doing immediately before the study.
Determining the source of rhythm when analyzing an ECG is a fundamental point, while the following are considered indicators of sinus rhythm:
- Identification of P waves before each ventricular complex;
- Constant configuration of atrial waves in the same lead;
- Constant value of the interval between the P and Q waves (up to 200 ms);
- The P wave is always positive (directed upward) in the second standard lead and negative in aVR.
At the conclusion of the ECG, the subject can find: “sinus rhythm with heart rate 85, normal position of the electrical axis.” We consider this conclusion to be the norm. Another option: “non-sinus rhythm with a frequency of 54, ectopic.” This result should be alarming, since serious myocardial pathology is possible.
The characteristics listed above on the cardiogram indicate the presence of sinus rhythm, which means that the impulse goes from the main node down to the ventricles, which contract after the atria. In all other cases, the rhythm is considered non-sinus, and its source lies outside the sinus system - in the fibers of the ventricular muscle, atrioventricular node, etc. Pulsation is possible from two places of the conduction system at once, in this case we are also talking about arrhythmia.
Correct conclusions about the regulation of heart rhythm can be made by studying long-term ECG recordings, since in the process of life all healthy people change their heart rate: at night the pulse is one, during the day - another. However, even shorter periods of recording ECG signs demonstrate pulse unevenness associated with the peculiarities of autonomic innervation and the functioning of the whole organism as a whole. Pulse assessment is helped by specially developed mathematical processing programs, statistical analysis - cardiointervalography, histography.
In order for the ECG result to be most accurate, all possible causes of changes in heart activity should be excluded. Smoking, quickly climbing stairs or running, or drinking a cup of strong coffee can change cardiac parameters. The rhythm, of course, will remain sinus if the node is working correctly, but at least tachycardia will be recorded. In this regard, before the study you need to calm down, eliminate stress and anxiety, as well as physical activity - everything that directly or indirectly affects the result.
Sinus rhythm and tachycardia
Let us remember again that sinus rhythm corresponds to a frequency of 60 - 90 per minute. But what to do if the parameter goes beyond the established limits while maintaining its “sinus”? It is known that such fluctuations do not always indicate pathology, so there is no need to panic prematurely.
Accelerated sinus rhythm of the heart (sinus tachycardia), which is not an indicator of pathology, is recorded when:
- Emotional experiences, stress, fear;
- Strong physical activity - in the gym, during heavy physical labor, etc.;
- After eating too much, drinking strong coffee or tea.
This physiological tachycardia is reflected in the ECG data:
- The length of the gap between the P waves and the RR interval decreases, the duration of which, with appropriate calculations, makes it possible to determine the exact heart rate figure;
- The P wave remains in its normal place - in front of the ventricular complex, which, in turn, has the correct configuration;
- According to calculations, the heart rate exceeds 90-100 per minute.
Tachycardia, with preserved sinus rhythm under physiological conditions, is aimed at providing blood to tissues that, for various reasons, begin to need it more - playing sports, jogging, for example. It cannot be considered a violation, and in a short period of time the heart itself restores the sinus rhythm to normal frequency.
If, in the absence of any diseases, the subject encounters tachycardia with sinus rhythm on the cardiogram, you should immediately remember how the study took place - whether he was worried, whether he rushed headlong to the cardiography room, or maybe he smoked on the stairs of the clinic just before taking an ECG.
Sinus rhythm and bradycardia
The opposite of sinus tachycardia is the slowing of its contractions (sinus bradycardia), which also does not always indicate pathology.
Physiological bradycardia with a decrease in the frequency of impulses from the sinus node to less than 60 per minute can occur with:
- State of sleep;
- Professional sports;
- Individual constitutional characteristics;
- Wearing clothes with a tight collar and a tightly tightened tie.
It is worth noting that bradycardia more often than an increase in heart rate indicates pathology, so close attention is usually paid to it. With organic lesions of the heart muscle, bradycardia, even if the “sinus” rhythm is maintained, can become a diagnosis requiring drug treatment.
During sleep, there is a significant decrease in heart rate - by about a third of the “daily norm”, which is associated with the predominance of the tone of the vagus nerve, which suppresses the activity of the sinus node. ECG is more often recorded in awake subjects, so such bradycardia is not recorded during routine mass studies, but it can be seen during 24-hour monitoring. If in the conclusion of Holter monitoring there is an indication of a decrease in sinus rhythm during sleep, then it is likely that the indicator will fit into the norm, which the cardiologist will explain to particularly worried patients.
In addition, it has been noted that about 25% of young men have a slower pulse in the range of 50-60, and the rhythm is sinus and regular, there are no symptoms of trouble, that is, this is a variant of the norm. Professional athletes are also prone to bradycardia due to systematic physical activity.
Sinus bradycardia is a condition when the pulse decreases to less than 60, but impulses in the heart continue to be generated by the main node. People with this condition may faint or experience dizziness; often this anomaly accompanies vagotonia (a variant of vegetative-vascular dystonia). Sinus rhythm with bradycardia should be a reason to exclude serious changes in the myocardium or other organs.
Signs of sinus bradycardia on the ECG will be a lengthening of the intervals between the atrial waves and the complexes of ventricular contractions, however, all indicators of the “sinus” rhythm are preserved - the P wave still precedes the QRS and has a constant size and shape.
Thus, sinus rhythm is a normal indicator on the ECG, indicating the preserved activity of the main pacemaker, and with normosystole the rhythm is both sinus and normal frequency - between 60 and 90 beats. In this case, there should be no cause for concern unless there are indications of other changes (ischemia, for example).
When should you worry?
Cardiography findings indicating pathological sinus tachycardia, bradycardia or arrhythmia with instability and irregularity of rhythm should be a cause for concern.
With tachy- and bradyforms, the doctor quickly determines whether the pulse is more or less abnormal than normal, clarifies complaints and refers for additional examinations - ultrasound of the heart, Holter, blood tests for hormones, etc. Having found out the cause, you can begin treatment.
Unstable sinus rhythm on the ECG is manifested by unequal intervals between the main teeth of the ventricular complexes, the fluctuations of which exceed 150-160 ms. This is almost always a sign of pathology, so the patient is not ignored and the cause of instability in the sinus node is found out.
Electrocardiography will also indicate that the heart beats with an irregular sinus rhythm. Irregular contractions can be caused by structural changes in the myocardium - scar, inflammation, as well as heart defects, heart failure, general hypoxia, anemia, smoking, endocrine pathology, abuse of certain groups of drugs and many other reasons.
An irregular sinus rhythm comes from the main pacemaker, but the frequency of the organ’s beats either increases or decreases, losing its constancy and regularity. In this case, they talk about sinus arrhythmia.
Arrhythmia with sinus rhythm can be a variant of the norm, then it is called cyclic, and it is usually associated with breathing - respiratory arrhythmia. With this phenomenon, the heart rate increases as you inhale, and decreases as you exhale. Respiratory arrhythmia can be found in professional athletes, adolescents during periods of increased hormonal changes, and people suffering from autonomic dysfunction or neuroses.
Sinus arrhythmia associated with breathing is diagnosed on an ECG:
- The normal shape and location of the atrial waves, which precede all ventricular complexes, are preserved;
- As you inhale, the intervals between contractions decrease, and as you exhale, they become longer.
Several tests can help distinguish physiological sinus arrhythmia. Many people know that during the examination they may be asked to hold their breath. This simple action helps to neutralize the effect of vegetatives and determine a regular rhythm, if it is associated with functional reasons and is not a reflection of pathology. In addition, taking a beta-blocker increases arrhythmia, and atropine relieves it, but this will not happen with morphological changes in the sinus node or heart muscle.
If the sinus rhythm is irregular and cannot be eliminated by holding your breath and pharmacological tests, then it’s time to think about the presence of pathology. It can be:
- Myocarditis;
- Cardiomyopathies;
- Ischemic disease, diagnosed in most older people;
- Heart failure with expansion of its cavities, which inevitably affects the sinus node;
- Pulmonary pathology - asthma, chronic bronchitis, pneumoconiosis;
- Anemia, including hereditary;
- Neurotic reactions and severe vegetative dystonia;
- Disorders of the internal secretion organs (diabetes, thyrotoxicosis);
- Abuse of diuretics, cardiac glycosides, antiarrhythmics;
- Electrolyte disturbances and intoxications.
Sinus rhythm, when irregular, does not exclude pathology, but, on the contrary, most often indicates it. This means that in addition to “sinus”, the rhythm must also be correct.
If the patient knows about his existing diseases, then the diagnostic process is simplified, because the doctor can act purposefully. In other cases, when an unstable sinus rhythm was found on the ECG, a complex of examinations is required - Holter (24-hour ECG), treadmill, echocardiography, etc.
Features of rhythm in children
Children are a very special part of people whose many parameters are very different from adults. So, any mother will tell you how often the heart of a newborn baby beats, but at the same time she will not worry, because it is known that babies of the first years and, especially newborns, have a pulse much faster than adults.
Sinus rhythm should be recorded in all children without exception, unless there is heart damage. Age-related tachycardia is associated with the small size of the heart, which must provide the growing body with the necessary amount of blood. The smaller the child, the faster his pulse, reaching 140-160 seconds per minute during the newborn period and gradually decreasing to the “adult” norm by the age of 8 years.
An ECG in children records the same signs of the sinus origin of the rhythm - P waves before ventricular contractions of the same size and shape, while tachycardia should fit into age parameters. The lack of activity of the sinus node, when the cardiologist indicates rhythm instability or ectopia of its driver, is a reason for serious concern for doctors and parents and a search for the cause, which in childhood most often becomes a congenital defect.
At the same time, when reading the indication of sinus arrhythmia according to the ECG data, the mother should not immediately panic and faint. It is likely that sinus arrhythmia is related to breathing, which is often observed in childhood. It is also necessary to take into account the conditions for taking an ECG: if the baby is laid on a cold couch, he is scared or confused, then a reflexive holding of breath will increase the manifestations of respiratory arrhythmia, which does not indicate a serious illness.
However, sinus arrhythmia should not be considered normal until its physiological nature is clearly proven. Thus, pathology of sinus rhythm is more often diagnosed in premature infants who have suffered from intrauterine hypoxia of children, with increased intracranial pressure in newborns. It can be provoked by rickets, rapid growth, VSD. As the nervous system matures, rhythm regulation improves, and disturbances may go away on their own.
A third of sinus arrhythmias in children are pathological in nature and are caused by hereditary factors, infection with high fever, rheumatism, myocarditis, and heart defects.
Sports for children with respiratory arrhythmia are not contraindicated, but only under the condition of constant dynamic monitoring and ECG recording. If the cause of unstable sinus rhythm turns out to be non-physiological, then the cardiologist will be forced to limit the child’s sports activities.
It is clear that parents are concerned about an important question: what to do if the sinus rhythm on the ECG is incorrect or an arrhythmia is recorded? First, you need to go to a cardiologist and give your child another cardiogram. If the physiological changes are proven, then observation and an ECG 2 times a year are sufficient.
If the instability of sinus rhythm does not fit within the normal range and is not caused by breathing or functional reasons, then the cardiologist will prescribe treatment in accordance with the true cause of the arrhythmia.
Source: miokard.lechenie-gipertoniya.ru
What is sinus rhythm on an ECG
The human heart is a kind of trigger for the productive work of the whole organism. Thanks to the impulses of this organ, which are issued on a regular basis, blood is able to circulate throughout the body, saturating the body with vital substances. If the heart is normal, then the whole body works as productively as possible, but sometimes you still have to face certain health problems.
Why do you feed pharmacies if hypertension is afraid of the usual like fire...
Tabakov has revealed a unique remedy against hypertension! To reduce blood pressure while preserving blood vessels, add to…
If a person comes for an examination to a doctor and the specialist suspects that something is wrong with his heart, he will send the patient for an ECG. Sinus rhythm on an ECG is a very important indicator and clearly provides data on the real state of the human heart muscle. What exactly can be determined by looking at the cardiogram is worth considering in more detail.
What is sinus rhythm
According to medical staff, sinus rhythm of the cardiogram is the norm for the human body. If there are equal spaces between the teeth shown on the cardiogram, and the height of these columns is also the same, then there are no deviations in the functioning of the main organ.
This means that sinus rhythm on the cardiogram is as follows:
- graphical representation of human pulse fluctuations;
- a set of teeth of different lengths, between which there are different intervals, showing the specific rhythm of heart impulses;
- schematic representation of the work of the heart muscle;
- an indicator of the presence or absence of abnormalities in the functioning of the heart and its individual valves.
Normal sinus rhythm is only present when the heart rate is at least 60 and no more than 80 beats per minute. This is the rhythm that is considered normal for the human body. and on the cardiogram it is displayed as teeth of the same size, located at the same distance from each other.
It is clearly worth remembering that the results of a cardiogram can be one hundred percent accurate only if the person is completely calm. Stressful situations and nervous tension contribute to the fact that the heart muscle begins to emit impulses faster, which means that it will definitely not be possible to obtain a reliable result about the state of a person’s health.
What criteria are used to decipher the ECG result?
The results of the cardiogram are deciphered by doctors according to a special scheme. Medical specialists have a clear understanding of which marks on the cardiogram are normal and which are abnormal. The ECG conclusion will be issued only after calculating the results, which were displayed in schematic form. A doctor, when examining a patient’s cardiogram in order to correctly and accurately decipher it, will pay special attention to a number of such indicators:
- the height of the bars displaying the rhythm of heart impulses;
- the distance between the teeth on the cardiogram;
- how sharply the indicators of the schematic image fluctuate;
- what specific distance is observed between the bars displaying the pulses.
A doctor who knows what each of these schematic marks means carefully studies them and can clearly determine what kind of diagnosis needs to be made. Cardiograms of children and adults are deciphered according to the same principle, but normal indicators for people of different age categories cannot be the same.
What sinus rhythm problems can be seen on an ECG?
Electrocardiogram readings can indicate clear signs of problems in the functioning of the heart muscles. With the help of this study, you can notice whether there is weakness of the sinus node, and what kind of health problems this causes. By looking at the cardiogram readings of a particular patient, a medical specialist can decipher the presence of problems of the following nature:
- sinus tachycardia on the ECG, indicating an excess of the contraction rhythm, which is considered normal;
- sinus arrhythmia on the ECG, indicating that the interval between contractions of the heart muscles is too long;
- sinus bradycardia on the ECG, indicating that the heart beats less than 60 times in one minute;
- the presence of too small an interval between the teeth of the cardiogram, which means disturbances in the functioning of the sinus node.
Sinus bradycardia is a common abnormality, especially when it comes to the health of a child. This diagnosis can be explained by many factors, among which may be physiological defects or simply a factor of chronic fatigue.
Deviation of the EOS to the left also indicates that the work of a vital organ is not working properly. Having identified such deviations, the doctor will send the patient for additional examination and ask him to undergo a number of necessary tests.
If a vertical position of the EOS is observed, this means that the heart has a normal location and is in its place, there are no serious physiological abnormalities. This situation is an indicator of the norm, which is also indicated in the conclusion of the doctor who deciphered the cardiogram.
If a horizontal position of the EOS is observed, then this cannot immediately be considered a pathological condition. Such axis indicators are observed in people who are short in stature but have fairly broad shoulders. If the axis deviates to the left or right, and this is very noticeable, then such indicators may indicate a pathological condition of the organ, an enlargement of the left or right ventricles. Axial displacement may indicate that certain valves are affected. If the axis shifts to the left, then the person most likely has heart failure. If a person suffers from ischemia, then the axis shifts to the right side. Such a deviation may also indicate abnormalities in the development of the heart muscle.
What can we say about normal indicators?
On an ECG, sinus rhythm is always and without fail compared with certain normal values. Only knowing these indicators completely will the doctor be able to understand the patient’s cardiogram and give the correct conclusion.
Normal indicators for children and adults are completely different factors. If we consider the norms for different age categories, they will be something like this:
- in children from birth to the first year of life, the direction of the axis is vertical, the heart beats with a heart rate of 60 to 150 beats per minute;
- children from one year to six years have a mainly vertical axis, but it can also be horizontal, without indicating deviations from the norm. Heart rate from 95 to 128;
- children from seven years of age and adolescents should have a normal or vertical axis position on the cardiogram, the heart should contract from 65 to 90 beats per minute;
- adults should have a normal axis direction on the cardiogram, the heart contracts at a frequency of 60 to 90 times per minute.
The above indicators fall under the category of the established norm, but if they are slightly different, this does not always become a sign of the presence of some serious pathologies in the body.
Why ECG readings may deviate from the norm
If the result of the electrocardiogram does not always correspond to the norm, this means that this state of the body could be provoked by the following factors:
- the person regularly drinks alcoholic beverages;
- the patient has been smoking cigarettes on a regular basis for quite a long time;
- a person is regularly exposed to various types of stressful situations;
- the patient often uses antiarrhythmic drugs;
- a person has problems with the functioning of the thyroid gland.
Of course, an accelerated heart rate or too slow may indicate problems of a more serious nature. If the results of the cardiogram are not normal, this may indicate acute heart failure, valve displacement, or congenital heart defects.
If the sinus rhythm is within the established norm, then the person should not worry, and the doctor will be able to make sure that his patient is healthy.
The sinus node regularly emits impulses that cause the heart muscles to contract correctly and carry the necessary signals throughout the body. If these impulses are given irregularly, which can be clearly recorded by a cardiogram, then the doctor will have every reason to assume that the person has health problems. After studying the heart rate, the doctor will determine the exact cause of all deviations and will be able to offer the patient competent treatment.
Why should a person undergo an ECG test?
The sinus rhythm, which is displayed on the ECG, clearly indicates whether there are deviations in the functioning of the heart and in which directions the problem is observed. Not only adults, but also children need to undergo such research regularly. The results of a completed cardiogram will help a person obtain the following information:
- does he have any congenital pathologies or diseases;
- What pathologies in the body cause heart problems;
- could a person’s way of life become the cause of disturbances in the functioning of the main organ;
- whether the heart is in the correct position and whether its valves are working correctly.
Normal sinus rhythm on an ECG is displayed as waves of the same size and shape, and the distance between them is also the same. If any deviations from this norm are observed, then the person will have to be further examined.
The sinus rhythm on the cardiogram must coincide with the established norm, and only in this case can a person be considered healthy. If impulses from the heart to other systems diverge too quickly or slowly, then this does not bode well. This means that doctors will have to further clarify the cause of the problem and engage in comprehensive treatment. If an uneven rhythm is observed on a teenager’s cardiogram, then this cannot be considered a pathological deviation, because such a condition may be associated with hormonal changes and the physiological maturation of the body.
If the sinus rhythm is within normal limits, then you will not have to undergo additional tests or repeat studies. Normal heart function, as well as pathological abnormalities, are always recorded by a cardiogram.
The sinus rhythm on the ECG should be smooth and clear, without any intermittent lines or too long or short intervals. If the presented indicators are normal, then we can safely say that the person is completely healthy. Deviations in the cardiogram are a reason for doctors to perform additional studies and prescribe tests. Only after additional examinations can we understand the exact cause of the deviations and begin treatment. A normal sinus rhythm is reflected by a clear and evenly spaced cardiogram. Additional attention will have to be paid to the location of the axis, regarding the parameters of which medical standards have also been established.