Intraatrial conduction disturbance
Such a complete blockade rarely affects the heart; this condition is dangerous, since the left and right atria begin to function independently of each other, and two independent atrial rhythms appear.
The condition is caused by the cessation of impulse transmission through the Bachmann beam. The patient's condition is characterized by intraventricular sinus rhythm with the addition of a negative P wave caused by overexcitation of the lp.
Atrial sinus rhythm PP is combined with atrial fibrillation of the left atrium and its tachycardia.
Causes:
- ischemia;
- myocardial infarction;
- atherosclerotic cardiosclerosis;
- heart defects;
- myocarditis.
Also, the cause of a serious condition can be an overdose of medications for the treatment of arrhythmia, digitalis poisoning, and electrolyte imbalance as a result of a lack or excess of potassium.
Types of interatrial signal flow difficulties:
- slowing down the passage of the impulse;
- inconsistent blocking of the signal going to the lp;
- atrial dissociation.
Factors
Based on medical statements, the main reason for the slowing of intraatrial conduction is neurocirculatory dysfunction. What does this mean and what does it mean for a healthy person? It all depends on the stage of conduction slowdown.
There are 3 stages:
- slight slowdown - has no effect on the functioning of the heart and blood vessels. Characterized by partial disturbance of heart rhythm;
- more pronounced slowdown - characterized by a slight increase in pressure on the heart muscle. The main threat is the transition to a high stage;
- slowdown significantly affects the movement of blood through the vessels. There is a risk of a heart attack or cardiac arrest.
A slight and more pronounced slowdown occurs, accompanied by atrial fibrillation, which represents untimely, erratic impulses that signal a contraction of the heart. In this case, the heart muscle, with a certain rhythm, does the work for nothing. The following reasons may contribute to this:
- the permissible level of glycoside is exceeded;
- presence of rheumatic fever;
- inflamed heart muscle;
- high stage of hypertension;
- various types of heart defects.
Statistics show that pensioners and children consult a doctor about slowing intravalvular conduction. At retirement age, neuronal fibers and the heart wear out at a physiological level. In children, the slowdown is congenital.
The slowdown that occurs from time to time can lead to intoxication of the body. This often happens in people who abuse alcohol and smoke a lot of cigarettes every day. If such conductivity is allowed to develop, when the impulse arrives in 2 cardiac compartments with a disturbed gap, then bradycardia and shortness of breath occur. While in this state, the patient may lose his mind for a short time, even if there was no physical activity, and he also suffers from a persistent headache. Further, intraventricular conduction is disrupted when irritating nodes are blocked. Therefore, part of the muscle does not contract, and the pressure increases significantly.
Treatment
Therapy consists of restoring cardiac conduction and hemodynamics of the body. An elderly person with suspected blockade is hospitalized in a hospital, especially with the development of Morgagni-Adams-Stokes syndrome.
Drug therapy for acute conditions:
- Taking anticholinergic drugs: platifilin, atropine, glucose.
- To enhance the sympathetic effect on the impulse conducting system, norepinephrine, ephedrine, alupent, and isadrine are prescribed.
- Hydrocortisone is used to relieve inflammation, swelling, and reduce potassium content in the signal transmission area.
- Lasix helps reduce potassium levels.
If medication is ineffective, doctors install an electrode in the right ventricle. Cardiac pacing is indicated for myocardial infarction with complete blocking of the signal.
Diagnostics
The basis of examination for suspected pathology is an ECG. During the examination, the doctor discovers the main signs of a particular condition. Extrasystoles are manifested by altered ventricular complexes, tachycardia paroxysm - by short intervals between us, etc. Do not try to interpret the ECG results yourself. Entrust the procedure to a cardiologist.
An ECG is not the only examination used to diagnose pathology.
Also performed:
- Daily monitoring of ECG and blood pressure.
- Tests with physical activity.
- Transesophageal ECG.
- Transesophageal electrophysiological study.
- MRI of the heart.
- Ultrasound of the heart, etc.
All diagnostic methods are aimed at detecting deviations from normal heart rhythm and recording partial or complete blockades. The patient may also be referred for an examination to assess the patency of various vessels.
Stopping intraventricular conduction
This conduction system consists of two bundle branches, left and right. The right leg is a wide muscular formation extending into the pancreas tissue.
The left leg consists of two branches, anterior and posterior, extending into the muscles of the posterior wall of the ventricle and representing the Purkinje network.
If it is difficult for the impulse to pass through these conductors, an intraventricular block develops.
Its types:
Single-bundle: left anterior branch of the His bundle; left posterior branch of the His bundle;
- right leg.
- Double bundle (bifascicular): left bundle branch and anterior, left branch.
- Three-fascicular (trifascicular).
Classification according to the course of the impulse transmission disorder:
- sustainable;
- intermittent;
- alternating.
Diseases that cause difficulty in ventricular conduction:
- ischemia;
- heart attack;
- cardiomyopathy;
- blockade of pg;
- toxic damage to the heart muscle;
- AVB.
conclusions
Disturbance in the conduction of electrical impulses from the right atrium to the left is caused by various diffuse pathologies of the myocardium of rheumatic, coronarogenic or unknown origin. Isolated intraatrial blockades do not cause hemodynamic disorders and clinical signs of heart failure, but may cause further high-grade arrhythmias. Treatment of the pathology is carried out depending on the underlying disease and existing symptoms and involves the use of pharmaceuticals or the installation of an artificial pacemaker.
Symptoms
Different types of blockages give different signs, but there are a few main symptoms:
- rapid heartbeat;
- angina pectoris;
- frequent fainting;
- dyspnea;
- dizziness.
Symptoms of nonspecific impulse transmission disorder:
- fever;
- dizziness;
- chronic fatigue;
- emotional lability;
- memory impairment;
- increased anxiety associated with fear of death.
Cautions
If symptoms are ignored and there is no timely treatment, cardiac conduction disturbances can lead to various complications, including death.
sudden cardiac arrest;
functional disorder of the heart;
worsening of the disease with pronounced symptoms;
The condition is considered potentially dangerous to the life and health of the patient, therefore, at the first signs of the disease, it is recommended to immediately consult a specialist.
Focal intraventricular block
This is a disturbance in the passage of the impulse, which has spread beyond the main branches of the NPG, it affects the Purkinje fibers, as well as the contractile myocardium, the posterior, lower parts of the left ventricle or the anterior upper.
On the ECG, the problem is visible as an extended QRS complex with a deformed ending. In most cases, a focal disorder is diagnosed together with a blockade of the posterior or anterior branch of the LPN.
In this case, the ECG shows a strong deviation of the left axis and a wide QRS complex.
Reasons for focal stopping of the passage of an electrical impulse:
- myocardial infarction;
- hyperkalemia;
- diffuse myocardial fibrosis;
- scar on the myocardium.
Therapy consists of preventing complete blockade with a Morgagni-Adams-Stokes attack; for this, patients are recommended to install a pacemaker.
Violation of intracardiac conduction. General principles of functioning of electrical conduction pathways. Therapy
The organ that commands the heart to contract is called the sinus node or pacemaker. The pacemaker works at a certain frequency to ensure that the myocardium contracts synchronously.
The function of conducting cardiac impulses is performed by cells capable of receiving and transmitting signals. Disruption of signal transmission through these cells is called a blockade.
They are divided into intracardiac, which are:
- Sinoatrial (signal transmission problem associated with the sinus node);
- atrioventricular (problem with the signal from the atrium to the ventricle);
- intraventricular (the impulse does not pass through the ventricles).
What leads to the cessation of the electrical signal:
- intracardiac conduction slows down due to high parasympathetic tone;
- scarring or inflammatory tissue disorder;
- drug overdose.
To diagnose the problem, cardiologists refer patients for a 24-hour Holter ECG, ECG, and stress tests.
Therapy consists of the treatment of underlying diseases, treatment of the physical disease that caused the disease; normalization of the tone of the autonomic nervous system, implantation of a pacemaker.
Signs
When diagnosing a minor conduction disorder, no visual symptoms are visible in the patient.
He may feel great and, according to other diagnostic indications, be completely healthy. It is dangerous for the heart rate to slow down to 50 beats per minute. And a person feels a different range of heartbeats. This means that there is a blockage in one area of the heart muscle. Symptoms occur:
- discomfort in the chest (as if there was seething inside);
- not severe pain;
- rapid sweating;
- sleep is disturbed;
- frequent attacks of dizziness.
These signs indicate insufficient oxygen supply to the organs.
With a significant slowdown in conduction, patients' vision quickly declines.
Signs of slow conduction in patients can differ significantly, since it varies depending on the part of the heart muscle that receives the signal from the sinus node with a delay. This defect can also occur in children. Their reaction is more noticeable due to the smaller blood volume compared to adults, and the heart rhythm is frequent.
Intracardiac blockades during pregnancy
During pregnancy, conduction disorders are associated with various heart diseases. Sino-aricular conduction problems are caused by weakness of the joint system, the cause of which cannot always be determined.
Pregnancy does not interfere with the installation of a pacemaker if necessary. There are some restrictions in the treatment of pregnant women; they are not prescribed atropine and drugs containing it.
Obstetrics are carried out naturally if there are no severe concomitant diseases.
AVs of the first and second degrees do not affect the woman’s condition; if every second and third contraction falls out of the rhythm, the underlying disease is treated.
For disorders that cause severe symptoms, under the supervision of a doctor, the pregnant woman takes glucocorticoids, not more than 40 mg.
The occurrence of a complete blockade requires measures to urgently hospitalize the woman for resuscitation measures. A temporary effect (until the installation of a pacemaker) in such cases is provided by the following drugs: alupent, atropine, ephedrine, isadrine.
Causes of the disease
Heart rhythm and conduction disturbances can occur due to physiological characteristics and cardiac pathologies.
Sinus tachycardia, for example, develops during physical and emotional stress. Respiratory bradyarrhythmia is normal. Atrial fibrillation and flutter are dangerous. They usually develop against the background of diseases of the cardiovascular system. As a rule, heart rhythm and conduction disturbances occur when:
- coronary heart disease;
- vices;
- arterial hypertension;
- cardiomyopathy.
Non-cardiac diseases such as:
- acute poisoning;
- fever;
- stomach ulcer;
- hyperthyroidism;
- adrenal tumor.
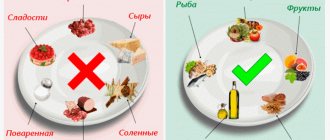
Risk factors for the development of pathology include:
- smoking and alcohol abuse;
- obesity;
- concomitant diseases (mainly the endocrine system).
Symptoms
A slight deviation of the normal pulse (it is by this that the number of blood emissions into the aorta per minute is recorded) does not have any effect on the body. Accordingly, there are no symptoms as such. The deviation is discovered by chance during a cardiogram.
With the development of the third degree of deceleration, Morgagni-Adams-Stokes attacks may occur, and bradycardia is observed. The patient complains of frequent fatigue, cold sweat, shortness of breath with minimal physical activity, frequent loss of consciousness for several seconds, a constant desire to sleep, dizziness, headache (resulting from high blood pressure). Often these patients experience seizures, usually in the lower extremities, where blood stagnation occurs. Often there is a sharp, dull pain in the chest area. Moreover, without previous factors such as physical activity, fatigue, etc. This indicates unspecified chaotic impulses that are supplied to the sinus node.