Mechanisms of thrombus formation
In a normally functioning body, blood clots form to prevent blood from flowing out of damaged vessels. When an injury occurs, accompanied by rupture of veins, arteries and capillaries, platelets in the blood are destroyed and thrombin and thromboplastin are released from them. Under the influence of the emerging components, fibrinogen (one of the components of blood serum) is converted into fibrin (protein), which accumulates on the walls of the damaged vessel, forming the basis of a blood clot.
Blood clots can partially close the venous lumen (parietal formations) or completely block the vessel, preventing the movement of blood (clogging).
Depending on the cells that form the blood clot, blood clots are distinguished:
- white – consist of platelets and leukocytes;
- red - based on red blood cells;
- mixed - include both the first and second.
The process of healthy thrombus formation helps restore normal blood flow, maintaining the integrity and vitality of organs and tissues.
Treatment
If the disease is in its initial stage, treatment does not require the patient to stay in the hospital. If the disease is in the acute phase, then hospital stay is mandatory. Since treatment requires strict bed rest.
Treatment is prescribed depending on the stage and development of ileofemoral thrombosis.
Conservative treatment
For this purpose, drugs such as:
- Antiplatelet agents: Aspirin, Cardiomagnyl, Dipyridamole.
- Direct anticoagulants: Heparin, Flenox, Novoparin.
- Indirect anticoagulants: Pradaxa, Warfarin, Marevan.
- Non-steroidal anti-inflammatory drugs: Diclofenac.
- Thrombolytics: Pharmakinase, Streptalyse.
During therapy, it is also possible to use painkillers and antispasmodics.
It is worth remembering that all medications have their contraindications.
Physiotherapy
Usually, procedures are prescribed that, as practice has shown, are the most effective. These include: UHF, magnetic therapy, electrophoresis with medicinal substances, paraffin baths.
In general, physical therapy eliminates swelling and pain quite quickly. At the same time, it normalizes blood circulation and is also considered the basis for preventing relapses.
Compression therapy
It can be considered a conservative method of treatment. This therapy helps improve the flow of lymph and blood. It is performed by bandaging the limbs with compression material, such as an elastic bandage, special stockings, tights. Therapy is prescribed in combination with bed rest.
Surgical treatment
When conservative treatment does not produce results, the doctor prescribes surgery. Since without surgery it is possible to develop: pulmonary embolism, the development of gangrene.
Reasons for development
The disease is provoked by:
- prolonged bed rest, the need to remain in a supine position;
- serious injuries to arms and legs;
- congenital anomalies associated with poor clotting, hemophilia,
- stagnation of blood in the veins;
- infectious diseases;
- treatment with hormonal medications;
- inflammation;
- suppuration;
- sepsis.
Predisposing factors to the occurrence of thrombosis are:
- pregnancy (due to intense hormonal changes, weight gain during this period);
- oncological neoplasms of a benign or malignant nature.
At risk are patients with diabetes mellitus, as well as people who are overweight.
Causes
The main cause of acute inflammation in the lower extremities is considered to be weakening of the walls of blood vessels and malfunctions of the venous valves. Normally, the valves prevent backward (downward) blood flow. If their structure is disrupted, venous return and stagnation occurs. This provokes blockage of blood vessels and further complicates the upward flow. The result of the pathological process is an increase in thrombotic masses.
The following factors can trigger the development of ileofemoral thrombosis:
- physical labor aimed at regularly lifting loads;
- weightlifting;
- “standing” work;
- passive lifestyle;
- obesity;
- pregnancy with a sharp increase in body weight and the early postpartum period;
- long-term use of hormones and birth control pills;
- prolonged bed rest;
- genetic inheritance to thrombosis;
- heavy blood loss;
- benign and malignant cancer tumors in the pelvic area.
Ileofemoral thrombosis usually affects one leg. Bilateral inflammation of the lower extremities is very rarely recorded. The risk of developing the disease increases when several unfavorable factors are combined.
Clinical manifestations
The disease manifests itself in characteristic symptoms. These are:
- severe swelling in the thigh area, spreading to the entire area of the lower extremities;
- change in the color of the epithelium (redness or bluishness of the skin appears);
- rashes of a brownish color (dark dots remain visible even after pressing on them);
- spasm, pain in the legs, in the groin area;
- feverish condition, general malaise.
Ileofemoral vein thrombosis, localized on the left or right, goes through several stages in its development. Symptoms become more severe as the disease progresses.
Prodromal stage
Characterized by:
- pain in the pelvic region, sacrum and legs;
- increase in temperature (local or general).
Stage of severe symptoms
Manifests:
- severe pain syndrome;
- swelling that covers the entire limb;
- decreased sensitivity in the legs;
- lack of pulsation in the vessels;
- pallor and bluishness of the skin, translucency of the venous network.
A patient who develops acute ileofemoral thrombosis requires immediate hospitalization.
Symptoms and diagnosis
The following manifestations are characteristic of acute ileofemoral thrombosis:
- Pain syndrome. Localized in the area of the inner thigh. Spreads to the calf muscles and groin area. It has a high intensity, pulling or aching character. The pain is constant or occurs in attacks. Unpleasant sensations intensify when palpating the affected veins.
- Swelling. Spreads to the groin, thigh and lower leg. With acute blockage of the veins, the limb quickly increases in volume. In some cases, swelling spreads to the gluteal muscles.
- Change in skin color. In the early stages, the skin has a pale tint. In the later stages of the disease, pallor gives way to cyanosis. Dark purple spots appear on the skin.
- Decreased sensitivity of the lower extremities. Impaired blood flow negatively affects the condition of nerve endings, causing them to stop receiving impulses. The patient feels a feeling of coldness in the area of the feet and legs.
Important information: What antithrombosis herbs (drugs) thin the blood from blood clots
Blue painful phlegmasia is considered the most dangerous form of the disease, characterized by occlusion of all deep veins. She calls:
- severe bursting pain;
- severe swelling of the leg;
- the appearance of blisters with bloody or serous contents;
- absence of arterial pulsation.
To identify the disease use:
- Analysis of Lowenberg's symptom. The lower leg is compressed with a tonometer cuff; inflating the device to certain levels does not cause pain if the blood vessels are in normal condition. With thrombosis, pain occurs when the cuff is inflated to 80 mmHg. Art.
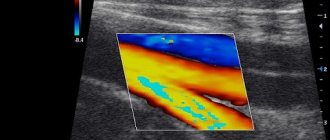
- Duplex scanning of blood vessels. Vascular ultrasound helps to obtain a color image, with the help of which the localization of thrombotic masses is determined. The density of the thrombus depends on the stage of the disease. With ileofemoral thrombosis, pronounced varicose veins are detected. The affected vessel does not respond to compression.
- X-ray examination of the vascular system of the pelvis. Used to diagnose thrombosis of veins located above the inguinal fold. Due to the presence of gas bubbles in the intestine, ultrasound examination of this area may give incorrect results.
- Radionuclide phlebography. The method is used for allergic reactions to a contrast agent. Fibrinogen labeled with radioactive isotopes is injected into a vein.
Diagnostic methods
After a visual initial examination and medical history, the doctor prescribes the patient to undergo a series of diagnostic tests. Among them:
- Duplex ultrasound of leg vessels. Provides a color image of the circulatory network, makes it possible to assess the patency of veins and arteries, determines the presence of blood clots in their lumen, and evaluates their density.
- X-ray contrast venography (descending or ascending). It is carried out if a threat of a blood clot in the groin area is suspected. It is an X-ray scan using contrast.
- Radionuclide phlebography. An image of the deep veins is created using a machine that emits radio waves. To make the picture clearer, a contrast agent is also injected intravenously.
Based on the results of all studies performed, the attending physician establishes an accurate diagnosis and prescribes an appropriate regimen of health-improving measures.
Be healthy!
Ileofemoral thrombosis is a lesion of the deep veins of the lower extremities associated with blockage of blood flow by thrombotic masses at the level of the iliofemoral segment. Vessel occlusion disrupts venous hemodynamics, which is manifested by fever, soft tissue swelling, pain, and changes in skin color on the side of the blockage. The diagnosis takes into account clinical data, the results of a biochemical blood test (thrombosis markers, coagulogram), ultrasound scanning of blood vessels and venography. The treatment program includes conservative correction (medication, compression therapy) and endovascular interventions.
General information
Ileofemoral (ilio-femoral) thrombosis is a dangerous type of phlebothrombosis in the inferior vena cava system with a high risk of complications. This is a fairly common disease - it accounts for 25% of all thrombotic lesions of deep vessels (1-2 cases per 1000 population annually). The frequency of blockage of the proximal sections of the venous system of the lower extremities is 3 times higher than the distal ones. After 50 years, the incidence of pathology increases exponentially, amounting to more than 300 cases per 100 thousand people in old and senile age. Women suffer from thrombotic conditions twice as often.
Causes
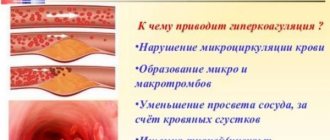
The onset of the disease is provoked by a number of factors that trigger the formation of intravascular blood clots. Pathological prerequisites are known as Virchow's triad - slowing of blood flow (stasis), changes in the rheological properties of blood (hypercoagulation), injury to the vascular wall. Damage to the ileofemoral segment occurs due to various reasons:
- Endothelial damage. The likelihood of thrombosis increases with invasive interventions (vascular catheterization), operations (on large joints, abdominal and pelvic organs), and fractures. Intravascular devices (stents, filters, artificial valves) and some biochemical disorders (hyperhomocysteinemia) have a damaging effect.
- Long-term adynamia. Phlebothrombosis often occurs due to prolonged immobilization of the lower extremities due to immobilization, anesthesia with muscle relaxants, paralysis, and strict bed rest. A similar mechanism is used during long air flights and car trips.
- Obstructions to blood flow. Slowing of hemodynamics in the iliac vessels occurs due to congenital and acquired mechanical obstacles (septa, adhesions). Extravasal (external) prerequisites for stasis are realized in May-Thurner syndrome (interruption of the vena cava), compression by tumors.
- Thrombophilia. The tendency to thrombus formation is due to a number of hereditary abnormalities of the coagulation system (deficiency of proteins C and S, pathological plasminogen, antithrombin deficiency). Of the acquired thrombophilias, an important role is played by antiphospholipid syndrome and dysfibrinogenemia.
The incidence of thrombotic disorders increases significantly in the third trimester of pregnancy and in the first week of the postpartum period. They are found in malignant tumors, cardiovascular pathology (myocardial infarction, stroke, cardiac decompensation), nephrotic syndrome and other diseases.
The occurrence of ileofemoral thrombosis is also influenced by age over 40 years, smoking, excess body weight, and taking certain medications (oral contraceptives, chemotherapy drugs). Typically, the disease develops due to a combination of several causes and risk factors.
Pathogenesis
Venous congestion contributes to an increase in the amount of activated coagulation factors, endothelial hypoxia, and the accumulation of thrombotic material. Damage to the wall is accompanied by the production of cytokines and stimulation of platelet aggregation. Exposure of the subendothelial layer only exacerbates this process, promoting the adhesion of blood platelets and activation of the coagulation cascade. Clot formation is accelerated by thromboplastin coming from damaged tissues.
Phlebothrombosis is characterized by constantly increasing obstruction of the vascular lumen, which only increases the severity of stasis. Laminar blood flow is replaced by turbulent one, the number of coagulation factors increases. Further development of ileofemoral thrombosis can occur in several ways: spontaneous lysis of pathological masses, spread in proximal or distal directions, avulsion and embolization, organization with the formation of persistent occlusion, partial recanalization.
Classification
Blockage of the ileofemoral segment is part of the structure of deep vein thrombosis of the lower extremity, being its central (proximal) type. According to the classification most common in clinical phlebology, there are several types of blood clots according to the nature of their attachment:
- Floating (oscillating). It is characterized by the presence of only one point of fixation to the vessel wall. Depending on the length, it can be segmented and widespread with a floating tip. The most dangerous from the point of view of embolization.
- Parietal. The thrombus is tightly attached to the venous wall. It does not completely obstruct the lumen of the ileofemoral segment (most of it remains free).
- Occlusive. Almost completely blocks the blood flow in the venous bed. It is a consequence of the progression of the parietal clot. Both of the latter types are considered non-embolic.
The thrombotic process can be descending, ascending, or spreading in both directions. Occurring in unchanged veins, it is primary, and when it develops again, the disease is recurrent. Left-sided phlebothrombosis is usually observed - the right iliofemoral area is affected three times less often.
Based on the clinical picture, ileofemoral thrombosis can be symptomatic or asymptomatic. Manifest variants go through two stages - compensation and decompensation. Taking into account the likely consequences, there are uncomplicated and complicated forms. According to clinical criteria, the degree of risk of thromboembolism is determined (high, moderate, low).
Symptoms
The primary process in many cases proceeds latently and asymptomatically until a hemodynamically significant occlusion of the femoroiliac segment occurs, spread over a significant distance, or detachment of a floating clot. The disease begins in the prodromal stage, when there is no significant disturbance of venous blood flow. During this phase, the risk of embolism is especially high, which is due to weak fixation of the clot with preserved hemodynamics.
At an early stage, the clinical picture is limited only to fever (without connection with other causes) and pain. An increase in temperature sometimes becomes the only sign of latent thrombosis. Pain affects the lumbosacral region, lower abdomen and limb on the affected side. At first they are localized near the inguinal fold and are of an unexpressed nature, but as the process spreads, they descend to the distal areas. Fever and pain are associated with inflammatory phenomena (phlebitis and periphlebitis), venous hypertension.
At the stage of pronounced clinical manifestations, patients are bothered by intense pain along the anterior inner surface of the thigh, in the calf muscles, and in the groin area. The affected limb increases in volume with swelling spreading from the foot to the buttock (sometimes moving to the genitals and the anterior abdominal wall). As a result of venous stagnation, the skin acquires a pale cyanotic color and becomes tense. There is a feeling of heaviness and swelling in the leg. The limb is warm to the touch, dense, with painful cords in the groin and femoral areas. After 3–4 days, the swelling decreases, and an enhanced pattern of subcutaneous vessels becomes visible.
Complications
The most serious and frequent complication of ileofemoral thrombosis is pulmonary embolism (PE) - occurring in 60 cases per 100 thousand population, it becomes fatal for 15–20% of patients. Alarming symptoms may occur in the early stages as the only manifestation of phlebothrombosis. Non-embolic forms lead to progressive venous insufficiency and the development of postthrombophlebitic disease.
Complicated pathologies include white and blue phlegmasia. The first is caused by severe swelling and compression of the skin capillaries (white lower limb syndrome). Blue painful phlegmasia, although undergoing reverse development, in some cases becomes the source of an extremely dangerous condition - venous gangrene with necrotic changes in tissues and signs of circulatory failure (hypovolemic shock).
Diagnostics
Ileofemoral thrombosis is identified based on anamnestic data (complaints, risk factors, history of the disease) and the results of a physical examination of the patient. To clarify the diagnosis and determine the localization of the clot, laboratory and instrumental methods are needed:
- Blood chemistry. Intravascular thrombus formation is confirmed using rapid tests, examining the level of D-dimer, fibrin degradation products, and soluble fibrin-monomer complexes (SFMC). The state of the coagulation system is analyzed using a coagulogram (prothrombin, thrombin, activated partial thromboplastin time, fibrinogen).
- Ultrasound scanning of the venous system. Duplex angioscanning allows you to visualize the internal structure of the affected areas, assess blood flow, and characteristics of blood clots. The diagnosis is confirmed by detecting echo-positive masses, an increase in the diameter of the vessels, and no response to compression by the sensor.
- Phlebography of the involved areas. X-ray contrast venography is used to identify floating clots when their apex is poorly visualized by ultrasound. Important signs of acute thrombosis include the phenomenon of amputation of the main veins, the presence of filling defects in the lumen, expansion of distal areas, and delayed removal of contrast.
Instead of traditional X-ray examination, CT venography can be used, which provides a three-dimensional image of the vascular system. In difficult cases, radioisotope scintigraphy helps to assess hemodynamic parameters, and plethysmography helps to study venous filling during exercise and at rest. Sometimes phlebotonometry is performed to measure the pressure in the vessels and determine the function of the valves.
Patients with suspected ileofemoral phlebothrombosis need the help of a vascular surgeon or phlebologist. Consultation with a hematologist and geneticist is necessary if hereditary thrombophilia is suspected; pregnant women require a gynecologist's opinion. Differential diagnosis is carried out with edema due to lymphostasis, circulatory failure, trauma, preeclampsia in pregnant women. It is necessary to exclude arterial thrombosis, anaerobic infection, and prolonged tissue crush syndrome.
Treatment
Acute thrombosis is an indication for hospitalization in a surgical hospital. Treatment has several objectives: to prevent progression of the process and the development of complications, restore patency of the affected areas, and minimize the risk of relapse. The following methods are used for this:
- Medication correction. Thrombolytics (streptokinase, celiac, alteplase) help dissolve the formed clot; further spread of the process is prevented by anticoagulants (unfractionated heparin and low molecular weight variants, warfarin). To improve the rheological parameters of the blood, antiplatelet agents (acetylsalicylic acid, dipyridamole, pentoxifylline) are prescribed, and ointments with heparin and non-steroidal anti-inflammatory drugs are applied topically.
- Compression therapy. In the structure of conservative measures, a special place is occupied by measures to improve the outflow of blood and lymph. Compression therapy involves elastic bandaging the limb and wearing special clothing (stockings, knee socks, tights). In combination with bed rest and postural drainage (elevating the limb), this can reduce venous hypertension.
- Endovascular surgery. Intravascular access operations are aimed at preventing embolization and restoring the patency of thrombosed areas. Endovascular technologies include regional selective thrombolysis and implantation of vena cava filters. In severe forms of pathology with a risk of gangrene, emergency thrombectomy is performed (in the first 3–4 days of the disease). As a radical solution, if there is a high probability of pulmonary embolism and it is impossible to install a vena cava filter, plication (rare suturing) of the vena cava can be performed in the area below the origin of the renal branches.
Prognosis and prevention
Lack of treatment in 20% of cases leads to the development of pulmonary embolism, but through active anticoagulant therapy it is possible to reduce mortality by 5–10 times. Within 5 years after therapy, a quarter of patients experience a recurrence of ileofemoral thrombosis. The vast majority of victims require a medical and social examination of their ability to work with the establishment of a disability group. Primary prevention of the disease is advisable when there is a high risk of thrombosis. It includes preventing injury, maintaining a sufficient level of physical activity, treating underlying pathology, and using low molecular weight heparins and compression stockings.
Conservative therapy
If, as a result of diagnostic procedures, the presence of pathology was established, then the following groups of medications are prescribed for the treatment of ileofemoral thrombosis:
- anti-inflammatory drugs (“Ibuprofen”, “Diclofenac”, “Troxerusin”, “Ketonal”): stop inflammatory processes, fight infections, reduce painful manifestations;
- antiplatelet agents (“Abciximab”, “Dipyrimadol”, “Indobufen”): prevent the formation of blood clots, preventing them from sticking together and blocking blood vessels;
- anticoagulants: taken to thin the blood
Heparin, a direct-acting drug, is injected; after a few days, Warfarin and Syncumar are prescribed.
Only a specialist can adequately assess the patient’s condition and prescribe the correct drug therapy. Self-medication of the disease is fraught with serious negative consequences for the patient’s health.
Therapy
Treatment of ileomephoral thrombosis occurs in a hospital setting; conservative traditional methods are most often used; surgical intervention is very rarely resorted to.
If you have been diagnosed with this, then in general treatment will consist of the following methods:
- Use of medications.
- Thrombolysis and similar procedures.
If there is a risk of a blood clot breaking off, which can lead to blockage of the pulmonary artery, the disease in the legs is cured by installing special vena cava filters. These filters can catch a blood clot if it detaches from the wall of a vein and travels through the bloodstream to the heart.
If the doctor has made a clear diagnosis of ileofemoral thrombosis, then therapy will begin with the use of the following medications:
- Means for oral administration.
- External agents, anticoagulants.
- Medicines that can thin the blood.
- Agents that relieve inflammation.
At the initial stages of the disease, a technique can be used to dissolve formed blood clots.
Radical treatment measures
In some situations, there is a need to use radical methods of treating the disease, which involve removing the blood clot. Surgical intervention is prescribed in cases such as:
When there is a threat of gangrene of the venous vessels.
A thrombotic type process that spreads over the area of the inferior vein.
If necessary, the surgeon will give a recommendation for a procedure to eliminate blood clots. This procedure is retrograde in nature. During this operation, the doctor makes a small incision near the femoral vein.
Often such treatment cannot be carried out. There is also a contraindication to this procedure: the presence of adhesions in the venous lumens.
Patients must begin treatment immediately, otherwise there will be a risk of complications, pulmonary embolism in particular . The use of preventive measures that focus on strengthening the walls of venous vessels and have a general therapeutic effect will help avoid the disease.
Surgical methods
Surgical treatment of thrombosis is carried out if the disease has already entered the second stage of development, as well as when drug therapy is ineffective and does not produce visible positive results.
The operation is carried out through:
- installation of filters in the inferior vena cava of the extremities;
- dissection of the vessel using sutures, thereby creating new blood channels;
- regional thrombolysis - injection into a vein or artery through a catheter of a thrombus-resorbable substance (streptase);
- surgical removal of a blood clot: this method is used if there is severe pain, severe swelling and blue discoloration of the limb
The procedure is fraught with the development of complications and death of the patient.
Removal of a blood clot is carried out by:
- removing it through a catheter installed in the operated area;
- complete excision of the pathological vein.
Treatment of ileofemoral thrombosis
All patients without exception with an established diagnosis of “ileofemoral thrombosis” are required to be hospitalized in an angiosurgical hospital. The patient must be transported in a supine position. Until medical assistance is provided, he must adhere to the strictest bed rest. If it is not possible to perform a qualitative examination of the victim, then he is prescribed anticoagulants, fibrinolytics and thrombolytics for up to 10 days.
General recommendations for the management of patients with acute ileofemoral thrombosis:
- Anticoagulant drugs: low molecular weight Heparin, Logiparin, Fraxiparin.
- Eliminating pain, removing the patient from a state of shock.
- Relieving spasm from blood vessels, normalizing hemodynamics.
- Drugs for thrombolysis: Streptokinase or Urokinase. However, it should be remembered that the use of thrombolytic drugs is always associated with the risk of bleeding and death of the patient. Therefore, thrombolysis drugs are prescribed only to patients under the age of 50 years in whom acute thrombosis occurred no later than 7 days before visiting the doctor. In this case, patients must have vena cava filters installed, otherwise there is a high probability of small particles of a blood clot spreading through the bloodstream and developing a pulmonary embolism.
- Fibrinolysis activator drugs: Complamin, Teonicol, Nicotinic acid (intravenous administration), Pyrogenal (intramuscular administration).
- Normalization of rheological blood parameters is carried out with the help of drugs Trental, Eufillin, Actovegin, etc.
- If inflammation develops, antibiotics are indicated.
Surgery for ileofemoral thrombosis is prescribed only for vital indications: if the patient is diagnosed with floating blood clots that pose a threat to pulmonary embolism, or if complications of thrombosis develop. These include: embologenic thrombosis, a high risk of developing gangrene against the background of blue phlegmasia, ascending thrombosis.
There are also relative indications for surgery, including:
- Lack of effect from drug treatment for 2-3 days.
- The duration of thrombosis is more than 8 days.
- Senile age.
Thrombectomy is the main method of surgical intervention for ileofemoral thrombosis. It should be remembered that with blue phlegmasia, conservative therapy is useless in 100% of cases. The prognosis for blue phlegmasia is largely determined by how timely the surgical intervention was performed (before the development of gangrene). In this case, patients are indicated for radical throbectomy. The risk of pulmonary embolism increases when thrombectomy is performed on the right iliac vein.
Complications and prognosis
Vein thrombosis is a disease that is classified as severe due to the fact that there is a high risk of complications. During illness, pulmonary embolism (PE) can occur - blockage of this vessel by a formed blood clot, which is fraught with death for the patient. A threat can be caused by incorrectly prescribed treatment or the patient’s failure to comply with all the instructions given by the doctor. At risk are patients who have genetic abnormalities, excess body weight, cardiac disorders, varicose veins, erythremia, cancer diseases, as well as people leading a sedentary lifestyle, elderly citizens, and women who have had a difficult birth.
Due to the development of thrombosis of deep blood vessels, there is a risk of tissue necrosis and gangrene due to cessation of blood circulation in the vessels of the lower extremities.
There is no complete confidence in the positive outcome of treatment, since a high probability of complications remains even if a special filter is installed. If the pathology is detected in childhood, the prognosis is often favorable.
The disease can be overcome if drug therapy is correctly prescribed, and also if all the instructions of the treating specialist are strictly followed.
Diagnostic methods
Ultrasound with duplex scanning is considered an informative and simple method. It helps to examine the lumen of the venous vessels of the lower extremity along their entire length, identify the location and degree of their blockages, visualize a blood clot and its attachment to the wall, and detect a dangerous floating blood clot that can break off in the near future.
The blocked vein becomes dense, its radius increases, and thrombotic masses are found inside.
If the ultrasound failed to clearly see the thrombus, then venography is prescribed.
Signs of acute vein thrombosis are:
- lack of contrast flow into the vein (vessel disconnection);
- filling defects;
- flow around the thrombus (contrast stripes similar to rails are visible);
- the tip of the clot floats above the blockage or moves further along the vessel;
- indirect symptoms – dilated popliteal veins, prolonged contrast delay.
Phlebography is performed with traditional X-ray control, and in complex cases of the disease it is combined with magnetic resonance imaging or radionuclide scanning with isotope-labeled fibrinogen.
Prevention
The main measures to prevent phlebothrombosis of the deep veins of the legs are:
- compliance with the diet: eating a large amount of greens, fresh vegetables and fruits, cereals, legumes; together with them, a person receives the required amount of vitamins and beneficial microelements;
- maintaining a healthy lifestyle: regular exercise, quitting smoking and drinking alcohol;
- organization of optimal sleep and rest patterns;
- wearing compression garments;
- treatment of diseases of the hematopoietic system.
In order not to miss the appearance of the initial stage of thrombosis, you should undergo preventive medical examinations in a timely manner, and if you experience discomfort in your legs, seek qualified help.
Causes of the disease
Ileofemoral thrombosis of the lower extremities can occur due to slow blood flow and clotting problems. The disease develops both for one specific reason and for a combination of them.
There are several provoking factors that are identified by doctors. They differ in that they are a certain mechanism for triggering the development of this disease:
- Prolonged stay in bed.
- Injury to limbs.
- Ingress of infections and bacteria.
- Long-term use of oral contraceptives without medical supervision.
- Pregnancy period.
- Recovery after childbirth.
- Oncological pathologies based in the pelvic organs.
- Toxic effects of medications.
- Cyst under the knee.
In most cases, ileofemoral phlebothrombosis begins to develop due to the fact that congestion in the veins occurs due to a lack of valves, the process of bearing a child and a long-term lack of motor activity in the legs.
The second provoking factor in terms of its “popularity” is blood clotting diseases, thrombophilia. After you have found out what the causes of the disease are, it is worth talking about its signs.
Prevention of the disease
To completely avoid thrombosis, you need to carefully monitor your lifestyle. You need to be moderately active and also eat right. It is necessary to eliminate all bad habits.
If the disease begins to develop, it is necessary to follow preventive measures aimed at preventing complications. This includes the elimination of risk factors, an adequate activity regimen, as well as correctly selected antiplatelet and anticoagulant therapy.
Although ileofemoral thrombosis is a serious threat to human health, it is still treatable, especially if it is started on time. The most important thing is not to give up and follow the doctor’s recommendations.
How is diagnosis carried out?
Most often, ileofemoral phlebothrombosis manifests itself with characteristic symptoms only at the late (acute) stage of its development, when the body no longer has the ability to compensate for impaired blood circulation. This is why people turn to a doctor when serious changes in tissues have already begun to occur.
To correctly diagnose the disease, the doctor listens to the patient’s complaints, collects anamnesis, conducts an external examination, and prescribes laboratory and instrumental tests:
| Study | Why is it carried out? |
| Ultrasound with duplex scanning | Thanks to this study, the condition of the vessels and blood flow is assessed. It is also determined whether there are changes in the vascular walls, narrowing of the lumen, atherosclerotic plaques, or blockage of the vessel. |
| Contrast venography | With its help, the patency of blood vessels and the level of damage are determined. |
| Radionuclide phlebography | Prescribed if the patient is contraindicated to administer contrast. Gives the same result as contrast. |
| MRI | A highly informative method that allows you to study in detail the structure of tissues and the condition of blood vessels. |
Possible complications
Ileofemoral thrombosis is a dangerous disease that is fraught with many complications. If the venous vessels in the thigh and groin area are thrombosed, acute venous insufficiency may occur.
When the lumen is completely blocked by a blood clot, gangrene of the leg develops. A person’s body temperature rises, blood pressure decreases, the pulse becomes weak and rapid, and the limb begins to turn black. If the iliac vein is damaged, the patient complains of pain in the abdomen and the functioning of the intestines is disrupted.
The most dangerous consequence is pulmonary thromboembolism. Blood clots obstruct the movement of blood through the pulmonary artery, leading to pulmonary infarction, heart failure, and respiratory failure.