Heart failure is a condition in which the heart muscle cannot contract fully. As a result, the organs suffer from a lack of blood.
The outcome of this condition is decompensated heart failure. Various instrumental methods are used for diagnosis, treatment is carried out conservatively and surgically.
Decompensated heart failure - end-stage disease
What is heart failure
The concept of heart failure refers to a condition in which the myocardium loses the ability to fully contract. This leads to insufficient blood supply to all organs.
There are two forms of HF:
- acute, associated with sudden and extensive myocardial damage (infarction, trauma);
- chronic - occurs more often, develops gradually.
It is for chronic heart failure that a decompensation phase is characteristic, which is characterized by a deep and irreversible impairment of the contractile function of the myocardium. Since the myocardium has pronounced compensatory abilities, this phase begins several decades after the onset of the disease.
Causes
There are several theories according to which chronic myocardial failure develops. The pathogenesis of the disease is based on a decrease in the ability of the heart to fill and empty, caused by various damage to muscle tissue.
The most common causes of decompensation of CHF are:
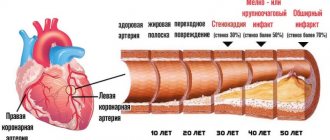
- cardiac ischemia;
- previous heart attack with extensive myocardial damage;
- severe hypertension;
- dilated cardiomyopathy;
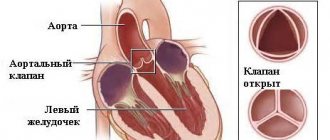
- congenital and acquired heart defects;
- diabetes mellitus not related to insulin.
In addition to the main causes, there are several factors that can aggravate the course of CHF and accelerate the development of decompensation.
These factors include:
- episodes of myocardial ischemia;
- heart rhythm disturbances;
- mitral prolapse;
- renal dysfunction;
- thyroid diseases;
- the effect of certain medications;
- poor nutrition combined with physical inactivity;
- abuse of alcohol, nicotine.
A decrease in immunity is of some importance, since every cold affects the condition of the myocardium.
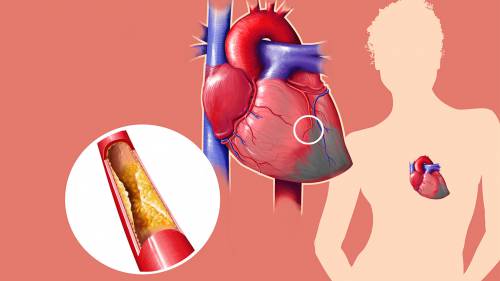
One of the main causes of pathology is coronary heart disease
Symptoms
What is decompensated heart failure? If we consider the symptoms of the disease, we can see that it is characterized by the same manifestations as the initial stages of heart failure, but they are more pronounced.
A patient with heart failure in the stage of decompensation will present the following complaints:
- shortness of breath on exertion, fatigue - in 98% of patients;
- palpitations - in 80% of patients;
- coughing, asthma attacks are observed quite rarely.
The objective symptoms include the following:
- Almost every patient has high blood pressure;
- increased heart rate;
- the presence of swelling in the legs, in the abdominal cavity;
- swelling of the neck veins;
- increase in liver size;
- cyanosis of the face, lips, fingertips;
- changes in the terminal phalanges of the fingers like drumsticks;
- percussion enlarged the borders of the heart;
- wheezing in the lungs indicates stagnation of venous blood.
The classic triad of signs for CHF is a combination of edema, shortness of breath and wheezing in the lungs. However, these symptoms can also be observed in other diseases of the cardiac and respiratory systems, so they cannot be considered fundamental for making a diagnosis.

Almost every patient with HF has shortness of breath
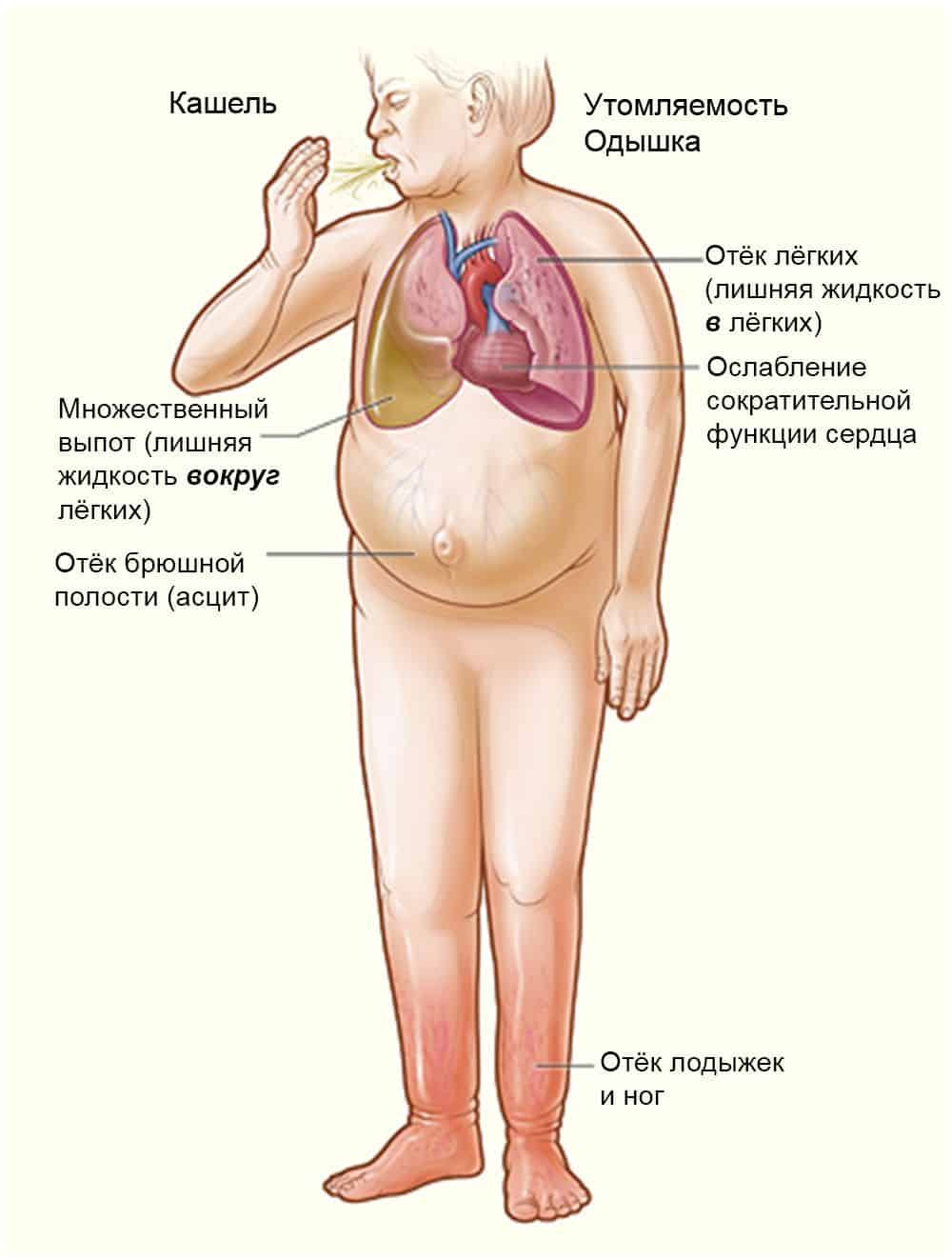
Characteristic signs of cardiac dysfunction
Diagnostics
To accurately confirm the diagnosis, a number of instrumental examination methods are used.
Table. Methods for diagnosing decompensated heart failure.
| Method | Possible changes |
| Electrocardiography |
|
| Holter monitoring | Daily ECG recording is of auxiliary value - it allows you to identify arrhythmias that can aggravate the course of the disease |
| Echocardiography | The method is paramount in the diagnosis of decompensated heart failure. It allows not only to detect dysfunction of the heart muscle, but also gives an assessment of its severity. The main parameter of cardiac ultrasound is the ejection fraction of the left ventricle, which allows one to determine the degree of impairment of cardiac contractility |
| MRI | A highly accurate method that allows you to determine the volume of the heart muscle and the thickness of the walls of the heart cavities. MRI allows you to detect the slightest scar changes and assess the degree of blood supply to muscle tissue |
Assessment of the general condition of the body and a person’s adaptability to physical activity is carried out using stress tests. The patient is asked to perform some physical exercise, at which time an ECG is recorded. After the end of the load, the pulse is calculated and blood pressure is measured.
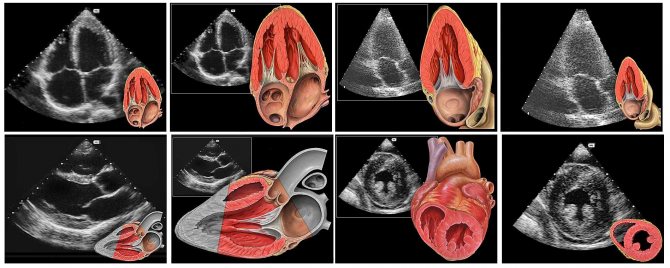
Ultrasound allows you to determine decompensation of heart failure with the greatest accuracy.
Laboratory diagnostics are of particular importance in identifying decompensated CHF.
The following changes may be detected:
- blood clotting disorder;
- anemia;
- the appearance of protein in the urine;
- increased levels of urea and creatinine.
One of the modern diagnostic methods is to determine the level of natriuretic peptide. If its content in the blood plasma increases, the patient should be examined for HF. A specialist will tell you more about diagnostic methods in the video in this article.
Compensation
Almost any organ or organ system has compensation
, ensuring the adaptation of organs and systems to changing conditions (changes in the external environment, changes in the body’s lifestyle, exposure to pathogenic factors). If we consider the normal state of the body in a normal external environment as equilibrium, then the influence of external and internal factors puts the body or its individual organs out of balance, and compensation mechanisms restore balance by introducing certain changes in the functioning of the organs or changing them themselves. So, for example, with heart defects or with constant significant physical activity (in athletes), hypertrophy of the heart muscle occurs (in the first case it compensates for the defects, in the second it provides more powerful blood flow for frequent work at increased load).
Compensation is not “free” - as a rule, it leads to the fact that the organ or system works under a higher load, which may cause a decrease in resistance to harmful influences.
Treatment methods
Therapeutic measures for decompensated heart failure are aimed at slowing down further progression of the disease, protecting target organs, and improving the patient’s quality of life.
These goals are achieved by carrying out the following activities:
- diet;
- establishing a physical activity regime;
- psychologist consultations;
- taking medications;
- electrophysiological correction of heart function;
- surgical intervention.
The greatest effectiveness of treatment is achieved by combining all of the above methods.
Diet
Therapeutic nutrition for decompensated heart failure helps normalize blood pressure, reduce the load on the heart, and provide the body with the necessary nutrients.
The diet is based on the following principles:
- reducing salt intake to 1 g per day;
- reducing fluid intake to one and a half liters per day;
- providing the necessary calorie content, sufficient protein content in food;
- enriching the diet with vitamins.
Body weight should be measured regularly. A weight gain of more than 2 kg in 3 days indicates an accumulation of fluid in the body.
An unfavorable sign is a decrease in body weight. A progressive decrease in the volume of fat and muscle tissue is called cardiac cachexia. This condition requires the introduction of specialized nutritional mixtures into the diet.
Physical activity
Physical activity is indicated for patients with decompensated heart failure, but with certain restrictions.
Contraindications to physical activity are:
- acute myocarditis;
- stenotic defects;
- severe arrhythmias;
- frequent attacks of angina pectoris.
For other patients, the degree of physical activity is determined by a six-minute test. Physical activity begins with breathing exercises, after 3-4 weeks the person moves on to light gymnastics. Simple and Nordic walking is considered the most optimal option for physical activity.
Recommendations for the regimen
Patients with decompensated heart failure are subject to some lifestyle restrictions:
- Abrupt climate change is not recommended;
- air travel is limited to no more than 2.5 hours without a break;
- smoking is excluded;
- sexual activity is limited;
- It is recommended to avoid emotional stress;
- it is necessary to get a full night's sleep;
- It is recommended to take short breaks from studying during the day.
Instructions on daily routine, nutrition, and lifestyle are given to the patient in special cardiology schools, which are organized at some medical institutions.
Drug therapy
Drugs used to treat CHF are divided into three groups according to their effectiveness:
- the main ones have proven effectiveness;
- additional - the effect is not present in all patients;
- auxiliary - used symptomatically.
The main group includes 6 classes of drugs.
Table. Drugs for the treatment of heart failure.
| Group of drugs | Effect | Method of appointment | Peculiarities |
| ACE inhibitors - Lisinopril, Ramipril, Enalapril | Slow down the progression of decompensation by reducing preload on the heart and reducing heart rate | Reception is started with minimal doses; if well tolerated, the dose is increased until the desired effect is achieved. | It is necessary to interrupt treatment with these drugs if:
|
| Beta blockers - Metoprolol, Atenolol | Slowing down the destruction of cardiomyocytes, stimulating the work of cardiac tissue, reducing heart rate, reducing the degree of ischemia | Prescribed in combination with an ACE inhibitor, taking a minimum dose, which is gradually increased | During the first two weeks of treatment with beta blockers, the condition may worsen slightly. This is due to a decrease in cardiac output, then the number of functioning cardiomyocytes increases and the condition returns to normal. |
| Aldosterone antagonists - Spironolactone | Helps remove excess fluid, reduces swelling | Prescribe high doses of the drug, which are gradually reduced as the condition improves | With long-term use, it is possible to develop gynecomastia - enlargement of the mammary glands in men. |
| Diuretics - Furosemide, Hypothiazide | Used to remove excess fluid and reduce the volume of bcc | Indicated for severe symptoms of decompensation | Simultaneous administration of potassium is necessary, since diuretics wash it out of tissues |
| Cardiac glycosides - Digoxin | Improve symptoms and improve the patient’s quality of life | Prescribed in minimal dosage | In women, digoxin is more likely to cause intoxication. |
| Angiotensin 2 receptor antagonists - Valsartan, Candesartan | Reduce the risk of death | Start with the minimum dose and gradually increase | The safest and most effective drug |
Additional drugs are prescribed in the presence of atherosclerosis, hypertension, and blood clotting disorders. They do not have a direct effect on the course of heart failure, but they reduce the severity of risk factors.
- Statins - Atorvastatin, Rosuvastatin. Indicated in the presence of severe atherosclerosis. Helps normalize cholesterol levels.
- Anticoagulants - Warfarin. Indicated for high risk of thrombosis in elderly patients.
These medications are prescribed by the attending physician if indicated. Auxiliary drugs are prescribed according to strict indications, as they do not have a positive effect on the course of heart failure.
The following groups are used:
- nitrates;
- calcium channel blockers;
- antiarrhythmics;
- antiplatelet agents;
- non-glycoside inotropes;
- cytoprotectors.
Patients with CHF are not recommended to take NSAIDs, glucocorticoids, or antidepressants. These drugs have a negative effect on the course of the disease.
Electrophysiological methods
Three main procedures are used:
- placement of a pacemaker;
- placement of ventricular electrodes;
- installation of a cardioverter-defibrillator.
Methods are used only after intensive drug therapy if its effectiveness is insufficient.
Surgery
Indicated when conservative therapy is unsuccessful. Several types of surgical interventions are performed.
- Coronary artery bypass grafting. The operation is aimed at restoring the vascular network of the myocardium and improving its blood circulation.
- Correction of mitral regurgitation. Performed in the presence of mitral prolapse.
- Heart transplantation. The most effective method for terminal heart failure, but the possibility of its use is limited.
Contraindications to surgical treatment are severe bleeding disorders, liver cirrhosis, and renal failure.
Decompensated heart failure is a serious condition, often resulting in death. It develops as a result of a breakdown in the compensatory capabilities of the myocardium.
The clinical picture consists of symptoms of circulatory disorders of internal organs. Treatment is carried out comprehensively, using medicinal and non-medicinal methods, and surgical intervention.
Diabetes mellitus type 2 subcompensation treatment
For diabetes of any type, it is customary to distinguish three variants of the course of the disease:
- Compensation stage;
- Subcompensated form;
- Decompensated stage.
Compensated diabetes is a course of pathology in which blood sugar levels are close to normal and, accordingly, there is no risk of developing diabetic complications. This can be achieved by constantly using prescribed medications, following a diet and adhering to a certain lifestyle.
The decompensated phase of diabetes mellitus is a consequence of insufficient therapy or its complete absence. At this stage of the disease, there is a high probability of developing ketacidosis, hyperglycemic coma.
A constant high level of glucose in the blood causes vascular damage, which in turn leads to impaired kidney function, visual function and the cardiovascular system suffer. Decompensation is difficult to reverse, the patient’s state of health is poor, and the prognosis for the course of the pathology is unfavorable.
Subcompensated diabetes mellitus is a borderline state between compensation and decompensation of the disease. Symptoms of the disease progress, and the risk of developing acute complications is increased.
With a prolonged phase without transition to a compensated form, the likelihood of late diabetic complications increases. Patients with subcompensated diabetes need to reconsider treatment and diet therapy.
Compensation for diabetes is easier to achieve in the second type of non-insulin-dependent disease. Type 1 pathology leads to irreversible destruction of insulin-producing cells, which is why treatment of this form of diabetes is more difficult.
More than half of patients live with subcompensated diabetes. To prevent the disease from passing into the decompensated phase, it is necessary to constantly be examined and, based on the tests, adjust therapy.
Subcompensated diabetes is an average condition when a person has diabetes mellitus of an average type between compensation and decompensation.
Compensation is an improvement in the patient’s health when all parameters are closer to normal due to medical therapy.
Decompensation is the reverse process when diabetes mellitus can cause serious complications in the patient's condition. With subcompensation, about 50 g of sugar is excreted in the urine.
Blood glucose levels are no more than 13.8 mmol/liter. Acetone cannot be detected. But with decompensation it can appear.
Hyperglycemic coma, when the patient develops subcompensation of diabetes mellitus, is impossible. Of course, the patient does not have the best state of health, but it is quite stable and does not worsen if all the rules and requirements for treatment are followed.
Subcompensated diabetes mellitus is a fairly serious condition that can cause dangerous health consequences. To make an accurate diagnosis and select treatment, it is necessary to conduct a detailed diagnosis.
There are a number of criteria that help determine the degree of compensation. Based on the research results, specialists prescribe medications and give recommendations for lifestyle correction.