Signs of heart problems in a child
Many diseases of the cardiovascular system can occur in a latent form for a long time and make themselves felt only at school age. But there are a number of signs that parents need to pay special attention to, and if at least one of them is present, consult a doctor immediately.
Fast fatiguability
If the baby gets tired quickly during breastfeeding or does not have the strength to take it, you need to make an appointment with a doctor.
If a child has heart problems, he will get tired much faster than his peers. This can be seen during active games in the yard, as well as in physical education lessons. If you notice this once, then there is no reason to worry, perhaps your baby is simply exhausted. But if fatigue occurs regularly, this is a serious reason to consult a cardiologist.
Fainting
If your child faints after suddenly getting out of bed or just running, you should immediately seek medical help. Even a single case of fainting should alert parents.
Swelling of the body and blue lips
You should worry if, towards evening, your child’s legs, arms, and fingers swell a little. If you notice such a feature in your baby, take him to the doctor.
Headache, paleness and sweating
Paleness, sweating of the palms and feet, as well as frequent headaches and dizziness with nausea may indicate problems with the child’s heart.
Shortness of breath and rapid pulse
If after slight physical exertion a child develops shortness of breath, his pulse is often rapid, and sometimes the baby complains of pain in the chest bone, it is worth showing him to an experienced doctor.
But you should not forget that not all heart defects are accompanied by shortness of breath or blue discoloration of the arms, legs and nasolabial triangle.
The parents’ task is to monitor the baby and do not hesitate to ask questions to the pediatrician, and the doctor’s task is to be attentive to the parents’ complaints, comparing them with the results of the examination, and promptly refer them to a cardiologist.
In addition, many heart diseases are congenital. They can be provoked by health problems in the mother, her bad habits, stress and poor ecology. In early childhood, a child may develop heart problems due to stress, heavy physical activity (attending a sports section), or as a result of complications from another illness.
The editors' opinion may not coincide with the opinion of the author of the article.
Source: www.moirebenok.ua
The heart of a child. Heart disease in children
The number of children with congenital pathologies increases every year. Among childhood diseases, one of the first places is occupied by diseases associated with the cardiovascular system. Heart diseases in children include congenital defects, arterial hypertension and hypotension, rheumatism, inflammatory diseases and acquired defects.
All these diseases are dangerous and can lead not only to disability, but also to the premature death of a child.
A child's heart, compared to an adult's, has a number of physiological characteristics that change with age.
The hearts of newborns are larger than those of adults when compared with their total body weight. Both ventricles are approximately equal, and the thickness of their walls is about 5 mm. The weight of the heart increases as the child grows: by 8 months the heart doubles in size, by the third year of life the weight of the heart triples, and by the age of six the weight increases 11 times. In newborns, the heart is located higher and lowers with age. In children, the pulse is normally faster than in adults. This phenomenon is caused by higher contractility of the heart muscle, which is increased due to intense metabolism and less influence of the vagus nerve on the work of the heart. For newborns, the normal heart rate is 120-140 beats per minute. With age, the heart rate gradually decreases. The normal children's pulse is unusual compared to an adult (respiratory arrhythmia is observed): when inhaling, the pulse frequency increases, and when exhaling it becomes less frequent. In addition, in the heart of a newborn child there are anatomical prerequisites for unnatural blood flow - the oval window, through which the right and left atria can communicate, and the ductus arteriosus, which connects the pulmonary trunk with the descending aorta. These formations function during the prenatal period and can remain active in a healthy child for quite a long time. The ductus arteriosus can remain open during the first two months of life, and the oval window - from 8 days to 4 years or more.
An increase in cardiac output in children is associated with increased demands on the organs and tissues of the growing body. Children's blood pressure is lower than that of adults and increases gradually as the child ages. For newborn babies, normal systolic pressure is approximately 70 mmHg. Art., by the 1st year of life it averages about 90 mm Hg. Art. Subsequently, pressure growth occurs intensively in the first two to three years of life and during puberty. Subsequently, the pressure increases in parallel with the increase in the speed of propagation of the pulse wave through the muscle vessels and depends on their tone.
Summarizing all that has been said, we can see that in childhood there are a number of factors that facilitate blood circulation through the vessels and chambers of the heart. Namely, the large mass of the heart relative to the body mass and rather wide openings between its sections and the great vessels. In young children, the low systolic blood volume is compensated by the high frequency of cardiac messages, as a result, the minute volume of blood relative to body weight is greater than in adults. Children also have structures that are uncharacteristic for an adult, through which communication between the systemic and pulmonary circulation is possible. All these factors, in addition to their adaptive function, also pose some danger. Namely, they significantly limit the reserve capacity of the heart at an early age due to the rigidity (weak elasticity) of the heart muscle, high heart rate and, consequently, shorter diastole.
The main heart diseases that occur in children:
Congenital heart disease (CHD) is an anatomical defect in the structure of the heart or great vessels that is present from birth. Congenital defects arise as a result of disturbances in the embryonic development of the cardiovascular system, or are formed as a result of the negative impact of adverse factors on the newborn’s body, for example, respiratory disorders. The latter is especially important for premature babies. All defects can be divided into three large groups.
- Congenital heart defect of the pale type - with arteriovenous shunt: atrial septal defect, ventricular septal defect, patent ductus arteriosus.
- Blue type congenital heart disease - with venoarterial shunt: tetralogy of Fallot, transposition of the great vessels, etc.
- Congenital heart disease without a shunt, but with an obstruction to blood flow: stenosis of the aorta and pulmonary artery.
Unfortunately, the number of cases of children born with heart defects has increased in recent years.
There are several groups of causes leading to congenital heart defects.
- Chromosomal abnormalities - 5%. In this case, congenital heart disease is part of the multisystem malformation syndrome. For example, with Down syndrome, defects of the interatrial and interventricular septa are very often observed. Down syndrome is a variant of chromosomal pathology that often occurs in completely healthy parents.
- Mutations of individual genes - 2-3%. As in the first case, congenital prophets of the heart with gene mutations are combined with developmental anomalies of other organs. Gene mutations are inherited.
- Environmental factors - 1-2%. The most important factors in this group include somatic diseases of the pregnant woman (for example, diabetes), the effect of X-ray radiation on the mother’s body in the first trimester of pregnancy, certain medications, viruses, alcohol, etc.
- Polygenic-multifactorial inheritance - 90%. In most cases, a predisposition to the defect is inherited, which is provoked by environmental factors acting on the embryo (fetus) or newborn.
Congenital heart defects are detected with fairly high accuracy during routine ultrasound scans during pregnancy. This procedure allows you to detect up to 90% of congenital heart defects.
The variety of anatomical and functional disorders determines the uniqueness of the clinical picture for each of the defects. However, there are several common symptoms that are characteristic of all congenital heart defects:
- change in skin color - pallor or cyanosis - depending on the type of defect;
- shortness of breath that appears or worsens with physical exertion;
- rapid fatigue, retardation in physical and mental development;
- Children with congenital heart disease often fall into the category of acute respiratory infections - often suffering from respiratory infections for a long time.
The main treatment method for congenital heart defects today remains surgery. Moreover, it is very important that surgical correction is performed as early as possible.
Prevention
Preventive measures for congenital heart pathologies in a child can be purely informative. Expectant parents should study their family medical history; pregnant women should undergo screening tests and an ultrasound scan.
To prevent acquired heart diseases in children, it is necessary to prevent viral and infectious diseases, especially purulent tonsillitis. If infected, it is important to treat the disease rather than eliminate the symptoms. Within a year after suffering from a sore throat, it is recommended to be observed by a doctor and regularly listen to systolic murmurs.
Hardening, daily walks in the fresh air, following a daily routine, proper nutrition, protection from stress are good measures to strengthen the cardiovascular system.
Articles on the topic
Show all
Users write on this topic:
Show all
Arm yourself with knowledge and read a useful informative article about heart disease in children. After all, being parents means studying everything that will help maintain a degree of health in the family on the island.
Find out what can cause the disease and how to recognize it in a timely manner. Find information about the signs that can help you identify illness. And what tests will help identify the disease and make a correct diagnosis.
In the article you will read everything about methods of treating a disease such as heart disease in children. Find out what effective first aid should be. How to treat: choose medications or traditional methods?
You will also learn how untimely treatment of heart disease in children can be dangerous, and why it is so important to avoid the consequences. All about how to prevent heart disease in children and prevent complications.
And caring parents will find on the service pages complete information about the symptoms of heart disease in children. How do the signs of the disease in children aged 1, 2 and 3 differ from the manifestations of the disease in children aged 4, 5, 6 and 7? What is the best way to treat heart disease in children?
Take care of the health of your loved ones and stay in good shape!
Adults, especially those who already suffer from heart disease, listen carefully to pain and discomfort in the chest, monitor alarming symptoms and, at the first sign of trouble, turn to a cardiologist. We all know: the heart is not to be trifled with!
Another thing is children. The child does not know the signs that indicate illness, and the youngest cannot even complain about feeling unwell. Children's heart diseases are sometimes diagnosed during a routine examination or even by accident, and sometimes when they are already in an advanced state. Some childhood cardiovascular diseases are so dangerous that if medical care is not provided to a small patient in time, you can lose the child or doom him to disability.
How to prevent trouble? In addition to regular visits to the family doctor, you need to carefully monitor the child and not brush off his complaints.
Symptoms and signs of heart disease in children:
- Tachycardia, or rapid heartbeat, is a completely normal phenomenon for children after active games, emotional events (fear or joy), in the heat or during infectious diseases. You need to sound the alarm if tachycardia becomes persistent, but there is no obvious dependence on the listed factors. A slow pulse that does not correspond to age is also suspicious: tell your doctor about this symptom.
- Pain in the chest and heart area does not necessarily indicate problems with the cardiovascular system. This could be neuralgia, diseases of the musculoskeletal system, or ordinary bronchitis. But the child’s systematic complaints of chest pain cannot be ignored.
- Shortness of breath, pale and bluish skin, swelling of the legs may clearly indicate a heart defect. Indirect signs of these disorders may include slow weight gain, lethargy, or the unreasonable cry of a small child.
- Slow physical development is one of the signs. If a child does not tolerate stress well in a physical education lesson or during games, faints or complains of dizziness, the cause may be an arrhythmia or another heart disease. Heart disease in adolescents makes up more than a third of all adolescence disorders, among which the leading ones are mitral valve prolapse and dystonia of various origins.
- A child’s poor performance at school always worries parents, but it’s not only laziness or poor memory that lead to low grades: if this symptom is combined with other complaints about well-being, just in case, it is necessary to check the state of the child’s cardiovascular system.
- If, during a routine examination, pathological ECG changes or increased activity of cardiac-specific enzymes (enzymes indicating myocardial damage) are detected, you should immediately contact a cardiologist.
Diseases of the cardiovascular system in children
Only a doctor can diagnose heart disease in a child by conducting an examination. Sometimes a simple cardiogram is enough for a confident diagnosis; in complex cases, they resort to X-ray examination, ultrasound or even tomography. The names of diseases of the cardiovascular system in children number in tens and hundreds. The most common ones are listed below.
- Congenital heart defects form in the fetus during intrauterine development. These are mainly anatomical deviations: septal defects, stenosis of the pulmonary artery and aorta. In medical practice, there are combinations of several defects. Most defects are treated through surgery - surgery on the heart and blood vessels.
- Acquired defects are a consequence of severe illnesses (myocarditis, endocarditis). Mitral valve insufficiency, mitral stenosis, and aortic valve insufficiency are common.
- Arrhythmias, or cardiac dysfunction of various origins, occur quite often in children. These are tachycardia, bradycardia, extrasystole, atrial fibrillation and others. Arrhythmias in children usually have a favorable course, are successfully treated with medication, and only in rare cases is more serious treatment prescribed.
- Rheumatism affects the cardiovascular system after infection in predisposed children with altered immune system reactivity. This is a serious disease, which in its acute form can cause heart inflammation or defects.
- Myocarditis, cardiomyopathies and other diseases of the heart muscle of a non-rheumatic nature. The cause in most cases is a severe infection (diphtheria, influenza, scarlet fever). In some cases, they can lead to an unfavorable outcome and require active treatment.
- Heart failure. It can occur with myocarditis, physical overload in children with heart disease, as well as with “advanced”, untreated cardiovascular diseases. Characteristic signs are cyanosis of the skin and shortness of breath, turning into an attack of suffocation.
Every parent wants the best for their child. You probably feel like that too. If so, follow these recommendations.
- Carry out regularly scheduled examinations of your child in accordance with the recommendations of the pediatrician.
- Remain calm and do not panic at the slightest discomfort in your child, use common sense. At the same time, listen to children's complaints and, if you suspect a disease, contact your pediatrician. The doctor will conduct a diagnosis, and in case of reasonable suspicion, give a referral to a cardiologist.
- Remember that wasted time in making a diagnosis can turn into a big disaster.
A healthy heart is the key to longevity and a decent quality of life. We are responsible for the health of our children, so we must make every effort to preserve their health. Remember this!
Heart disease in newborns, unfortunately, is not uncommon. Every year, doctors record an increase in congenital pathologies of the cardiovascular system in infants. You can blame the environment, the wrong lifestyle of parents, doctors, but the fact remains that such children require special attention! How to recognize cardiac dysfunction in a newborn in time and what to do?
When you first hear the diagnosis of a “heart murmur,” you should not panic - this is observed in 70% of infants and is considered normal.
There are harmless and disturbing noises.
Harmless (or, as doctors say, functional) noises
associated with the adaptation of the heart to life in new conditions. The fact is that in the prenatal period the child’s heart did not work at full capacity - he was helped by the mother’s respiratory and circulatory systems. But in the first minutes after birth, the baby’s lungs expand and start working, requiring both the heart and blood vessels to switch to a new mode and give full effort. But it happens that the heart experiences temporary transition difficulties, for example, when the oval window or the ductus duct is open.
It is important to know: the heart murmur is completely harmless if it is short, can be heard well at the left edge of the sternum, changes or disappears in an upright position, and otherwise the baby feels great. However, for a final answer about the origin of the baby’s heart murmur, the doctor often needs to conduct additional examinations. If the pediatrician has doubts about the origin of the noise, the little patient will be sent for a consultation with a cardiologist.
thinkstockphotos/fotobank.ua
Congenital heart defects of the pale type
This group includes defects of the interatrial and interventricular septa and patent ductus arteriosus. With each of these defects, there is an anastomosis between the left and right parts of the heart or great vessels. Since the pressure in the left parts of the heart and aorta is much greater than in the right, blood is discharged from left to right. That is, part of the arterial blood mixes with venous blood and again goes into the pulmonary circulation. This leads to overload of the pulmonary circulation. Therefore, the main clinical manifestation of these defects will be shortness of breath during exercise. Pallor appears only with a significant amount of shunting. With age, symptoms of heart failure appear in both circles.
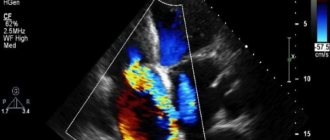
Diagnosis is based on data from echocardiography, or, more simply, ultrasound of the heart. For open ductus arteriosus, only surgical treatment is indicated.
If there is a defect in the interventricular septum in its lower (muscular) part, spontaneous closure of the defect or a significant reduction in its size is possible. If the hole is located in the upper, membranous part, correction is only possible through surgery. Treatment of atrial septal defect is also surgical. In some cases, when the atrial septal defect is a patent foramen ovale, the defect may never manifest as heart failure. Therefore, an unclosed oval window is classified as a group of minor developmental anomalies.
Blue type congenital heart defects
This group got its name because of the cyanotic skin color of children suffering from such defects. The bluish color of the skin is caused by the entry of venous blood from the right sections into the systemic circulation.
Tetralogy of Fallot is a complex congenital heart defect. In the classic version, four signs are detected: a ventricular septal defect, stenosis of the right ventricular outflow tract, dextraposition (incorrect location) of the aorta and hypertrophy of the right ventricular myocardium. Since dextraposition of the aorta is secondary, associated with a high location of the ventricular septal defect, it is often said that the aorta originates from the left and right ventricles.
Symptoms of tetralogy of Fallot. The main symptom is cyanosis, which reaches its maximum by the year of life. One of the constant signs is shortness of breath, which in tetralogy of Fallot is characterized by arrhythmic deep breathing with a normal frequency. Quite quickly, “drum sticks” and “watch glasses” form - thickening of the nail phalanges of the fingers along with an increase in the size of the nail plate. The most severe manifestation of tetralogy of Fallot is dyspnea-cyanotic attacks. The mechanism of their occurrence is associated with spasm of the outflow tract of the right ventricle, as a result of which almost all oxygen-depleted blood from the right ventricle enters the aorta. The consequence of this is severe hypoxia of the brain, manifested by anxiety, fear, loss of consciousness and convulsions. The lack of blood flow to the lungs is manifested by a sharp attack of shortness of breath. Possible death.
Treatment. All children with tetralogy of Fallot are recommended for surgical treatment, which is carried out in two stages. In the preoperative period, bacterial complications are prevented with antibiotics.
Complete transposition of the great vessels
With this congenital heart defect, blood from the right ventricle flows into the aorta, and from the left into the pulmonary artery. Severe shortness of breath and cyanosis appear immediately after birth. Without surgical treatment, the life expectancy of patients usually does not exceed two years.
Birth defects that obstruct blood flow
The narrowing of the aortic opening creates an obstacle to the flow of blood from the left ventricle to the aorta. The narrowing may be at the level of the aortic valve, above or below it. In this case, the pulmonary circulation suffers from congestion, and the large circulation suffers from a lack of blood. Symptoms of the disease are pale skin, tachycardia, shortness of breath, palpitations, pain in the heart area, headache and dizziness, fainting. These symptoms sharply intensify with physical activity, so children should not play sports or perform heavy physical activity, as they can lead not only to exacerbation of symptoms, but also to the death of the child. Treatment. Aortic stenosis is treated surgically. Treatment is prescribed when symptoms are severe.
Coarctation of the aorta is a segmental narrowing of the aortic lumen. The length of the area of stenosis may vary, but, as a rule, it begins above the origin of the left subclavian artery. Thus, in the upper half of the body there is increased blood pressure, lower - low blood pressure and signs of tissue ischemia. With severe arterial hypertension in the upper half of the body, headache, nausea, vomiting, changes in vision, and frequent nosebleeds are observed. Insufficient blood supply to the lower half causes numbness in the lower extremities, a crawling sensation, weakness when walking, pain in the legs, and constantly cold feet. When measuring blood pressure in the legs, a decrease is detected. These symptoms sharply intensify with physical activity.
Diagnostics. Diagnosis of coarctation of the aorta is usually not difficult and is based on data from the clinical picture and instrumental methods - ECG, echocardiography (EchoCG). However, sometimes this congenital heart defect remains unrecognized, because in the first months to a year of life, children can grow and develop normally.
Treatment. Treatment of coarctation is only surgical. Without such treatment, children usually do not survive beyond 2-3 years of age.
Isolated pulmonary stenosis
Pulmonary artery stenosis is characterized by an obstruction to the flow of blood from the right ventricle into the pulmonary circulation. With minor stenosis, the child's growth and development are not impaired, and clinical symptoms may appear in adulthood. With severe stenosis, the child early experiences shortness of breath, pain in the heart, palpitations, and later swelling in the legs and accumulation of fluid in the cavities. This course of the defect requires surgical treatment.
How do heart and vascular diseases manifest?
In order to suspect heart problems in a child, you need to know how cardiovascular diseases manifest in children.
Of course, it is much easier when the child is already old enough, can speak and can complain about what is bothering him. With kids this matter is much more difficult. But still, the semiotics of lesions of the cardiovascular system in children is quite extensive, and there are many symptoms that will help to suspect problems without words.
These include:
- color of the skin;
- dyspnea;
- swelling;
- heart murmurs;
- heart rhythm disturbances;
- chest pain;
- pathological pulsations, etc.
Skin color in heart disease
Changes in skin color in diseases of the heart and blood vessels are the first sign. At first, her pallor is observed, but still the main symptom is cyanosis.
First of all, the nasolabial triangle acquires a blue tint. Therefore, if cyanosis appears on the lips and tip of the nose, it is necessary to show the child to a cardiologist. Later the blue discoloration spreads to the entire face, neck, and upper chest.
Cyanosis can also occur on the arms and legs - acrocyanosis. This symptom also needs to be paid attention to, as it may be a sign of peripheral circulatory failure.
Dyspnea
This is also one of the first symptoms of heart disease. Indicates congestion in the pulmonary circulation. Shortness of breath can only occur during physical exertion and prolonged crying, and maybe at rest (a very unfavorable sign). Therefore, if you notice that your child is breathing too quickly, it would be a good idea to show him to the doctor.
Edema
Pastiness and swelling of the lower extremities always accompany cardiovascular diseases. They indicate circulatory failure, most often due to insufficient work of the right ventricle.
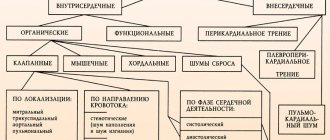
Heart murmurs
Heart murmurs during auscultation are caused by disruption of blood flow due to various deformations and anomalies in the structure of the heart. Murmurs can be diastolic and systolic, functional and organic. Systolic murmurs are often functional in nature, that is, they are not associated with disturbances in the structure of the heart.
Diastolic murmur predominantly occurs with organic pathologies - congenital defects, stenosis, valve insufficiency, etc. In any case, the nature and cause of the heart murmur will be determined by the doctor, and based on these signs he will be able to suggest a diagnosis.
Heart rhythm disturbances
With heart disease in children, an increase or decrease in heart rate may be observed, and arrhythmias may be detected. It must be borne in mind that tachycardia is not always a sign of disease.
It often occurs in emotional children during periods of worry, during adolescence, during stress, and prolonged crying. Bradycardia can occur during sleep or in children actively involved in sports.
Chest pain
Cardiogenic pain is localized behind the sternum and radiates to the left arm, scapula, and lower jaw. They can be of a pressing or cutting nature.
Babies under one year old cannot say that something hurts, but this is indicated by frequent and causeless crying, refusal to eat, and anxiety. You should not ignore such symptoms; it is better to play it safe and consult a doctor.
Pathological pulsations
Due to disturbances in the structure of the heart, an increased load is placed on its various parts and some vessels, which is why visible pathological pulsations appear on the body. The carotid arteries, veins in the neck, vessels in the stomach area, in the intercostal spaces to the right and left of the sternum, in the jugular fossae and other places may swell and pulsate.
Cardiac tremors (“cat purring”) is one of the types of pathological pulsations. Occurs with stenosis of the aorta or pulmonary artery. Due to the intense work of the heart, a “heart hump” can form in the area of its apex - a bulge in the area of the ribs due to an increased apical impulse.
Arterial hypertension and hypotension in children
Arterial hypertension and hypotension are most often signs of neuro-circulatory (vegetative-vascular) dystonia, which, in addition to changes in pressure, is manifested by shortness of breath, weakness, pain in the heart, weakness, fatigue, and neurotic disorders. All these disorders are functional in nature and are not dangerous to the life and health of the child. But it is still better for such children to be registered with a pediatrician, since with age, functional disorders can transform into organic changes.
It is extremely important not to miss acute rheumatic fever in childhood. It is caused by group A β-hemolytic streptococcus. Acute rheumatic fever occurs 1-5 weeks after a sore throat. During acute rheumatic fever, antibodies are formed against the body's own tissues, but the heart suffers the most. Clinical manifestations. The fever itself is manifested by temporary inflammation of large joints, carditis - inflammation of the myocardium and endocardium. Small painless subcutaneous nodules appear on the legs and arms, and a rash in the form of ring erythema is possible on the skin. Damage to the nervous system is noticeable by changes in the emotional sphere and convulsive syndrome in the form of irregular twitching - chorea. All manifestations of acute rheumatic fever are temporary, except for carditis. Even myocarditis can go away without a trace. Rheumatic endocarditis is extremely dangerous, since inflammation of the endocardium spreads to the heart valves, leading to the formation of various acquired defects. The mitral valve is most often affected. Mitral valve insufficiency, stenosis, or a combination of these defects is formed. If acute rheumatic fever is not recognized in time, then acquired heart disease remains undiagnosed for a long time and progresses. At the age of 20-30, signs of heart failure begin to appear. First, blood stagnates in the pulmonary circulation, which is manifested by shortness of breath and night attacks of suffocation. With decompensation of mitral disease, stagnation occurs in a large circle in the form of edema, accumulation of fluid in the cavities and damage to internal organs.
To prevent acquired mitral valve disease it is necessary:
- Prevention of purulent tonsillitis, and if they occur, adequate treatment and only in a hospital setting.
- After suffering a purulent sore throat, observation by a local pediatrician is necessary for at least a year. Timely listening to the systolic murmur at the apex of the heart allows the pediatrician to take timely measures to prevent the occurrence of mitral disease.
Treatment
Absolutely all newborns with a confirmed heart defect are subject to mandatory and regular monitoring by a pediatrician (usually a local doctor) and a cardiologist. Until a year old, the toddler will be examined and examined every three months. After a year - once every six months. In cases of severe or complex defects, the newborn will be monitored monthly.
In addition to monitoring the child’s condition, specialists will provide parents with mandatory instructions - a special baby needs special care:
To treat serious pathologies (both congenital and acquired), surgical techniques are often used. In addition, therapeutic methods of treatment are used before and after the necessary operation.
If the pathology is more than just serious, surgical intervention in the newborn’s body cannot be avoided. Such an intervention, depending on the specific situation, is performed either open heart or using a minimally invasive method. In any case, the newborn is temporarily connected to a heart-lung machine. After the operation, the child is under the strict guidance of a cardiologist until the unpleasant issue with a heart defect is completely resolved.
In some cases, the issue cannot be resolved by surgical intervention alone. Therefore, two operations are performed - the first to improve and stabilize the general condition of the patient, the second - to completely eliminate all existing defects and abnormalities in the functioning of the newborn’s heart.
Did you know? Regardless of the complexity of your specific case, if you contact specialists in a timely manner, the prognosis for the child is favorable in the vast majority of cases.
Inflammatory heart diseases
Myocarditis is inflammation of the heart muscle due to various reasons. An important etiological factor in the development of myocarditis is rheumatism. Myocarditis can also be the result of bacterial and viral infections, sometimes an allergic process and other less significant causes.
Clinical picture. Myocarditis is manifested by weakness, fatigue, shortness of breath, palpitations, shortness of breath, and a feeling of heaviness in the chest. If myocarditis is combined with endocarditis, then signs of developing heart disease are detected, and when combined with pericarditis, severe pain syndrome is detected. Diagnosis of myocarditis is based on ECG, EchoCG, X-ray data, results of physical (external examination of the child) and laboratory examination. Treatment is aimed at eliminating the causes of myocarditis and preventing complications.
Pediatric cardiology has its own characteristics. Unlike adults, children rarely complain of symptoms characteristic of diseases of the cardiovascular system, so it is necessary to conduct a more thorough survey of the child and focus on physical and instrumental examination. It should also be remembered that if the defect is mild, the child can grow and develop normally for a long time, play and run around with healthy children. However, untimely diagnosis of heart disease can lead to severe heart failure in a person and early death. Using a Cardiovisor can come to the rescue. Thanks to the services of the Kardi.ru service, the child’s heart will always be under reliable control, since the cardiovisor can be used even at home.
Congenital and acquired diseases
The main problem is in diagnosing heart disease in children, which consists in the child’s inability to accurately and in detail describe his feelings and problems. In this regard, the majority of heart diseases in children are detected during a routine medical examination at a difficult stage of their development completely by chance.
Sadly, every year the number of children diagnosed with childhood heart disease is increasing. Not the least important among them are congenital diseases, including heart defects.
According to statistics, this group of diseases is only 1% inferior to congenital diseases of the nervous system.
Unlike adults, in children the majority of diseases of the cardiovascular system are congenital. The main reason for their development is the negative impact of environmental factors or the improper lifestyle of the woman carrying the child.
Until recently, such pathologies led to the death of the fetus or newborn child. The development of medicine today gives such children not only a chance of survival, but also a full recovery.
The existence of modern methods of intrauterine diagnostics makes it possible to determine the presence of cardiovascular diseases in unborn children, which increases the chance of recovery.
But there is a group of congenital cardiovascular diseases that can be identified and prevented only after the baby is born. For this, modern diagnostic methods are used. Thanks to their use, specialists are able to timely determine the presence of congenital heart disease in approximately 90% of newborns.
If we talk about the reasons that provoke the development of congenital heart defects in children, the following can be distinguished:
- exposure to external factors (they can affect a woman’s body both before pregnancy and directly during pregnancy). In many cases, their exposure is preventable;
- random mutations, which include infectious diseases (lead to gene mutations).
All congenital defects can be divided into the following groups:
- white (skin becomes noticeably pale);
- blue (cyanosis of the skin is observed).
As for acquired heart diseases in children, their causes are not very different from those that provoke the development of congenital pathologies. These include obesity, infection, high cholesterol, high blood pressure, etc.
I would especially like to dwell on type 2 diabetes. Nowadays it can be found not only in adults, but also in adolescents and preschoolers. The disease sooner or later leads to the development of changes in the structure and functioning of the cardiovascular system of the human body, as well as the metabolic process in the tissues of the child’s heart.
Diseases of the cardiovascular system in children can be either acquired or congenital.
The danger of childhood heart disease
Defects such as tetralogy of Fallot, transposition of the great vessels, etc. pose a direct threat to the life of the child immediately after birth. Sick children either undergo surgery or die soon after. Postoperative mortality in these cases is also high.
But many congenital heart defects are fraught with hidden dangers. When these defects are detected, children are recommended to undergo surgical treatment of the defect, but parents refuse the operation because the child does not look sick. When symptoms of heart failure appear at the age of 20-25, it is already too late to have surgery due to the very high operational risk. Thus, the person lives the last few years as a severely disabled person and dies at a young age.
Why are children born with heart defects?
The cause of congenital heart disease in a newborn may be the use of drugs by the mother.
The pathological development of a congenital disease has not been fully identified by medicine. The following general factors influence the abnormal development of the heart:
- Woman's age category: over 35 years old
- Chronic poisoning by drugs, tobacco products, and alcoholic beverages
- Polluted atmosphere
- Chronic diseases of the expectant mother
- Increased levels of radioactive background
- Treatment during pregnancy with serious medications such as antibiotics, anti-inflammatory drugs
- Chromosomal diseases
- Extremities are constantly cool
- There are noises in the myocardium when listening
- Genetic predisposition
- Infection of a pregnant woman with viral diseases (rubella, influenza, herpes)
- Unfavorable obstetric history in the past (premature birth, miscarriage, abortion)