Causes and symptoms
The causes and mechanisms of capillaritis on the legs, as a rule, are not always clear. Sometimes, the cause may be an immunological factor , an increase in venous pressure (varicose veins or phlebitis of the lower extremities) or an allergy. It is quite easy to notice the disease, since it directly affects the color and condition of the skin .
If the skin has a purple tint , the disease is in its final stages. But usually, the skin is characterized by red that never go away. This occurs due to venous pressure, which causes red blood cells to burst through the capillaries.
If the skin color has a browner or yellowish tint , this indicates an excess of iron in the body, which also leads to the destruction of red blood cells.
Some forms of capillaritis indicate cell necrosis. In this case, you can observe spots with a black crust throughout the entire area of the disease. If you do not start treatment, noticing these signs, the disease can cause some complications, which will immediately appear on the skin - it will turn white. White skin is a sign of atrophy.
Capillaritis can also be caused by dilatation of capillary networks . Thus, inflammation will become noticeable on the skin in the form of small red and purple lines.
Unfortunately, these symptoms are not enough to confidently identify the disease of capillaritis. Sometimes a microscopic biopsy may be needed to take a closer look at the affected area.
There is no truly effective therapy for the treatment of capillaritis. But you can use a series of vitamins to protect the capillaries.
The danger of capillaritis in children
Despite the fact that capillaritis is a disease characteristic mainly of adults, children can also get it.
There are two main forms of capillaritis in children.
The most common form of capillaritis is Henoch-Schönlein . It affects ages from 4 to 10 years .
This disease is characterized by the appearance of precise and obvious symptoms such as purple spots , itching and abdominal pain , very similar to colic . Typically, this form of the disease tends to go away on its own, without the use of any medications.
Another type of capillaritis that affects children, especially those under 5 years of age, is Kawasaki . It is characterized by symptoms such as:
- fever;
- swollen lymph nodes;
- conjunctivitis;
- inflammation of the lips, tongue, hands and feet;
- joint pain and rashes.
This form of capillaritis usually spreads to all areas of the arteries and can lead to cardiovascular complications. Like other types of capillaritis, this form can go away on its own, but to avoid complications in most cases, the use of immunoglobulin is recommended.
Causes
Among the causes of keratoma, one can note disturbances in the course of certain processes in the body. These are especially common:
- Pathologies in the gastrointestinal tract.
- Pathologies in the functioning of the endocrine system.
- Hormonal problems.
Often the primary cause may be the patient’s poor diet, for example, lack of a specific schedule, overeating or fasting, as well as eating substances harmful to the body in large quantities.
Other causes include:
- Pathologies in the functioning of the immune system that could arise as a result of recent recovery from an infectious or other disease.
- Strong experiences that can be isolated or occur on an ongoing basis, periodically. Strong fear, fright.
- Obtaining any virus that infects epithelial tissue.
Most often these are not the primary reasons. They simply contribute to the appearance and development of keratopapillomas on the skin.
A particularly common type of illness is senile disease. It affects the epithelial tissue of older people who are over sixty years old. After a certain period of time, the formation itself disappears.
As a rule, it manifests itself in group rashes. In a normal case, correcting the situation does not require the intervention of doctors, because the disease arises due to the characteristics of the body of people of this age environment.
Treatment in adults
The treatment course for capillaritis includes drugs that are divided into two types. These are corticosteroids , which keep inflammation under control, and immunosuppressants , which regulate the action of cells of the immune system, especially in the case of autoimmune capillaritis.
As for steroids, the dose and duration of therapy directly depend on the severity of the problem . Please be aware that these medications may also cause side effects . Sometimes it is necessary to resort to surgery , especially when capillaritis affects certain organs, such as the heart or lungs. The purpose of the operation is to improve the functionality of the organs.
It is important to keep in mind that medications used to control the disease may have side effects. It is also necessary to include proteins, peas, citrus fruits, liver and vegetables in your diet.
How to Cure Dermatitis – Medicines and Natural Remedies
Since atopic dermatitis is not one disease, but a large group of very different diseases, it is impossible to define a single therapeutic protocol. Treatment will vary depending on the cause that is leading to the inflammation . However, despite the possible variety, the most commonly used for the treatment of dermatitis are:
- corticosteroids, which fight inflammation locally or, in more severe cases, systemically;
- immunosuppressants, which weaken the immune system;
- antihistamines, which help keep itching symptoms under control.
Light therapy is also often used. That is, exposure of the skin to natural or artificial light.
Natural Treatments for Dermatitis
Some natural remedies may be helpful while waiting to consult your doctor:
- Fresh wraps and baths that relieve itching.
- Clothing made from natural fibers, soft, which do not cause additional irritation to the skin.
- Protecting affected areas from scratching. Since friction of damaged skin exacerbates inflammation and itching.
- Wash clothes with delicate detergents and rinse thoroughly.
- Probiotics. Living organisms (lactobacillus) that are able to overcome the gastric barrier and colonize the intestines. Some studies have shown their effectiveness in eliminating atopic dermatitis.
- Rice bran wraps. Relieves symptoms of itching, particularly in the case of atopic dermatitis. Also available as a powder for dissolving in water and bathing newborns.
- Creams based on bovine cartilage. Relieves symptoms of contact dermatitis.
- Chamomile compresses. Relieves symptoms of itching and reduces inflammation.
- Coconut oil. It has soothing and softening properties and makes the skin elastic, preventing bacterial infections of injuries.
Treatment in children
When we talk about capillaritis, we mean a special pathology, the name of which is Henoch-Schönlein . It affects the lower limbs of children. This disease is expressed by inflammation of the capillaries. This pathology tends to manifest itself in children between 5 and 15 years of age . It is accompanied by various symptoms, including redness of the skin. In addition to the external rash, the disease is accompanied by joint pain or arthritis . But these symptoms disappear after a few days.
Other manifestations of the disease may include swelling (especially in very young patients) and skin lesions noticeable to the touch. They usually form in the lower extremities or in the buttock area . But, in rare cases, a rash can appear on the hands, accompanied by convulsions, bleeding of the brain and lungs. Henoch-Schönlein disease is not inherited and is not at all contagious .
Unfortunately, it is not yet entirely clear what exactly causes this type of pathology, but it is assumed that it may be caused by the use of certain medications . For example, infectious agents from insect bites, chemicals or certain foods.
As noted above, the disease regresses without any specific therapy, but if necessary, the healing process can be accelerated with the help of painkillers and anti-inflammatory drugs.
Classification of the disease
Clinical forms of hemorrhagic vasculitis:
- lightning;
- cutaneous;
- articular (rheumatoid);
- renal;
- abdominal;
- mixed.
Character of the current:
- acute – up to two months;
- protracted – up to six months;
- chronic – a long period, relapses, recession and exacerbation phases are noted.
Degrees of Henoch-Schönlein disease:
- light. The general condition of the patient does not cause concern, rashes are rare and not abundant, mild joint pain is observed;
- medium-heavy. The condition worsens, the skin becomes covered with profuse rashes, abdominal pain periodically occurs, joints ache and twist, as with arthritis;
- severe course of the disease. General weakness, malaise, angioedema, a rash covers large areas of the skin, and ulcers appear. Gastrointestinal bleeding, kidney damage occurs, and renal failure may develop.
Causes
Inflammation of the blood vessels of the legs can be primary and secondary. In the first case, it is an independent disease. The reasons are not known for certain. Heredity plays an important role.
Causes of secondary vasculitis:
- connective tissue diseases, for example, rheumatoid arthritis, systemic lupus erythematosus;
- infectious diseases, in particular those caused by hepatitis virus or staphylococcus;
- tumor formations;
- weakening of the body's defenses;
- hypothermia of the extremities;
- injuries;
- sunburn or thermal skin lesions;
- severe chronic diseases;
- allergies to certain medications (vasculitis is most often caused by taking analgesics, antibiotics and drugs containing iodine);
- regular stressful situations.
The cause of inflammation of the walls of the vessels of the extremities can be vaccination or diagnosis using a contrast agent.
Causes of vasculitis
The inflammatory process can be caused by the presence of a chronic infection in the body, severe intoxication, including toxic poisons, taking certain medications, overheating or, conversely, hypothermia, injury, burns. Sometimes the disease is autoimmune in nature (when, for an unknown reason, the immune system begins to attack the cells of its own body).
Skin vasculitis usually occurs during prolonged interaction with toxic substances. The poison penetrating into the layers of the epidermis has a negative effect on small blood vessels, provoking inflammation of their walls and the appearance of signs characteristic of this process.
Vasculitis in a child caused by vaccination. The body of young children often reacts in a similar way to serum injected into it. Cancer patients undergoing intravenous chemotherapy also face a similar problem. In this case, the drugs literally burn the walls of blood vessels; the disease goes away when the amount of medication administered per day is reduced or some time after its discontinuation.
In some cases, vasculitis is considered as a completely separate disease, not associated with the presence of other pathologies in the body. The causes of primary vasculitis have not yet been established.
YOU WOULD BE INTERESTED
HIV infection
Types and symptoms
Inflammation of blood vessels in the legs can be of the following types:
- Hemorrhagic angiitis. This variety is characterized by damage to the capillaries and blood vessels located in the internal organs, inflammation of the skin of the legs and joints. The most common cause of this type of disease is damage to the capillaries in the legs.
- Allergic. Occurs against the background of an allergic reaction.
- Cryoglobulinemic. This species is characterized by damage to small vessels in the legs.
- Systemic. Both large and small vessels are affected. More often the cause is an allergy or infection.
- Cutaneous leukocytoclastic. Capillaries and arterioles are affected.
- Erythema nodosum. The vessels of the subcutaneous tissue are affected.
- Wegener's granulomatosis. The vessels of the respiratory system become inflamed most often, and in 30% of cases the skin. The inflammatory process is accompanied by the formation of granules and areas of necrosis.
Deep vasculitis of the vessels of the lower extremities (erythema nodosum) is more difficult to treat than superficial vasculitis.
Symptoms of angiitis differ depending on the type, nature of the lesion and location of the inflammatory process. For example, hemorrhagic vasculitis manifests itself as spots on the legs.
Initial symptoms may resemble any other disease. The patient feels weak, body temperature rises, and joint pain bothers him.
With inflammation of the blood vessels of the lower extremities, one of the main symptoms is skin rashes. The rash is very similar to lupus, then subcutaneous hemorrhages and hemorrhagic spots appear, and ulcers form. The patient is bothered by itching and burning.
In the presence of severe chronic diseases, such as diabetes, the symptoms are more pronounced.
Unlike the hemorrhagic form of angiitis, with nodular angiitis there is no pigmentation. First, bright red nodules appear, most often they are localized at the bottom of the lower leg. The patient feels pain. Over time, the nodules disappear and the skin recovers.
Causes and risk factors of dermatitis
Since dermatitis includes a fairly large group of diseases, the causes will obviously vary greatly depending on the specific type.
In cases where the exact causes cannot be identified, it is assumed that dermatitis is caused by a combination of factors:
- Genetic reasons. Several studies have linked the occurrence of dermatitis to mutations in a corresponding set of genes. Among them, the most important ones appear to be mutations in genes that encode the protein filaggrin, which binds keratin to the structure of epithelial cells. Epidemiological studies have found that patients suffering from celiac disease are three times more likely to develop dermatitis.
- Environmental reasons. As in the case of asthma and other allergic conditions such as rhinitis, it has been hypothesized that the basis of dermatitis is excessive hygiene, which deprives the immune system of the necessary exposure to external factors through which it is “trained” to classify and recognize foreign bodies. The absence of these conditions obviously increases the likelihood that the immune system will make a mistake.
Risk factors for dermatitis
Certain conditions increase the likelihood of developing certain types of dermatitis.
Here are the most common ones:
- Age. Dermatitis can generally appear at any age, but for some the risk is higher. A typical example is atopic dermatitis, which affects children under 5 years of age in 90% of cases.
- Working in an aggressive environment. Working in contact with metals, chemicals and certain cleaning products increases the risk of contact dermatitis.
- Having allergies. People who suffer from asthma, rhinitis, or have close relatives with allergies are at greater risk of developing certain types of dermatitis.
Treatment
Treatment for vasculitis of the lower extremities is long-term. It includes:
- taking medications;
- diet;
- massage and exercise therapy;
- use of traditional medicine.
The effectiveness of treatment depends on how well the patient complies with the doctor’s recommendations. It is impossible to get rid of this vascular pathology unless the effect of the provoking factor is eliminated, therefore the quality of diagnosis affects the result of therapy.
Medicines
Inflammatory processes in the vessels of the lower extremities are treated comprehensively:
- NSAIDs – Indomethacin, Diclofenac;
- antihistamines – Claritin, Erius, Suprastin;
- glucocorticosteroids – Prednisolone;
- drugs to strengthen blood vessels - Venorutin, Ascorutin;
- means that improve blood flow - Prodectin;
- vitamins – ascorbic acid, calcium preparations.
For infectious processes, antibacterial agents are prescribed. To quickly heal the skin and eliminate the symptoms of local inflammation, ointments and gels are suitable, for example, Troxevasin, Iruksol, Solcoseryl.
Exercise therapy
When the vessels in the legs become inflamed, blood circulation is impaired. To improve blood flow and reduce the manifestations of vasculitis, you need to do therapeutic exercises.
The following exercises are effective:
- "bike";
- "scissors";
- "birch";
- "rising on your toes."
Exercise therapy promotes better blood circulation, so itching and burning disappear.
A therapeutic massage will help relieve leg pain.
Folk remedies
Traditional therapy involves the use of the following means:
- infusion of elderberry flowers, Japanese sophora fruits, nettle leaves and yarrow;
- a decoction of calendula flowers, elderberry, mint, horsetail, yarrow and poplar buds.
If the vessels of the skin of the legs become inflamed, you can make compresses from pine resin. To do this you will need 100 g of pine resin, 25 g of beeswax and 20 g of vegetable oil. Heat all ingredients in a water bath and mix until smooth. The prepared mixture should be applied to the affected areas.
Diet
Diet plays an important role in the treatment of the disease. You need to exclude all kinds of allergens from your diet. These are citrus fruits, chocolate, red berries, products with dyes and preservatives. You should avoid salty, spicy and fried foods.
It is beneficial to eat foods rich in vitamin C. It is recommended to eat fresh fruits and vegetables, as well as take vitamin supplements.
Prevention
Preventive actions:
- quit smoking and alcohol;
- avoid hypothermia and overheating;
- observe the work and rest schedule;
- avoid stress;
- Avoid excessive exercise, but moderate exercise is beneficial;
- increase immunity.
Treatment for vasculitis is long and difficult, so it is better to take preventive measures. This disease must be diagnosed and treated on time. Vasculitis of the blood vessels of the legs without treatment leads to severe complications, including heavy internal bleeding.
Author: Oksana Belokur, doctor, especially for xVarikoz.ru
Source: xvarikoz.ru
The manifestation of telangiectasia - the result on the face and not only
Telangiectasias have an average diameter of 0.1 to 0.3 mm and can be red, blue or purple depending on whether the blood flowing through them is venous or arterial. Thin red spider veins that do not rise above the surface of the skin usually develop from arterioles and capillaries. Thicker blue vessels, which may protrude slightly above the skin, usually arise from venules and carry venous blood.
The shape of the vessels can be:
- linear - that is, represent practically one line or several lines running in parallel;
- arachnids - with a clearly defined center and rays diverging from it;
- tree-like - with a branching structure that looks like a tree.
Red capillary linear spider veins most often appear on the face. This disease is called rosacea. Red and blue linear and tree-like telangiectasias can usually be found on the legs.
Most often, spider veins appear on both legs, but usually there are significantly more of them on one side than on the other. Their most common location is the area under the knee. Next - the middle third of the outer surface of the thigh, the front and outer surface of the lower leg, the lower third of the inner surface of the thigh, ankles and foot.
The capillary mesh on the legs itself does not cause discomfort, it does not hurt and does not interfere with life. But, as we have already said, most often the appearance of “stars” and “mesh” indicates problems with blood vessels. According to the international CEAP classification, telangiectasia is the first stage of chronic venous diseases of the lower extremities [2]. This means that if symptoms such as heaviness in the legs, fatigue or swelling have not yet appeared, then there is a high probability of acquiring them in the future if there is no timely treatment.
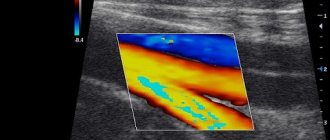
Diagnostics
To determine the cause of the appearance of spider veins and select a course of treatment, you need to consult a phlebologist. He conducts an examination, identifies the number and prevalence of spider veins, and risk factors for the development of varicose veins. Duplex ultrasound scanning is mandatory - this is a study that allows you to see the direction and speed of blood flow in superficial and deep vessels. Only after this can the doctor give his opinion and talk about the prognosis.
In addition, a phlebologist can give directions for examination of the condition of the liver, heart, female reproductive and hormonal systems. Since these factors can also cause disruption of blood supply and the appearance of dilated blood vessels in the legs.
Treatment of spider veins
Therapy for telangiectasia should be aimed not only at the purely cosmetic elimination of this symptom, but also at the cause of the manifestation of the vascular network in order to prevent the appearance of new formations in the future.
If the doctor suggests that you remove the asterisks and does not prescribe any other treatment, then after some time the vascular network will appear again. Such a specialist most likely hopes that you will return to him for a second course of treatment. But the disease can progress all this time.
The basis of treatment should be the elimination of provoking factors and the very cause of the appearance of the vascular capillary network. In therapy, external agents (ointments, gels) can be used to stimulate blood circulation at the site of application. Compression knitwear can also be included in this group. But these are only auxiliary methods that bring results only in combination with drug treatment.
Since spider veins on the legs are one of the first external signs of varicose veins, their treatment should be taken seriously. It is imperative to take medications with angioprotective and venotonic effects. To prevent thrombosis, it is also advisable to use antiplatelet agents. Also, in some cases, additional medications that suppress inflammation and pain are required.
Of course, it is difficult to take so many pills every day, so pharmaceutical companies are striving to develop drugs that will combine all of these actions at once. At the moment, such a drug is the new domestic drug “Angionorm”. It combines antiplatelet, antiplatelet activity, angioprotective and anti-inflammatory properties, venotonic and microcirculation-improving effects. That is, all the properties necessary for the treatment of varicose veins are “in one tablet.” It's convenient and profitable.
As for eliminating the cosmetic defect of the vascular network itself, a number of modern non-surgical procedures are used for this: for example, sclerotherapy (when a special solution is injected into the vessel, causing the walls of the vessels to stick together and their subsequent resorption), laser coagulation, ozone therapy and others. The specific method should be selected by a phlebologist, depending on the prevalence of telangiectasia, the thickness of the vessel and other factors. However, let us remind you that only an integrated approach - with the mandatory inclusion of drug treatment - will help not only remove existing stars, but also prevent their subsequent appearance, improve the condition of blood vessels in general and reduce or completely eliminate the symptoms of venous insufficiency and incipient varicose veins.
The appearance of spider veins, even in the absence of other symptoms, is the first sign that you should definitely consult a doctor. Timely and correct treatment will help not only get rid of a cosmetic defect, but also prevent or slow down the development of a serious disease. Take care of your health and don’t miss the moment.
Source: www.kp.ru
Vasculitis (pathology of skin vessels)
Many diseases of the vascular walls of the skin and internal organs have long been known and described in detail. However, in the last 2-3 decades there has been a tendency to combine these dermatoses into a separate nosological group, calling them “vasculitis” - vascular skin diseases. Clinically, the group of vasculitis is continuously expanding, new syndromes are being described, and attempts are being made to create a generally acceptable classification. The complexity of the issue lies in the extreme diversity and variegation of the clinical symptomatology of vasculitis, in the absence in most cases of reliable data on their etiology, in the significant differences in the pathogenesis of a number of diseases included in the general group of vasculitis.
Vascular dermatoses are the result of primary damage to the dermohypodermal (arterial, venous, capillary) vascular system. They can develop under the influence of allergic (hyerergic) mechanisms, hereditary burden, hormonal influences, infectious diseases, toxic and pharmacological factors, static load, radiation and temperature effects. Immunopathological mechanisms are of particular importance in the development of skin vasculitis. Shifts in the immunological status are most pronounced in patients with acute, disseminated and necrotic forms of skin vasculitis.
In the diagnosis of vasculitis, along with clinical symptoms, the results of pathohistological studies are of leading importance. Pathohistological manifestations are based on lesions of the vascular wall of a histological and submicroscopic (microcirculatory) nature, changes in the skin and subcutaneous tissue.
Allergic skin vasculitis
The participation of blood vessels in the formation of inflammatory skin diseases is an essential component of the pathomorphosis of many dermatoses. However, vascular reactions in diseases such as eczema, psoriasis, atonic dermatitis and many others are not the leading ones. In this regard, a group of dermatoses has been identified in which inflammatory damage to blood vessels occurs primarily, predominates in the pathological inflammatory reaction and requires specific pathogenetic treatment. In accordance with the currently existing classification (Shaposhnikov OK et al., 1989), allergic vasculitis of the skin is divided into 2 groups - superficial and deep. Superficial allergic vasculitis of the skin includes dermatoses accompanied by damage to capillaries, arterioles and venules of the dermis. The group of deep allergic vasculitis of the skin includes dermatoses in which medium- and large-caliber vessels located at the border of the dermis and hypodermis, as well as in the hypodermis, are affected.
Etiology and pathogenesis.
Vascular dermatoses are polyetiological diseases. Previously, the allergic component was considered the leading pathogenetic factor, but currently infectious and autoimmune mechanisms are distinguished. According to OK Shaposhnikov, in the formation of skin vasculitis, the main role is played by infectious effects, with the leading role played by streptococci and staphylococci. Viral flora, mycobacterium tuberculosis, and some types of pathogenic fungi are important. The participation of strepto- and staphylococci in the formation of vasculitis is confirmed by the following data: isolation of these microorganisms from lesions or foci of chronic infection, detection in the blood of high titers of antistreptolysin-0 and anti-a-toxin of staphylococcus, the presence of antibodies to streptostaphylococci, detection of high concentrations of antistaphylococcal hemagglutinins , as well as the reproduction of acute vasculitis in experimental animals (monkeys, rabbits) when they are administered an immune complex - streptoantigen with antistreptococcal antibodies. The pathological autoimmune reaction observed in patients with allergic vasculitis of the skin is ensured by the insufficiency of the functional activity of humoral and cellular factors of the T-system of immunity, the presence of an increased concentration of circulating immune complexes in the blood and their deposition in the vascular endothelium. A correlation has been established between the concentration of immune complexes, the antigen-antibody reaction and the severity of vasculitis. Most authors studying the pathogenesis of skin vasculitis emphasize the complex effect of many factors: infection, immune deficiency, changes in blood coagulation properties, hypovitaminosis, exogenous provoking influences (radiation, drug intolerance, trauma, intoxication, temperature changes), as well as endogenous disorders (neurovisceral disorders, hormonal and cardiovascular pathology).
Clinical picture.
Clinical symptoms vary depending on the size and type of affected vessels, the severity of inflammatory pathological symptoms and the participation in the pathomorphosis of homeostasis disorders, neuroendocrine and visceral pathology.
Superficial allergic vasculitis of the skin includes hemosiderosis (hemorrhagic-pigmentary dermatoses), hemorrhagic vasculitis (Henoch-Schönlein disease), Ruther's allergic arteriolitis, nodular necrotizing vasculitis (Werther-Dümling dermatitis), hemorrhagic leukoclastic microbid (Miescher-Storck microbid) and acute smallpox lichenoid parapsoriasis (Habermann-Fly type of parapsoriasis).
The group of deep allergic vasculitis of the skin includes various clinical types of erythema nodosum, manifested in acute and chronic forms.
Superficial allergic vasculitis
Hemosiderosis (hemorrhagic pigmentary dermatoses). Diseases of this group are various nosological purple-pigmented lesions that form as a result of inflammatory changes in the endothelium of capillaries and precapillaries with the deposition of iron-containing pigment - hemosiderin and an increase in hydrostatic pressure in the vessels. These include a number of clinical varieties: ring-shaped, telangiectatic purpura (Majocca's disease), Schamberg's disease, purpuric lichenoid pigmentary dermatitis (Gougerot-Blum syndrome), eczematoid purpura (Dukas-Kapetan-kis), pruritic purpura (Leventhal), arcuate telangiectatic purpura ( Touraine), angiodermitis purpurosa pigmentosa (ocher dermatitis, Favre-Chais syndrome), white cutaneous atrophy (Miliana), reticular senile hemosiderosis and orthostatic purpura. The listed clinical varieties of skin hemosiderosis are often combined in the same patient and are often different stages of a single pathological process, which is based not only on inflammation of the endothelium of precapillaries and capillaries, but also on a violation of their permeability, increased fragility with sweating of formed elements and protein components of the plasma .
Annular telangiectatic purpura (Majocca's disease) and arcuate telangiectatic purpura (Touraine's disease)
- diseases of the same type, as they manifest themselves as similar purpuric spots of oval-round or arcuate shape, formed as a result of dilation of capillaries, telangiectasia and individual point hemorrhages. The process proceeds in stages from the initial telangiectatic phase with hemorrhagic pigment efflorescence to the final stage of atrophy. Atrophy is often focal, in the area of the follicles. There are no subjective sensations. Sometimes isolated, purple spots are observed on the mucous membranes of the oral cavity.
Progressive pigmentary dermatosis of Schamberg
(dermatosis pigmentosa progressiva Schamberg).
The disease occurs almost exclusively in men. A rash of pinpoint, scattered, red-brown spots appears, usually comparable in appearance to cayenne pepper grains. As a result of the fusion of spots and the deposition of hemosiderin, round, pigmented plaques riddled with telangiectasia are formed. During diascopy, the spots do not disappear, but only fade slightly; in the later stages of the process, atrophy, thinning and depigmentation of the skin develop in the lesions. The rash first appears on the legs, and then spreads to the feet and thighs. Occasionally, the skin of the trunk and upper extremities is involved in the process. The disease has a chronic course. After a few months from the onset of the disease, the rash begins to resolve, although the entire process can last many years. The etiology is unclear. Pay attention to the disturbance of cholesterol metabolism in these patients.
The lesions are a consequence of fragility and endothelial proliferation of capillaries. In the last stage of the process, hemosiderin deposits and slight epidermal atrophy occur.
Lichenoid purpuric pigmentary dermatitis (Gougerot-Blum syndrome)
occurs chronically. The rashes are represented by hemorrhagic pigmented spots of a yellowish-brown color. Against their background, in the center are towering round or polygonal papular elements the size of millet grains of intense purple color. When lichenoid efflorescences merge, plaques of various sizes, round or irregular in shape, with peeling on the surface are formed. Mild itching is noted. The general condition of the patients is not disturbed.
Most often the process is localized on the lower extremities, and then the rash spreads to the trunk, upper extremities and face. In children, Gougerot-Blum dermatitis initially forms on the face and upper extremities, accompanied by burning, itching or paresthesia. Rashes in children manifest as erythematous-lichenoid efflorescences or plaques, with a diffuse progressive spread of the rash. The course of dermatosis is chronic, relapsing. The diagnosis is based on characteristic lichenoid elements combined with erythematous-squamous spots, which makes it possible to differentiate this disease from lichen planus, in which the rash is monomorphic. Gougerot-Blum dermatitis differs from eczema and atopic dermatitis by the presence of purple spots, telangiectasia, and a positive Konchalovsky-Rumpel-Leede sign.
Eczematoid purpura (Doukas-Kapetanakis)
characterized by the appearance of erythematous-squamous spots of varying sizes, yellowish-brown in color, with slight pityriasis-like peeling and the presence of hemorrhage. Individual elements sometimes become eczematized, especially when localized on the legs. The rashes appear symmetrically, first on the legs, then on the thighs, buttocks, and torso, and are sometimes accompanied by itching. The disease occurs in both men and women at any age, most often from 40 to 50 years.
Classification
The disease is divided into many subtypes, differing in the causes of development, localization, specificity, and type of affected vessels. There are two main forms:
- primary vasculitis (or leukocytoclastic), which is an independent disease and not accompanied by other pathologies;
- secondary (or rheumatoid), developing against the background of other diseases - rheumatoid arthritis, dermatomyositis, systemic lupus erythematosus.
Vasculitis of the lower extremities is also divided into diseases of large, medium or small vessels.
According to the severity of the pathology, there are:
- mild - the rash is not extensive, the general condition of the person is unchanged;
- medium - the rash is clearly expressed, pain in the joints, red blood cells are detected in a urine test, the patient feels weakness, loss of appetite;
- severe - rashes over almost the entire surface of the body, noticeable changes in the joints, kidney failure develops, pulmonary and intestinal bleeding are common, the person’s condition is classified as severe.
Based on localization, vasculitis is divided into segmental (affecting individual areas) and systemic, when there is no specific location. The second option is the most difficult to treat, since vascular inflammation occurs in different parts of the body, which complicates the possibility of adequate therapy.
In medical practice, the disease is classified according to Ivanov’s method, recommended for use:
- dermal - damage to the vessels of the upper layer of the skin, which is divided into several subtypes depending on the clinical picture (hemorrhagic, urticarial, ulcerative-necrotic, etc.);
- dermohypodermal - a disease of the vessels located between the upper and deep layers of the skin, manifested in a nodular form, often with ulcerations;
- hypodermal - damage to blood vessels in the deep layers of the skin, often manifested by a nodular-ulcerative course.
Each type and subtype of the disease has a separate clinical picture.
Symptoms and manifestations
At the initial stage of vasculitis there are no pronounced symptoms, and it happens that the disease is not immediately recognized. Despite the fact that its manifestations are varied, there are common signs:
- inflammatory changes in the skin;
- the appearance of edema, rash, hemorrhage, necrosis;
- the lesion appears symmetrically on both legs;
- rashes appear in the form of red dots, nodules, erosion, ulcers;
- the initial manifestation occurs mainly on the legs.
Vasculitis is characterized by the presence of purpura. This is a reddened area rising above the surface of the skin, which can be clearly felt with your fingers .
In addition, a person feels joint and muscle pain, general weakness, itching and burning in the affected areas of the skin, and his temperature rises above 38 degrees.
When vessels of different sizes are affected, the symptoms of the disease are somewhat different:
- Small vessels. Small red spots on the legs, blisters, superficial ulcers, the affected areas are swollen and hardened. A person complains of stomach cramps, inflammation of the eyes, and possible hemorrhage in the lungs.
- Medium vessels. Subcutaneous nodes and affected areas become bluish, deep ulcers, gangrene, neuritis appear on the fingers, and the walls of blood vessels become thinner. The patient's blood pressure increases and there is a risk of heart attack.
- Large vessels. The appearance of bruises, dilatation of the aorta, lack of pulse.
Causes of the disease
To this day, the reasons causing the development of pathology have not been fully studied. The main provoking factor is considered to be a failure in the body’s immune system. The trigger can be a previous infectious disease, especially a viral one.
As inflammation progresses, it increasingly affects the blood vessels, impairing the blood supply to the organ, which leads to hemorrhage and necrosis, since in the absence of adequate nutrition the cells die.
The following factors can provoke damage to the blood vessels of the lower extremities:
- frequent colds without appropriate treatment;
- hereditary predisposition;
- inflammation of the thyroid gland;
- diseases that have become chronic;
- untreated or advanced arthritis;
- tendency to allergies.
Constant stress, hypothermia, injuries, and uncontrolled use of certain medications have a negative impact.
Sometimes bruises appear on the skin along with the rash.
Experts believe that the cause of their occurrence is autoimmune disorders, while in other cases, vasculitis is provoked by hereditary diseases and ailments caused by a malfunction of internal organs.
Causes of the disease
The root cause of this pathology is an allergic lesion of the body. The triggering of such a reaction is provoked by a number of unfavorable factors. Often we are talking about food, chemicals or medicines. An important requirement is that the trigger must provoke an atypical reaction in the body. Allergens themselves can be different, so there are different forms and symptoms of the disease.
This type of lesion often occurs in children. For them, this pathology is many times more severe. Quite often, capillary toxicosis can develop against the background of complicated tonsillitis, after medical interventions. In general, capillary toxicosis in children is most often the result of the direct influence of an allergen on a weak, unprotected organism. In adults, the principle of development of the disease is slightly different. Capillary toxicosis in adults is provoked by a latent infection. With hemorrhagic vasculitis, the damage can spread to any organs. That is, the disease quite often develops in the kidney and cardiac structures.
In general, we can identify the following etiological factors that provoke capillary toxicosis:
- acute bacterial infections;
- long-term infectious diseases with frequent relapses;
- viral diseases;
- radioactive or radiation exposure;
- diabetes;
- systemic diseases;
- allergic reaction to medications or vaccinations;
- frequent and prolonged hypothermia.
A reason such as a hereditary predisposition to the disease cannot be ruled out.
Which doctor treats, how is the disease diagnosed?
When the first signs indicating this disease are detected, a person is interested in which doctor is treating it.
If you notice a rash on the skin of your legs or any other symptoms of vasculitis, you should consult a physician. To make the correct diagnosis, he will refer you for a consultation to specialized specialists - a dermatologist, rheumatologist, neurologist, allergist, hematologist and others .
The attending physician prescribes additional examination:
- clinical and biochemical analysis of blood and urine;
- ECG, X-ray, ultrasound;
- biopsy;
- immunological analysis.
Most often, if the disease is detected for the first time, the final diagnosis is made by a rheumatologist, who, if necessary, refers the patient to a specialist. He, based on the existing conclusion, prescribes treatment aimed at eliminating the cause of vasculitis.
After completion of therapy, the patient must be monitored by appropriate doctors for two years to avoid relapses.
Treatment
To get rid of vasculitis, drug treatment is required. In each case, therapy is selected individually after establishing the exact form of the disease.
Traditional methods
Classic treatment consists of taking medications such as:
- non-hormonal anti-inflammatory drugs (Naproxen, Indomethacin), which relieve inflammation and pain, but they are contraindicated for stomach ulcers, kidney and liver diseases, and during pregnancy;
- glucocorticosteroid drugs, for example Prednisolone, to suppress the immune system, which has become aggressive to its own body;
- cytostatic substances (“Cyclophosphamide”) that slow down cell division;
- antihistamines (“Suprastin”), if the erythematous nodosum form of the disease is diagnosed;
- products containing vitamin C and calcium, which help maintain vascular tone and prevent their fragility.
Physiotherapeutic procedures will be useful - ultraviolet blood irradiation, plasmapheresis, oxygen therapy.
Traditional therapy
Folk remedies also have a positive effect in the treatment of vasculitis. In order to avoid negative consequences, you should consult a doctor before using them.
For therapy use:
- decoctions of violet, a collection of nettle leaves, knotweed, elderflower flowers, yarrow, Japanese sophora berries;
- homemade ointments from a mixture of birch buds and interior fat, from pine resin, which can be used to smear sore spots;
- elderberry infusion, alcoholic lemon tincture.
Treatment with decoctions of plants containing vitamins is useful. Black currant leaves, St. John's wort, and rose hips are used.
To improve blood supply to the legs, exercises such as “bicycle”, “scissors”, “birch”, and lifting to the tips of the toes are recommended.
Treatment of vasculitis
Therapy in this case has several goals:
- preventing the development of the disease and complications;
- eliminating the threat of death (in especially severe cases);
- relieving the patient of unpleasant symptoms;
- preventing the occurrence of pathology in the future.
The use of glucocorticoids - drugs based on hormones produced by the pancreas (Prednisolone), and cytostatics - drugs that help slow down the processes of cell division (Cyclophosphamide) helps reduce the inflammatory process. Treatment of vasculitis is long-term and is carried out in a hospital setting. For mild forms of the disease, non-steroidal drugs can be prescribed. For example, Indomethacin. Non-hormonal drugs are better tolerated by patients; their use is not accompanied by side effects.
As a supplement for vasculitis, medications are used to help dilate blood vessels and restore the elasticity of the vascular wall, preventing the occurrence of thrombosis.
Vasculitis can be fatal. Without treatment, death occurs in more than half of all cases of the disease. The five-year survival rate of patients with timely medical care ranges from 60 to 90%.
YOU WOULD BE INTERESTED
Hemorrhagic stroke