| Ventricular septal defect | |
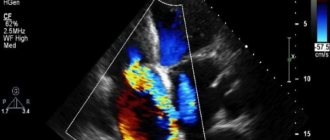
| Echocardiographic image of a ventricular septal defect in the muscular part. | |
| ICD-10 | 21.021.0 |
| ICD-9 | 745.4745.4 |
| OMIM | 614429, 614431, 614432, 614429, 614431 and 614432 |
| DiseasesDB | 13808 |
| MedlinePlus | 001099 |
| eMedicine | med/3517 |
| MeSH | D006345 and D006345 |
Ventricular septal defect
Ventricular septal defect
(VSD) is a congenital heart defect characterized by a defect between the right and left ventricles of the heart.
Epidemiology
Play media file
Video with subtitles
Ventricular septal defect (VSD) is the most common, both in isolated form and as part of many other heart defects. Among congenital heart diseases, the frequency of this defect varies from 27.7 to 42%.[1] It is equally common in both boys and girls. There is evidence of autosomal dominant and recessive types of inheritance. In 3.3% of cases, direct relatives of patients with VSD are also found to have this defect.[2]
Possible complications of IVS hypertrophy
What complications are possible with the development of cardiopathy of the type under discussion? Everything will depend on the specific case and individual development of the person. After all, many will never know throughout their lives that they have this condition, and some may experience significant physical ailments. We list the most common consequences of thickening of the interventricular septum. So:
1. Heart rhythm disturbances such as tachycardia. Such common types as atrial fibrillation, ventricular fibrillation and ventricular tachycardia are directly associated with IVS hypertrophy. 2. Disorders of blood circulation in the myocardium. Symptoms that occur when the outflow of blood from the heart muscle is disrupted include chest pain, fainting and dizziness. 3. Dilated cardiomyopathy and the associated decrease in cardiac output. The walls of the heart chambers, under conditions of pathologically high load, become thinner over time, which is the cause of the appearance of this condition. 4. Heart failure. The complication is very life-threatening and in many cases ends in death. 5. Sudden cardiac arrest and death.
Of course, the last two conditions are terrifying. But, nevertheless, with a timely visit to the doctor, if any symptom of cardiac dysfunction occurs, a timely visit to the doctor will help you live a long and happy life.
Classification
The interventricular septum has 3 sections: the upper part is membranous
, adjacent to the central fibrous body, the middle part is
muscular
, and the lower part is
trabecular
. Accordingly, these departments are also called ventricular septal defects, but most of them have perimembranous localization (up to 80%). Muscular VSDs account for 20%[1][3].
Based on size, defects are divided into large
,
medium
and
small
. To correctly assess the size of the defect, its size must be compared with the diameter of the aorta. Small defects measuring 1-2 mm, located in the muscular part of the interventricular septum, are called Tolochinov-Roger disease. Due to the good auscultatory picture and the absence of hemodynamic disturbances, the expression “much ado about nothing” is appropriate to characterize them. Separately, there are multiple large defects of the interventricular septum, of the “Swiss cheese” type, which have an unfavorable prognostic value [3].
Reasons for development
The defect forms in the fetus from 3 weeks to 2.5 months of intrauterine development. If the course of pregnancy is unfavorable, pathologies may occur in the structure of internal organs. Factors that increase the risk of VSD:
- Heredity. Predisposition to VSD can be transmitted genetically. If one of your close relatives has had defects of various organs, including the heart, there is a high probability of abnormalities occurring in the child;
- Viral diseases of an infectious nature (influenza, rubella) that a woman suffered in the first 2.5 months of pregnancy. Herpes and measles are also dangerous;
- Taking medications - many of them can cause intoxication of the embryo and lead to the formation of various defects. Particularly dangerous are antibacterial, hormonal, anti-epileptic drugs and those affecting the central nervous system;
- Bad habits of the mother - alcohol, smoking. This factor, especially at the beginning of pregnancy, increases the risk of abnormalities in the fetus several times;
- The presence of chronic diseases in a pregnant woman - diabetes, problems of the nervous, cardiac system and the like can provoke pathologies in the baby;
- Vitamin deficiency, deficiency of essential nutrients and microelements, strict diets during pregnancy increase the risk of birth defects;
- Severe toxicosis in early pregnancy;
- External factors - hazardous environmental conditions, harmful working conditions, increased fatigue, overexertion and stress.
The presence of these factors does not always cause severe illness, but it increases the likelihood. To reduce it, you need to limit their exposure as much as possible. Timely measures taken to prevent problems in the development of the fetus are a good prevention of congenital diseases in the unborn child.
Hemodynamics
Intracardiac hemodynamic disturbances in VSD begin to form some time after birth, usually on days 3–5 of life.[4] In the early neonatal period, a heart murmur may be absent due to equal pressure in the right and left ventricles due to the so-called neonatal pulmonary hypertension. A gradual drop in pressure in the pulmonary artery system and in the right ventricle creates a pressure difference (gradient) between the ventricles, resulting in a discharge of blood from left to right (from an area of high pressure to an area of low pressure). [5][6] The additional volume of blood entering the right ventricle and pulmonary artery leads to congestion of the pulmonary circulation vessels, where pulmonary hypertension develops.
There are three stages of pulmonary hypertension according to V.I. Burakovsky
.
- Blood stagnation ( hypervolemic stage of pulmonary hypertension
) can lead to pulmonary edema, frequent infection, and the development of pneumonia that manifests in early life, has a severe course and is difficult to treat.
If hypervolemia cannot be managed with conservative methods, in such cases a palliative operation is performed - narrowing of the pulmonary artery according to Muller
. The essence of the operation is to create a temporary artificial stenosis of the pulmonary artery, which prevents excess blood from entering the ICC. However, the increased load that falls on the right ventricle dictates in the future (after 3-6 months) the need for radical surgery.[7] - During the natural course of the defect, over time, the Kitaev reflex (spasm in response to overdistension) is triggered in the vessels of the pulmonary circulation, which leads to the development of a transitional stage of pulmonary hypertension
. During this period, the child stops getting sick, becomes more active, and begins to gain weight. The stable condition of the patient during this phase is the best period for radical surgery.[7] The pressure in the pulmonary artery (and accordingly in the right ventricle) during this phase ranges from 30 to 70 mm Hg. Art. The auscultatory picture is characterized by a decrease in noise intensity with the appearance of an accent of the second tone above the pulmonary artery.[3] - Subsequently, if surgical correction of congenital heart disease is not performed, processes of hardening of the pulmonary vessels begin to form ( high pulmonary hypertension
- Eisenmenger syndrome). This pathological process does not develop in reverse and leads to a significant increase in pressure in the pulmonary artery (sometimes up to 100-120 mm Hg).[3]
Auscultation can be heard as a pronounced accent of the second tone over the pulmonary artery (“metallic” tint).[8] Systolic murmur becomes weakly intense, and in some cases may be completely absent. Against this background, it is possible to record the appearance of a new diastolic murmur caused by insufficiency of the pulmonary valves (Graham-Still murmur).[8] The clinical picture of the disease shows many pathological signs: cardiac “hump”, expansion of the boundaries of relative cardiac dullness, more to the right. Areas of weakened and harsh breathing can be heard over the lungs, and wheezing may occur. The most characteristic sign of Eisenmenger syndrome is a gradual increase in cyanosis, first peripheral, and later diffuse. This occurs due to cross-discharge of blood in the area of the ventricular septal defect, which, when the pressure in the right ventricle exceeds, becomes right-left, that is, changes its direction. The presence of stage 3 pulmonary hypertension in a patient may be the main reason for cardiac surgeons to refuse to perform an operation.[4]
What is septal hypertrophy?
It is important to know! An effective remedy for normalizing heart function and cleaning blood vessels exists!
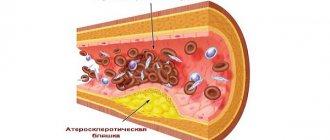
... One of the characteristic symptoms of hypertrophic cardiomyopathy is hypertrophy of the IVS (interventricular septum). When this pathology occurs, thickening of the walls of the right or left ventricle of the heart and the interventricular septum occurs. This condition itself is a derivative of other diseases and is characterized by an increase in the thickness of the walls of the ventricles.
Despite its prevalence (IVS hypertrophy is observed in more than 70% of people), it is most often asymptomatic and is detected only during very intense physical activity. After all, hypertrophy of the interventricular septum itself is its thickening and the resulting reduction in the useful volume of the chambers of the heart. As the thickness of the cardiac walls of the ventricles increases, the volume of the heart chambers also decreases.
In practice, this all leads to a reduction in the volume of blood that is released by the heart into the vascular bed of the body. To provide the organs with a normal amount of blood under such conditions, the heart must contract stronger and more often. And this, in turn, leads to its early wear and tear and the occurrence of diseases of the cardiovascular system.
Clinical picture
The clinical picture of VSD consists of a symptom complex of heart failure, which usually develops at 1-3 months of life (depending on the size of the defect).[6] In addition to signs of heart failure, VSD can manifest with early and severe pneumonia. When examining a child, you can identify tachycardia and shortness of breath, expansion of the boundaries of relative cardiac dullness, and a displacement of the apex impulse down and to the left. In some cases, the symptom of “cat purring” is identified. The systolic murmur, as a rule, is intense, heard over the entire region of the heart, well carried to the right side of the chest and to the back with maximum intensity in the IV intercostal space to the left of the sternum. Palpation of the abdomen reveals hepatomegaly and splenomegaly. Changes in peripheral pulsation are not typical. Children with VSD usually develop hypertrophy quickly.
Therapeutic measures for VSD
If in a small child the hole does not close until 12 calendar months of life, but does not increase, then drug treatment is carried out. Such a small patient is under the supervision of a doctor until the age of three.
Small areas of the defect heal on their own, and there is no need to take medications. If the defect remains the same, then you need to take medications.
Prescribed groups of drugs:
- Cardiac glycosides - can increase the functionality of the myocardium and regulate the heart rhythm - the drug Digoxin, Korglykon;
- Diuretics - reduce the blood pressure index (blood pressure), and also remove excess fluid from the body - Indapamide, Furosemide;
- Group of cardioprotectors - improves myocardial nutrition, increases its work - medication Riboxin, Panangin;
- Anticoagulants - prevent blood clots from forming - the drug Phenilin;
- Beta blockers - normalize proper contraction of the heart muscle - the drug Bisoprol;
- ACE inhibitors - Captopril.
A woman should begin preventive measures to prevent VSD pathology before conceiving a child. Before planning a pregnancy, it is worth getting your body vaccinated and performing laboratory tests.
During the period of bearing a child, especially in the first trimester of intrauterine development of the fetus, a woman must avoid hypothermia, viruses (chickenpox, measles, rubella) and infections that can negatively affect the intrauterine development of the heart organ and vascular system.
Diagnostics
Diagnosis of any heart defect consists of an X-ray examination of the chest organs, electrocardiography and two-dimensional Doppler echocardiography.
During X-ray examination
chest organs describe the shape of the heart and the state of the pulmonary pattern, and determine the size of the cardiothoracic index (CTI).
All these indicators have their own characteristics for different degrees of pulmonary hypertension. In the first, hypervolemic stage
, a flattened waist and immersion of the apex of the heart into the diaphragm, and an increase in CTI are revealed.
From the side of the pulmonary pattern, its intensification, indistinctness, and blurriness are noted. The extreme degree of hypervolemia in the lungs is pulmonary edema. In the transitional stage
of pulmonary hypertension, normalization of the pulmonary pattern and some stabilization of the size of the CTI are noted.
The sclerotic stage
of pulmonary hypertension is characterized by a significant increase in the size of the heart, mainly due to the right sections, enlargement of the right atrium (formation of a right atrio-vasal angle), bulging of the pulmonary artery arch (Moore index more than 50%), elevation of the apex of the heart, which forms a aperture acute angle. In terms of the pulmonary pattern, the symptom of a “cut tree” is often described: bright, clear, enlarged roots, against the background of which the pulmonary pattern can be traced only to a certain level. On the periphery there are signs of emphysema. The chest has a swollen shape, the course of the ribs is horizontal, the diaphragm is flattened and stands low.[7]
ECG
has its own patterns, closely related to the phase of the course of congenital heart disease and the degree of pulmonary hypertension. First, signs of left ventricular overload are revealed - an increase in its activity, then the development of its hypertrophy. Over time, signs of overload and hypertrophy of the right parts of the heart - both the atrium and the ventricle - appear - this indicates high pulmonary hypertension. The electrical axis of the heart is always deviated to the right. Conduction disturbances may occur, ranging from signs of incomplete right bundle branch block to complete atrioventricular block.[8]
With Doppler echocardiography
The location of the defect and its size are specified, and the pressure in the right ventricle and pulmonary artery is determined. In the first stage of pulmonary hypertension, the pressure in the pancreas does not exceed 30 mmHg, in the second stage - from 30 to 70 mmHg, in the third - more than 70 mmHg[4]
What is septal hypertrophy?
It is important to know! An effective remedy for normalizing heart function and cleaning blood vessels exists! ...
One of the characteristic symptoms of hypertrophic cardiomyopathy is hypertrophy of the IVS (interventricular septum). When this pathology occurs, thickening of the walls of the right or left ventricle of the heart and the interventricular septum occurs. This condition itself is a derivative of other diseases and is characterized by an increase in the thickness of the walls of the ventricles.
Despite its prevalence (IVS hypertrophy is observed in more than 70% of people), it is most often asymptomatic and is detected only during very intense physical activity. After all, hypertrophy of the interventricular septum itself is its thickening and the resulting reduction in the useful volume of the chambers of the heart. As the thickness of the cardiac walls of the ventricles increases, the volume of the heart chambers also decreases.
In practice, this all leads to a reduction in the volume of blood that is released by the heart into the vascular bed of the body. To provide the organs with a normal amount of blood under such conditions, the heart must contract stronger and more often. And this, in turn, leads to its early wear and tear and the occurrence of diseases of the cardiovascular system.
Treatment
Treatment of this defect involves conservative treatment of heart failure and surgical correction of the heart defect. Conservative treatment consists of inotropic support drugs (sympathomimetics, cardiac glycosides), diuretics, cardiotrophs.[6] In cases of high pulmonary hypertension, angiotensin-converting enzyme inhibitors - capoten or captopril - are prescribed.
Surgical interventions are divided into palliative operations (in the case of VSD - the operation of narrowing of the pulmonary artery according to Muller) and radical correction of the defect - plastic surgery of the ventricular septal defect with a patch of pericardial leaves under conditions of artificial circulation, cardioplegia and hypothermia.[3]
Possible complications of IVS hypertrophy
What complications are possible with the development of cardiopathy of the type under discussion? Everything will depend on the specific case and individual development of the person. After all, many will never know throughout their lives that they have this condition, and some may experience significant physical ailments. We list the most common consequences of thickening of the interventricular septum. So:
1. Heart rhythm disturbances such as tachycardia. Such common types as atrial fibrillation, ventricular fibrillation and ventricular tachycardia are directly associated with IVS hypertrophy. 2. Disorders of blood circulation in the myocardium. Symptoms that occur when the outflow of blood from the heart muscle is disrupted include chest pain, fainting and dizziness. 3. Dilated cardiomyopathy and the associated decrease in cardiac output. The walls of the heart chambers, under conditions of pathologically high load, become thinner over time, which is the cause of the appearance of this condition. 4. Heart failure. The complication is very life-threatening and in many cases ends in death. 5. Sudden cardiac arrest and death.
Of course, the last two conditions are terrifying. But, nevertheless, with a timely visit to the doctor, if any symptom of cardiac dysfunction occurs, a timely visit to the doctor will help you live a long and happy life.
Notes
- ↑ 1 2 Sharykin.
Congenital heart defects. - Teremok, 2005. - 384 p. - https://www.mma.ru/article/id34653 Ventricular septal defect. Medical encyclopedia of MMA
- ↑ 1 2 3 4 5 Prakhov A.V.
Neonatal cardiology. - NGMA, 2008. - 388 p. - ↑ 1 2 3 Buncle G.
Congenital defects of the heart and large vessels. - 1980. - 312 p. - Vishnevsky A.A., Galankin N.K.
Congenital defects of the heart and large vessels. - 1962. - 210 p. - ↑ 1 2 3 Belozerov Yu.M.
Pediatric cardiology. - MEDpress-inform, 2004. - 600 p. - ↑ 1 2 3 Belokon N.A., Podzolkov V.P.
Congenital heart defects. - 1991. - 352 p. - ↑ 1 2 3 Vasilenko V.Kh., Feldman S.B., Mogilevsky E.B.
Heart defects. - 1983. - 366 p.